Abstract
The present dataset is concerned with an article entitled “Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: A cross-sectional study” [1]. This data article consists of a dataset regarding the mental health of Bangladeshi healthcare professionals (HCPs) during the ongoing COVID-19 pandemic. We collected the data from July 15, 2020, to September 20, 2020, using Google survey tools (Google Forms). A total of 355 complete responses have been obtained from the Bangladeshi HCPs aged between 20–60 years (male: 204, female: 151). We obtained informed consent from all participants for this study. We assessed the sociodemographic profile and four psychometric measures of HCPs working in Bangladesh during the COVID-19 pandemic. A structured questionnaire was used to collect the demographic information. We used the UCLA loneliness scale-8 (UCLA-8), the patient health questionnaire-9 (PHQ-9), the 7-item generalized anxiety disorder scale (GAD-7), and the Pittsburgh sleep quality index (PSQI) were applied to measure loneliness, depression, generalized anxiety, and sleep disturbance, respectively. This dataset presents the descriptive analysis of psychometric variables of participants. Also, the dataset might be used as a platform for future research on psychometric evaluation using the above scales. We included participants regardless of the sociodemographic backgrounds of HCPs. Therefore, the policymakers, government, and non-government organizations can use this data to develop different programs for promoting the mental health of HCPs and the general population in Bangladesh.
Keywords: Healthcare professionals, HCPs, Mental health, Loneliness, Depression, Anxiety, Sleep disturbance, COVID-19, Bangladesh
Specifications Table
| Subject | Public Health. |
| Specific subject area | Mental health, psychology, and COVID-19. |
| Type of data | Primary data, tables, and figure. |
| How data were acquired | Google survey tools (Google Forms). |
| Data format | Raw and analyzed. |
| Parameters for data collection | We obtained responses from Bangladeshi healthcare professionals aged between 20 to 60 years. The target group was social media users who agreed to participate in this study regardless of their background or sociodemographic factors. |
| Description of data collection | We used Google survey tools (Google Forms) to conduct this study from July 15, 2020, to September 20, 2020. We collected responses from healthcare professionals (HCPs) using a self-administered structured questionnaire that included informed consent, sociodemographic information, and four distinct mental health assessment scales (UCLA-8, PHQ-9, GAD-7, and PSQI). We sent the questionnaires to the respondents through social media platforms and personal emailing. Also, we arranged phone calls to settle any concerns raised by the respondents. Moreover, we supplied the detailed questionnaire and responses as supplementary files 1 and 2. |
| Data source location | Researchers from the University of Asia Pacific, Dhaka, have collected data from across Bangladesh. |
| Data accessibility | Data is within this article. |
| Related research article | Repon, M., Pakhe, S. A., Quaiyum, S., Das, R., Daria, S., & Islam, M. R. (2021). Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: A cross-sectional study. Science progress, 104(2), 368504211026409. 10.1177/00368504211026409 https://journals.sagepub.com/doi/10.1177/00368504211026409 |
Value of the Data
-
•
Researchers can use this dataset to compare the mental health of other populations during this ongoing health emergency.
-
•
The dataset allowed for quick data collection during global health emergencies.
-
•
The present dataset can initiate studies to measure the severity of mental health problems among HCPs in Bangladesh to understand the gravity of the issue.
-
•
The dataset is useful for policymakers and government or non-government organizations to take proper measures for promoting mental health.
1. Data Description
The World Health Organization (WHO) endorsed the COVID-19 as a global pandemic on March 11, 2020 [1], [2]. Since then, the world fighting this pandemic, and nobody knows when it will stop. The Bangladesh government declared a country-wide lockdown on March 26, 2020, to curb the spreading of this virus among its citizens [3]. The COVID-19 responses have impacted the personal, social, and work-life of many people across the globe [4], [5], [6], [7]. Also, the pandemic has more or less impact in every sector in a country [8], [9], [10]. Therefore, the COVID-19 pandemic tremendously affected the mental health of the general population of any country [11,12]. As frontline fighters, the impact of the COVID-19 pandemic on the mental health of HCPs was high due to this relatively unknown and lethal virus [13]. The ongoing pandemic has placed HCPs in a situation of intense psychological pressure and moral responsibilities [14].
