Abstract
Background/aims
The aim of this study was to identify the trends in antidepressant (AD) medication use in two Irish general practices over a 5-year period, 2016 to 2020. The rationale for this study is attributed to the growing prevalence of depression amongst the Irish general public as well as concerns surrounding long-term AD medication use.
Methods
The research was undertaken in 2021 examining AD prescription rates from 2016 to 2020. The medications of interest were selective serotonin and norepinephrine reuptake inhibitors (SSRI and SNRIs): sertraline, escitalopram, fluoxetine and venlafaxine. The number of medical card holders (MCH) and prescription dispensing rates were analysed for observable trends.
Results
AD medication use is rising amongst the Irish MCH population. The number of MCH prescribed AD grew from 9.42 to 12.3 per 100 MCH between the years 2016 and 2020, respectively. The year 2020 represented the largest proportion of MCH prescriptions, 6.32 AD prescriptions per 1000 MCH prescriptions. The years 2019 to 2020 represented the largest annual increase in prescription dispensing with a growth of 0.45 per 1000 MCH prescriptions. Annual figures show a continual increase in AD dispensing refill rates from 4.14 to 5.67 per 1000 MCH prescriptions in 2016 and 2020, respectively.
Conclusion
This study illustrates a steady rise in AD medication within the general practice setting, with an observed rise in prescription dispensing rates. The high proportion of refill prescriptions demonstrates the long-term use of AD medications. This may be indicative of chronic depression or may highlight a lack of appropriate medication cessation strategies.
Keywords: Antidepressants, Depression, General practice, Long-term use, Medication, Prescribing
Introduction
Depression is defined by the World Health Organization (WHO) as a persistent feeling of sadness and lack of interest or pleasure [1]. WHO reports that depression affects over 330 million people worldwide and is now the leading cause of disability in today’s society. The Organisation for Economic Co-operation and Development (OECD) Health at a Glance report found that Ireland has one of the highest rates of mental health illness within Europe, with it being reported in 2016 that 18.5% of the Irish population had a mental health illness [2]. The first-line treatment for depression tends to be lifestyle modification such as the promotion of exercise, sleep, good nutrition and social support. Exercise has been found to work as a monotherapy in the treatment of depression in addition to augmentation with psychotherapy [3]. Treatment tends to be a stepwise approach and varies on a patient-to-patient basis. Healthcare providers may offer psychological treatments such as cognitive behavioural therapy (CBT) or instead opt for pharmacological intervention if prior efforts fail [4]. Examples of such interventions include SSRIs or tricyclic antidepressants (TCAs).
In recent years, following a rise in the incidence of depression, antidepressant medication usage has risen accordingly. In 2016, an article published by the English National Health Services organization reported antidepressant prescription dispensing increased by 3.7 million items (6.0%), from 61.0 to 64.7 million, between 2015 and 2016 (antidepressants were the area with the largest increase in prescription items in 2016—NHS [5]. Numerous factors have been identified which may explain this marked rise in antidepressant medication expenditure, including an overall increase in the incidence of depression, effective pharmaceutical marketing strategies or even inappropriate prescribing by doctors [6]. While antidepressants may be a convenient, relatively effective treatment option, they carry some problematic adverse side effects including dizziness, nausea, dry mouth, sweating, tiredness and insomnia [7].
Furthermore, the cessation of antidepressant medication is known to be associated with unwanted withdrawal symptoms. The National Institute for Health and Care Excellence (NICE) guidance previously reported that withdrawal from antidepressants is ‘mild and self-limiting’ [8]. However, more recent studies have indicated that withdrawal effects from antidepressants may be more severe and longer in duration than previously believed [9]. Research has documented a lack of understanding surrounding prescribing habits relating to antidepressant medications. A study conducted by Bosman et al. expresses a miscommunication between general practitioners and the patient regarding antidepressant use and appropriate cessation [10]. Hence, greater research to ensure general practitioners have a clear understanding of antidepressant prescribing such as adverse effects and appropriate cessation is paramount [11].
Our aim with this study is to assess the patterns in prescribing AD medication within primary care, with the hope that the trends identified will support the need for greater resource allocation towards a better understanding of AD prescribing activity amongst GPs. Furthermore, we aim to indirectly assess the mental well-being of the Irish population through analysis of AD use.
