Abstract
Purpose
During coronavirus disease-19 (COVID-19) pandemic, hospitals faced challenges which were different than previous years. The purpose this study was to report frequency of firearm injuries (FI) to head and neck during the COVID-19 pandemic.
Materials and Methods
This cross-sectional study reviewed patients in the Trauma Registry at Grady Memorial Hospital (GMH) in Atlanta, GA. Patients were included if they sustained FI to head and neck, were listed in TR, and were treated at GMH. Patients were stratified according to date of injury into 1) before COVID-19 pandemic, (BC19) or 2) during initial 5 months of COVID-19 pandemic, (C19). Variables were patient demographics, illegal substance use, etiology, place of injury, distressed communities index, location of injury, Glasgow Coma scale on arrival, cardiopulmonary resuscitation in Emergency Department (ED), shock on admission, disposition from ED, length of stay, days on mechanical ventilation and discharge status. Descriptive, univariate, and bivariate analysis were completed. Chi square test was used for categorical variables. Statistical significance was P < .05.
Results
There were 215 patients who met inclusion criteria. There were 96 patients (78 males) with a mean age of 31.5 years old during BC19. There were 119 patients (101 males) with a mean age 32.7 years old during C19. There was a 10.4% increase in FI to head and neck during COVID-19. Our data showed that alcohol use was associated with FI during C19 (P≤ .0001). FI to base of skull occurred 34.5% more often during C19 (P = .002). Cranial injuries occurred 26% more often during BC19 (P = .03). During BC19, 85.4% of the patients arrived alive to GMH, but only 16% arrived alive during C19 (P ≤ .0001).
Conclusions
There were more FI to head and neck during COVID-10 pandemic than during the previous time period.
The coronavirus disease-19 (COVID-19) was declared a global pandemic in March 2020 by the World Health Organization.1 Almost immediately, local and national governments mandated to “stay at home” for the majority of the population. Rates of unemployment increased.2 This new social situation introduced anxiety, depression, distress, and fear.3 Concurrently, the Federal Bureau of Investigation (FBI) reported that significantly more firearms were sold in March 2020 than in previous months4 resulting in an increase in access to firearms. This increase in access coupled with stress, anxiety, and mental illnesses, lead to an increase in firearm injuries (FI).5
COVID-19 added to an already existing problem of mortality from firearms which ranks among the leading causes of death in the United States (US).6 Firearm-related injuries and/or deaths result in over $48 billion in medical expenses.7
Data on the impact of COVID-19 on FI is sparse. Specifically, there is a paucity of literature regarding the incidence of FI to head and neck during the COVID-19 pandemic nationally or regionally. The purpose of this study was to measure changes in the frequency of FI injuries during the pandemic. We hypothesized that frequency of FI to head and neck increased during the pandemic. The specific aims were to compare the frequency, demographics, and injury severity before and during the initial months of the pandemic.
Materials and Methods
STUDY DESIGN AND SAMPLE
This retrospective cohort study (Institutional Review Board #00000432) reviewed patients in the Trauma Registry (TR) at Grady Memorial Hospital (GMH) in Atlanta, GA. Study included patients who: 1) sustained FI to head and neck, 2) were included in TR as per American College of Surgeons guidelines,8 and 3) were treated at GMH. Patients were stratified according to date of injury indicated 2 groups: 1) March 13 to August 13, 2019 (ie, before COVID-19 pandemic, [BC19]) or 2) March 13 to August 13, 2020 (ie, during initial 5 months of COVID-19 pandemic, [C19]). March 13 was chosen because COVID-19 was announced as a national emergency on that date. This method of stratification was previously described by our group.9
VARIABLES
The primary predictor variable was time: before and during COVID-19 pandemic. The primary outcome variable was FI to head and neck. The research team collected patient-related variables: 1) demographics (age, gender, race, insurance status [none/self-pay, commercial, government-subsidized]), 2) substance use (alcohol and/or illicit drug/s), 3) etiology (assault or self-inflicted), 4) place of injury (home, public building, street, unknown location), and 5) patient's distressed communities index (DCI). Variables regarding distribution of FI were: 1) isolated soft tissue (face), boney (cranial bones [ie, frontal, parietal, orbit], base of skull [ie, occipital, sphenoid, temporal, maxilla, zygomaticomaxillary complex, nose/naso-orbito-ethmoid, mandible]), intraoral injuries, and/or neck, and 2) other locations of injuries (lower and/or upper limb, abdomen, chest, pelvic). Severity of injury was described using the following variables: 1) Glasgow Coma scale (1-15) on arrival to GMH, 2) cardiopulmonary resuscitation in the Emergency Department (ED), 3) diagnosis of shock on admission (ie, systolic blood pressure <90 mm Hg10), 4) disposition from ED (intensive care unit [ICU], floor/step down unit, operating room, morgue), 5) ICU length of stay (LOS), 6) total days on mechanical ventilation (MV), 7) hospital LOS, and 8) discharge status (alive, expired).