According to the findings, the composition of physicians, pharmacists, nurses, and medical technologists were 30%, 23%, 26%, and 22%, respectively. Among all HCPs, males and females were 57 and 43%. Only 36% HCPs were above 40 years of age, and the majority of the respondents were from a lower economic class (72%) residing in the urban area (76%).
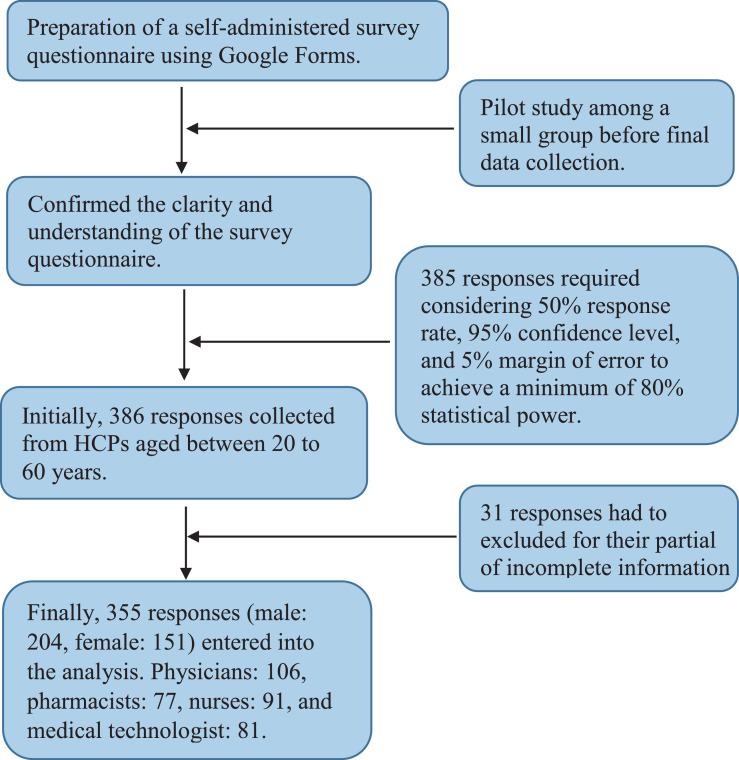
The dataset provides (i) evaluation of loneliness by using the UCLA loneliness scale-8 (UCLA-8) in Table 1, (ii) evaluation of depression by the patient health questionnaire-9 (PHQ-9) in Table 2, (iii) evaluation of anxiety applying the 7-item generalized anxiety disorder scale (GAD-7) in Table 3, (iv) evaluation of sleep disturbances by the Pittsburgh sleep quality index (PSQI) in Table 4, (v) distribution of different psychometric parameters among the respondents in Table 5, (vi) the severity of different psychometric parameters among the respondents in Table 6. We presented a detailed data collection procedure using a flowchart (Fig. 1). Also, we provided the questionnaire and raw data as supplementary files (supplementary file-1 and file-2, respectively).
Table 1.
Distribution of responses based on the UCLA loneliness scale-8 (UCLA-8).