Methodology
Study design
A study was conducted at two general practice clinics located in the Republic of Ireland, in May 2021 by two medical students in association with the practice teams. This examined AD prescription rates from 2016 to 2020. All data was anonymized to remove any personal information in keeping with General Data Protection Regulations (GDPR). This project involved secondary analysis of this anonymous data. Ethical approval was obtained for this study from the Education and Health Sciences Research Ethics Committee, University of Limerick, 2021_04_10_EHS.
Irish healthcare system
Ireland does not have universal registration with a GP. Almost 45% of the population is registered through the Primary Care Reimbursement Service (PCRS), https://www.hse.ie/eng/staff/pcrs/pcrs-publications/annual-report-2019.pdf, with the remainder being described as private patients and able to see any GP. All adult patients aged over 80 years and those below defined income levels are registered with the PCRS. Those registered with the PCRS have either a ‘doctor visit card’ (which covers hospitalization and primary care visits) or a ‘medical card’ (which covers hospitalization and primary care visits and medication costs).
Study population
The population of interest was medical card holders (MCHs) registered at the chosen Irish general practice clinics who were prescribed antidepressant medication during the time period of 1 January 2016 to 30 December 2020. This population was chosen on the basis that they likely represented a more consistent population with regard to attendance and being registered to the one general practice. The exclusion criteria included any non-medical card holder patient registered at either general practice, ‘walk-in’ patients and any patients under the age of 18 years old. The selection of MCHs maintained patient consistency throughout the study.
Tools
After the study was completed using the practice software SOCRATES®, all data was then transferred to Microsoft Excel spreadsheets and fully anonymized to remove any patient identifiable information.
Study variables
The medications of interest assessed were first-line pharmacological agents utilized in the treatment of depression which included two drug classes selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs): venlafaxine, sertraline, escitalopram and fluoxetine. Outlined below are the study variables assessed:
Total registered medical card holders at general practice
The annual number of medical card holders prescribed antidepressant medication
The annual number of antidepressant prescriptions for medical card holders (including the prescription status initiation vs refill)
Once data extraction was complete, each patient was anonymized through the employment of a random coding sequence in replacement of patient details. During data analysis, the results obtained from each year were amended so that each patient was accounted for only once with either an initiation or refill status. This amendment of data removed the possible anomalies through multiple data entries per patient.
Statistical analysis
Descriptive analysis was employed to analyse the obtained data using Microsoft Excel. This involved analyzing per 100 patients who were prescribed AD medication as well as per 1000 prescriptions which were AD medication both for annual trends. The results were illustrated in both a table and line graph format.
Results
Population
A population of 2611 medical card patients was registered in the year 2016, expanding to a total of 2936 patients.
MCH antidepressant use rates
There has been an annual rise in the number of medical card holders who were prescribed antidepressant medications (Fig. 1). The year 2016 demonstrates a rate of 9.42 per 100 MCH, growing to 12.3 per 100 in 2020, respectively. This equated to a total 5-year increase of 2.88 per 100 patients. Annual growth of medical card holders on antidepressant medications ranged from 0.38 to 1.17 per 100 MCH. The year-to-year growth displayed in Fig. 1 shows a notable increase from the year 2017 onwards, with 2018 to 2019 demonstrating the largest annual increase of 1.06 per 100 MCH prescribed antidepressant medications. Compared to the previous 2 years, 2020 illustrated a reduced annual growth in medical card patients on antidepressant medication at 1.03 per 100 MCH.
Fig. 1.
