Abstract
Background
The coronavirus disease (COVID-19) pandemic has been a continuous global threat since the first identification of the disease in December 2019. COVID-19 vaccination is a crucial preventive approach that can halt this pandemic. However, many factors affect the willingness of the public to be vaccinated against COVID-19 at the early stage of the vaccination programme. We used network analysis to investigate the interrelation of vaccination willingness and its associated factors.
Methods
A population-representative sample of 539 Chinese adults completed a battery of online self-assessments, including those on vaccination willingness, health status, attitude towards vaccines, COVID-19-related psychological elements and other variables. Network analysis was performed using the R qgraph package.
Results
In total, 445 (82.6%) participants scored high on their willingness to vaccinate. Attitude towards vaccines, the influence of people around an individual and health status were directly significantly related to vaccination willingness. The betweenness of age was the highest and, the emotional states had the strongest centrality.
Limitations
Network analysis is not sufficient to determine the causal relationships of the links between nodes. In addition, there are other latent essential elements that were not evaluated. Finally, the sample size was relatively small.
Conclusion
Network analysis showed that attitude toward vaccines and emotional states are the most critical factors affecting vaccination willingness, which indicates that we should pay attention to the impact of the dissemination of Internet information on vaccination willingness and public emotional states during a pandemic which is very important for promoting vaccination programs.
Keywords: COVID-19, Vaccination willingness, Associated factors, Early stage, Network analysis
1. Background
The coronavirus disease (COVID-19) pandemic has been a continuous global threat since the first identification of the disease in December 2019. Unfortunately, there is currently no specific antiviral treatment for COVID-19 (Borges do Nascimento et al., 2021; Huang et al., 2020). Vaccination against COVID-19 has been considered one of the most promising and cost-effective health interventions for the prevention and control of the pandemic. On this basis, the development, testing and use of vaccines are unprecedented (Lurie et al., 2020). There are conventional inactivated vaccines (from Sinovac, Bharat Biotech, and Sinopharm), viral vector vaccines (from Oxford-AstraZeneca and Gamaleya Research Institute), and RNA vaccines (from Moderna and Pfizer-BioNTech), which have been adopted in the latest vaccination programs of a number of countries, including China, Russia, the United States, the United Kingdom and India (Kim et al., 2021).
At the beginning of the pandemic, a few studies surveyed adults to assess public willingness to be vaccinated against COVID-19. Although many of these studies were based on non-representative convenience samples, most of the sampled population intended to be vaccinated (Lazarus et al., 2021; Reiter et al., 2020). However, with the development of the pandemic, a large amount of incorrect information about COVID-19, such as information underestimating the severity of the pandemic or ignoring the detrimental effects of the pandemic, has spread widely (Roozenbeek et al., 2020). At the same time, there have been many reports on the Internet about problems after vaccination, such as fever, muscle soreness and even immune system diseases (Kelly et al., 2021; Palacios et al., 2020). These findings have led to increasing public doubts about the safety and reliability of the vaccine, all of which may affect expectations for vaccination. Many studies have shown that people's willingness to vaccinate gradually decreases over time (Finney Rutten et al., 2021; Robinson et al., 2021; Wang et al., 2021).
Thus, to control COVID-19, it is very important to understand the public's willingness to vaccinate and the associated factors, which can serve as an early warning system to prompt necessary measures to prevent the decline of vaccine acceptance and trust. Numerous studies have begun to focus on the factors that may influence people's willingness to vaccinate (Abedin et al., 2021; Robinson et al., 2021). For example, in a systematic review and meta-analysis of 28 nationally representative samples from 13 countries, Robinson and colleagues showed that being younger, having a lower education level, having a lower income and belonging to an ethnic minority group were consistently associated with being less likely to intend to vaccinate (Robinson et al., 2021). In addition, Palgi et al. found that vaccine hesitancy contributed to high clinical levels of anxiety, depression and fear among the vaccinated population (Palgi et al., 2021). Taylor et al. reported that vaccination attitudes were closely related to awareness of the pandemic, such as the dangerousness of COVID-19 (Taylor et al., 2020). Many patients with active chronic diseases, such as systemic lupus erythaematosus (Mason et al., 2021), malignant tumours (Thakkar et al., 2021) and Guillain-Barré syndrome (Maramattom et al., 2021), are not recommended to be vaccinated, so people's health status has a great impact on vaccination. Due to people's social attributes, people are also affected by the people around them during the pandemic (Singh and Misra, 2020), and their coping styles and knowledge about COVID-19 also affect their willingness to vaccinate (Finney Rutten et al., 2021; Taylor et al., 2020). However, it is unclear whether these factors that may affect the willingness to vaccinate are related to each other.