| Indicate how often each of the statements below is | ||
|---|---|---|
| descriptive of you. | Frequency (n) | Percentage (%) |
| 1. In the past 30 days, I lack companionship. | ||
| Never (1) | 42 | 11.83 |
| Rarely (2) | 47 | 13.24 |
| Sometimes (3) | 167 | 47.04 |
| Often (4) | 99 | 27.89 |
| 2. In the past 30 days, there is no one I can turn to. | ||
| Never (1) | 70 | 19.72 |
| Rarely (2) | 63 | 17.75 |
| Sometimes (3) | 155 | 43.66 |
| Often (4) | 67 | 18.87 |
| 3. In the past 30 days, I feel left out. | ||
| Never (1) | 68 | 19.15 |
| Rarely (2) | 69 | 19.44 |
| Sometimes (3) | 154 | 43.38 |
| Often (4) | 64 | 18.03 |
| 4. In the last 30 days, I feel isolated from others. | ||
| Never (1) | 55 | 15.49 |
| Rarely (2) | 65 | 18.32 |
| Sometimes (3) | 144 | 40.56 |
| Often (4) | 91 | 25.63 |
| 5. In the last 30 days, I am unhappy being so withdrawn. | ||
| Never (1) | 53 | 14.93 |
| Rarely (2) | 68 | 19.16 |
| Sometimes (3) | 172 | 48.45 |
| Often (4) | 62 | 17.46 |
| 6. In the last 30 days, people are around me but not with me. | ||
| Never (1) | 44 | 12.39 |
| Rarely (2) | 104 | 29.30 |
| Sometimes (3) | 115 | 32.39 |
| Often (4) | 92 | 25.92 |
| 7. In the last 30 days, I am an outgoing person. | ||
| Never (1) | 36 | 10.14 |
| Rarely (2) | 104 | 29.30 |
| Sometimes (3) | 137 | 38.59 |
| Often (4) | 78 | 21.97 |
| 8. In the last 30 days, I can find companionship when I want it. | ||
| Never (1) | 21 | 5.92 |
| Rarely (2) | 120 | 33.80 |
| Sometimes (3) | 143 | 40.28 |
| Often (4) | 71 | 20.00 |
Table 2.
Distribution of responses based on the patient health questionnaire-9 (PHQ-9).
| Indicate how often each of the statements below is descriptive of you. | Frequency (n) | Percentage (%) |
|---|---|---|
| 1. In the last two weeks, little interest or pleasure in doing things. | ||
| Not at all (0) | 105 | 29.58 |
| Several days (1) | 143 | 40.28 |
| More than half of the days (2) | 52 | 14.65 |
| Nearly every day (3) | 55 | 15.49 |
| 2. In the last two weeks, feeling down, depressed or hopeless. | ||
| Not at all (0) | 105 | 29.58 |
| Several days (1) | 143 | 40.28 |
| More than half of the days (2) | 52 | 14.65 |
| Nearly every day (3) | 55 | 15.49 |
| 3. In the last two weeks, trouble falling or staying asleep, sleeping too much. | ||
| Not at all (0) | 102 | 28.73 |
| Several days (1) | 164 | 46.20 |
| More than half of the days (2) | 50 | 14.08 |
| Nearly every day (3) | 39 | 10.99 |
| 4. In the last two weeks, feeling tired or having little energy. | ||
| Not at all (0) | 83 | 23.38 |
| Several days (1) | 166 | 46.76 |
| More than half of the days (2) | 60 | 16.90 |
| Nearly every day (3) | 46 | 12.96 |
| 5. In the last two weeks, poor appetite or overeating. | ||
| Not at all (0) | 103 | 29.01 |
| Several days (1) | 167 | 47.04 |
| More than half of the days (2) | 57 | 16.06 |
| Nearly every day (3) | 28 | 7.89 |
| 6. In the last two weeks, feeling bad about yourself-or that you are a failure or have let yourself or your family down. | ||
| Not at all (0) | 116 | 32.68 |
| Several days (1) | 151 | 42.54 |
| More than half of the days (2) | 50 | 14.08 |
| Nearly every day (3) | 38 | 10.70 |
| 7. In the last two weeks, trouble concentrating on things, such as reading the newspaper or watching television. | ||
| Not at all (0) | 102 | 28.73 |
| Several days (1) | 137 | 38.59 |
| More than half of the days (2) | 82 | 23.10 |
| Nearly every day (3) | 34 | 9.58 |
| 8. In the last two weeks, moving or speaking so slowly or the opposite-moving around a lot more than usual. | ||
| Not at all (0) | 146 | 41.13 |
| Several days (1) | 130 | 36.62 |
| More than half of the days (2) | 49 | 13.80 |
| Nearly every day (3) | 30 | 8.45 |
| 9. In the last two weeks, thoughts that you would be better off dead, or of hurting yourself in some way. | ||
| Not at all (0) | 175 | 49.30 |
| Several days (1) | 124 | 34.93 |
| More than half of the days (2) | 27 | 7.61 |
| Nearly every day (3) | 29 | 8.16 |
Table 3.
