Abstract
Children and adolescents infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are predominantly asymptomatic or have mild symptoms compared with the more severe coronavirus disease 2019 (COVID-19) described in adults. However, SARS-CoV-2 is also associated with a widely reported but poorly understood paediatric systemic vasculitis. This multisystem inflammatory syndrome in children (MIS-C) has features that overlap with myocarditis, toxic-shock syndrome and Kawasaki disease. Current evidence indicates that MIS-C is the result of an exaggerated innate and adaptive immune response, characterized by a cytokine storm, and that it is triggered by prior SARS-CoV-2 exposure. Epidemiological, clinical and immunological differences classify MIS-C as being distinct from Kawasaki disease. Differences include the age range, and the geographical and ethnic distribution of patients. MIS-C is associated with prominent gastrointestinal and cardiovascular system involvement, admission to intensive care unit, neutrophilia, lymphopenia, high levels of IFNγ and low counts of naive CD4+ T cells, with a high proportion of activated memory T cells. Further investigation of MIS-C will continue to enhance our understanding of similar conditions associated with a cytokine storm.
Subject terms: Inflammatory diseases, Paediatric research, Rheumatic diseases, Innate immunity, Inflammatory diseases
In this timely Review, the authors compare and contrast two forms of childhood inflammatory vasculitis: Kawasaki disease and the coronavirus disease 2019 (COVID-19)-associated multisystem inflammatory syndrome in children, highlighting epidemiological, clinical and immunological differences that suggest they should be classified as distinct syndromes.
Key points
Multisystem inflammatory syndrome in children (MIS-C) is characterized by exaggerated innate and adaptive immune responses following infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in predisposed children.
Clinical presentation of MIS-C involves multiple organ systems, with prominent involvement of the gastrointestinal and cardiovascular systems.
The factors that trigger the development of MIS-C in children exposed to or infected with SARS-CoV-2 are not yet known.
Results from epidemiological, clinical and immunological investigations have revealed that although MIS-C has phenotypic similarities to Kawasaki disease, they are different syndromes.
The approach to treatment of MIS-C aims to mute the augmented inflammatory response.
Introduction
Our understanding of the coronavirus disease 2019 (COVID-19) pandemic caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has improved greatly since the first human cases were reported in December 2019 in Wuhan City, China1,2. COVID-19 is known to involve multiple organ systems, with the major disease burden resulting from respiratory, cardiovascular, thrombotic and neurological complications3–5. Cellular entry of SARS-CoV-2 depends on binding of the viral spike (S) protein to cellular receptors such as angiotensin-converting enzyme 2 (ACE2) receptor, which is expressed in multiple organ systems6,7, and on S-protein priming by host-cell proteases8,9. In some individuals these steps are followed by a cascade of inflammatory events, resulting in a ‘cytokine storm’7. This massive pro-inflammatory cellular and cytokine response is a feature of patients with severe COVID-19 disease10.
Although morbidity and mortality from primary COVID-19 infection have remained limited in children, we have witnessed the emergence of a new inflammatory disorder associated with COVID-19, termed multisystem inflammatory syndrome in children (MIS-C) in the USA and paediatric inflammatory multisystemic syndrome (PIMS) in Europe11–15. Current evidence suggests that MIS-C is a post-infectious, immunologically mediated disorder related to prior SARS-CoV-2 exposure or infection16–18. Epidemiological, clinical and immunological investigations have revealed that MIS-C has phenotypic similarities to Kawasaki disease, a childhood inflammatory vasculitis, and it has been suggested that SARS-CoV-2 acts as an additional infectious trigger of Kawasaki disease, leading to an exaggerated phenotype along the same disease spectrum. However, in this Review we present evidence that although MIS-C has some features that overlap with Kawasaki disease, they are distinct syndromes that differ in degrees of hyperinflammation and dysregulated immune responses (Table 1).
Table 1.
