Dear Editor,
Average noise levels in the intensive care unit (ICU) are constantly above the recommended values with peaks exceeding 80 dB(A) (Crawford et al., 2018) due to monitoring devices, mechanical ventilators, infusion pumps, and other life-support equipment. Most of the disruptive noises, with levels from 75 dB(A) to 85 dB(A), are caused by alarms, phones, staff activities, and conversations (Crawford et al., 2018, Darbyshire et al., 2019). Face masks, reusable respirators, and coverall hoods limit the ability to hear alarms and voices, forcing health care staff to raise their voices (Imbriaco et al., 2021). Therefore, noise levels increase together with stress and the risk of errors and complications (Nguyen et al., 2021). We hypothesized that noise levels in the ICU could be increased during the COVID-19 pandemic due to the massively increased workload and the use of personal protective equipment (PPE).
We compared noise levels between COVID-19 ICUs and non-COVID-19 ICUs in four open space ICUs in two tertiary level hospitals in Northern Italy. Noise levels were evaluated in a COVID-19 ICU and a cardiothoracic ICU, both of 14-beds, and in a 10-beds COVID-19 ICU and an 11-beds general/surgical/trauma ICU. Sound measurements were performed simultaneously, over a continuous period of one week, from February 8th, 2021 until February 15th, 2021, during the second peak of the COVID-19 pandemic. Sound levels were measured in decibel using an A-weighted scale dB(A) with a noise meter application (Decibel X by SkyPaw Co) installed on tablets positioned in a central location of the unit, on a shelf of a supply column, at the height of the patient’s head.
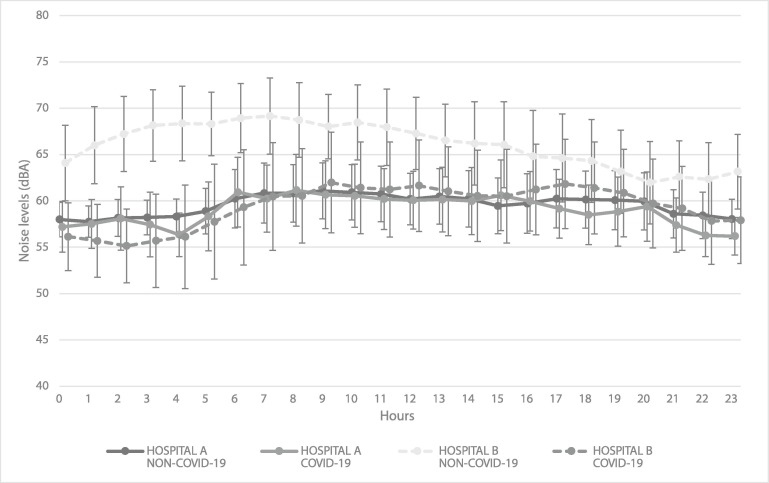
We found that the average noise level among the four ICUs was 60.9 (±3) dB(A), with minimum and maximum values of 51.1 and 100 dB(A), respectively (Fig. 1 ). Average noise levels in the two COVID-19 ICUs was 59 (±4.4) dB(A) while in the two non-COVID-19 ICUs was 63 (±5.2) dB(A) (p < 0.001). In Hospital A, the noise level in the COVID-19 ICU was 58.9 (±3.6) dB(A) compared to 59.5 (±2.9) dB(A) in the non-COVID-19 ICU (p < 0.001). In Hospital B, noise levels were 59.2 (±5.4) dB(A) and 66.1 (±4.7) dB(A) in the COVID-19 and non-COVID-19 ICUs, respectively (p < 0.001). ICU bed occupancy was constantly over 90% during the study in all of ICUs.
Fig. 1.
Trend of mean (and standard deviation) sound pressure levels measured as A-weighted decibels (dB(A)) over the 24 h in the four intensive care units. Hospital A = IRCCS San Raffaele Scientific Institute, Milan, Italy; Hospital B = Maggiore Hospital Carlo Alberto Pizzardi, Bologna, Italy.
Despite the use of PPE and their potential role in limiting hearing and speaking, noise levels in COVID-19 and non-COVID19 ICUs were similar but consistently above the recommended levels, with peak levels exceeding 90 dB(A), both during daytime and overnight. Telephones and working areas seem to be an important source of noise. The evaluation of noise levels in the ICU setting, even if performed with simple instruments such as commercial applications and tablets, may represent a valuable approach to promote noise reduction strategies, with clear benefits for patients and health care providers (Scquizzato et al., 2020). The potential limitations on communication caused by PPE, associated with a high noise environment such as the ICU, should be carefully considered for risk reduction strategies.
Author contribution
All authors made a significant contribution to the conception, study design, data collection, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval statement
Ethical board approval is not required at our institutions for studies not involving patient data.
CRediT authorship contribution statement
Guglielmo Imbriaco: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Supervision. Arianna Gazzato: Conceptualization, Investigation, Data curation. Alessandro Monesi: Conceptualization, Investigation, Data curation. Tommaso Scquizzato: Investigation, Formal analysis, Data curation, Visualization, Writing – review & editing. Federico Semeraro: Conceptualization, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Authors would like to thank the SkyPaw team, developers of the Decibel X app, for their support, and all the ICU staff who have been working tirelessly during the COVID-19 emergency.
References
- Crawford K.J., Barnes L.A., Peters T.M., Falk J., Gehlbach B.K. Identifying determinants of noise in a medical intensive care unit. J. Occup. Environ. Hyg. 2018;15(12):810–817. doi: 10.1080/15459624.2018.1515491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbyshire J.L., Müller‐Trapet M., Cheer J., Fazi F.M., Young J.D. Mapping sources of noise in an intensive care unit. Anaesthesia. 2019;74(8):1018–1025. doi: 10.1111/anae.2019.74.issue-810.1111/anae.14690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbriaco G., Monesi A., Ferrari P. Nursing perspectives from an Italian ICU. Nursing (Lond). 2021;51:46–51. doi: 10.1097/01.NURSE.0000724372.73357.bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen D.D., McCabe P., Thomas D., Purcell A., Doble M., Novakovic D., Chacon A., Madill C. Acoustic voice characteristics with and without wearing a facemask. Scientific reports. 2021;11(1):5651. doi: 10.1038/s41598-021-85130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scquizzato T., Gazzato A., Landoni G., Zangrillo A. Assessment of noise levels in the intensive care unit using Apple Watch. Crit. Care. 2020;24:20–22. doi: 10.1186/s13054-020-02852-3. [DOI] [PMC free article] [PubMed] [Google Scholar]