Distribution of responses based on the 7-item generalized anxiety disorder (GAD-7) scale.
| Indicate how often each of the statements below is descriptive of you. | Frequency (n) | Percentage (%) |
|---|---|---|
| 1. In the last two weeks, I am feeling nervous, anxious, or on edge. | ||
| Not at all (0) | 79 | 22.25 |
| Several days (1) | 146 | 41.13 |
| More than half of the days (2) | 60 | 16.90 |
| Nearly every day (3) | 70 | 19.72 |
| 2. In the last two weeks, I am not being able to stop or control worrying. | ||
| Not at all (0) | 79 | 22.25 |
| Several days (1) | 147 | 41.42 |
| More than half of the days (2) | 62 | 17.46 |
| Nearly every day (3) | 67 | 18.87 |
| 3. In the last two weeks, I am worrying too much about different things. | ||
| Not at all (0) | 70 | 19.72 |
| Several days (1) | 156 | 43.94 |
| More than half of the days (2) | 58 | 16.34 |
| Nearly every day (3) | 71 | 20.00 |
| 4. In the last two weeks, I felt trouble in relaxing. | ||
| Not at all (0) | 102 | 28.73 |
| Several days (1) | 150 | 42.25 |
| More than half of the days (2) | 46 | 12.96 |
| Nearly every day (3) | 57 | 16.06 |
| 5. In the last two weeks, I am being so restless that it's hard to sit still. | ||
| Not at all (0) | 108 | 30.42 |
| Several days (1) | 132 | 37.19 |
| More than half of the days (2) | 67 | 18.87 |
| Nearly every day (3) | 48 | 13.52 |
| 6. In the last two weeks, I becoming easily annoyed or irritable. | ||
| Not at all (0) | 73 | 20.56 |
| Several days (1) | 151 | 42.54 |
| More than half of the days (2) | 72 | 20.28 |
| Nearly every day (3) | 59 | 16.62 |
| 7. In the last two weeks, I am feeling afraid as if something awful might happen. | ||
| Not at all (0) | 78 | 21.97 |
| Several days (1) | 143 | 40.28 |
| More than half of the days (2) | 39 | 10.99 |
| Nearly every day (3) | 95 | 26.76 |
Table 4.
Distribution of responses based on the Pittsburgh sleep quality index (PSQI).
| Indicate how often each of the statements below is descriptive of you. | Frequency (n) | Percentage (%) |
|---|---|---|
| 1. During the past month, when have you usually gone to bed at night? | ||
| Before 10.00 PM | 4 | 1.13 |
| 10.01 PM to 12.00 AM | 116 | 32.68 |
| 12.01 AM to 2.00 AM | 199 | 56.05 |
| After 2.00 AM | 36 | 10.14 |
| 2. During the past month, how long (in minutes) has it usually take you to fall asleep each night? | ||
| Less than 15 minutes | 0 | 0.00 |
| 15-30 minutes | 315 | 88.73 |
| 31-60 minutes | 22 | 6.20 |
| More than 60 minutes | 18 | 5.07 |
| 3. During the past month, when have you usually gotten up in the morning? | ||
| Before 5.00 AM | 48 | 13.52 |
| 5.00 AM to 7.00 AM | 155 | 43.66 |
| 7.01 AM to 9.00 AM | 119 | 33.52 |
| After 9.00 AM | 33 | 9.30 |
| 4. During the past month, how many hours of actual sleep did you get at night? | ||
| Less than 4 hours | 6 | 1.69 |
| 4 to 6 hours | 290 | 81.69 |
| 7 to 8 hours | 58 | 16.34 |
| More than 8 hours | 1 | 0.28 |
| 5. During the past month, how many hours do you spend in bed? | ||
| Less than 5 hours | 55 | 15.49 |
| 5 to 7 hours | 245 | 69.02 |
| 8 to 10 hours | 53 | 14.93 |
| More than 10 hours | 2 | 0.56 |
| 6. During the past month, how many times, you cannot get to sleep within 30 minutes? | ||
| Not during last month (0) | 88 | 24.79 |
| Less than once a week (1) | 133 | 37.47 |
| Once or twice a week (2) | 96 | 27.04 |
| Three or more in week (3) | 38 | 10.70 |
| 7. During the past month, how many times, you wake up in the middle of the night or early morning? | ||
| Not during last month (0) | 73 | 20.57 |
| Less than once a week (1) | 143 | 40.28 |
