Abstract
Objective:
Evidence suggests that social anxiety (SA) is a risk factor for problematic alcohol and cannabis use, particularly during states of social stress. Unfortunately, laboratory studies to date have overlooked decision-making mechanisms (e.g., use willingness) and contextual features of commonly used social stress tasks that may clarify what is driving these links. The current study begins to address this gap by testing the effects of SA and laboratory-induced peer rejection on acute alcohol and cannabis use willingness within a simulated party setting.
Method:
80 emerging adults (18–25 years; 70% women) endorsing lifetime alcohol and cannabis use were randomly assigned to experience rejection or neutral social cues. They rated their willingness to use alcohol and cannabis before and after cue exposure within the simulated party. A hierarchical regression tested the main and interaction effects of SA symptoms and experimental condition (Rejection vs. Neutral) on alcohol and cannabis use willingness, controlling for past-year use frequency and willingness to accept any offers (e.g., food, non-alcoholic drinks).
Results:
There were statistically significant main (but not interaction) effects of SA and experimental condition on cannabis use willingness. Higher SA and Rejection exposure were each associated with greater cannabis use willingness. There were no main nor interaction effects on alcohol willingness.
Conclusions:
Results suggest that elevated SA increases cannabis use willingness across social contexts, regardless of Rejection exposure, while Rejection exposure increases use willingness similarly across levels of SA. Together, findings reinforce the need to consider social contextual factors and poly-substance use in laboratory settings.
Keywords: Social anxiety, social stress, rejection, cannabis, willingness
Introduction
Alcohol and cannabis are the two most widely used substances in the United States with initial rates of use and use-related disorders peaking in emerging adulthood (Franco et al., 2019; Grant et al., 2015; Hasin et al., 2016; Schulenberg et al., 2019). Emerging adults (18–25 years) in college are at particularly high risk for substance use, in part, because college campuses provide more opportunities to use substances in higher risk contexts (e.g., at parties with people they do not know well) and regularly engage with substance using peers (Allen et al., 2017; Arnett, 2005; Lewis et al., 2019). Socially anxious individuals who are hypersensitive to social cues and the fear of potential rejection may be at an even greater risk for developing use-related problems during this time (Abrams et al., 2001; Buckner et al., 2012; Conway et al., 2016).
Epidemiologically, elevated social anxiety (SA) frequently co-occurs with, and temporally precedes, both alcohol and cannabis use disorder (Buckner et al., 2012; Conway et al., 2016). Tension reduction and self-medication models suggest that individuals with elevated SA use alcohol and cannabis as a means of reducing their SA symptoms which increases their risk for use-related problems (Buckner, Heimberg, et al., 2013; Carrigan & Randall, 2003). Evidence of the coping pathway includes individuals with elevated SA reporting greater retrospective coping motives and real-time cravings following laboratory-induced stressors (Buckner, Ecker, et al., 2013; Buckner, Heimberg, et al., 2011; Buckner, Silgado, et al., 2011; Buckner & Heimberg, 2010). There is also evidence that these indicators may not fully capture the SA experience and early risk processes (Cloutier et al., 2016; Lemyre et al., 2019). For example, the tendency to avoid social situations and conform to others behaviors may lead to decreases and increases in substance use and related problems. Further, individuals who have not yet developed a substance use disorder may not experience the physiological urge of craving nor report intentional, coping motives and still be at increased risk. Capturing subclinical mechanisms of the SA-substance use link may offer key insight into effectively intervening before serious comorbidities have formed.
Behavioral willingness refers to a broader state of openness to use a substance (Gerrard et al., 2008). Like craving, use willingness can be elicited in the lab, predicts substance use behaviors, and is influenced by prior use. Whereas variation in craving is often only observed in heavier users, use willingness predicts real-time and long-term use behaviors across age and use levels (Anderson et al., 2013; Gibbons, Gerrard, Lune, et al., 2004; Ladd et al., 2016; Lewis et al., 2019). By capturing the overall tendency to use substances in response to internal (craving/ coping) and external (mimicking/conformity) cues, use willingness may be able to more meaningfully mark both existing and emerging substance use risks.
Because individuals with elevated SA are hypersensitive to social contexts and the stressors that occur within them (e.g., rejection), the extent to which SA elevates substance use risk also may be sensitive to the assessment environment (Battista et al., 2010; Buckner, Heimberg, et al., 2013; Cloutier et al., 2020; Lemyre et al., 2019). Tasks lacking explicit social or substance use cues like mock tests, impromptu job talks, or online ball-tossing games may not elicit substance use-related thoughts or behaviors as they would emerge in real-world contexts (Deros et al., 2018; Dimoff & Sayette, 2017). More generalizable tasks such as unstructured conversations may be challenging to standardize and implement as they require training confederates (Beidel et al., 2000). Comparing social stressors to non-social conditions (e.g., reading a magazine), confounds social stress with social contexts (Buckner et al., 2016).
Examining use decision-making and affect during rejection can further our understanding of the SA-substance use link. Rejection is a common experience that most people dislike, avoid, and respond to with approach motivations and affiliative behaviors (Hudd & Moscovitch, 2020; Mallott et al., 2009). Though broadly adaptive, the common approach/affiliative response to rejection also can increase willingness to engage in risky behaviors (Tamir & Hughes, 2018). As fear and avoidance of rejection are core features of SA, individuals with greater SA show hyper-vigilance to social threat (APA, 2013). Once rejected, they report more cognitive and affective disruption as well as dampened affiliative responding (Auyeung & Alden, 2020; Zadro et al., 2006). In a substance using context (e.g., at a party), individuals with elevated SA may have competing responses to use substances to alleviate negative affect or conform to what others are doing to avoid further rejection and remain abstinent to maintain control or disengage from the social context entirely to avoid further rejection (Lemyre et al., 2019). Testing whether elevated SA during rejection (c.f., socially) leads to increased use willingness, can help clarify the relative role of SA, social context, and rejection-related stress on substance use decision-making.