Comparison of Kawasaki disease and MIS-C
| Comparison | Kawasaki disease | MIS-C |
|---|---|---|
| Demographics | ||
| Age | 6 months to 5 years | 6–11 years |
| Sex | Male predominance (~1.5:1) | No apparent predominance |
| Race or ethnicity | Highest incidence in Japan, China, South Korea and Taiwan | Highest incidence in children of African and Hispanic heritage |
| Pathogenesis | ||
| Trigger | Unknown but some data suggest possible preceding viral or bacterial infection | Onset ~3–6 weeks after SARS-CoV-2 exposure |
| Immunological characteristics | ||
| Similarities | Enhancement of IL-1β+ neutrophils and immature neutrophils | |
| Differences | T cell activation by a conventional antigen | SARS-CoV-2 viral spike (S) protein acts like a superantigen, triggering a cytokine storm |
| High levels of IL-17 | High levels of IL-15, IFNγ in severe cases | |
| Relatively less frequent MAS-like cytokine profile | >50% of patients with MIS-C have a MAS-like cytokine phenotype | |
| Lymphopenia is rare | Lymphopenia | |
| Anti-SARS-CoV-2 IgG not reported | Anti-SARS-CoV-2 IgG | |
| Clinical features | ||
| Similarities | Similar associations with fever, rash, cervical lymphadenopathy, neurological symptoms, extremity changes | |
| Differences | Relatively high incidence of conjunctival injection and oral mucous membrane changes | Relatively high incidence of gastrointestinal symptoms, myocarditis and shock, and coagulopathy |
| Management | ||
| Common | IVIG, glucocorticoids, acetylsalicylic acid | IVIG, glucocorticoids, acetylsalicylic acid |
| Rare | Infliximab, ciclosporin and anakinra | Anakinra, tocilizumab |
IVIG, intravenous immunoglobulin; MAS, macrophage activation syndrome; MIS-C; multisystem inflammatory syndrome in children; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Overview of Kawasaki disease
Kawasaki disease is a paediatric, self-limited, systemic inflammatory vasculitis that was first described in 1967 in Japan by Dr Tomisaku Kawasaki19. The most important long-term sequelae of Kawasaki disease relate to abnormalities of the coronary artery, and it is now the most common cause of acquired heart disease in children in the developed world20. A diagnostic feature of Kawasaki disease is fever that persists for more than 5 days when untreated. Additional typical clinical features include polymorphic skin rash (erythema), involvement of lips and oral mucosa (lip fissures, strawberry tongue), lymphadenopathy (cervical, often unilateral), non-exudative bilateral conjunctivitis and extremity changes (erythema and oedema of palms and soles that desquamate after 2–3 weeks, usually seen in the subacute phase)20.
Aetiology
The aetiology of Kawasaki disease is uncertain, and there is no single specific diagnostic test. The general consensus, based on results from multiple studies, is that Kawasaki disease is an immune-mediated disease triggered by infection (or infections) in patients with a genetic predisposition21–25. Some epidemiological features offer clues to the pathogenesis of Kawasaki disease. It is typically noted in children between the ages of 6 months and 5 years, with an estimated incidence of 25 cases per 100,000 children younger than 5 years in North America20,26. It is believed that children younger than 6 months, who have immature immune systems, are protected by passive immunity provided by the transplacental transfer of maternal antibodies, whereas children older than 5 years have developed protective antibody responses to the ubiquitous antigens that most encounter uneventfully in early childhood27. There is a male predominance (~1.5:1) in the incidence of Kawasaki disease, a feature that is shared by many common childhood infectious diseases28,29.
Seasonal variation in the incidence of Kawasaki disease has been noted, with peak incidence occurring in winter and spring in the USA and UK, and in summer in China and Korea30–34. Seasonal variation is least evident in Japan, the country with the highest incidence of Kawasaki disease35,36. Geographical variation and clustering in the incidence of Kawasaki disease also occurs, with the highest incidence reported in Japan, China, South Korea and Taiwan35,37–39. These epidemiological features point towards a transmissible infectious agent, which tends to occur in certain regions of the world with a seasonal variation in its incidence. Evidence exists for the presence of concurrent infections (with bacteria or common respiratory viruses, including coronaviruses) in patients with Kawasaki disease40–42. Immunohistochemistry analyses have shown infiltration of IgA plasma cells indicative of the antigen-driven immune response in inflamed tissues and the presence of cytoplasmic antigens suggestive of an infectious aetiology in bronchial and vascular endothelial cells and macrophages43. However, to date no single organism has been directly proved to cause Kawasaki disease44,45.