| Once or twice a week (2) | 107 | 30.14 |
| Three or more in week (3) | 32 | 9.01 |
| 8. During the past month, how many times, you have to get up to use the bathroom? | ||
| Not during last month (0) | 104 | 29.30 |
| Less than once a week (1) | 121 | 34.08 |
| Once or twice a week (2) | 87 | 24.51 |
| Three or more in week (3) | 43 | 12.11 |
| 9. During the past month, how many times, you cannot breathe comfortably? | ||
| Not during last month (0) | 154 | 43.38 |
| Less than once a week (1) | 106 | 29.86 |
| Once or twice a week (2) | 77 | 21.69 |
| Three or more in week (3) | 18 | 5.07 |
| 10. During the past month, how many times, you cough or snore loudly? | ||
| Not during last month (0) | 122 | 34.37 |
| Less than once a week (1) | 132 | 37.18 |
| Once or twice a week (2) | 81 | 22.82 |
| Three or more in week (3) | 20 | 5.63 |
| 11. During the past month, how many times, you feel too cold? | ||
| Not during last month (0) | 155 | 43.66 |
| Less than once a week (1) | 115 | 32.39 |
| Once or twice a week (2) | 75 | 21.13 |
| Three or more in week (3) | 10 | 2.82 |
| 12. During the past month, how many times, you feel too hot? | ||
| Not during last month (0) | 111 | 31.27 |
| Less than once a week (1) | 87 | 24.50 |
| Once or twice a week (2) | 111 | 31.27 |
| Three or more in week (3) | 46 | 12.96 |
| 13. During the past month, how many times, you had bad dreams? | ||
| Not during last month (0) | 95 | 26.76 |
| Less than once a week (1) | 140 | 39.44 |
| Once or twice a week (2) | 96 | 27.04 |
| Three or more in week (3) | 24 | 6.76 |
| 14. During the past month, how many times, you have pain during sleep? | ||
| Not during last month (0) | 132 | 37.18 |
| Less than once a week (1) | 105 | 29.58 |
| Once or twice a week (2) | 91 | 25.63 |
| Three or more in week (3) | 27 | 7.61 |
| 15. During the past month, how many times, you have trouble in sleeping because of any other reasons? | ||
| Not during last month (0) | 108 | 30.42 |
| Less than once a week (1) | 124 | 34.93 |
| Once or twice a week (2) | 106 | 29.86 |
| Three or more in week (3) | 17 | 4.79 |
| 16. During the past month, how often have you taken medicine to help you sleep? | ||
| Not during last month (0) | 189 | 53.24 |
| Less than once a week (1) | 88 | 24.79 |
| Once or twice a week (2) | 64 | 18.03 |
| Three or more in week (3) | 14 | 3.94 |
| 17. During the past month, how many times you did not sleep due to any program or other important case? | ||
| Not during last month (0) | 107 | 30.14 |
| Less than once a week (1) | 124 | 34.93 |
| Once or twice a week (2) | 106 | 29.86 |
| Three or more in week (3) | 18 | 5.07 |
| 18 .During the past month, how much of a problem has it been for you to keep up enough enthusiasm to get things done? | ||
| Not during last month (0) | 113 | 31.83 |
| Less than once a week (1) | 140 | 39.44 |
| Once or twice a week (2) | 76 | 21.41 |
| Three or more in week (3) | 26 | 7.32 |
| 19. During the past month, how would you rate your sleep quality overall? | ||
| Very good (0) | 53 | 14.93 |
| Fairly good (1) | 194 | 54.65 |
| Fairly bad (2) | 90 | 25.35 |
| Very bad (3) | 18 | 5.07 |
Table 5.
Different psychometric parameters among the respondents.
| Psychometric parameters (total responses, N = 355) | Frequency (n) | Percentage (%) |
|---|---|---|
| Loneliness | ||
| Yes | 315 | 88.73 |
| No | 40 | 11.27 |
| Depression | ||
| Yes | 158 | 44.51 |
| No | 197 | 55.49 |
| Generalized anxiety | ||
| Yes | 276 | 77.75 |
| No | 79 | 22.25 |
| Sleep disturbance | ||
| Yes | 308 | 86.76 |
| No | 47 | 13.24 |
Table 6.