This study expands prior work by examining the effects of SA and peer rejection on alcohol and cannabis use willingness in emerging adults with a range of SA symptoms and use levels. To reduce potential social-contextual confounds while maximizing generalizability, we used a laboratory-based experimental design where both conditions (Rejection vs. Neutral) and primary outcomes (use willingness) were integrated into a simulated party setting (Anderson et al., 2014; Cloutier et al., 2020). Of available tasks, mental imagery combined with audio/visual simulations provided an ideal balance of standardization, feasibility, and validity concerns (Anderson & Parent, 2007; Blackhart et al., 2009; Holmes & Mathews, 2010). Both SA and Rejection were expected to positively relate to alcohol and cannabis use willingness as main and interaction effects. While the same pattern was expected for both alcohol and cannabis, they were examined separately to directly test substance-specific differences (Egan et al., 2019; Yurasek et al., 2017). To account for prior use and poly-use, past-year alcohol and cannabis use frequency were included as covariates. To confirm the specificity of the effects to substance use (c.f., willingness to accept any offer), participants’ willingness to accept control items were included as covariates.
Method
Participants
All procedures were approved by the [omitted for blind review] Institutional Review Board before participant contact. Participants were recruited from a general undergraduate subject pool (49% psychology majors) at a large university in [omitted for blind review], where cannabis was illegal for recreational and most medical purposes. Participants aged 18–25 years reporting any lifetime cannabis use on an online screener were invited to the lab to confirm eligibility and screen for active substance use disorder recovery. Of the 91 participants who attended the laboratory visit, six were ineligible due to age (n = 4), no lifetime cannabis use (n = 1), or active recovery (n = 1). Data from five were lost due to technical errors (e.g., software crash), resulting in a final sample of 80 participants. See Table 1 for detailed descriptive statistics.
Table 1.
Sample Demographics and Between Group Comparisons across Experimental Conditions
| Variable | Total Sample (n = 80) | Rejection1 (n = 41) | Neutral (n = 39) |
|---|---|---|---|
| 2Gender % | |||
| Men | 28.7% | 29.3% | 28.2% |
| Women | 70.0% | 68.3% | 71.8% |
| Trans-Men | 1.3% | 2.4% | 0.0% |
| Sexual Orientation % | |||
| Heterosexual | 70.0% | 70.7% | 69.2% |
| Sexual Minority | 30.0% | 29.3% | 30.8% |
| Gay/Lesbian | 7.5% | 7.3% | 7.7% |
| Bisexual | 12.5% | 12.2% | 12.8% |
| Questioning | 2.5% | 0.0% | 5.1% |
| Pansexual | 5.0% | 7.3% | 2.6% |
| Asexual | 1.3% | 2.4% | 0.0% |
| Demisexual | 1.3% | 2.4% | 0.0% |
| Ethnicity % | |||
| Hispanic | 29.1% | 27.5% | 30.8% |
| Race/Ethnicity % | |||
| White | 66.1% | 59.4% | 73.3% |
| Black | 22.6% | 28.1% | 16.7% |
| Asian | 4.8% | 3.1% | 6.7% |
| Middle Eastern | 1.6% | 0.0% | 3.3% |
| Multiple | 4.8% | 9.4% | 0.0% |
| Past Year Disorders (SCID-V) % | |||
| Social Anxiety Disorder | 13.8% | 22.0% | 5.1% |
| Cannabis Use Disorder | 13.8% | 9.8% | 17.9% |
| Alcohol Use Disorder | 19.4% | 14.6% | 15.4% |
| Age M (SD) | 20.06 (1.95) | 19.85 (1.88) | 20.28 (2.03) |
| Social Interaction Anxiety Scale (SIAS) M (SD) | 22.40 (14.28) | 24.00 (14.90) | 20.72 (13.59) |
| Past Year Use Frequency M (SD) | |||
| Cannabis | 3.53 (1.88) | 3.05 (1.71) | 4.03 (1.93) |
| Alcohol | 4.06 (1.71) | 3.50 (1.64) | 4.62 (1.62) |
| Age of Onset M (SD) | |||
| Cannabis | 17.08 (1.86) | 16.85 (1.92) | 17.31 (1.79) |
| Alcohol | 16.47 (2.01) | 16.18 (2.30) | 16.74 (1.67) |
| Baseline Use Willingness M (SD) | |||
| Cannabis | 3.69 (2.85) | 3.61 (3.09) | 3.77 (2.62) |
| Alcohol | 4.06 (2.46) | 3.71 (2.16) | 4.44 (2.39) |
Note: One-way ANOVA’s and Chi Square tests evaluated whether experimental groups differed on any of the specified variables; variables that were statistically different (p <.05) across groups are bolded.
n= 38 for alcohol analyses after excluding for 3 cases reporting no lifetime alcohol use
Complete identities reported for descriptive purposes; gender was aggregated in subsequent analyses.
Baseline Measures
Social anxiety.
Typical SA was assessed with the 17-item Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998; Rodebaugh et al., 2011). Participants rated on a 0 (no at all) to 4 (extremely) scale the extent to which each item generally describes them (e.g., “I worry about expressing myself in case I appear awkward”). The SIAS evidences good psychometrics, such as internal consistency (current α = .87) and discriminant validity (Rodebaugh et al., 2007, 2011).
Substance use frequency.
Participants retrospectively rated how often they consumed alcohol and cannabis in their lifetime and past-year on a 1 (0 occasions) to 7 (40+ occasions) scale based on widely used national survey questions (Schulenberg et al., 2019).
Diagnostic status.
Trained doctoral psychology students or research assistants administered the Structured Clinical Interview for DSM–5 Disorders- RV to determine past-year diagnoses for cannabis use disorder (CUD), alcohol use disorder (AUD), and SAD (First et al., 2015). The inter-rater reliability was excellent, ranging from 86% for SAD to 98% for CUD.
Experimental Task and Measures
A gender-matched research assistant, blinded to study condition, provided instructions and training on two practice SIDE scenarios. Training helped to confirm understanding of the ‘Talk Aloud’ procedures (described below) and foster engagement in the imagined scenario (also see Anderson & Parent, 2007). After two successful practices or four attempts, the assistant read:
You will first walk into a friend’s house in the late afternoon/early evening. You will walk through their living room without anyone in it, overhear a conversation, then go through a series of rooms where your friends will ask you to join in on what they are doing. Whenever you see the word ‘GO’ be sure to say everything you can about how you are feeling in that moment – say as much as you can until you see ‘STOP’, then answer the questions that pop up onto the screen.
Please see Figure 1 for a graphical overview of the experimental task and timing of assessments.
Figure 1.