Network analysis presents the characteristics and information of a system in the form of a network. The system is composed of "nodes" and "edges". Network analysis presumes that nodes (such as factors, symptoms, or other psychopathological features) are clustered because they are, in some way, causally linked to one another. In network analysis, links are called "edges". The existence of significant links does not mean that nodes are affected by some potential factors such as latent variables. Instead, network analysis presumes that nodes may directly affect each other. If there is a causal relationship between nodes, the change in the central node is most likely to lead to the change in other nodes in the network through the diffusion of activation. Compared with the peripheral nodes, the central nodes are the defining feature of the network. Identifying central nodes has the potential to inform which elements to target in interventions. Significant edges might represent causal effects (directional or unidirectional), but experimental designs are required to determine causality. Therefore, network analysis provides a source of assumptions regarding causal relationships between variables in a network (Epskamp et al., 2018; Taylor et al., 2020). Among the network analysis methods, the Gaussian graphical model has the longest history and is the most widely used (Epskamp et al., 2018). This model can obtain indicators that are difficult to capture with the traditional latent variable model and describe the correlations and structure between the observed variables. In the process of research on practical problems, these indicators can often provide researchers with important insights into the relationship between variables (Borsboom, 2008; Epskamp et al., 2018). Centrality is an important index in network analysis; it represents the number, strength and closeness of a node with other nodes, including the strength, expected influence, closeness and betweenness. Changes in nodes with a higher centrality affects other nodes to a greater extent (Epskamp et al., 2018). From the perspective of cognitive-behavioral approaches to vaccination, emotional states and pandemics, the use of network analysis has a good theoretical framework because cognitive-behavioral models suggest that the factors in a network interact with each other.
Accordingly, the purpose of this study was to use network analysis to further explore the relationship between the elements that may influence willingness to vaccinate against COVID-19. It is unknown how vaccination willingness is related to age; income; health status; knowledge about pandemics; and other COVID-19 related mental elements, such as depression, anxiety, hypochondria, awareness of COVID-19 risk, attitude towards vaccines, the influence of people around the individual and coping style during the pandemic. It is also unknown how these factors are interconnected with one another. Based on a review of the previous literature, the elements that may affect vaccination willingness are listed in Table 1 .
Table 1.
Variables and their corresponding scales used in the network analysis.
| Variable (and scale) | No. of items | McDonald's ω | Sample item |
| Education | 1 | - | |
| Income | 1 | - | |
| Age | 1 | - | |
| Health status | 1 | - | |
| Vaccination willingness | 1 | If the unit/community organizes vaccination, will you participate? | |
| Influence of other people's choices on vaccination willingness | 1 | In general, what percentage (%) of people around you have been vaccinated? You will decide to vaccinate as soon as possible. | |
| Attitude towards vaccines | 8 | 0.81 | I think vaccination is very important. |
| Perception of the risk of coronavirus disease | 9 | 0.82 | Coronavirus disease is a serious disease. |
| Knowledge level of coronavirus disease | 5 | 0.79 | What is the recommended age group for vaccination? |
| Depression (PQEPHE) | 6 | 0.82 | Lack of energy, mental fatigue, inattention, or poor memory. |
| Neurasthenia (PQEPHE) | 5 | 0.76 | Uncontrolled thinking. |
| Fear (PQEPHE) | 6 | 0.78 | Worrying about yourself and your family being infected. |
| Obsession and anxiety (PQEPHE) | 6 | 0.76 | Knowing that something will not help, but being unable to control repeatedly thinking about or doing it, such as repeatedly washing one's hands. |
| Hypochondriasis (PQEPHE) | 2 | 0.73 | Going to the hospital to see a doctor to determine if you are infected. |
| Positive coping tendency (SCSQ) | 12 | 0.72 | An attitude and method that may be adopted when encountering setbacks: trying to see the good side of things. |
| Negative coping tendency (SCSQ) | 8 | 0.71 | An attitude and method that may be adopted when encountering setbacks: trying to forget the whole thing. |
Abbreviations: PQEPHE, Psychological questionnaire on emergent public health events; SCSQ, Simple Coping Style Questionnaire.
2. Methods
2.1. Study design and participants
From May 8 to June 4, 2021, we performed a cross-sectional survey. Unvaccinated Chinese adults aged 18–60 years old were invited to participate in an anonymous self-report online survey delivered in Chinese through Wen Juan Xing (https://www.wjx.cn/vm/YIIyx1V.aspx), a professional online questionnaire survey platform. During this period, we collected data at the beginning of the large-scale implementation of the national vaccination program in China.
A total of 1000 questionnaires were distributed. Filters were used to exclude data from participants who submitted incomplete or careless responses. Based on the length of our questionnaire, a certain amount of time was required to complete the questionnaire. Therefore, we eliminated questionnaires that were completed in a very short time. We assumed that respondents who completed the questionnaire very quickly were likely to have filled it out without carefully reading and understanding the questionnaire items. In addition, the questionnaire could be submitted only after all the questions were completed, so there were no missing values in our dataset. After applying the above exclusion criteria, 546 questionnaires were obtained. Finally, we also excluded seven samples with obvious logical errors on forward- and reverse-worded items. At the same time, to encourage the subjects to better complete the survey, we gave each respondent who had completed the questionnaire an economic reward.