DISTRESSED COMMUNITIES INDEX
The DCI was previously used to evaluate the impact of a community's socioeconomic status and the effect of health disparities on surgical procedure outcome.10 , 11 It was developed by the Economic Innovation Group.12 DCI exists for all zoning improvement plans (zip codes) in the United States (US) in which more than 500 people reside (ie, 99% of US population). DCI is a composite score based on the following metrics: 1) no high school degree, 2) housing vacancy rate, 3) adults not working, 4) poverty rate, 5) median income ratio, 6) change in employment, and 7) change in business establishments.10, 11, 12 Metrics are then averaged and converted to percentiles. DCI ranges between 0 (ie, no distress) to 100 (ie, severe distress).10 , 13 DCI over 80 indicates distress; DCI below 20 indicates prosperity.14 The research team used DCI to describe the sample's well-being or distress.
DATA ANALYSIS
Data was de-identified and recorded in a standardized collection form. Data was analyzed using IBM SPSS Statistical software for Windows (version 26; IBM; Armonk, NY). Descriptive statistics were performed. Univariate and bivariate analysis were calculated. Chi-square test was used for categorical variables. Statistical significance was P < .05.
Results
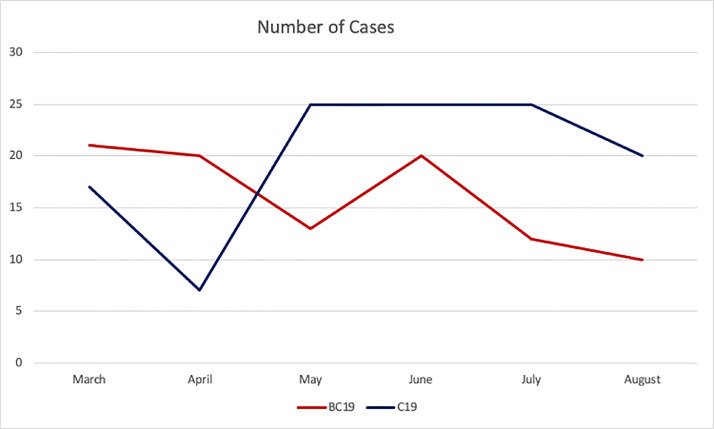
During the study period, 948 patients sustained FI. Of them, 215 patients had FI to head and neck and met inclusion criteria. There were 96 patients (78 males) with a mean age of 31.5 years old (range, 7 to 82) who sustained FI before the pandemic (ie, BC19 group). There were 119 patients (101 males) with an average age of 32.7 years old (range, 14 to 82) during the first 5 months of pandemic (ie, C19 group). Our data showed an initial decrease in number of FI to head and neck cases during March and April. During the rest of study period, there was an increase in the number of cases. Overall, there was a 10.4% increase in the incidence of FI to the head and neck during the first 5 months of the COVID-19 pandemic (Fig 1 ).
FIGURE 1.
Incidence of firearm injuries to head and neck per month before COVID-19 (BC19) and during COVID-19 (C19).