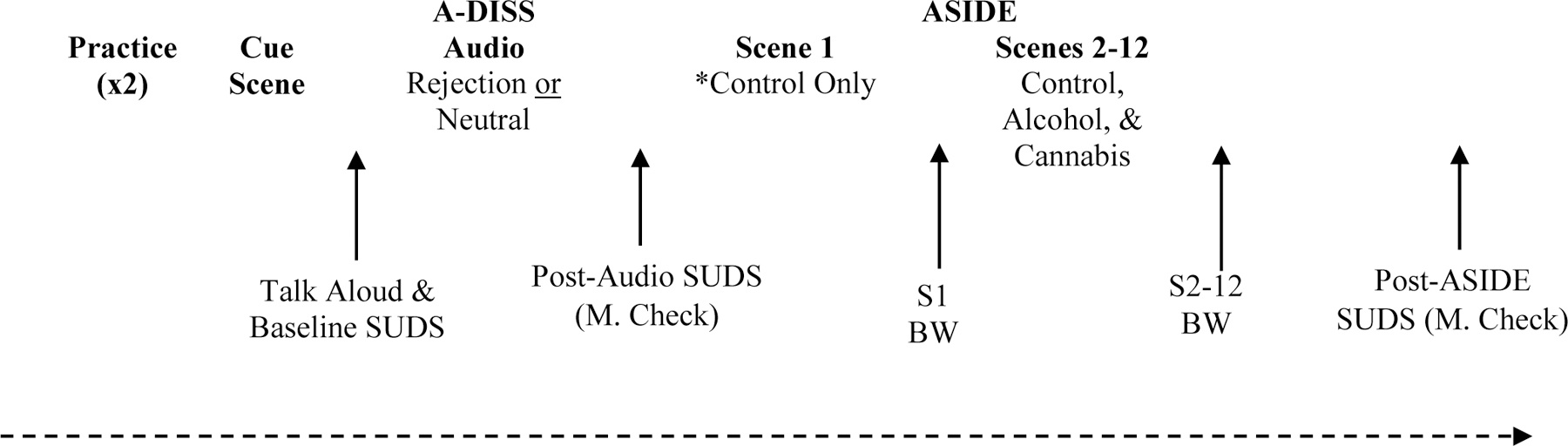
Graphical depiction of the experimental task where the A-DISS was integrated in the ASIDE protocol. See Cloutier et al. (2020) and Anderson et al. (2014; 2013) for validity information on each of these tasks.
SUDS= Subjective Units of Distress Scale; M. Check = Manipulation Check; S = scene; BW= Behavioral Use Willingness ratings.
Rejection and control conditions.
The Audio – Dialogue Inductions of Social Stress (A-DISS) was used as a rejection induction (Cloutier et al., 2020). Participants imagine overhearing peers talking in the other room while listening to pre-recorded audio. In the Rejection condition, participants hear peers criticizing their appearance and behavior at a recent social event (e.g., “s/he just looked so out of place”); in the Neutral condition, participants hear peers discussing an unidentified teacher critically (e.g., “Honestly, the teacher doesn’t seem to care very much about what she’s teaching.”) and positively (e.g., “… she’s not that bad!”). The voice actors are the same across conditions and use binary gender pronouns matched to the participant. The A-DISS has evidence of construct and internal validity among young adults (Cloutier et al., 2020).
Simulated party context.
The Simulated Intoxication Digital Elicitation task (SIDE) was used to both simulate a relevant social context and assess participants’ willingness to use each substance within that context (Anderson et al., 2014). The SIDE includes 13 30-second video scenes. The first is a ‘cue scene’ of an empty living room with all of the stimulus items which creates a context for the remaining scenes and diminishes novelty effects from first seeing the items. The remaining 12 scenes show two actors talking to the participant about a neutral topic (e.g., playing basketball) before offering them food (3 scenes), non-alcoholic drinks (3 scenes), alcoholic drinks (3 scenes), or cannabis (3 scenes). After each scene, participants complete an open-ended 30 second ‘Talk Aloud’ about their thoughts and feelings at that moment. The ‘Talk Alouds’ foster engagement in the mental imagery component while providing near-concurrent, open-ended responses (see Anderson & Parent, 2007; Holmes & Matthews, 2010). Then, participants quantitatively rate their willingness to accept the offer made in the scene (e.g., “how willing would you be to accept the joint?”).
Manipulation checks.
Subjective Units of Distress Scales (SUDS; Perrin et al., 2000) were administered after the Cue Scene (Baseline) and A-DISS (Condition Exposure) to confirm the efficacy of each condition. Participants rated how anxious, rejected, and insecure they felt in that moment on 1 (not at all) to 9 (extremely) scales. Similar items have been used in lab studies of SA repeatedly assessing state-affect (Buckner, Silgado, et al., 2011; Cloutier et al., 2020).
Alcohol/Cannabis use willingness.
To assess baseline use willingness, two face valid items were added to the SUDS battery after the SIDE Cue Scene. Participants rated how willing they were to use alcohol or marijuana if it were offered to them on a 1 (not at all) to 9 (extremely) scale. The primary use willingness variables were derived from the quantitative SIDE ratings. After each scene, participants rated their willingness to use the item offered on a 1 (not at all willing) to 7 (very willing) scale. Alcohol, cannabis, non-alcoholic drinks, and food scales were then computed with possible scores ranging from 3–21 for each offer type. The SIDE ratings have shown good concurrent and predictive validity (Anderson et al., 2013, 2014).
Analytic Approach & Results
Preliminary Analyses
Three participants did not report lifetime alcohol use so were excluded from the alcohol use willingness analyses (final n = 77; 76% women). One-way ANOVA and Chi-Square analyses tested the equivalence of experimental conditions on baseline traits (e.g., age, SA symptoms, gender) and use willingness. As shown in Table 1, there were no condition differences on age, gender, SIAS scores, past-year CUD, AUD, cannabis problems, or baseline use willingness for alcohol or cannabis. There were differences in past-year substance use and SAD - participants in the Neutral condition reported more frequent alcohol and cannabis use and more participants in the Rejection condition met diagnostic criteria for SAD. As shown in Table 2, SIAS scores were positively correlated with SA diagnoses but were unrelated to age, gender, substance use frequency, or baseline use willingness (p’s > .05). Thus, past-year use was the only baseline covariate included in the primary analyses. Despite condition differences, SAD was excluded from primary analyses due to the low number of positive cases overall and within each subgroup.