A population-representative sample was obtained by stratified random sampling through Wen Juan Xing, which preserves a pool of latent subjects who have agreed to be contacted to participate in investigations. According to the data from the seventh China census, men and women account for 51 and 49% of the total population, respectively, so we stratified the dissemination of the questionnaire accordingly. Wen Juan Xing contacted and selected respondents to meet sampling quotas based on gender, age, geographic region, and socioeconomic status in China. Accordingly, the adult participants aged 18–60 years in our research were representative of the population in terms of the abovementioned demographic factors. All the datasets received were automatically uploaded to the Wen Juan Xing platform at the end of the survey. This study was approved by the Ethics Committee of Wengjiang District People's Hospital of Chengdu (reference number: EC-2020-002), and all participants provided written informed consent prior to completing the survey.
2.2. Measures
The respondents completed a battery of self-assessments collecting demographic information and information on the elements shown in Table 1, which were applied to obtain the 16 foci for the present network analysis. The total McDonald's ω was used as the reliability index of internal consistency (McNeish, 2018). For the scales used in our study, we used McDonald's ω to test the internal consistency. Generally, values greater than 0.90 are excellent, those in the range of 0.80–0.90 are good and those from 0.70 to 0.80 indicate acceptable reliability. Table 1 shows that according to the current data analysis, most of the McDonald's ω values generally had acceptable reliability. The lists of all items comprising each measure are shown in the supplementary materials.
2.3. Statistical analysis
A Gaussian graphical model (regularized partial correlation network model) was developed using the R qgraph package (Epskamp et al., 2018). We also computed the four indices of centrality using qgraph, and these indices used to evaluate the characteristics of the links between nodes (the factors we focused on) in the network. Four common node centrality indices were computed: strength, betweenness, closeness and expected influence (Epskamp et al., 2018). The strength of a given node was calculated as the sum of the absolute values of the weight (regularized partial correlations) linking the node with other nodes. Expected influence refers to the sum of the weighted edges or correlations for one node. The central node has the largest number of statistically significant connections with other nodes in the network. Strength and expected influence were considered the main indicators of centrality because they are the most supported as reliable and stable indicators of centrality (Epskamp et al., 2018). Specifically, strength has previously been used as an index most often (Opsahl and Skvoretz, 2010), while expected influence has been reported more recently (Opsahl and Skvoretz, 2010). Thus, we reported both the strength and expected influence in this research. Betweenness refers to the frequency of the most effective (shortest) path between a given node and other nodes in the network,f, how essential a given element is when linking to other elements. Closeness refers to the degree of connection between a node and other nodes in the network.
To determine whether some nodes in the network were significantly more central than other nodes, node centrality difference tests were calculated with the R package bootnet (Epskamp et al., 2018), which examines the difference in node strength. The reliability of the node strength values and node connections was tested through the correlation of the stability coefficient, which was also computed by bootnet (Epskamp et al., 2018). Values greater than 0.25 indicate moderate stability, and values greater than 0.5 indicate strong stability (Epskamp and Fried, 2018).
3. Results
A total of 539 participants from 76 cities in 27 provinces were included in the study. A total of 445 (82.6%) participants scored high on their willingness to vaccinate, 19 (3.5%) participants scored low on their willingness to vaccinate, and the rest (13.9%) were uncertain according to their scores. The higher the score, the more willing the respondent was to be vaccinated. The age of the respondents ranged from 18 to 60 (average age 31.47 ± 8.93 year). A total of 51% of the sample was male, and most (98.9%) of the participants had a high school degree or above.
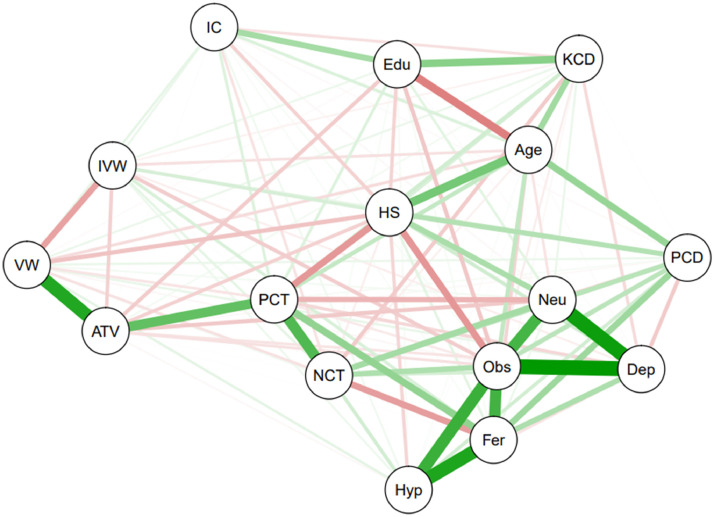
Fig. 1 shows the visual results of the network formed by applying a Gaussian graphical model or partial correlation model to vaccination willingness and its related factors. Vaccination willingness was related to many factors. However, when all the nodes in the network were connected, the network image was too complex to explain the results effectively. The solution was to introduce a penalization factor (Friedman et al., 2008).
Fig. 1.
Partial correlation network model of vaccination willingness and its associated factors. Abbreviations: HS, health status; VW, vaccination willingness; IVW, influence of other people's choices on vaccination willingness; ATV, attitude towards vaccines; PCD, perception of the risk of coronavirus disease; PCT, positive coping tendency; NCT, negative coping tendency; Dep, depression; Neu, neurasthenia; Fer, fear; Obs, obsession and anxiety; Hyp, hypochondria; KCD, knowledge level of coronavirus disease; IC, income; Edu, education.