The majority of patients in both groups were Black (BC19: n = 80, 83.3%; C19: n = 96, 80.7%) and/or uninsured/self-pay (BC19: n = 57, 59.4%; C19: n = 83, 69.7%). The most common etiology of FI in both groups was assault (BC19: n = 81, 84.4%; C19: n = 102, 85.7%). Most FI occurred at the victim's home (BC19: n = 40, 41.7%; C19: n = 37, 31.1%).
Substance use was alcohol (BC19: n = 31, 32.3%; C19: n = 5, 4.2%) and/or illicit drugs (BC19: n = 13, 13.5%; C19: n = 96, 80.7%). Alcohol use had a statistically significant difference between the 2 cohorts (P ≤ .0001). There was no statistical difference in demographics, etiology, and place of injury between the 2 cohorts (Table 1 ).
Table 1.
Demographic Data
| Variables | Before COVID-19 (BC19) n, (%) | COVID-19 (C19) n, (%) | P Value |
|---|---|---|---|
| 96 | 119 | ||
| Age, mean (yr), (range) | 31.5 (7-82) | 32.7 (14-82) | .55 |
| Gender | .48 | ||
| Male | 78 (81.3) | 101 (84.9) | |
| Female | 18 (18.8) | 18 (15.1) | |
| Racial distribution | .79 | ||
| Black | 80 (83.3) | 96 (80.7) | |
| White | 10 (10.4) | 16 (13.4) | |
| Other | 6 (6.3) | 7 (5.9) | |
| Insurance status | .13 | ||
| Uninsured/self-pay | 57 (59.4) | 83 (69.7) | |
| Commercial | 15 (15.6) | 19 (16) | |
| Government subsidized | 24 (25) | 17 (14.3) | |
| Substance Abuse | |||
| Alcohol | 31 (32.3) | 5 (4.2) | <.0001* |
| Illegal substance | 13 (13.5) | 19 (16) | .58 |
| Etiology | .49 | ||
| Assault | 81 (84.4) | 102 (85.7) | |
| Self-inflicted | 15 (15.6) | 15 (12.6) | |
| Place of injury | .4 | ||
| Home | 40 (41.7) | 37 (31.1) | |
| Public Building | 11 (11.5) | 13 (10.9) | |
| Street | 22 (22.9) | 32 (26.9) | |
| Unknown location | 23 (24) | 37 (31.1) | |
| DCI, mean, (range), % | 71 (3.7-98) | 64.6 (3.7-99.7) | .07 |
Abbreviation: DCI, Distressed communities index.
Statistical significance (P .05).
During BC19, DCI was 71 (range, 3.7 to 98). During C19, DCI was 64.6 (range, 3.7 to 99.7) (Table 1). The mean DCI during the pandemic was 6.4% lower than before the pandemic. This value did not have statistical significance, but there was a trend towards significance (P = .07).
Table 2 summarizes the distribution of FI. During BC19, the most common FI was isolated soft tissue injuries to the face (n = 26, 27%), followed by cranial bones injuries (n = 25, 26%). During C19, the most common FI was isolated soft tissue injuries to face (n = 37, 37.1%), followed by base of skull injuries (n = 41, 34.5%). Our data showed that there were statistically more base of skull injuries during C19 (P = .001). In contrast, there were more cranial bone injuries during BC19 (P= .03) (Table 2). Most common extracranial locations were upper limb (BC19: n = 27, 28.1%; C19: n = 31, 26.1%), chest (BC19: n = 27, 28.1%; C19: n = 21, 17.6 %), and lower limbs (BC19: n = 19, 19.8%; C19: n = 20, 16.8%).
Table 2.