Severity of different psychometric parameters among the respondents.
| Psychometric parameters (total responses, N=355) | Frequency (n) | Percentage (%) |
|---|---|---|
| Loneliness | 315 | 88.73 |
| Mild | 115 | 36.50 |
| Moderate | 160 | 50.79 |
| Severe | 40 | 12.71 |
| Depression | 158 | 44.50 |
| Mild | 103 | 65.19 |
| Moderate | 45 | 28.48 |
| Severe | 10 | 6.33 |
| Generalized anxiety | 276 | 77.75 |
| Mild | 118 | 42.75 |
| Moderate | 106 | 38.41 |
| Severe | 52 | 18.84 |
| Sleep disturbance | 308 | 86.76 |
| Mild | 189 | 61.36 |
| Moderate | 104 | 33.77 |
| Severe | 15 | 4.87 |
Fig. 1.
Flowchart of collecting responses from the participants.
2. Experimental Design, Materials, and Methods
We conducted a nationwide online survey to investigate the effects of the COVID-19 pandemic on mental health among Bangladeshi HCPs. We collected responses between July 15, 2020, and September 20, 2020, using Google Forms. Respondents got the questionnaire link via different social media and personal emailing. However, we conducted a pilot study for clarity and understanding of the procedure. Also, we communicated with the respondents through phone calls or video conferencing to solve any confusion regarding the questionnaire during data collection. We designed the Google Forms in a way that we can avoid multiple responses from a single respondent. Also, we tracked the IP addresses of the individual respondents to ensure data sanity. We divided the questionnaire into two major sections: (1) questionnaire about sociodemographic, (2) questionnaire about psychometric measures. We used a structured questionnaire to collect demographic information, and we applied four internationally validated psychometric scales to assess mental health. We used UCLA-8, PHQ-9, GAD-7, and PSQI to assess loneliness, depression, generalized anxiety disorder, and sleep problems, respectively [15], [16], [17], [18]. We used every scale entirely, and we did not change anything on those scales. We measured loneliness by eight questions on how frequently they felt the following statements in the last 30 days. Respondents rated each question from 1 to 4 based on the answer: 1 (never), 2 (rarely), 3 (sometimes), and 4 (always) (often). Then there were nine questions concerning how frequently the respondents had been concerned by any of the following difficulties in the previous 30 days to evaluate depression level. Participants rated all the questions related to depression from 0 to 3 based on the response: 0 (not at all), 1 (several days), 2 (more than half of the days), and 3 (nearly every day). Psychometric measures included seven questions indicating how frequently the respondents were affected by the following issues in the last 30 days to assess respondents' anxiety levels. The responses range from 0 to 3 scale based on the answer: 0 (not at all), 1 (several days), 2 (more than half of the days), and 3 (nearly every day). Finally, we assessed the sleep disturbance by asking nineteen questions. The responses of these nineteen questions were then grouped into seven areas to measure the overall sleep quality. We performed data analyzes using Microsoft excel 2016 and presented them as frequency and percentage.
Funding
The author(s) did not receive any financial support for this work.
Ethics Statement
We obtained approval of this study protocol from the ethical review committee of the department of psychiatry, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh (2020/3609). Also, we obtained informed consent from all participants for their participation in this study and publication of anonymous data in the journal article.
CRediT authorship contribution statement
Md. Rabiul Islam: Data curation, Conceptualization, Formal analysis, Writing – original draft, Supervision, Writing – review & editing. Sumaiya Quaiyum: Data curation, Conceptualization, Formal analysis, Writing – original draft. Sajuti Akter Pakhe: Data curation, Conceptualization, Formal analysis, Writing – original draft. Md Azim Uddin Repon: Data curation, Conceptualization, Formal analysis, Writing – original draft. Mohiuddin Ahmed Bhuiyan: Supervision, Writing – review & editing, Data curation.
Declaration of Competing Interest
The author(s) do not have any conflict of interest to declare.
Acknowledgments
We are thankful to the respondents for their participation in this study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.dib.2021.107506.
Appendix. Supplementary materials
The survey questionnaire and the responses to the questions in English have been supplied as supplementary file 1 and 2.