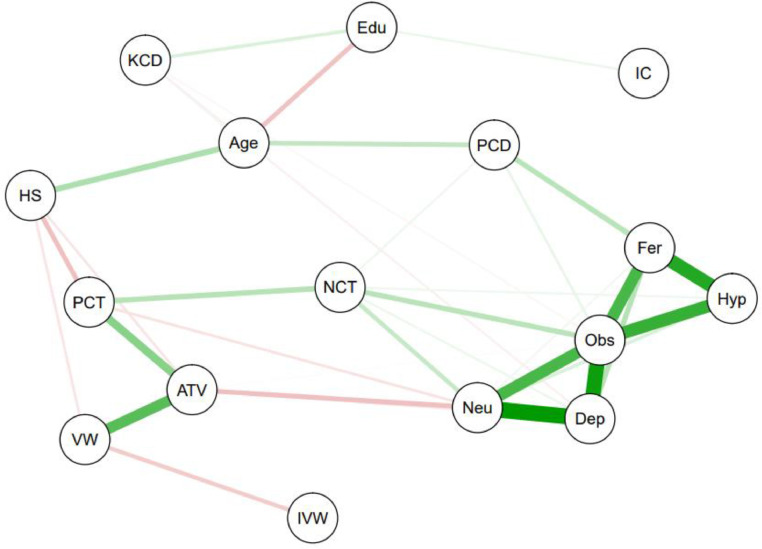
Based on the partial correlation network model, Fig. 2 shows the penalization factor and uses the Graphic Least Absolute Shrinkage and Selection Operator (GLASSO) (Friedman et al., 2008) to show the connections (regularized partial correlations) between nodes in the network (for all connections, p < 0.05). The magnitude of the strength of links among nodes is shown by thicker, shorter lines, with negative relationships in red and positive relationships in green. The numerical values of the edges are shown in Supplementary Table S1. Regarding the strength of the (correlations between nodes) node connections and nodes, the stability analyzes showed that the correlation stability coefficients were 0.55 and 0.6 respectively, indicating that the results were stable. The average correlations between centrality indices of networks sampled with persons dropped and those of the original sample are shown in Supplementary Fig. S2, which indicates that the centrality is reliable.
Fig. 2.
Graphic Least Absolute Shrinkage and Selection Operator (GLASSO) network model of vaccination willingness and its associated factors. Abbreviations: HS, health status; VW, vaccination willingness; IVW, influence of other people's choices on vaccination willingness; ATV, attitude towards vaccines; PCD, perception of the risk of coronavirus disease; PCT, positive coping tendency; NCT, negative coping tendency; Dep, depression; Neu, neurasthenia; Fer, fear; Obs, obsession and anxiety; Hyp, hypochondria; KCD, knowledge level of coronavirus disease; IC, income; Edu, education.
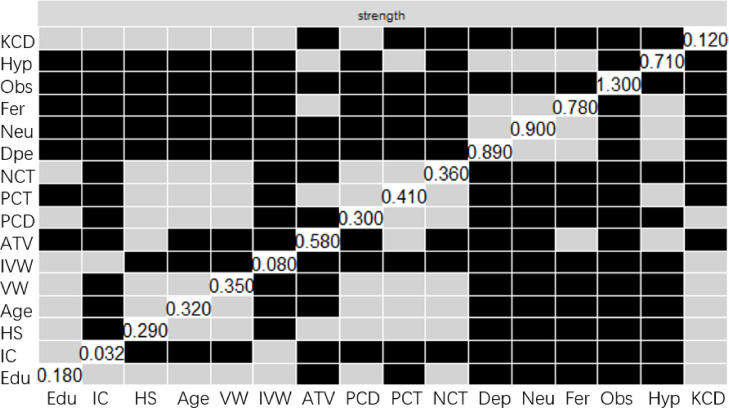
Table 2 exhibits the four centrality indices and Fig. 3 shows the bootstrapped difference test, which examines the significance of node strength. Of all the indices, the five factors in the psychological questionnaire on emergent public health events (PQEPHE) showed the strongest centrality (see quantitative data in Table 2), with the strengths of their links with other nodes being significantly higher than the strengths of all other elements (p < 0.05). Analysis of the PQEPHE revealed that the most central node was attitude toward vaccines (ATV) (strength = 0.57, closeness = 0.0027, betweenness = 30), the strength of which was significantly higher than those of the remaining factors in the network (p<0.05). For vaccination willingness, the main focus of our research, the centrality of strength was 0.34, the closeness was 0.0024 and the betweenness was 14. It should be noted that the betweenness of age was 34 (p < 0.05), which was the highest betweenness value of all 16 factors. In addition, the closeness of the positive coping tendency value was 0.0027 (p < 0.05), which was the highest closeness value except for the emotional state, as reflected by the PQEPHE. Income had the lowest centrality value, and its strength was 0.03, closeness was 0.0010 and betweenness was 0.
