Abstract
Since the emergence of the coronavirus disease 2019 (COVID-19) pandemic, multiple but rare complications of this infection have been described, comprising cerebral venous sinus thrombosis (CVST) and immune thrombocytopenic purpura (ITP). Although these two complications have been reported as separate entities, to the best of our knowledge, their concurrent presentation has not been reported. In this case report, we present a middle-aged man with a history of COVID-19 infection who developed a sudden-onset severe occipital headache followed by right-sided blindness (right homonymous hemianopia). Upon his diagnostic workup, brain computed tomography scan with and without contrast was indicative of thrombosis of the left transverse venous sinus and hemorrhagic venous infarction. In addition, laboratory data revealed thrombocytopenia, which upon investigation confirmed a diagnosis of ITP. We postulate three pathophysiological mechanisms for this circumstance: either COVID-19 infection caused ITP and then ITP gave rise to CVST, or COVID-19 complications themselves resulted in ITP and CVST independently and simultaneously, or another plausible mechanism is immune-mediated thrombocytopenia caused by the anti-platelet 4-factor antibody, which is the proposed mechanism for CVST after the COVID-19 vaccine.
Keywords: COVID-19, SARS-CoV-2, Corona virus, Cerebral venous sinus thrombosis, Immune thrombocytopenic purpura, Intracranial complication, ITP, CVST
Key Summary Points
| Cerebral venous sinus thrombosis (CVST) and immune thrombocytopenic purpura (ITP) are known as rare complications of SARS-CoV-2 infection, but their simultaneous development in a patient with a history of COVID-19 has not been reported. |
| The pathophysiology of CVST occurrence in COVID-19 is similar to that of other arterial and venous thrombosis that occurs in patients with COVID-19, and encompasses systemic inflammation and cytokine storm, direct immune-mediated post-infection mechanism, and virus-induced angiitis. |
| ITP in the context of COVID-19 should be considered after ruling out other possible underlying causes of thrombocytopenia, including hemophagocytic lymphohistiocytosis (HLH), thrombotic thrombocytopenic purpura (TTP), sepsis, heparin-induced thrombocytopenia (HIT), and drug-induced thrombocytopenia. |
| In this study, we suggest three possible pathophysiological mechanisms which justify the development of CVST and ITP in a patient at the same time: (1) COVID-19 infection caused ITP and then ITP itself gave rise to CVST by its paradoxical tendency for thrombosis; (2) COVID-19 infection caused both ITP and CVST independently and simultaneously; or (3) immune-mediated thrombocytopenia was caused by the anti-platelet 4-factor antibody, which is the proposed mechanism for CVST after the COVID-19 vaccine. |
Introduction
Since the onset of the coronavirus disease 2019 (COVID-19) pandemic, various manifestations ranging from asymptomatic or mild upper respiratory tract infection to severe pneumonia and subsequent multi-organ failure have been observed [1, 2]. Besides these typical presentations, rare and atypical complications of this infection have been reported, and among those serious complications are cerebral venous sinus thrombosis (CVST) and immune thrombocytopenic purpura (ITP). It has been reported that the incidence of CVST is 0.02% in patients with laboratory-confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [3]. Additionally, ITP is an infrequent complication of COVID-19 infection [4]. Although these two rare conditions are known to occur separately in the context of COVID-19 infection, herein we report a case of COVID-19 infection complicated by both CVST and ITP during the same course and then discuss the possible mechanisms which justify these two phenomena simultaneously.
No identifiable data were disclosed in this article; however, written consent was obtained from the patient.