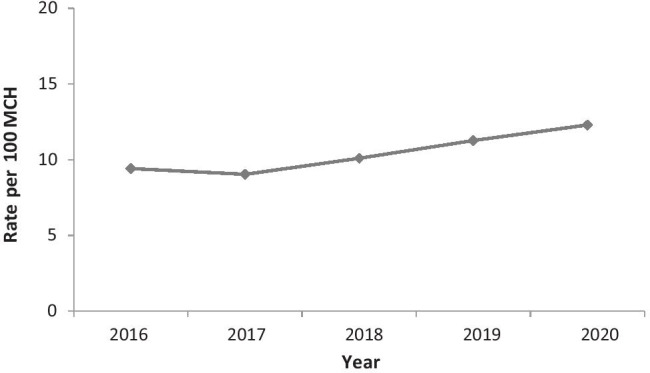
Rate per 100 MCH prescribed antidepressant medication
MCH prescription rates
Figure 2 represents the annual number of antidepressant prescriptions per 1000 total prescriptions of all MCH. The results demonstrate a rate of 4.84 per 1000 MCH prescriptions which were antidepressant medication in 2016. The year 2020 represented the largest proportion of MCH prescriptions which were antidepressants at a rate of 6.32 per 1000 MHC prescriptions. Growth rates in the number of MCH antidepressant prescriptions have been comparable across years, with an average annual rise in prescriptions of 0.37 per 1000 MCH prescriptions. While annual growth differed, there was a similar rate each year, which varied between 0.31 and 0.45 per 1000 MCH prescriptions. The largest annual increase in antidepressant prescriptions per 1000 MCH prescriptions was noted between 2019 and 2020, with a rise of 0.45 per 1000 MCH prescriptions.
Fig. 2.
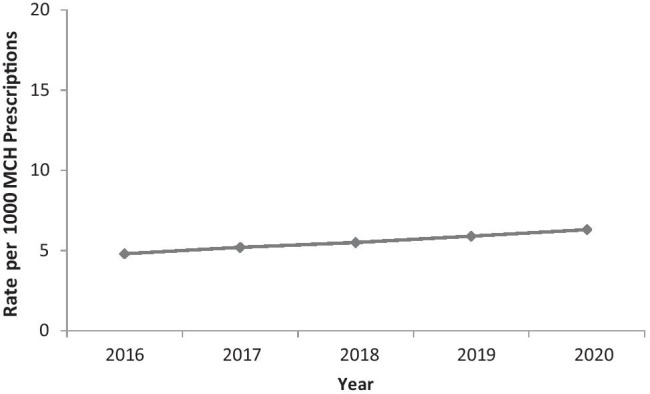
Rate of antidepressant medication prescriptions per 1000 MCH prescriptions
Prescription status
Figure 3 illustrates the annual antidepressant medication dispensing rates per 1000 of MCH total prescriptions, designated as either refill or new initiation. Annual figures show a continual increase in antidepressant refill rates from 4.14 to 5.67 per 1000 MCH prescriptions in 2016 and 2020, respectively. Of the data, the highest proportion of antidepressant medications which were refill scripts occurred in the year 2020, at 5.67 per 1000 MCH prescriptions. Conversely, antidepressant initiation rates varied on a year-to-year basis with a range of 0.6 to 0.83 per 1000 MCH prescriptions. Of the annual rates, 2019 represents the highest rate of antidepressant initiation prescriptions at 0.83 per 1000 MCH prescriptions. The results in Table 1 show that the majority of dispensed antidepressant medications were refill prescriptions, a trend which was similar across each of the 5 years. Despite a larger total number of antidepressant medications being dispensed in the year 2020, data supports decreased rates of antidepressant initiations relative to the previous year of 2019, 0.65 (2020) versus 0.83 (2019) per 1000 MCH prescriptions.
Fig. 3.
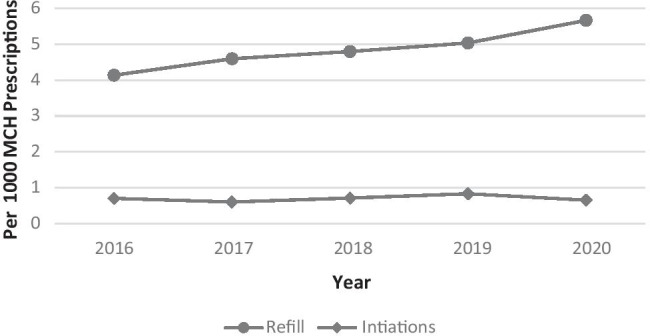
Annual rate of antidepressant prescriptions (refill vs initiations) per 1000 MCH prescriptions
Table 1.