Table 2.
Centrality indices for elements in the network analysis. Large values indicate that a given element had greater importance in the network, as indicated by its connections with other elements in the network.
| Variable (and scale) | Strength | Closeness | Betweenness | Expected influence |
| Education | 0.17 | 0.0020 | 21 | −0.01 |
| Income | 0.03 | 0.0010 | 0 | 0.03 |
| Age | 0.31 | 0.0025 | 34 | 0.14 |
| Health status | 0.28 | 0.0024 | 20 | −0.05 |
| Vaccination willingness | 0.34 | 0.0024 | 14 | 0.12 |
| Influence of other people's choices on vaccination willingness | 0.07 | 0.0016 | 0 | −0.07 |
| Attitude towards vaccines | 0.57 | 0.0027 | 30 | 0.23 |
| Perception of the risk of coronavirus disease | 0.29 | 0.0025 | 17 | 0.29 |
| Knowledge level of coronavirus disease | 0.11 | 0.0014 | 0 | 0.04 |
| Depression (PQEPHE) | 0.88 | 0.0028 | 5 | 0.76 |
| Neurasthenia (PQEPHE) | 0.89 | 0.0028 | 17 | 0.64 |
| Fear (PQEPHE) | 0.78 | 0.0028 | 21 | 0.78 |
| Obsession and anxiety (PQEPHE) | 1.28 | 0.0029 | 30 | 1.24 |
| Hypochondriasis (PQEPHE) | 0.71 | 0.0027 | 0 | 0.71 |
| Positive coping tendency (SCSQ) | 0.40 | 0.0027 | 25 | 0.14 |
| Negative coping tendency (SCSQ) | 0.35 | 0.0025 | 4 | 0.35 |
Abbreviations: PQEPHE, Psychological questionnaire on emergent public health events; SCSQ, Simple Coping Style Questionnaire.
Fig. 3.
Strength bootstrapped difference tests (α = 0.05) on node strength of the elements in the network. Gray boxes indicate nodes that do not differ significantly from one-another and black boxes represent nodes that do differ significantly from one-another and white boxes in the centrality plot show the value of node strength. Abbreviations: HS, health status; VW, vaccination willingness; IVW, influence of other people's choices on vaccination willingness; ATV, attitude towards vaccines; PCD, perception of the risk of coronavirus disease; PCT, positive coping tendency; NCT, negative coping tendency; Dep, depression; Neu, neurasthenia; Fer, fear; Obs, obsession and anxiety; Hyp, hypochondria; KCD, knowledge level of coronavirus disease; IC, income; Edu, education.
In the model in which we introduced the penalization factor, there were only three factors related to vaccination willingness, among which health status (edge_weights = −0.04) and the influence of people around the individual (edge_weights = −0.07) were negatively correlated with vaccination willingness, and ATV (edge_weights = 0.23) was positively correlated with vaccination willingness. As shown in Fig. 2, ATV, which was directly related to vaccination willingness, was also directly affected by other elements, such as positive coping tendency (edge_weights = 0.17), health status (edge_weights = −0.04), neurasthenia (edge_weights = −0.09) and depression (edge_weights = −0.04). In addition, health status, which was directly negatively related to vaccination willingness, was directly related to age (edge_weights = 0.12), positive coping tendency (edge_weights = −0.09) and ATV(edge_weights = −0.04). The weights of all edges are shown in Supplementary Table S1 and all the above associations were significant (p < 0.05).
As expected, the connections among factors in this network were consistent with cognitive-behavioral conceptualizations. For example, participants who were more willing to be vaccinated had a more positive attitude towards vaccines. Participants with a positive attitude towards vaccines also had a more positive coping style in their daily life. At the same time, the psychological status of the public during the pandemic, such as neurasthenia, affected their attitude towards vaccines.
4. Discussion
Many psychological factors play a role in willingness to vaccinate against COVID-19, including diverse aspects of mental status, coping tendency, age, ATV and other elements included in the current network analysis. After applying the GLASSO method (Friedman et al., 2008), we could remove relatively weak connections in the network. By reducing the number of connections, the model was able to fit the network structure, which made the model easier to explain and more accurately predicted connections. Compared with Figs. 1, Fig. 2 is more concise and shows the important connections in the network more clearly, which makes the model easier to interpret. To our knowledge, the present research is the first comprehensive network analysis of vaccination willingness and its related factors during COVID-19 that has been performed to investigate how those various factors are interconnected.
Consistent with previous studies (Abedin et al., 2021; Schwarzinger et al., 2021; Wang et al., 2020), our GLASSO network analysis indicated that ATV had the greatest association with vaccination willingness. In addition to the five psychological states contained in the PQEPHE, the strength of this factor was the highest, which meant that ATV was the core factor in the network. ATV was also linked to health status, positive coping tendency and neurasthenia. This finding indicated that the general attitude of the public towards vaccines, such as the awareness of vaccine safety and effectiveness and the degree of trust in the public health system, had the greatest correlation with vaccination willingness. As our network analysis model showed, health status and neurasthenia were negatively correlated with ATV, and positive coping tendency and ATV were positively correlated. These factors reflect the inherent biological and psychological state of individuals, which renders the acceptance of a particular intervention difficult. Therefore, to influence and promote the public's willingness to vaccinate by influencing ATV, more media publicity and information transparency can be used to increase public knowledge about the vaccine and trust in the public health system.