Case Presentation
A 47-year-old man with a past medical history of diabetes mellitus presented to the emergency department of the hospital with an abrupt-onset severe headache and right-sided blindness. On the day before admission, he had experienced a headache more prominent at his occiput, which he called the worst headache he had ever had, and gave it a pain score of 10/10. Shortly after his headache, right-sided blindness occurred. There was a history of COVID-19 infection 20 days earlier, confirmed by a reverse transcription polymerase chain reaction (RT-PCR) test, with pulmonary symptoms which led to intensive care unit admission for 3 days. He did not receive any type of COVID-19 vaccine prior to his admission. During the physical examination, he was drowsy but oriented to person, place, and time. He had a blood pressure of 170/100 mmHg. Dysarthric speech, right homonymous hemianopia, and alexia without agraphia were noticeable. Other neurologic examinations were unremarkable. Systemic examinations were normal, and there was no evidence of petechiae or purpura. Brain computed tomography scan revealed an intraparenchymal hemorrhage with considerable edema surrounding it in the left occipital lobe, along with a string (or cord) sign suggesting thrombus or stagnation in the left transverse sinus (Fig. 1). A diagnosis of hemorrhagic venous infarction due to transverse sinus thrombosis was presumed. Unfortunately, vascular imaging for venous sinus thrombosis was not available at that time. In the initial laboratory data, a D-dimer level of 1030 was measured, which was not repeated in his admission course. In addition, a platelet count of 20,000 was notable, while platelet count in the recent admission at the time of discharge was 150,000, and the patient had not received any medication apart from his diabetic drug regimen until this current admission. To investigate the etiology of thrombocytopenia, a peripheral blood smear (PBS) was prepared, which revealed giant platelets without any evidence of schistocytes (Fig. 2). COVID-19 RT-PCR, hepatitis C virus (HCV), hepatitis B virus (HBV), and human immunodeficiency virus (HIV) antibody results were negative. The patient received 10 units of platelets and dexamethasone 8 mg three times a day, and his platelet count increased temporarily to 49,000. Bone marrow aspiration and biopsy demonstrated hypolobulated megakaryocytes (Fig. 3). The patient was started on intravenous immunoglobulin (IVIG) 20 g for 5 days, and thrombocytopenia responded dramatically after 2 days and platelet count increased to 115,000. Given the exclusion of the other possible causes of thrombocytopenia, PBS and bone marrow finding, and finally, a remarkable response to treatment with corticosteroids and IVIG, a diagnosis of ITP was considered. He was discharged 8 days after admission in stable condition. At 1-month follow-up, on prednisolone 25 mg twice daily, the platelet count was 140,000 and neurological symptoms including homonymous hemianopia were improved substantially, although he reported some difficulties in reading (Fig. 4).
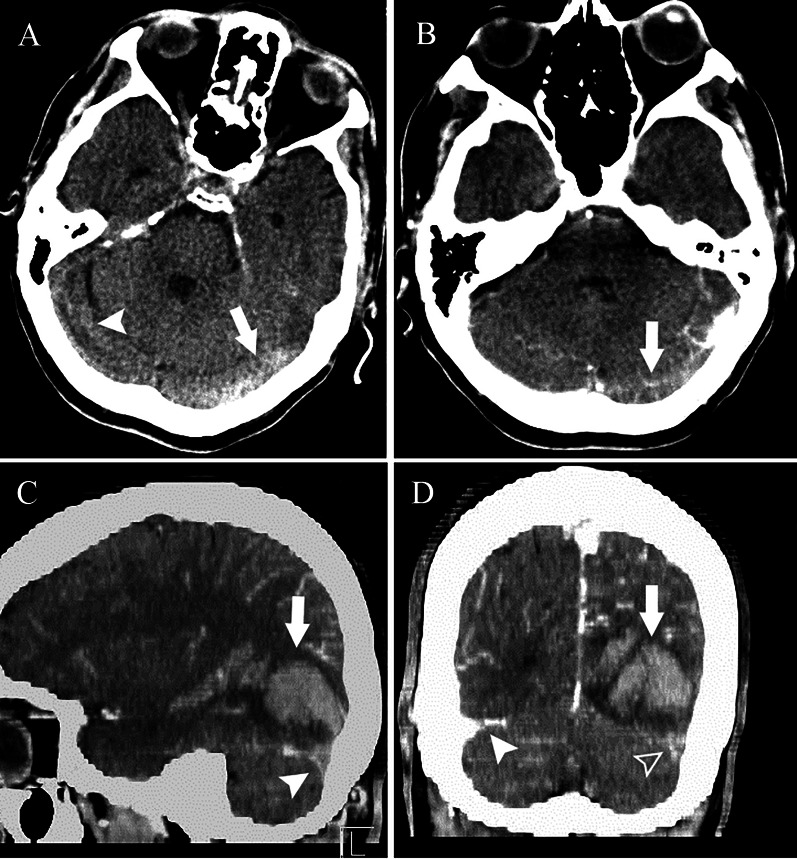
Fig. 1.
Brain computed tomography (BCT) of the patient. a Axial BCT without contrast material demonstrates stagnation in the left transverse sinus which appears hyperattenuated (cord sign) (arrow), while the right transverse sinus lumen is patent (arrowhead). b Axial BCT with contrast reveals filling defect in the left transverse sinus (arrow). c Sagittal BCT with contrast shows occipital lobe hemorrhagic venous infarct (arrow) along with empty delta sign and filling defect in the left transverse sinus (arrowhead). d Coronal BCT with contrast reveals the hematoma (arrow) as well as empty delta sign in the left transverse sinus (blank arrowhead) compared to normal contrast filling in the right transverse sinus (arrowhead)
Fig. 2.