Annual medical card holder antidepressant medication summary data
| Year | Per 100 MCH on AD medication | Per 1000 prescriptions which were AD |
|---|---|---|
| 2016 | 9.42 | 4.84 |
| 2017 | 9.04 | 5.2 |
| 2018 | 10.1 | 5.51 |
| 2019 | 11.27 | 5.87 |
| 2020 | 12.3 | 6.32 |
| Year | Per 1000 prescriptions which were AD refills | Per 1000 prescriptions which were AD initiations |
| 2016 | 4.14 | 0.7 |
| 2017 | 4.6 | 0.6 |
| 2018 | 4.8 | 0.71 |
| 2019 | 5.04 | 0.83 |
| 2020 | 5.67 | 0.65 |
Discussion
Summary of findings
This study examines the use of antidepressant medication amongst the MCH population in the Irish Midlands region. With the aim of assessing prescription patterns within the primary care setting and to potentially detect a lack of appropriate antidepressant medication cessation. This research is novel in that along with analyzing trends in the prescription of AD drugs, we also examined which elements of these prescriptions were refills and which were first-time initiations of drug therapy.
This study found a rise in antidepressant medication over the study time period, 2016 to 2020. The year 2016 noted a rate of 9.42 per 100 MCH’s prescribed antidepressant medication. This figure rose to 12.3 per 100 MCH by the year 2020.
With regard to prescription dispensing rates, in 2016, it was found antidepressant medications represented 4.84 per 1000 of total prescriptions obtained from the MCH population. This figure grew to 6.32 per 1000 MCH prescriptions by the year 2020. Further analysis of prescribing rates displayed a rise in the proportion of antidepressant medications which were refill prescriptions in contrast to initiation prescriptions. Antidepressant refill prescriptions grew from 4.14 to 5.67 per 1000 MCH prescriptions over the 5-year period.
Annual change from 2019 to 2020 illustrated a rise in antidepressant prescription rates during the year 2020, with antidepressants prescriptions increasing from 5.87 to 6.32 per 1000 MCH prescriptions in 2019 and 2020, respectively. In comparison, there was a similar increase in the number of MCH’s prescribed antidepressant medication during the year 2020 relative to previous years.
Irish rates
Figures from the Irish literature have displayed trends of increasing antidepressant use amongst the general public. In particular, there has been a 28% increase in the amount of antidepressant prescriptions dispensed, as well as an 18% rise in patients needing antidepressant medication in general practice from 2012 to 2017 [12]. In keeping with these findings, our data revealed a similar rise in the number of MCH prescribed antidepressant medications during the year 2020 relative to previous years.
Additional data obtained from the Irish Public Care Reimbursement Service (PCRS) reported an escalation in both prescribing frequency and total drug expenditure during 2020 in comparison with 2019. In particular, October 2019 represented a prescribing frequency of 324,381 versus October 2020 344,087 [13]. Equating to a 0.29% increase in the proportion of the total PCRS scheme represented by antidepressant medication. These statistics published by the HSE correlate clearly with our findings, as illustrated above. A UK-based study in Northern Ireland has displayed increased rates of antidepressant prescribing throughout their population aged 16 and over during the years 2011 to 2015 with up to 24.3% of the population on psychotropic drugs over the 5-year period [14].
International rates
Although antidepressant use varies according to region, comparative data can be seen internationally with similar trends depicted in the Irish population. A study conducted by Kantor et al. in the USA outlined a rise in antidepressants prescription rates by 6.8–13% between 1999 and 2012 [15]. Furthermore, Australian data has reported a near doubling in the use of antidepressants from the years 2000 to 2016 [16]. Most recent estimates from over 1000 general practices in Australia reported a steady rise in all types of psychotropic medication prescribing rates in the year 2020.
Our research agrees with the aforementioned global antidepressant trends, as it depicts a 5-year increase in antidepressant use by the Irish medical card population. Rates have continued to increase on an annual basis in the general practice setting amongst this population.
Long-term use
Chronic antidepressant usage has been an increasingly recognized issue in the literature. A recent study conducted in the International Journal of Geriatric Psychiatry illustrated a trend that 6% of older adults are classified as long-term antidepressant users [17]. Research published in the British Medical Journal by Kelly et al. documented reports on Irish general practitioners’ opinions on AD’s. They described being less likely to cease AD medication prescriptions for two subgroups, those with long-term depression and those who were elderly [18].