The influence of people around the individuals was negatively correlated with vaccination willingness. As far as we know, there are no studies that have directly focused on whether this factor affects willingness to vaccinate against COVID-19 (Wake, 2021). However, an article published by Chan et al. in 2015 showed that community-dwelling elderly individuals are dependent on the influence of vaccinated nonelderly community members (Chan et al., 2015). Therefore, our research, to some extent, addresses for the current gap in related fields. Our results showed that the more willing a person is to be vaccinated, the less likely he or she is to be affected by the vaccination of the people around him or her. Specifically, as long as the individual's willingness to be vaccinated is strong enough, even if the people around him or her are not vaccinated, he or she will be vaccinated. However, due to the social attributes of humans, we are easily affected by the surrounding environment. Although Fig. 2 shows that the influence of the proportion of people around an individual who are vaccinated is not connected with any other factors in the model, according to Fig. 1, which does not introduce the penalization factor, this factor would affect the attitude of participants towards the vaccine, and the attitude of participants towards the vaccine would affect the willingness of participants to vaccinate. Therefore, it is possible that if the sample size were increased and the test effectiveness improved, this factor could withstand the test of the penalization factor and continue to be related to the ATV. This is the value of network analysis, which directly shows the relationship between interrelated factors to facilitate better understanding of the relationship between them.
As shown in Fig. 2, another factor that had a negative impact on vaccination willingness was the health status of the participants; specifically, the worse the health status of the participants was, the lower their vaccination willingness. Our results are inconsistent with those of similar studies before COVID-19 (Chan et al., 2015). Previous studies have shown that elderly people with poor health or chronic diseases are more likely to be vaccinated (Chan et al., 2015). The same results were obtained before COVID-19 vaccination began. For example, information on vaccination willingness was collected by Seale et al. in Australia in March 2020 (Seale et al., 2021) and Yoda et al. in Japan in September 2020 (Yoda and Katsuyama, 2021). However, with the development of COVID-19 vaccination, the information collected recently showed no significant relationship between health status and vaccination willingness (Robinson et al., 2021). This is a very interesting phenomenon, which may have occurred because COVID-19 is a topic of global concern, so the public receives a massive amount of information about the epidemic every day. Prior to the start of the vaccination program, the public had not yet received any information about the side effects of the vaccine. At that point, more information was received about the vaccine being developed rapidly or about the mortality rate of people who were weak and sick being higher after infection. With the development of vaccination programs, a growing awareness of vaccine side effects by the public has gradually occurred; patients with immune system diseases or acute diseases have been advised to be cautious or postpone vaccination (Maramattom et al., 2021; Mason et al., 2021; Thakkar et al., 2021); and some rumours about vaccine side effects have even spread among the public (Tasnim et al., 2020). We believe that the transmission of different information derived from public opinion in different periods leads to the fluctuating relationship between vaccination willingness and health status. Therefore, especially during major public health events, public health departments can create a favourable public opinion environment for vaccination by properly guiding public opinion. In addition, the timely refutation of rumours is also very important in the present Internet society characterized by rapid information dissemination.
The value of betweenness of age was the highest among all factors, although there were few nodes directly related to age. Betweenness refers to the number of times a node acts as the shortest connection between the other two nodes. The higher the number of times a node acts as the shortest connection between two other nodes (‘betweenness’), the greater its betweenness centrality. Our results indicated that the contact of many nodes in the network depended on age, so age controlled and restricted other nodes. For example, the health status of individuals will gradually deteriorate with age, which is also shown in Fig 2. Several previous studies have shown that age has an impact on vaccination willingness (Lin et al., 2020; Wake, 2021). In our network analysis (Fig. 2), although age was not directly related to vaccination willingness, the high betweenness of age showed that it still affected vaccination willingness through interaction with other factors.
Notably, the five psychological state subfactors of the PQEPHE showed strong centrality in the model of this study, which indicated that they played an important role in the network. This could largely be due to the fact that the five mental states (neurasthenia, depression, obsession, hypochondriasis and fear) included in the scale have strong connections, and that the mental states interact with each other (Boschloo et al., 2015). If a person's neurasthenia score is high, other psychological problems may also be prominent. More importantly, the high centrality of various emotional states showed that emotional state was the core node in the network analysis. The higher the centrality, the greater the impact on other nodes in the network, so emotional states will not only affect vaccination willingness but also affect other factors related to vaccination willingness, such as ATV and health state. Numerous previous studies have discussed the relationship between emotional states and vaccination willingness (Detoc et al., 2020; Shanafelt et al., 2020). However, no study has shown the relationship between emotional state and other factors. Network analysis can clearly show the interaction between nodes, which facilitates a better understanding of the relationship between things to enable the development of appropriate countermeasures.