Table 2.
Bivariate Correlations of Retrospective Social Anxiety Symptoms, Marijuana Outcomes, and Potential Covariates
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1.SIAS Score | - | .44** | −.15 | −.14 | .07 | .09 | −.04 | .10 | .06 | −.01 |
| 2. Social Anxiety Disorder | - | −.14 | −.19 | −.20 | −.05 | −.18 | −.08 | .06 | −.02 | |
| 3. Cannabis Frequency | - | .39** | −.23* | −.03 | .00 | −.06 | .42** | .15 | ||
| 4. Alcohol Frequency | - | −.13 | −.16 | .28* | .23* | .26* | .44** | |||
| 5. Age of Cannabis Onset | - | .56** | .29* | −.06 | −.25* | −.13 | ||||
| 6. 1Age of Alcohol Onset | - | .08 | −.11 | −.15 | −.14 | |||||
| 7. Age | - | −.11 | .02 | .25** | ||||||
| 8.Gender (Men)2 | - | .03 | −.05 | |||||||
| 9. Baseline Marijuana Use Willingness | - | .40* | ||||||||
| 10. Baseline Alcohol Use Willingness | - |
Note: n= 80; SIAS = Social Interaction Anxiety Scale.
n= 77 (participants who did not report lifetime alcohol use were not asked about past year use frequency or age of alcohol onset).
Women=1, Men=0; thus positive correlations reflect higher scores among women and negative correlations higher scores among men (including trans)
p ≤ .05,
p ≤ .01.
Repeated measures ANOVA’s tested the efficacy of the Rejection condition in increasing SUDS levels from baseline. The 3 (Time) x 2 (Condition) interaction was significant for anxiety, F[2, 156] = 18.654, p < .001, Partial η2 = .193, rejected, F[2, 152] = 69.165, p < .001, Partial η2 = .476, and insecure, F[2, 154] = 45.763, p < .001, Partial η2 = .373. As shown in Figure 2, only participants in the Rejection condition had increased SUDS levels; those in the Neutral condition maintained similar, low SUDS levels that never departed from baseline.
Figure 2a-c.
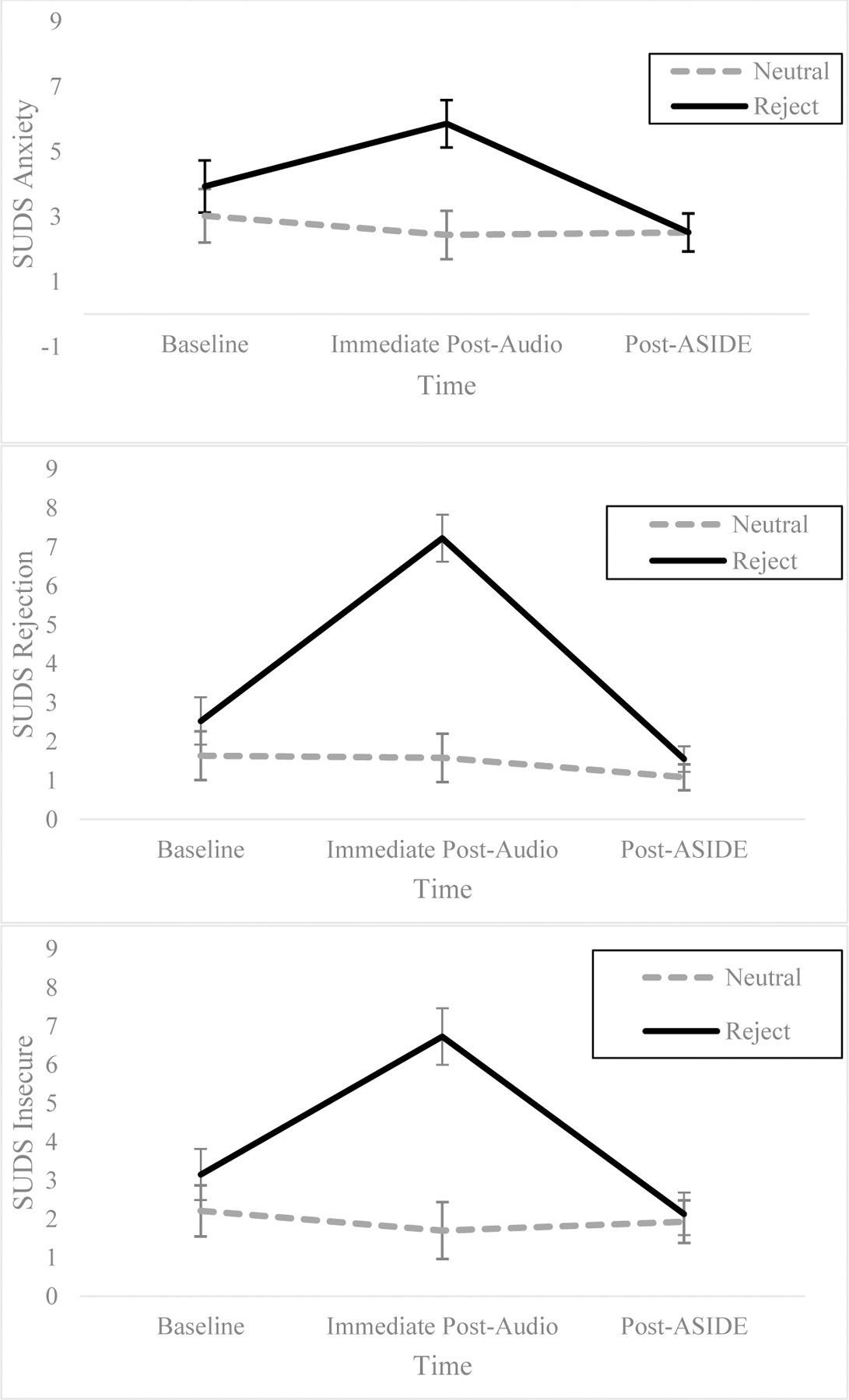
Condition x time Repeated Measures ANOVA predicting Subjective Units of Distress Scale (SUDS) at baseline (post-cue scene), post-audio exposure, and at the end of the ASIDE simulation Adjusted means and 95% CI are plotted.