Distribution of Firearm Injuries to Head and Neck
| Before COVID-19 (BC19)n (%) | COVID-19 (C19) n (%) | P Value | |
|---|---|---|---|
| Isolated soft tissue injuries | |||
| Face | 26 (27) | 37 (37.1) | .3 |
| Boney injuries | |||
| Maxilla | 5 (5.2) | 6 (5) | >.99 |
| Mandible | 12 (12.5) | 14 (11.8) | .87 |
| ZMC | 0 | 2 (1.7) | .5 |
| Nose/NOE | 3 (3.1) | 1 (0.8) | .33 |
| Orbit | 6 (6.3) | 13 (10.9) | .24 |
| Base of skull | 14 (14.6) | 41 (34.5) | .001* |
| Cranial | 25(26) | 17(14.3) | .03* |
| Intraoral injuries | 1(1) | 2 (1.7) | >.99 |
| Neck | 21 (21.9) | 24 (20.2) | .76 |
| Other location/s | |||
| Upper limb | 27 (28.1) | 31 (26.1) | .73 |
| Chest | 27 (28.1) | 21 (17.6) | .07 |
| Lower limb | 19 (19.8) | 20 (16.8) | .57 |
| Pelvic | 8 (8.3) | 16 (13.4) | .24 |
| Abdomen | 9 (9.4) | 14 (11.8) | .57 |
Abbreviations: NOE, naso-orbito-ethmoid; ZMC, zygomaticomaxillary complex.
Statistical significance (P .05).
Table 3 consists of details regarding severity of FI. Regarding the specific variables which were investigated to summarize the severity of FI (ie, Glasgow Coma scale, cardiopulmonary resuscitation in ED, shock on admission, disposition form ED, ICU/hospital LOS, days on MV, discharge status), our data showed that there was no statistical difference in severity of FI between the 2 cohorts (Table 3).
Table 3.
Severity of Firearm Injuries
| Before COVID-19 (BC19)n (%) | COVID-19 (C19)n (%) | P Value | |
|---|---|---|---|
| GCS mean, (range) | 10.6 (3-15) | 10.6 (3-15) | >.99 |
| CPR in ED | 2 (2.1) | 5 (4.2) | .47 |
| Shock on admission* | 22 (22.9) | 24 (20.2) | .65 |
| Disposition from ED | .75 | ||
| OR | 35 (36.5) | 40 (33.6) | .66 |
| ICU | 18 (18.8) | 31 (26.1) | .21 |
| Morgue | 19 (19.8) | 24 (20.2) | .95 |
| Floor/Step down | 17 (17.7) | 17 (14.3) | .49 |
| Home | 7 (7.3) | 7 (5.9) | .68 |
| ICU LOS mean (days), (range) | 9.4 (1-71) | 6.9 (1-36) | .25 |
| Days on MV mean, (range) | 7.8 (1-70) | 4.9 (0-29) | .22 |
| Hospital LOS mean (days), (range) | 11.4 (1-136) | 7.9 (1-48) | .16 |
| Discharge Status | .84 | ||
| Alive | 69 (71.9) | 87 (73.1) | |
| Expired | 27 (28.1) | 32 (26.9) |
Abbreviations: CPR, cardiopulmonary resuscitation; ED, emergency department; GCS, Glasgow Coma scale; ICU, intensive care unit; LOS, length of stay; MV, mechanical ventilator; SBP, systolic blood pressure; SD, standard deviation.
Shock on admission is defined as SBP <90 mm Hg.8
Discussion
The purpose of this study was to measure changes in the frequency of FI injuries during the pandemic. Our hypothesis was that the incidence of FI to head and neck increased during the pandemic. The specific aims were to compare the frequency, demographics, and injury severity before and during the initial 5 months of the pandemic. To our knowledge, this is the first descriptive analysis of FI to head and neck during the COVID-19 pandemic.