Regarding limitations, network analysis, which is also a statistical modeling method, is not sufficient to determine the causal relationships of the links between nodes. However, from the perspective of cognition and behavior, it is plausible that ATV plays a causal role in promoting vaccination willingness, which has been confirmed by many studies (Yoda and Katsuyama, 2021). The second limitation of this research is that there are other latent essential elements that have not been evaluated. To our knowledge, this network analysis was the first to focus on vaccination willingness. Other possibly relevant elements could be studied in future network analyzes. For example, working in the healthcare field and receiving any vaccine in the past could be considered in future studies to determine how these experiences are related to the factors in the network. Recent studies have confirmed a significant correlation between these experiences and willingness to vaccinate (Yoda and Katsuyama, 2021). Third, although we used stratified random sampling to sample individuals from 76 cities in 27 provinces of China to obtain a population-representative sample, the sample size was only 539 individuals, which is relatively small for a country with a population of 1.4 billion. Future research should continue to use a stratified random sampling method and increase the sample size as much as possible to increase the statistical effectiveness. Finally, because our study was a cross-sectional study, it is unclear whether public vaccination willingness and related factors will change with time. Accordingly, further studies with a population-representative sample are needed to examine whether the network changes over time. Understanding whether and to what extent vaccination willingness and factors related to COVID-19 are dynamic is important for the development and delivery of interventions that are appropriately responsive to the needs of these services.
5. Conclusion
In summary, our results showed that in the early stage of the COVID-19 vaccination programme, most Chinese respondents showed a positive attitude towards vaccination, with 82.6% willing to vaccinate. Network analysis indicated that ATV, the influence of people around the individual and health status were directly related to vaccination willingness and were also directly related to age, coping style, neurasthenia and other factors. ATV and emotional states were the most critical factors in the network affecting vaccination willingness. Therefore, we should pay attention to the impact of the dissemination of Internet information on vaccination willingness and public emotional states during a pandemic. We need to guide the dissemination of such information and properly address the public emotional states during a pandemic to make vaccination progress smoother. At the same time, we also need to pay attention to the impact of age on vaccination willingness. With the development of vaccination programmes, future research needs to include more factors that may affect public vaccination willingness, use population-representative samples and increase the sample size to continue to pay attention to vaccination willingness and its related factors.
CRediT authorship contribution statement
Zuxing Wang: Data curation, Formal analysis, Conceptualization, Visualization, Funding acquisition, Writing – original draft, Project administration, Supervision. Jun Xiao: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Fugui Jiang: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Jieying Li: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Yang Yi: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Wenjiao Min: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Arui Tan: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Run Liang: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Shuyun Liu: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Lili Chen: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Peijia Wang: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Xiaoqiang Xiao: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Yuanyuan Luo: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Xiaohong Qin: Conceptualization, Visualization, Writing – original draft, Project administration, Supervision. Mengsha Qi: Data curation, Formal analysis, Funding acquisition, Writing – original draft, Project administration, Supervision.
Declaration of Competing Interest
The authors have no conflict of interest to declare.
Acknowledgments
Statement
This article is original, is not under simultaneous consideration by another publication, nor has it been previously published elsewhere and its content has not been anticipated by any previous publication.
Funding
This study was supported by research grants from the Innovation and Entrepreneurship Project of Sichuan Provincial Science and Technology Department (Grand code 2020JDRC0135), National Key Research and Development Plan (grant number 2017YFC0113907), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2019PT310020) and Establishment, Evaluation System Construction and Promotion of Group Model of Psychosomatic Nursing Happiness Perception Training in General Hospital (2018ZX04).
Acknowledgment
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.10.088.
Appendix. Supplementary materials
References
- Abedin M., Islam M.A., Rahman F.N., Reza H.M., Hossain M.Z., Hossain M.A., Arefin A., Hossain A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges do Nascimento I.J., O'Mathúna D.P., von Groote T.C., Abdulazeem H.M., Weerasekara I., Marusic A., Puljak L., Civile V.T., Zakarija-Grkovic I., Pericic T.P., Atallah A.N., Filoso S., Bragazzi N.L., Marcolino M.S., International Network of Coronavirus Disease 2019 (InterNetCOVID-19) Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect. Dis. 2021;21:525. doi: 10.1186/s12879-021-06214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. J. Clin. Psychol. 2008;64:1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Boschloo L., van Borkulo C.D., Rhemtulla M., Keyes K.M., Borsboom D., Schoevers R.A. The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One. 2015;10 doi: 10.1371/journal.pone.0137621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan D.P., Wong N.S., Wong E.L., Cheung A.W., Lee S.S. Household characteristics and influenza vaccination uptake in the community-dwelling elderly: a cross-sectional study. Prev. Med. Rep. 2015;2:803–808. doi: 10.1016/j.pmedr.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Fried E.I. A tutorial on regularized partial correlation networks. Psychol. Methods. 2018;23:617–634. doi: 10.1037/met0000167. [DOI] [PubMed] [Google Scholar]