Primary Analyses
Two hierarchical regressions tested whether the greatest alcohol and cannabis use willingness was associated with higher SIAS scores and Rejection exposure. Condition assignment was dummy-coded and entered with SIAS scores in Step 2, and the interaction term was entered in Step 3. The overall models predicting alcohol (R2 =.194, F[5,76]=3.422, p = .008) and cannabis (R2 =.518, F[5,79]=15.875, p<.001) use willingness were statistically significant. As shown in Table 3, covariates accounted for most of the variance in both models. For the alcohol model, neither the main nor the interaction effects were statistically significant. For the cannabis model, the main effects of SIAS scores and condition in Step 2 were statistically significant; however, the interaction term was not. As depicted in Figure 3, main effects indicated that elevated SIAS scores and the Rejection condition were each associated with greater cannabis use willingness
Table 3.
Hierarchical Multiple Regressions Predicting Marijuana and Alcohol Use Willingness
| Predictor | ∆R2 | β | sr 2 | p | ∆R2 | β | sr 2 | p |
|---|---|---|---|---|---|---|---|---|
| Cannabis Use Willingness (N = 80) | Alcohol Use Willingness (n = 77)* | |||||||
|
|
|
|||||||
| Step 1 | .46 | < .001 | .18 | .002 | ||||
| Past Yr. Cannabis Use | .675 | .916 | < .001 | .025 | .177 | .830 | ||
| Past Yr. Alcohol Use | .002 | .148 | .985 | .414 | .900 | .001 | ||
| Other Willingness | .199 | .020 | .023 | .137 | .036 | .203 | ||
| Step 2 | .06 | .011 | .01 | .628 | ||||
| Past Yr. Cannabis Use | .724 | .805 | < .001 | .044 | .167 | .707 | ||
| Past Yr. Alcohol Use | .075 | .130 | .431 | .439 | .848 | .001 | ||
| Other Willingness | .228 | .017 | .007 | .125 | .034 | .256 | ||
| Condition | .187 | .001 | .039 | .070 | .024 | .541 | ||
| SIAS Score | .176 | .012 | .036 | .077 | .008 | .484 | ||
| Step 3 | .00 | .563 | .00 | .681 | ||||
| Past Yr. Cannabis Use | .713 | .800 | < .001 | .034 | .165 | .777 | ||
| Past Yr. Alcohol Use | .079 | .129 | .411 | .442 | .840 | .001 | ||
| Other Willingness | .226 | .017 | .008 | .118 | .033 | .292 | ||
| Condition | .109 | .001 | .503 | -.003 | .024 | .988 | ||
| SIAS Score | .120 | .012 | .348 | .027 | .008 | .873 | ||
| Condition X SIAS Score | .110 | .021 | .563 | .104 | < .001 | .681 | ||
Note: Past Yr. = number of cannabis or alcohol use occasions in the past year. Other Willingness = ASIDE willingness to accept control offers of food (cannabis model) or non-alcoholic beverages (alcohol model). SIAS = Social Interaction Anxiety Scale. Condition coded such that Neutral = 0 (referent) and Rejection = 1. sr2= squared structure coefficient. ∆R2 = R-square change.
three cases who reported no alcohol use in their lifetime were excluded from these analyses only.
Figure 3.
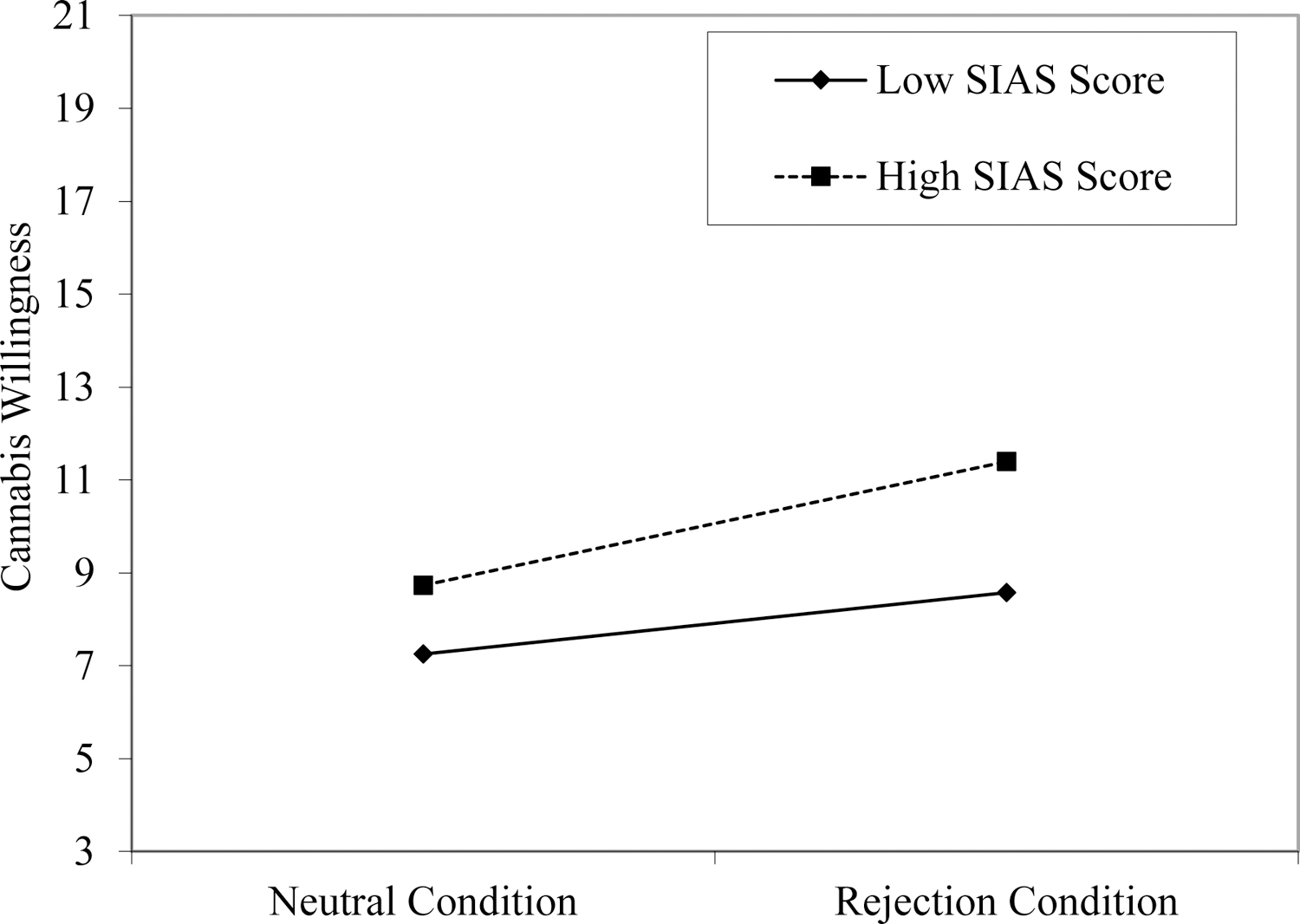
Main effects of SIAS Score and experimental condition on mean cannabis use willingness. SIAS Score was analyzed continuously but is plotted with +/− 1 SD of the mean for presentation only.