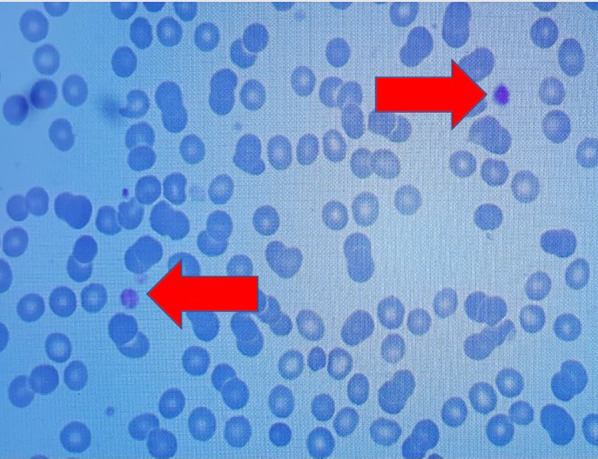
Peripheral blood smear indicates giant platelets (red arrows)
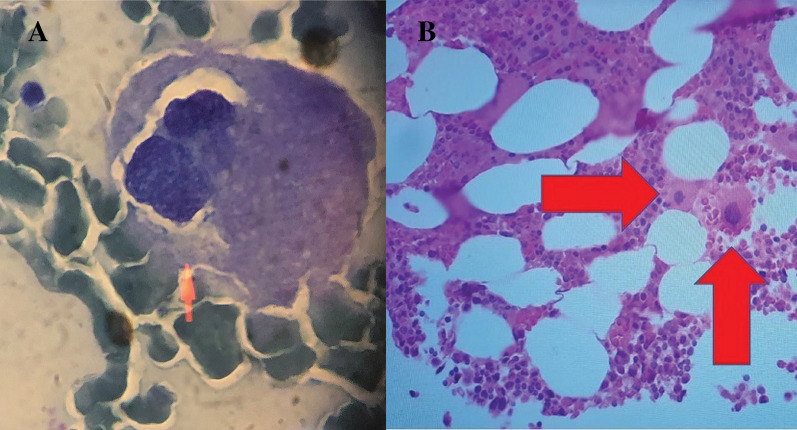
Fig. 3.
Bone marrow aspiration (a) and biopsy (b) display hypolobulated megakaryocytes and otherwise normal bone marrow
Fig. 4.

Chest computed tomography of the patient shows resolving pattern of previous involvement (bilateral multilobar peripherally dominant ground-glass opacities and consolidation in both lungs) by COVID-19 pneumonia
Discussion
We presented a patient with SARS-CoV-2 infection which was complicated by transverse sinus thrombosis followed by hemorrhagic venous infarction and ITP simultaneously. CVST is a rare but potentially life-threatening complication of COVID-19 infection with various manifestations depending on the location of cerebral venous sinus involvement. According to the literature, it has a frequency of 0.08% among hospitalized patients infected with COVID-19 and constitutes 4.2% of all cerebrovascular incidents in the context of COVID-19 infection [5]. Mechanisms that are suggested for CVST in COVID-19 infection, like other arterial and venous thrombosis occurring in COVID-19 patients, include systemic inflammation and cytokine storm, direct immune-mediated post-infection mechanism, and virus-induced angiitis [5–7]. Based on the findings of a systematic review and meta-analysis, CVST develops within 1 to 8 weeks of the respiratory or systemic symptoms of SARS-CoV-2 infection, which was the case in our patient [5]. On the other hand, ITP has also been recently identified as a complication of COVID-19, although its diagnosis remains challenging because of the presence of other causes of thrombocytopenia in patients with underlying COVID-19, including hemophagocytic lymphohistiocytosis (HLH), thrombotic thrombocytopenic purpura (TTP), sepsis, heparin-induced thrombocytopenia (HIT), and drug-induced thrombocytopenia. In this case, we made an effort to essentially rule out these possible diagnoses, as the prothrombin time (PT) and partial thromboplastin time (PTT) levels were within the normal limit, which made sepsis less likely, and there was no evidence of schistocytes in PBS, which thus did not favor a diagnosis of TTP. In addition, the bone marrow study and the clinical picture were not supportive of HLH, and finally, there was no offending agent known to cause thrombocytopenia such as heparin in the patient’s drug history or our treatment regimen, which excluded the possibility of HIT and drug-induced thrombocytopenia as a diagnosis. Nonetheless, a diagnosis of ITP does not require bone marrow evaluation, and it was done to rule out other differential diagnoses. Based on a systematic review, a considerable number of COVID-19 cases with ITP develop ITP manifestations after about 3 weeks of COVID-19 symptoms, which was true in the case of our patient [8]. As mentioned above, and based on the review of the literature, several cases of COVID-19 infection complicated by CVST or by ITP have been reported, but to the best of our knowledge, this is the first case of a patient who developed CVST and ITP at the same time. A case of COVID-19 infection complicated by ITP and internal jugular vein thrombosis was reported in which the suggested pathophysiologies were the paradoxical tendency of ITP for thrombosis formation, which is attributed to the release of young hyperactive platelets from bone marrow [9, 10]. Furthermore, COVID-19 itself may have caused ITP through the following mechanisms: inhibition of platelet synthesis due to direct infection of the bone marrow cells or platelets by the virus dysfunctional marrow microenvironment; virus-mediated liver damage leading to decreased thrombopoietin production; pulmonary