Our data showed a transient decrease in FI injuries to head and neck during first 2 months of C19. This initial decrease in FI cases parallels the declaration of COVID-19 outbreak as a pandemic.1 Gradually, the number of cases reached a 10.4% increase and surpassed the period BC19. During the same period, the Federal Bureau of Investigation (FBI) reports indicated an increase in purchases of firearms. As the pandemic progressed, the number of FI to head and neck increased. An increase in stress, depression, and anxiety secondary to COVID-induced lifestyle,3 high unemployment rates,15 , 16 and easier access to firearms created an ideal setting for this increase in FI. Specifically, the US government issued shelter-in-place orders in order to decrease transmission of COVID-19 and potentially overwhelming health care systems.17 , 18 Organizations and institutions encouraged their employees to work remotely, 19 , 20 but schools and childcare facilities closed.21 Therefore, people worked from home and provided childcare concomitantly, which increased stress levels.22 Restaurants, gyms, and various entertainment venues closed23 , 24; people did not have an outlet to relieve stress and anxiety.25 Physical contact with family and friends was limited26; individuals who used social interactions and physical touch to restore calmness were not able to do so because of the risk of transmission.26 As a result, the COVID-19 pandemic created levels of stress, anxiety, and social isolation that communities have never experienced.27 Furthermore, despite a higher rate of burnout, an outlet for stress did not exist.28
Concomitantly, the pandemic introduced a sudden economic recession with progressing economic hardship and an increase in unemployment.29 Specifically, by May 2020, 20 million Americans lost their jobs and became unemployed.30 This unemployment created unrest and fear; citizens felt a need for self – preservation,31 , 32 which occasionally manifested as purchasing firearms. The FBI reported that over 700,000 additional firearms were sold than in previous months.4 , 33 This amount represents over 120,000 firearms per day in March 2020.4
Social isolation, anxiety, fear of contagion, uncertainty, chronic stress, and economic difficulties have been shown to lead to the development or exacerbation of psychiatric disorders (ie, depression, anxiety, substance use).3 A positive correlation between access to firearms, stress, anxiety, mental illnesses, and FI was previously discussed.5 A recent study reported a positive correlation between unemployment and the increase in firearm violence.31 , 32 Our finding is consistent with these reports which showed an increase in total FI during the COVID-19 pandemic.16 , 31 , 32 , 34 Similar to our results, studies stated that access to firearms, burnout from the new lifestyle, an increase in stress, depression, and anxiety lead to additional FI.3 , 30
The DCI during the COVID-19 pandemic decreased by 6.4%. This decrease indicates that the overall distress is decreased in this cohort. Our data showed that the decrease is trending toward significance, which indicates that a larger sample size would potentially show a statistical significance. Overall, there is no consensus regarding the decrease in community distress during C19. This is the subject of an ongoing investigation at our institution.
Our data showed an increase in base of skull FI. The study team separated FI into specific locations such as base of skull, facial bone, and intraoral sites. This separation was important because assault typically causes base of skull injuries35 but self-inflected injuries cause orbital/ocular injuries.35 A FI to base of skull is typically fatal since the damage extends locally to cause significant brain damage.35 However, in our cohort, patients who sustained FI to base of skull did not present with similar devastating injuries.
Although there was an increase in incidence of FI to head and neck, LOS (in hospital and in ICU) and days on MV were shorter during the COVID-19 pandemic. The authors contribute this finding to the unprecedented bed demands during the pandemic.36 It is possible that inpatient teams made intentional efforts to hasten discharges in anticipation of need for beds for patients with COVID. Hospitals were required to adjust resources to keep ICU units available for the expected increase in COVID-19 admissions.13
Finally, a hidden consequence of the COVID-19 pandemic is its impact on trauma quality initiatives (ie, updating TR).37 There was a large increase in the need for direct patient care during the initial stages of the pandemic. Therefore, some staff who were assigned to TR were deployed from their routine roles of abstracting charts to direct patient care.37 In our study, this likely decreased the speed by which data was available in TR.
This study had a few limitations. First, this study relied on a large data set (ie, institutional TR) which had some missing and incomplete information. In addition, it is possible that our data underestimates the true incidence of FI to the head and neck because this TR only included hospitalized patients. Patients who sustained minor injuries from FI were likely not admitted to hospital and thus were not included. Lastly, our data only represents the initial 5 months of the pandemic. As the pandemic continues, epidemiology of FI may change.