Discussion
As expected, SA and Rejection exposure were each independently associated with greater cannabis use willingness. This result is consistent with both ideas that cannabis is used as a means of attenuating negative affect and reconnecting with social networks (Buckner, Heimberg, et al., 2013; Mallott et al., 2009). While these same models also suggest SA would exacerbate or dampen the effects of rejection on use willingness, the lack of a moderation is not wholly contradictory. Participants with higher SA were still more willing to use cannabis than those with lower SA. That SA positively related to use willingness during both the social scenarios and not the cue scene (baseline period), highlights the risk in social situations where others are using and not just where cannabis is available - even in anticipation of an upcoming social event. Over time, this elevated willingness to use cannabis across social contexts may lead to greater use and problems, even if SA does not exacerbate the effects of rejection in a given moment. Combined with prior work and theory, results suggest at early cannabis use levels, SA increases conformity use patterns and sensitivity to social use cues; over time and with more experience, SA may accelerate coping motivated use and problems (Cloutier et al., 2016; Cooper, 1994). Critically, we did not directly test this hypothesis and would be strengthened in a longitudinal design.
Although inconsistent with hypotheses, other laboratory studies also have failed to find the effects of SA on alcohol outcomes. Emerging adults may be more wary about consuming alcohol offered by strangers, particularly in a sample with a majority of women in a novel or potentially unsafe context (Bacon et al., 2015; Bacon & Engerman, 2018). As both substances were offered in random order, participants may have considered using cannabis to be a safer way of engaging with the social context. Selecting for cannabis use also may have diluted effects observed in studies that selected for heavy alcohol use. As such, these results offer more robust estimates for primary cannabis users, while reinforcing the need to consider polysubstance use and test for substance specific mechanisms in future work (Egan et al., 2019; Yurasek et al., 2017).
Despite strong empirical support that willingness prospectively predicts real-world use, future studies incorporating real-time assessments of use and competing mechanisms (e.g., expectancies, motives, intentions, craving) across methods (e.g., laboratory-based; EMA) are needed (Anderson et al., 2013, 2014; Lewis et al., 2019). Another concern is whether this study was statistically powered to detect the moderation of SA and Rejection. While designed around estimates suggesting medium-high effects on craving (Buckner et al., 2011; 2016), the current results suggest negligible effects requiring a much larger sample (n > 1,000). Lastly, this study tested a range of SA symptoms with the SIAS and relied on blind random assignment to evenly distribute key characteristics across conditions. While SIAS scores were evenly distributed, SAD was not, and the low number of cases with SAD prevented further testing. Complex assignment approaches with larger samples containing more SAD cases may have produced larger effects.
The experimental design was a strength that also extends the A-DISS and SIDE validation work (Anderson et al., 2013; Cloutier et al., 2020). Together, the A-DISS and SIDE offer a standardized social stressor embedded within a relevant context to model real-time alcohol and cannabis use cognitions. Overhearing a conversation about a teacher in the Neutral condition, kept it procedurally identical to the Rejection condition without eliciting real-time SA. This helped clarify the extent to which participants with elevated SA were more willing to use alcohol or cannabis within the context of rejection, rather than in social contexts or stress more broadly. The next steps include directly comparing the current task against other widely used tasks while considering other substances across different ages (Lewis et al., 2019; Litt et al., 2018).
This study tested whether individuals with higher SA were more willing to use alcohol and cannabis after experiencing rejection versus a socially neutral cue. We extend prior work by isolating the specific effects of SA and rejection on cannabis use, while accounting for alcohol use. That elevated SA was associated with cannabis use willingness across conditions suggests a proclivity to use in any social context where cannabis is available, even without social stressors. Results reinforce the need to carefully model social contexts and poly-substance use in future research. Clinically, this study suggests the value of use willingness as a malleable target for early college interventions, particularly for emerging adults whom have not yet formalized their substance use patterns nor developed more serious use-related problems. For example, prototype willingness model based interventions have demonstrated efficacy and could be enhanced by targeting individual SA symptoms or contexts involving rejection (Pomery et al., 2009).
Public Health Significance Statement.
Substance use often occurs in social settings where multiple substances are available; because socially anxious individuals are hypersensitive to social cues, this study reinforces the need to carefully model individual- and context-level interactions on substance use risk in laboratory-based designs. Specifically, findings suggest that in social settings where both alcohol and cannabis are available, experiencing rejection increases vulnerability for cannabis use, but not alcohol use. Findings also suggest that young adults with elevated social anxiety are more willing to use cannabis in social situations, even without experiencing rejection or elevated anxiety symptoms.
Acknowledgments
Research supported by: R. Cloutier was partially supported by a National Institute of Health National Research Service Award (1F31DA041105) while at the University of North Texas (presently at the Pennsylvania State University and supported by T32DA017629). N. Kearns was supported by a National Institute of Health National Research Service Award (1F31AA027142–01). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
The authors have no known conflicts of interest to disclose.
Portions of these results were presented at the 2018 conventions of the Collaborative Perspectives on Addiction and the American Psychological Association.