It seems that a gap exists in the current primary care knowledge, specifically pertaining to the withdrawal effects of these psychotropic medications. In a recent 2019 UK-based survey, only 17% of general practitioners believed in the ability to distinguish withdrawal effects from depression relapse. Moreover, 68% of these doctors desired more training pertaining to the common effects associated with tapering of dosage [19]. As a result, patients were more likely to remain on psychotropic medications for longer durations in fear of relapse [19, 20].
Interestingly, a 2019 study by Read et al. suggested that approximately 65% of patients have never discussed the idea of stopping the use of antidepressant medications. Likewise, 48% of patients did not have their antidepressant medications frequently reviewed with their general practitioner [21]. Furthermore, the literature proposes that while most mental health issues are managed within the general practice setting, there is a need for ongoing communication and frequent review with health care practitioners.
COVID-19 impact
The COVID-19 pandemic has had a profound global impact in a manner that is still not fully elucidated. Recent literature has described detrimental effects on health care services, including restricted access to services and also highlighted the potential exacerbations of mental health conditions [22]. It is therefore imperative to acknowledge the pandemic as a potential reasoning behind the rise in antidepressant rates amongst the Irish population during the years 2019 to 2020.
Our data suggests a rise in long-term antidepressant use, as indicated by increasing refill dispensing rates seen during 2020. This yearly growth trend highlights the potential negative impact of mental well-being amongst the Irish population—which appears to be progressing and subsequently now at the highest figures over the 5-year period. It is plausible that these figures have been influenced by the COVID-19 pandemic. Such a proposal aligns with a recent study by McLoughlin et al. which supports the deleterious effects of COVID-19 on Irish patients with preexisting mental health conditions [23]. In addition, a study by Hyland et al. 2021 sought to quantify rates of depression and general anxiety in the Republic of Ireland as a direct effect of COVID-19. The multi-wave study proposed that both conditions were commonly experienced in the population during the initial COVID-19 outbreak. Of the general population, a reported 27.7% experienced either general anxiety or depression during the first pandemic lockdown [24].
Further considerations must be made regarding access to services, including general practice. An Irish study by Homeniuk and Collins showed a decrease in face-to-face consultation in general practice during the COVID-19 pandemic, with increased rates of telemedicine [25].
International reports also suggested decreased attendance to both urgent and routine medical care facilities [26]. Such findings could potentially explain why rates of new antidepressant initiations were lower in comparison with prior years, whereas refills were highest. Nevertheless, it is difficult to assess the effect of COVID-19 on the most recent annual data. While rates are highest in the present year, there are numerous factors that may influence these results.
Clinical implications
The observed rise in dispensing rates, in conjunction with the rise in the proportion of refills, supports the speculation that antidepressant medication is being utilized on a long-term basis. This highlights a potential pitfall, a lack of appropriate cessation following antidepressant medication use. Long-term antidepressant usage is undoubtedly present amongst the Irish population. Several clinical adverse effects should be addressed following this growing issue to avoid patients unnecessarily subjecting themselves to the pharmaceutical risks. Firstly, it has been noted within a longitudinal analysis study that antidepressant use increases the hazard rate for drugs used for cardiovascular disease (1.59 fold), diabetes (1.30) and cancer (1.50) [27]. Older studies have suggested serious potential risks, antidepressants users were reported to have a 14% higher risk of heart attacks and strokes. In addition to a 33% greater risk of death, according to findings in a meta-analysis of 17 studies that was published in the journal Psychotherapy and Psychosomatics [28].
Furthermore, a lack of understanding surrounding antidepressant prescribing poses a risk of inappropriate prescribing. In particular, if general practitioners are not made aware of withdrawal symptoms and their management, patients may be incorrectly reinitiated on antidepressant medication if withdrawal symptoms are mistaken for a relapse. Surveys of antidepressant users suggest 30–50% have no evidence-based indication to continue, but coming off antidepressants is often difficult due to fears of relapse, withdrawal and a lack of psychological treatments [29].
From the healthcare provider’s perspective, a study in the UK found that only a minority (29%) of general practitioners felt their knowledge about antidepressant medication withdrawal was ‘adequate’. In addition, 68% stated they would like more training in this field of primary care [19]. Furthermore, on an international basis, Australian general practitioners have voiced concern regarding the discontinuation of antidepressant medication, particularly stating the difficulty of the decision and the desire for more support in this area of primary care [30].