In conclusion, FI increased during the COVID-19 pandemic in comparison to its historic cohort.
Our data showed that FIs to head and neck continued to be a public health concern during the COVID-19 pandemic.
Press Release
This article's Press Release can be found, in the online version, at http://dx.doi.org/10.1016/j.joms.2021.06.034.
Footnotes
Accepted for abstract presentation during 103 AAOMS Annual Meeting on September 27 to October 2, 2021 in Nashville, TN.
Conflict of Interest Disclosures: None of the authors have any relevant financial relationship(s) with a commercial interest.
References
- 1.World Health Organization (WHO), WHO announces COVID-19 outbreak a pandemic. Available at:http://www.euro.who.int/en/health-topics/healthemergencies/coronavirus-covid-19/news/news/2020/3/whoannounces-covid-19-outbreak-a-pandemic. Accessed August 17, 2021.
- 2.U.S. Bureau of Labor and Statistics. Employment recovery in the wake of the COVID-19 pandemic. Available at: https://www.bls.gov/opub/mlr/2020/article/employment-recovery.htm. Accessed August 17, 2021.
- 3.Sher L. The impact of the COVID-19 pandemic on suicide rates. Qjm. 2020;113(10):707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Instant Criminal Background Check System (NICS). NICS firearm checks: month/year. Available at: https://www.fbi.gov/file-repository/nics_firearm_checks_-_month_year.pdf/view. Accessed August 17, 2021.
- 5.Swanson JW, McGinty EE, Fazel S, Mays VM. Mental illness and reduction of gun violence and suicide: bringing epidemiologic research to policy. Ann Epidemiol. 2015;25(5):366–376. doi: 10.1016/j.annepidem.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention. Leading causes of death by age group. Available at:https://www.cdc.gov/injury/images/lccharts/leading_causes_of_death_by_age_group_2017_1100w850h.jpg. Accessed August 17, 2021.
- 7.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med. 2015;79:5–14. doi: 10.1016/j.ypmed.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Surgeons. Resources for optimal care of the injured patient. Available at: https://www.facs.org/-/media/files/quality-programs/trauma/vrc-resources/resources-for-optimal-care.ashx. Accessed August 17, 2021.
- 9.Amin D, Manhan AJ, Abramowicz S, Mittal R. Profile Of Head And Neck Burns During COVID-19 Pandemic. J Burn Care Res. 2021 Jul 23:irab135. https://www.doi:org/10.1093/jbcr/irab135. Epub ahead of print. PMID: 34297091. [DOI] [PubMed]
- 10.Mehaffey JH, Hawkins RB, Charles EJ, et al. Socioeconomic “distressed communities index” improves surgical risk-adjustment. Ann Surg. 2020;271(3):470–474. doi: 10.1097/SLA.0000000000002997. [DOI] [PubMed] [Google Scholar]
- 11.Charles EJ, Johnston LE, Herbert MA, et al. Impact of medicaid expansion on cardiac surgery volume and outcomes. Ann Thorac Surg. 2017;104(4):1251–1258. doi: 10.1016/j.athoracsur.2017.03.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Economic Innovation Group. Distress communities index. Available at: https://eig.org/dci/interactive-map. Accessed August 17, 2021.
- 13.Sherman WF, Khadra HS, Kale NN, Wu VJ, Gladden PB, Lee OC. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin Orthop Relat Res. 2021;479:266–275. doi: 10.1097/CORR.0000000000001484. PMID: 32969846; PMCID: PMC7899709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Economic Innovation Group. The 2016 distressed communities index. Available at: 2016-Distressed-Communities-Index-Report.pdf. Accessed August 17, 2021.
- 15.Madan AK, Sapozhnik J, Tillou A, Raafat A, McSwain NE. Unemployment rates and trauma admissions. World J Surg. 2007;31(10):1930–1933. doi: 10.1007/s00268-007-9190-4. [DOI] [PubMed] [Google Scholar]
- 16.Kim D-Y, Phillips SW. When COVID-19 and guns meet: a rise in shootings. J Crim Justice. 2021;73 doi: 10.1016/j.jcrimjus.2021.101783. 101783-101783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The White House. Available at: https://www.whitehouse.gov/priorities/covid-19/. Accessed August 17, 2021.