References
- Abrams K, Kushner M, Lisdahl Medina K, & Voight A (2001). The pharmacologic and expectancy effects of alcohol on social anxiety in individuals with social phobia. Drug and Alcohol Dependence, 64(2), 219–231. 10.1016/S0376-8716(01)00125-9 [DOI] [PubMed] [Google Scholar]
- Allen HK, Caldeira KM, Bugbee BA, Vincent KB, O’Grady KE, & Arria AM (2017). Drug involvement during and after college: Estimates of opportunity and use given opportunity. Drug and Alcohol Dependence, 174, 150–157. 10.1016/j.drugalcdep.2017.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KG, Brackenbury L, Quackenbush M, Buras M, Brown SA, & Price J (2014). A-SIDE: Video simulation of teen alcohol and marijuana use contexts. Journal of Studies on Alcohol and Drugs, 75(6), 953–957. 10.15288/jsad.2014.75.953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KG, Duncan K, Buras M, Packard CD, & Kennedy C (2013). C-SIDE: Drinking simulation for college students. Journal of Studies on Alcohol and Drugs, 74(1), 94–103. 10.15288/jsad.2013.74.94 [DOI] [PubMed] [Google Scholar]
- Anderson KG, & Parent SJ (2007). Adolescent decision-making about substance use: A video-based assessment. In Galwye (Ed.), Progress in Educational Psychology Research (pp. 3–21). Nova Science Publishers. [Google Scholar]
- Arnett EJ (2005). The developmental context of substance use in emerging adulthood. Journal of Drug Issues, 35(2), 235–253. 10.1177/002204260503500202 [DOI] [Google Scholar]
- Auyeung K, & Alden LE (2020). Accurate Empathy, Social Rejection, and Social Anxiety Disorder. Clinical Psychological Science, 8(2), 266–279. 10.1177/2167702619885410 [DOI] [Google Scholar]
- Bacon AK, Cranford AN, & Blumenthal H (2015). Effects of ostracism and sex on alcohol consumption in a clinical laboratory setting. Psychology of Addictive Behaviors, 29(3), 664–672. 10.1037/adb0000054 [DOI] [PubMed] [Google Scholar]
- Bacon AK, & Engerman B (2018). Excluded, then inebriated: A preliminary investigation into the role of ostracism on alcohol consumption. Addictive Behaviors Reports, 8(May), 25–32. 10.1016/j.abrep.2018.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battista SR, Stewart SH, & Ham LS (2010). A Critical review of laboratory-based studies examining the relationships of social anxiety and alcohol intake. Current Drug Abuse Reviews, 3(1), 3–22. 10.2174/1874473711003010003 [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, & Morris TL (2000). Behavioral treatment of childhood social phobia. Journal of Consulting and Clinical Psychology, 68(6), 1072–1080. 10.1037/0022-006X.68.6.1072 [DOI] [PubMed] [Google Scholar]
- Blackhart GC, Nelson BC, Knowles ML, & Baumeister RF (2009). Rejection elicits emotional reactions but neither causes immediate distress nor lowers self-esteem: A meta-analytic review of 192 studies on social exclusion. Personality and Social Psychology Review, 13(4), 269–309. 10.1177/1088868309346065 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Ecker AH, & Vinci C (2013). Cannabis use vulnerability among socially anxious users: Cannabis craving during a social interaction. Psychology of Addictive Behaviors, 27(1), 236–242. 10.1037/a0029763 [DOI] [PubMed] [Google Scholar]
- Buckner JD, & Heimberg RG (2010). Drinking Behaviors in Social Situations Account for Alcohol-Related Problems Among Socially Anxious Individuals. Psychology of Addictive Behaviors, 24(4), 640–648. 10.1037/a0020968 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Ecker AH, & Vinci C (2013). A biopsychosocial model of social anxiety and substance use. Depression and Anxiety, 30(3), 276–284. 10.1002/da.22032 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, & Schmidt NB (2011). Social anxiety and marijuana-related problems: The role of social avoidance. Addictive Behaviors, 36(1–2), 129–132. 10.1016/j.addbeh.2010.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Schneier FR, Liu SM, Wang S, & Blanco C (2012). The relationship between cannabis use disorders and social anxiety disorder in the National Epidemiological Study of Alcohol and Related Conditions (NESARC). Drug and Alcohol Dependence, 124(1–2), 128–134. 10.1016/j.drugalcdep.2011.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Silgado J, & Schmidt NB (2011). Marijuana craving during a public speaking challenge: Understanding marijuana use vulnerability among women and those with social anxiety disorder. Journal of Behavior Therapy and Experimental Psychiatry, 42(1), 104–110. 10.1016/j.jbtep.2010.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Ecker AH, & Jeffries ER (2016). Cannabis craving in response to laboratory-induced social stress among racially diverse cannabis users: The impact of social anxiety disorder. Journal of Psychopharmacology, 30(4), 363–369. 10.1177/0269881116629115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrigan MH, & Randall CL (2003). Self-medication in social phobia: A review of the alcohol literature. Addictive Behaviors, 28(2), 269–284. 10.1016/S0306-4603(01)00235-0 [DOI] [PubMed] [Google Scholar]
- Cloutier RM, Bilsky SA, Baxley C, Anderson KG, & Blumenthal H (2020). Development of a novel social rejection task to explore the unique and overlapping affective features of social anxiety and depression. Cognitive Therapy and Research, in press. [DOI] [PMC free article] [PubMed]
- Cloutier RM, Blumenthal H, & Mischel ER (2016). An Examination of Social Anxiety in Marijuana and Cigarette Use Motives among Adolescents. Substance Use and Misuse, 51(3), 408–418. 10.3109/10826084.2015.1110174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Swendsen J, Husky MM, He JP, & Merikangas KR (2016). Association of Lifetime Mental Disorders and Subsequent Alcohol and Illicit Drug Use: Results from the National Comorbidity Survey-Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry, 55(4), 280–288. 10.1016/j.jaac.2016.01.006 [DOI] [PubMed] [Google Scholar]
- Deros DE, Racz SJ, Lipton MF, Augenstein TM, Karp JN, Keeley LM, Qasmieh N, Grewe BI, Aldao A, & De Los Reyes A (2018). Multi-Informant Assessments of Adolescent Social Anxiety: Adding Clarity by Leveraging Reports from Unfamiliar Peer Confederates. Behavior Therapy, 49(1), 84–98. 10.1016/j.beth.2017.05.001 [DOI] [PubMed] [Google Scholar]