In order to combat this dilemma, research has presented several ideas to overcome these issues including the greater promotion of psychological therapies utilization, patient information leaflets on antidepressants cessation and software reminder prompts within general practice to all promote appropriate antidepressant prescribing [18].
Strengths and limitations
The strengths of this study are in the secondary data analysis approach which limits both selection and recall bias. Secondary data reviews allow for patient information to be obtained in a manner that does not alter any outcome. Moreover, the study included a relatively large sample size (n = 2936). Given the nature of this study, a few limitations should be taken into consideration. Only the most common SSRI/SNRI drugs were considered, thus not a comprehensive list of all possible prescribed antidepressant drugs. Also, this study cannot distinguish between those who are prescribed AD drug refills in secondary care clinics as opposed to those who receive AD drug re-fills primary care/general practice (as the GP is identified as the prescriber in both cases in all PCRS data sets).
Furthermore, each general practitioner may adopt a slightly different approach for their guideline in the treatment of depression; consequently, older AD medications such as tricyclic antidepressants (e.g. amitriptyline) may have been employed and are subsequently not included in the collated data. Additionally, the use of SSRI/SNRI medications is not limited to the medical treatment of depression. It is possible that persons may take SSRI/SNRIs for generalized anxiety disorder, or other non-mental health-based conditions (neuropathic pain, fibromyalgia etc.). COVID-19 restrictions during 2021 precluded a larger study, and thus, this study was primarily based in the midlands of Ireland. Lastly, it is difficult to account for confounders that may impact mental health. While COVID-19 may be partially responsible for the changes in the rates of antidepressant prescribing during the year 2020, other factors may have also influenced the results.
Future research
We accept that a sample population including a greater variety of Irish general practice clinics would reflect a more representative sample of antidepressant medication use in Ireland. Furthermore, insight into the demographics of patients requiring antidepressant medication monitoring would be of interest to identify high-risk groups such as gender and age category. Such identification would enable the risk management and screening for long-term depression in these high-risk subgroups.
Recommendations
Findings from this study, in conjunction with recent Irish literature, support the need for further interventions and guidelines surrounding the topic of antidepressant prescribing, including after long-term use. In doing so, it should achieve reduced rates of chronic prescribing and reduce the number of patients subjected to the adverse effects of antidepressant medication unnecessarily [31]. Moreover, the promotion of psychological intervention such as cognitive behavioural therapy may lessen the use of pharmaceutical agents as first-line treatment options for depression-access to this type of support will of course require further investment by the government in psychological services. Greater emphasis on virtual consultations may improve doctor and patient communication to ensure a mutual understanding and agreement regarding antidepressant medication use and necessity. Digital strategies in delivering mental health support appear promising, but barriers regarding access and availability must be addressed [32].
Conclusion
This study has highlighted the rising use of antidepressant medication amongst the Irish medical card holder population from 2016 to 2020, in two general practices in the Irish midlands. Secondly, it has brought to light the growing rates of antidepressant refill dispensing, indicating greater rates of long-term antidepressant use. Taking into consideration these findings, Irish general practitioners will likely benefit from greater resources being invested in mental health to improve both access to non-pharmacological therapies (psychology) and to help disseminate knowledge on deprescribing strategies for AD’s when appropriate.
Acknowledgements
We would like to thank our research supervisor, Dervla Kelly, and Prof. Deirdre McGrath, head of School of Medicine, University of Limerick. In addition, we would like to extend our thanks to Dr. Sean Montague, Dr. Andrew Lavin, and Dr. Jerry O’Flynn for supporting the research.
Author contribution
The idea for this study was proposed by AM. All authors contributed to the development of the concept and design. Data collection: KL and AM. The introduction was written by KL and AM. Methodology: AM, KL and DK. Results: KL and AM. Discussion: AM and KL. Limitations: AM. Tables and figures were created and edited by KL and AM. Original draft preparation: AM and KL. Writing—review and editing: PH, DK, AM and KL. Supervision: DK. All authors commented on the previous versions of the manuscript. All authors read, commented, and approved the final manuscript.
Data availability
Data is available by reasonable request from the authors.
Declarations
Ethics approval
Education and Health Sciences Research Ethics Committee, University of Limerick, 2021_04_10_EHS.