- 18.Center for Disease Control and Prevention. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6935a2.htm. Accessed August 17, 2021.
- 19.Xiao Y, Becerik-Gerber B, Lucas G, Roll SC. Impacts of working from home during COVID-19 pandemic on physical and mental well-being of office workstation users. J Occup Environ Med. 2021;63(3):181–190. doi: 10.1097/JOM.0000000000002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bouziri H, Smith DRM, Descatha A, Dab W, Jean K. Working from home in the time of COVID-19: how to best preserve occupational health? Occup Environ Med. 2020;77(7):509–510. doi: 10.1136/oemed-2020-106599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poulain T, Meigen C, Sobek C, et al. Loss of childcare and classroom teaching during the Covid-19-related lockdown in spring 2020: a longitudinal study on consequences on leisure behavior and schoolwork at home. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0247949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown SM, Doom JR, Lechuga-Peña S, Watamura SE, Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. 2020;110(Pt 2) doi: 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blocken B, van Druenen T, van Hooff T, Verstappen PA, Marchal T, Marr LC. Can indoor sports centers be allowed to re-open during the COVID-19 pandemic based on a certificate of equivalence? Build Environ. 2020;180 doi: 10.1016/j.buildenv.2020.107022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher KA, Tenforde MW, Feldstein LR, et al. Community and close contact exposures associated with COVID-19 among symptomatic adults ≥18 years in 11 outpatient health care facilities - United States, July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1258–1264. doi: 10.15585/mmwr.mm6936a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hiremath P, Suhas Kowshik CS, Manjunath M, Shettar M. COVID 19: impact of lock-down on mental health and tips to overcome. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. 2020;32(10):1217–1220. doi: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 28.Lippi G, Sanchis-Gomar F, Henry BM. Coronavirus disease 2019 (COVID-19): the portrait of a perfect storm. Ann Transl Med. 2020;8(7):497. doi: 10.21037/atm.2020.03.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shehzad K, Xiaoxing L, Bilgili F, Koçak E. COVID-19 and spillover effect of global economic crisis on the United States' financial stability. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.632175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalesan B, Galea S. Patterns of gun deaths across US counties 1999-2013. Ann Epidemiol. 2017;27(5):302–307.e303. doi: 10.1016/j.annepidem.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Tsouvelas G, Konstantakopoulos G, Vakirtzis A, Giotakos O, Papaslanis T, Kontaxakis V. Criminality in Greece during the years of financial crisis: 2008-2014. Psychiatriki. 2018;29(1):19–24. doi: 10.22365/jpsych.2018.291.19. [DOI] [PubMed] [Google Scholar]
- 33.Caputi TL, Ayers JW, Dredze M, Suplina N, Burd-Sharps S. Collateral crises of gun preparation and the COVID-19 pandemic: infodemiology study. JMIR Public Health Surveill. 2020;6(2):e19369. doi: 10.2196/19369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sutherland M, McKenney M, Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med. 2021;39:225–226. doi: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reddy AK, Baker MS, Sobel RK, Whelan DA, Carter KD, Allen RC. Survivors of self-inflicted gunshot wounds to the head: characterization of ocular injuries and health care costs. JAMA Ophthalmol. 2014;132(6):730–736. doi: 10.1001/jamaophthalmol.2013.8201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rees EM, Nightingale ES, Jafari Y, et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Medicine. 2020;18(1):270. doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haut ER, Leeds I, Livingston DH. The effect on trauma care secondary to the COVID-19 pandemic: collateral damage from diversion of resources. Ann Surg. 2020;272(3):e204–e207. doi: 10.1097/SLA.0000000000004105. [DOI] [PMC free article] [PubMed] [Google Scholar]