- Finney Rutten L.J., Zhu X., Leppin A.L., Ridgeway J.L., Swift M.D., Griffin J.M., St Sauver J.L., Virk A., Jacobson R.M. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin. Proc. 2021;96:699–707. doi: 10.1016/j.mayocp.2020.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Hastie T., Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9:432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly H., Sokola B., Abboud H. Safety and efficacy of COVID-19 vaccines in multiple sclerosis patients. J. Neuroimmunol. 2021;356 doi: 10.1016/j.jneuroim.2021.577599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.H., Marks F., Clemens J.D. Looking beyond COVID-19 vaccine phase 3 trials. Nat. Med. 2021;27:205–211. doi: 10.1038/s41591-021-01230-y. [DOI] [PubMed] [Google Scholar]
- Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl.Trop. Dis. 2020;14 doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N., Saville M., Hatchett R., Halton J. Developing Covid-19 vaccines at pandemic speed. N. Engl. J. Med. 2020;382:1969–1973. doi: 10.1056/NEJMp2005630. [DOI] [PubMed] [Google Scholar]
- Maramattom B.V., Krishnan P., Paul R., Padmanabhan S., Soumya C.V., Syed A.A., Mangat H.S. Guillain-barré syndrome following ChAdOx1-S/nCoV-19 vaccine. Ann. Neurol. 2021 doi: 10.1002/ana.26143. [DOI] [PubMed] [Google Scholar]
- Mason A., Anver H., Lwin M., Holroyd C., Faust S.N., Edwards C.J. Lupus, vaccinations and COVID-19: what we know now. Lupus. 2021 doi: 10.1177/09612033211024355. 9612033211024355. [DOI] [PubMed] [Google Scholar]
- McNeish D. Thanks coefficient alpha, we'll take it from here. Psychol. Methods. 2018;23:412–433. doi: 10.1037/met0000144. [DOI] [PubMed] [Google Scholar]
- Palacios R., Patiño E.G., de Oliveira Piorelli R., Conde M., Batista A.P., Zeng G., Xin Q., Kallas E.G., Flores J., Ockenhouse C.F., Gast C. Double-blind, randomized, placebo-controlled phase III clinical trial to evaluate the efficacy and safety of treating healthcare professionals with the adsorbed COVID-19 (inactivated) vaccine manufactured by sinovac - PROFISCOV: a structured summary of a study protocol for a randomised controlled trial. Trials. 2020;21:853. doi: 10.1186/s13063-020-04775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y., Bergman Y.S., Ben-David B., Bodner E. No psychological vaccination: vaccine hesitancy is associated with negative psychiatric outcomes among Israelis who received COVID-19 vaccination. J. Affect. Disord. 2021;287:352–353. doi: 10.1016/j.jad.2021.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated. Vaccine. 2020;38:6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Jones A., Lesser I., Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39:2024–2034. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roozenbeek J., Schneider C.R., Dryhurst S., Kerr J., Freeman A., Recchia G., van der Bles A.M., van der Linden S. Susceptibility to misinformation about COVID-19 around the world. R. Soc. Open Sci. 2020;7 doi: 10.1098/rsos.201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. the lancet. Public Health. 2021;6:e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale H., Heywood A.E., Leask J., Sheel M., Durrheim D.N., Bolsewicz K., Kaur R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect. Dis. 2021;21:120. doi: 10.1186/s12879-021-05833-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Singh A.K., Misra A. Editorial: herd mentality, herds of migrants/people, and COVID-19 in India. Diabetes metab. syndr. 2020;14:497. doi: 10.1016/j.dsx.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opsahl F.A.T., Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc. Netw. 2010;32:245–251. doi: 10.1016/j.socnet.2010.03.006. [DOI] [Google Scholar]
- Tasnim S., Hossain M.M., Mazumder H. Impact of Rumors and Misinformation on COVID-19 in Social Media. Journal of preventive medicine and public health = Yebang Ŭihakhoe chi. 2020;53:171–174. doi: 10.3961/jpmph.20.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Rachor G.S., Asmundson G. Worry, avoidance, and coping during the COVID-19 pandemic: a comprehensive network analysis. J. Anxiety Disord. 2020;76 doi: 10.1016/j.janxdis.2020.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakkar A., Gonzalez-Lugo J.D., Goradia N., Gali R., Shapiro L.C., Pradhan K., Rahman S., Kim S.Y., Ko B., Sica R.A., Kornblum N., Bachier-Rodriguez L., McCort M., Goel S., Perez-Soler R., Packer S., Sparano J., Gartrell B., Makower D., Goldstein Y.D., Wolgast L., Verma A., Halmos B. Seroconversion rates following COVID-19 vaccination among patients with cancer. Cancer Cell. 2021 doi: 10.1016/j.ccell.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wake A.D. The willingness to receive COVID-19 vaccine and its associated factors: "vaccination refusal could prolong the war of this pandemic" - a systematic review. Risk Manag. Healthc. Policy. 2021;14:2609–2623. doi: 10.2147/RMHP.S311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., Fang H. Acceptance of COVID-19 Vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8 doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Lu X., Lai X., Lyu Y., Zhang H., Fenghuang Y., Jing R., Li L., Yu W., Fang H. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: a longitudinal study. Vaccines. 2021;9 doi: 10.3390/vaccines9030191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoda T., Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines. 2021;9 doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.