Conflict of interest
The authors declare no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Who.int (2021) Depression [Online]. Available at https://www.who.int/health-topics/depression#tab=tab_1. Accessed 3 Aug 2021
- 2.Mental Health Ireland (2018) Mental health and wellbeing [Online]. Mental Health Ireland. Available at https://www.mentalhealthireland.ie/research/. Accessed 7 Aug 2021
- 3.Schmitter M, Spijker J, Smit F et al (2020) Exercise enhances: Study protocol of a randomized controlled trial on aerobic exercise as depression treatment augmentation. BMC Psychiatry 20(1) [DOI] [PMC free article] [PubMed]
- 4.Who.int (2020) Depression [Online]. Available at https://www.who.int/en/news-room/fact-sheets/detail/depression. Accessed 13 Aug 2021
- 5.NHS Digital (2021) Antidepressants were the area with largest increase in prescription items in 2016 - NHS Digital [Online]. Available at https://digital.nhs.uk/news-and-events/news-archive/2017-news-archive/antidepressants-were-the-area-with-largest-increase-in-prescription-items-in-2016. Accessed 3 Sept 2021
- 6.BMJ (2009) Explaining the rise in antidepressant prescribing: A descriptive study using the general practice research database. 339(Oct23 1):b4361-b4361 [Online]. Available at https://www.bmj.com/content/339/bmj.b3999. Accessed 3 Aug 2021 [DOI] [PMC free article] [PubMed]
- 7.Chang J, Zamparelli A, Nettis M, Pariante C (2021) Antidepressant drugs: Mechanisms of action and side effects [Online]. ResearchGate. Available at https://www.researchgate.net/profile/Maria-Nettis2/publication/350444516_Antidepressant_Drugs_Mechanisms_of_Action_and_Side_Effects/links/606451bda6fdccbfea1aaf53/Antidepressant-Drugs-Mechanisms-of-Action-and-Side-Effects.pdf?origin=publication_detail. Accessed 7 Aug 2021
- 8.Iacobucci G (2019) NICE updates antidepressant guidelines to reflect severity and length of withdrawal symptoms. BMJ 367:l6103 [Online]. Available at https://www.bmj.com/content/367/bmj.l6103.full. Accessed 28 Jul 2021 [DOI] [PubMed]
- 9.Davies J, Read J. A systematic review into the incidence, severity and duration of antidepressant withdrawal effects: Are guidelines evidence-based? Addict Behav. 2019;97:111–121. doi: 10.1016/j.addbeh.2018.08.027. [DOI] [PubMed] [Google Scholar]
- 10.Bosman R, Huijbregts K, Verhaak P et al (2016). Long-term antidepressant use: A qualitative study on perspectives of patients and GPs in primary care. Br J Gen Pract 66(651):e708-e719 [Online]. Available at https://bjgp.org/content/66/651/e708. Accessed 2 Aug 2021 [DOI] [PMC free article] [PubMed]
- 11.Bowers H, Kendrick T, van Ginneken N et al (2021) A digital intervention for primary care practitioners to support antidepressant discontinuation (advisor for health professionals): development study. J Med Intern Res 23(7):e25537 [Online]. Available at https://www.jmir.org/2021/7/e25537. Accessed 5 Aug 2021 [DOI] [PMC free article] [PubMed]
- 12.Health Service Executive (2017) Primary care reimbursement service statistical analysis of claims and payments. Dublin: HSE
- 13.Health Service Executive (2020) Primary care reimbursement service statistical analysis of claims and payments. Dublin: HSE
- 14.Conlan K, McGrath J, Teeling M (2021) Antipsychotic prescribing in GMS paediatric and young adult population in Ireland 2005–2015: Repeated cross-sectional study. Ir J Psychol Med 1–10 [Online].https://pubmed.ncbi.nlm.nih.gov/33745473/ Accessed 12 Aug 2021 [DOI] [PubMed]
- 15.Kantor E, Rehm C, Haas J, Chan A, Giovannucci E (2015) Trends in Prescription Drug Use Among Adults in the United States From 1999-2012. JAMA, [online] 314(17), p.1818. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4752169/ [DOI] [PMC free article] [PubMed]