References
- 1.Repon M., Pakhe S.A., Quaiyum S., Das R., Daria S., Islam M.R. Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: A cross-sectional study. Sci. Prog. 2021;104(2) doi: 10.1177/00368504211026409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. 2020. WHO Director-General's opening remarks at the media briefing on COVID-19-11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020. Accessed June 26, 2021.
- 3.Anadolu Agency. Bangladesh imposes total lockdown over COVID-19. 2020. https://www.aa.com.tr/en/asia-pacific/bangladesh-imposes-total-lockdown-over-covid-19/1778272. Accessed June 26, 2021.
- 4.Islam M.R., Qusar M., Islam M.S. Mental health of children amid COVID-19 pandemic in Bangladesh: an exploratory observation. Asia Pac. J. Public Health. 2021;33(4):469–470. doi: 10.1177/10105395211004371. [DOI] [PubMed] [Google Scholar]
- 5.Islam M.R., Hossain M.J. Increments of gender-based violence amid COVID-19 in Bangladesh: a threat to global public health and women's health. Int. J. Health Plan. Manag. 2021 doi: 10.1002/hpm.3284. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islam M.R., Hossain M.J. Social stigma and suicide in Bangla7desh: the COVID-19 has worsened the situation. Chronic stress. 2021:5. doi: 10.1177/24705470211035602. (Thousand Oaks, Calif.) 24705470211035602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahman F.I., Islam M.R. Sexual violence against woman at quarantine center during coronavirus disease 2019 in Bangladesh: risk factors and recommendations. Women's Health. 2021;17 doi: 10.1177/17455065211043851. (London, England) 17455065211043851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daria S., Islam M.R. The second wave of COVID-19 pandemic in Bangladesh: an urgent call to save lives. Asia Pac. J. Public Health. 2021 doi: 10.1177/10105395211021686. 10105395211021686. [DOI] [PubMed] [Google Scholar]
- 9.Daria S., Islam M.R. The use of cow dung and urine to cure COVID-19 in India: a public health concern. Int. J. Health Plan. Manag. 2021 doi: 10.1002/hpm.3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daria S., Asaduzzaman M., Shahriar M., Islam M.R. The massive attack of COVID-19 in India is a big concern for Bangladesh: the key focus should be given on the interconnection between the countries. Int. J. Health Plan. Manag. 2021 doi: 10.1002/hpm.3245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das R., Hasan M.R., Daria S., Islam M.R. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open. 2021;11(4) doi: 10.1136/bmjopen-2020-045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Islam M.R., Daria S., Das R., Hasan M.R. A nationwide dataset on the mental health of the Bangladeshi population due to the COVID-19 pandemic. Data Brief. 2021;38 doi: 10.1016/j.dib.2021.107347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.BBC. 2021. What we know and don't know about Covid-19. https://www.bbc.com/future/article/20210224-the-knowns-and-unknowns-of-covid-19. Accessed June 26, 2021.
- 14.Sarma R., Vig S., Rathore P., Pushpam D., Mishra S., Gupta N., Garg R., Kumar V., Bharati S.J., Bhatnagar S. Concerns of health care professionals managing non-COVID patients during the COVID-19 pandemic: a descriptive cross- sectional study. Indian J. Palliat. Care. 2020;26(Suppl 1):S21–S26. doi: 10.4103/IJPC.IJPC_155_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buysse D.J., Reynolds C.F., 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 16.Ganguly S., Samanta M., Roy P., Chatterjee S., Kaplan D.W., Basu B. Patient health questionnaire-9 as an effective tool for screening of depression among Indian adolescents. J. Adolesc. Health. 2013;52(5):546–551. doi: 10.1016/j.jadohealth.2012.09.012. official publication of the Society for Adolescent Medicine. [DOI] [PubMed] [Google Scholar]
- 17.Hays R.D., DiMatteo M.R. A short-form measure of loneliness. J. Personal. Assess. 1987;51(1):69–81. doi: 10.1207/s15327752jpa5101_6. [DOI] [PubMed] [Google Scholar]
- 18.Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The survey questionnaire and the responses to the questions in English have been supplied as supplementary file 1 and 2.