- Dimoff JD, & Sayette MA (2017). The case for investigating social context in laboratory studies of smoking. Addiction, 112(3), 388–395. 10.1111/add.13503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan KL, Cox MJ, Suerken CK, Reboussin BA, Song EY, Wagoner KG, & Wolfson M (2019). More drugs, more problems? Simultaneous use of alcohol and marijuana at parties among youth and young adults. Drug and Alcohol Dependence, 202(February), 69–75. 10.1016/j.drugalcdep.2019.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured Clinical Interview for DSM‐ 5: Research Version. American Psychiatric Associatio. [Google Scholar]
- Franco S, Olfson M, Wall MM, Wang S, Hoertel N, & Blanco C (2019). Shared and specific associations of substance use disorders on adverse outcomes: A national prospective study. Drug and Alcohol Dependence, 201(April), 212–219. 10.1016/j.drugalcdep.2019.03.003 [DOI] [PubMed] [Google Scholar]
- Gerrard M, Gibbons FX, Houlihan AE, Stock ML, & Pomery EA (2008). A dual-process approach to health risk decision making: The prototype willingness model. Developmental Review, 28(1), 29–61. 10.1016/j.dr.2007.10.001 [DOI] [Google Scholar]
- Gibbons FX, Gerrard M, Lune L. S. Vande, Wills TA, Brody G, & Conger RD (2004). Context and Cognitions: Environmental Risk, Social Influence, and Adolescent Substance Use. Personality and Social Psychology Bulletin, 30(8), 1048–1061. 10.1177/0146167204264788 [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Vande Lune LS, Wills TA, Brody G, & Conger RD (2004). Context and cognitions: Environmental risk, social influence, and adolescent substance use. Personality and Social Psychology Bulletin, 30(8), 1048–1061. 10.1177/0146167204264788 [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Patricia Chou S, Jung J, Zhang H, Pickering RP, June Ruan W, Smith SM, Huang B, & Hasin DS (2015). Epidemiology of DSM-5 alcohol use disorder results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Jung J, Zhang H, & Grant BF (2016). Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: Findings from the national epidemiologic survey on alcohol and related conditions-III. American Journal of Psychiatry, 173(6), 588–599. 10.1176/appi.ajp.2015.15070907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, & Mathews A (2010). Mental imagery in emotion and emotional disorders. Clinical Psychology Review, 30(3), 349–362. 10.1016/j.cpr.2010.01.001 [DOI] [PubMed] [Google Scholar]
- Hudd T, & Moscovitch DA (2020). Coping with social wounds: How social pain and social anxiety influence access to social rewards. Journal of Behavior Therapy and Experimental Psychiatry, 68(April), 101572. 10.1016/j.jbtep.2020.101572 [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (1997). The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications: Harvard Review of Psychiatry: Vol 4, No 5. Harvard Review of Psychiatry, 4(5), 231–244. 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Ladd BO, Garcia TA, & Anderson KG (2016). A novel application in the study of client language: Alcohol and marijuana-related statements in substance-using adolescents during a simulation task. Psychology of Addictive Behaviors, 30(6), 672–679. 10.1037/adb0000202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemyre A, Gauthier-Légaré A, & Bélanger RE (2019). Shyness, social anxiety, social anxiety disorder, and substance use among normative adolescent populations: A systematic review. American Journal of Drug and Alcohol Abuse, 45(3), 230–247. 10.1080/00952990.2018.1536882 [DOI] [PubMed] [Google Scholar]
- Lewis MA, Litt DM, King KM, Fairlie AM, Waldron KA, Garcia TA, Loparco C, Lee CM, Lewis MA, Litt DM, King KM, Fairlie AM, Garcia TA, & Lee CM (2019). Examining the Ecological Validity of the Prototype Willingness Model for Adolescent and Young Adult Alcohol Use Adolescent and Young Adult Alcohol Use. Psychology of Addictive Behaviors. [DOI] [PMC free article] [PubMed]
- Litt DM, Lewis MA, Spiro ES, Aulck L, Waldron KA, Head-Corliss MK, & Swanson A (2018). #drunktwitter: Examining the relations between alcohol-related Twitter content and alcohol willingness and use among underage young adults. Drug and Alcohol Dependence, 193(July), 75–82. 10.1016/j.drugalcdep.2018.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallott MA, Maner JK, Dewall N, & Schmidt NB (2009). Compensatory deficits following rejection: The role of social anxiety in disrupting affiliative behavior. Depression and Anxiety, 26(5), 438–446. 10.1002/da.20555 [DOI] [PubMed] [Google Scholar]
- Pomery EA, Gibbons FX, Reis-Bergan M, & Gerrard M (2009). From willingness to intention: Experience moderates the shift from reactive to reasoned behavior. Personality and Social Psychology Bulletin, 35(7), 894–908. 10.1177/0146167209335166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Klein SR, Yarkoni T, & Langer JK (2011). Measuring social anxiety related interpersonal constraint with the flexible iterated prisoner’s dilemma. Journal of Anxiety Disorders, 25(3), 427–436. 10.1016/j.janxdis.2010.11.006 [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, & Heimberg RG (2007). The Reverse of Social Anxiety Is Not Always the Opposite: The Reverse-Scored Items of the Social Interaction Anxiety Scale Do Not Belong. Behavior Therapy, 38(2), 192–206. 10.1016/j.beth.2006.08.001 [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Johnston L, O’Malley P, Bachman J, Miech R, & Patrick M (2019). Monitoring the Future national survey results on drug use, 1975–2018: Volume II, college students and adults ages 19–60: Vol. II. 10.3998/2027.42/150623 [DOI] [Google Scholar]
- Tamir DI, & Hughes BL (2018). Social Rewards: From Basic Social Building Blocks to Complex Social Behavior. Perspectives on Psychological Science, 13(6), 700–717. 10.1177/1745691618776263 [DOI] [PubMed] [Google Scholar]
- Yurasek AM, Aston ER, & Metrik J (2017). Co-use of Alcohol and Cannabis: A Review. Current Addiction Reports, 4(2), 184–193. 10.1007/s40429-017-0149-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zadro L, Boland C, & Richardson R (2006). How long does it last? The persistence of the effects of ostracism in the socially anxious. Journal of Experimental Social Psychology, 42(5), 692–697. 10.1016/j.jesp.2005.10.007 [DOI] [Google Scholar]