- 16.Davey C, Chanen A (2016) The unfulfilled promise of the antidepressant medications. Med J Aust 204(9):348–350 [Online]. Available at https://onlinelibrary.wiley.com/doi/abs/10.5694/mja16.00194. Accessed 5 Aug 2021 [DOI] [PubMed]
- 17.O'Neill A, McFarland J, Kelly D. Long-term antidepressant use in a cohort of older people. Int J Geriatr Psychiatry. 2021;36(8):1241–1251. doi: 10.1002/gps.5518. [DOI] [PubMed] [Google Scholar]
- 18.Kelly D, Graffi J, Noonan M et al (2021) Exploration of GP perspectives on deprescribing antidepressants: A qualitative study. BMJ Open 11(4):e046054 [DOI] [PMC free article] [PubMed]
- 19.Read J, Renton J, Harrop C, et al. A survey of UK general practitioners about depression, antidepressants and withdrawal: Implementing the 2019 Public Health England report. Ther Adv Psychopharmacol. 2020;10:204512532095012. doi: 10.1177/2045125320950124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowers H, Williams S, Geraghty A et al (2019) Helping people discontinue long-term antidepressants: Views of health professionals in UK primary care. BMJ Open 9(7):e027837 [DOI] [PMC free article] [PubMed]
- 21.Read J, Gee A, Diggle J, Butler H. Staying on, and coming off, antidepressants: the experiences of 752 UK adults. Addict Behav. 2019;88:82–85. doi: 10.1016/j.addbeh.2018.08.021. [DOI] [PubMed] [Google Scholar]
- 22.Kelly B. Impact of COVID-19 on mental health in Ireland: Evidence to date. Ir Med J. 2020;113(10):214. [Google Scholar]
- 23.McLoughlin J, O’Grady M, Hallahan B (2021) Impact of the COVID-19 pandemic on patients with pre-existing mood disorders. Ir J Psychol Med 1–10 [DOI] [PMC free article] [PubMed]
- 24.Hyland P, Shevlin M, Murphy J et al (2021) A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID-19 pandemic. Psychiatry Res 300:113905 [DOI] [PMC free article] [PubMed]
- 25.Homeniuk R, Collins C (2021) How COVID-19 has affected general practice consultations and income: General practitioner cross-sectional population survey evidence from Ireland. BMJ Open 11(4):e044685 [DOI] [PMC free article] [PubMed]
- 26.Nshimyiryo A, Barnhart D, Cubaka V et al (2021) Barriers and coping mechanisms to accessing healthcare during the COVID-19 lockdown: A cross-sectional survey among patients with chronic diseases in rural Rwanda. BMC Pub Health 21(1) [DOI] [PMC free article] [PubMed]
- 27.Teng A, Taylor Z, Pfeffer J, Williams, L, (2020) Using longitudinal prescription data to examine the incidence of other chronic diseases following antidepressant use. Journal of Psychiatric Research, [online] 125, pp.7-12. Available at: https://pubmed.ncbi.nlm.nih.gov/32171110/ [DOI] [PubMed]
- 28.Petersen A (2019) New concerns emerge about long-term antidepressant use [Ebook]. Anxiety & Depression Association of America, pp 1–6. Available at https://adaa.org/sites/default/files/New%20Concerns%20Emerge%20About%20Long-Term%20Antidepressant%20Use.pdf. Accessed 9 Aug 2021
- 29.Kendrick T. Strategies to reduce use of antidepressants. Br J Clin Pharmacol. 2020;87(1):23–33. doi: 10.1111/bcp.14475. [DOI] [PubMed] [Google Scholar]
- 30.Donald M, Partanen R, Sharman L, et al. Long-term antidepressant use in general practice: A qualitative study of GPs’ views on discontinuation. Br J Gen Pract. 2021;71(708):e508–e516. doi: 10.3399/BJGP.2020.0913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walsh, M. and Duffy, I (2018) A Descriptive Study of Antidepressant Prescribing In a Semi-Rural Practice. Irish Medical Journal, 111(5), p.75 [PubMed]
- 32.Bäuerle A, Graf J, Jansen C, et al. An e-mental health intervention to support burdened people in times of the COVID-19 pandemic: CoPE It. J Public Health. 2020;42(3):647–648. doi: 10.1093/pubmed/fdaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available by reasonable request from the authors.