endothelial damage followed by platelet aggregation in the lungs, subsequent formation of microthrombi, and platelet consumption; and finally, the destruction of platelets by the immune system manifested as a dramatic fall from baseline [8, 9]; on the other hand, thrombosis may be caused by a SARS-CoV-2-mediated coagulopathy mechanism [9]. Hence, we also hypothesized the same mechanisms for our patient: either COVID-19 infection caused ITP and ITP then gave rise to CVST, or COVID-19 complications themselves resulted in ITP and CVST independently and simultaneously. Another plausible mechanism that cannot be ignored is the immune-mediated thrombocytopenia caused by the anti-platelet 4-factor antibody, which is the proposed mechanism for CVST after the COVID-19 vaccine [11]. Unfortunately, the laboratory tests for this antibody were not available at that time, but as this condition is also an immune-mediated thrombocytopenia, it can be assumed to be in the spectrum of ITP.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
MGM and APM wrote the initial draft and revised it. LB and ME were the attending physicians and provided the patient's data and prepared figures.
Disclosures
Leyla Bahadorizadeh, Maziar Emamikhah, Arash Pour Mohammad, and Milad Gholizadeh Mesgarha declare no conflict of interest.
Compliance with Ethics Guidelines
No identifiable information was disclosed in writing this case report; however, written consent was obtained from the patient for publishing his medical data for scientific purposes.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Bidari A, Hassanzadeh M, Naderkhani M, Gholizadeh Mesgarha M, Pour Mohammad A, Azadeh A, et al. Predictors of critical COVID-19 in an Iranian population: age and disabilities play a special role TT. MJIRI. 2021;35(1):737–743. doi: 10.47176/mjiri.35.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegler JE, Cardona P, Arenillas JF, Talavera B, Guillen AN, Chavarría-Miranda A, et al. Cerebrovascular events and outcomes in hospitalized patients with COVID-19: the SVIN COVID-19 Multinational Registry. Int J Stroke Off J Int Stroke Soc. 2021;16(4):437–447. doi: 10.1177/1747493020959216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martincic Z, Skopec B, Rener K, Mavric M, Vovko T, Jereb M, et al. Severe immune thrombocytopenia in a critically ill COVID-19 patient. Int J Infect Dis. 2020;1(99):269–271. doi: 10.1016/j.ijid.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldini T, Asioli GM, Romoli M, Carvalho Dias M, Schulte EC, Hauer L, et al. Cerebral venous thrombosis and severe acute respiratory syndrome coronavirus-2 infection: a systematic review and meta-analysis. Eur J Neurol. 2021. [DOI] [PMC free article] [PubMed]
- 6.Fifi JT, Mocco J. COVID-19 related stroke in young individuals. Lancet Neurol. 2020;19(9):713–715. doi: 10.1016/S1474-4422(20)30272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhattacharjee S, Banerjee M. Immune thrombocytopenia secondary to COVID-19: a systematic review. SN Compr Clin Med. 2020;1–11. [DOI] [PMC free article] [PubMed]
- 9.Bucke D, Alizadeh K, Hallam S. COVID-19 complicated by immune thrombocytopaenic purpura and internal jugular vein thrombosis. BMJ Case Rep. 2021;14(7). [DOI] [PMC free article] [PubMed]
- 10.Lafaurie M, Maquet J, Baricault B, Ekstrand C, Christiansen CF, Linder M, et al. Risk factors of hospitalisation for thrombosis in adults with primary immune thrombocytopenia, including disease-specific treatments: a French nationwide cohort study. Br J Haematol. 2021. [DOI] [PubMed]
- 11.Ropper AH, Klein JP. Cerebral venous thrombosis. N Engl J Med. 2021;385(1):59–64. doi: 10.1056/NEJMra2106545. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.