Involvement of superantigens
The potential pathogenic role of superantigens has been evaluated, on the basis of observations of preferential expression of T cell receptor (TCR) β genes encoding variable regions Vβ2 and Vβ8.1 in the peripheral blood lymphocytes of patients with acute Kawasaki disease46–48. Superantigen activity has been identified in the gut microbiota of such patients, and culture supernatants of these bacteria contain a heat shock protein (Hsp60, also known as GroEL) that induces T cell division and production of pro‐inflammatory cytokines49. However, in studies using flow cytometry in large series of patients with Kawasaki disease, TCR skewing and over-presentation of the described TCR clones has not been found, and it is currently believed that Kawasaki disease is a result of T cell activation by a conventional antigen50,51.
Involvement of nutritional disorders
The role of nutritional disorders, including vitamin D deficiency, in the pathogenesis of Kawasaki disease is subject to debate52. Vitamin D has an anti-inflammatory effect mediated through elevation of expression of IL-10 and inhibition of expression of vascular endothelial growth factor53,54. Results from a German population-based study showed that vitamin D supplementation has a protective effect against the development of Kawasaki disease55. Low serum concentrations of vitamin D might contribute to the development of coronary artery complications in children with Kawasaki disease56. However, other results have identified elevation of vitamin D levels during the acute phase of Kawasaki disease in children who subsequently developed coronary arterial lesions57. The contribution of other nutritional factors has also been suggested. For example, iron-deficiency anaemia is associated with development of coronary abnormalities in Kawasaki disease58. These varied results suggest the need for further investigation and research to elucidate the role of malnutrition in the pathogenesis of Kawasaki disease.
The role of microbiota
Disturbances in the normal microbiota (dysbiosis) have been proposed to have a role in the pathogenesis of various autoimmune and inflammatory disorders, including Kawasaki disease59–61. Stools from children with Kawasaki disease contain higher numbers of Gram-positive bacteria from the Streptococcus, Staphylococcus, Eubacterium and Peptostreptococcus genera, as well as Hsp60-producing Gram-negative bacteria, and lower numbers of lactobacilli than stools from children with other febrile illnesses or healthy controls49,61,62. Dysbiosis is associated with reduction in the production of short-chain fatty acids (particularly butyrate) and is proposed to lead to aberrant immune responses that are associated with Kawasaki disease63.
Genetic susceptibility
Epidemiological and genetic studies of Kawasaki disease have shed light on the role of genetic susceptibility in its development64. Kawasaki disease is prevalent in Japan, but also in children of Japanese ancestry living in Hawaii65. Siblings of children with Kawasaki disease have a 10-fold higher risk of development of the condition than children in the general population66. Several candidate genes have been identified through genome-wide association studies and linkage studies. The four major groups of genes that have been studied in Kawasaki disease are those associated with T cell activation (ORAI1 and STIM1), B cell signalling (CD40, BLK and FCGR2A), apoptosis (CASP3) and transforming growth factor-β (TGFβ) signalling (TGFB2, TGFBR2, MMP and SMAD)64. CASP3 encodes caspase 3, which is an effector caspase with a vital role in the execution phase of apoptosis. A single-nucleotide polymorphism in the CASP3 gene is associated with susceptibility to Kawasaki disease67. TGFβ is another vital protein with a central role in immunoregulation that affects multiple populations of leukocytes. Abnormalities in TGFβ signalling resulting from genetic variation are involved in Kawasaki disease susceptibility and outcomes68. Understanding the roles of these genetic alterations has implications for potential therapeutic approaches69. In addition to these groups, mutations in ITPKC, which is involved in Ca2+ mobilization and activation of NLRP3 inflammasomes, could result in enhancement of IL-1β and IL-18 production, disease susceptibility, coronary abnormalities and resistance to treatment with intravenous immunoglobulin (IVIG)70,71. Notably, immunosuppressive agents such as ciclosporin, a T cell inhibitor that blocks the calcineurin–NFAT pathway, have shown promise in the treatment of high-risk IVIG-resistant Kawasaki disease72. The observed association of HLA polymorphisms with Kawasaki disease varies; the predominant variant in a Japanese cohort was HLA-Bw54, whereas HLA-Bw51 was predominantly identified in white and Jewish populations73–75. Epigenetic regulation of inflammatory and immunoregulatory genes by factors such as methylation, microRNAs and long noncoding RNAs has been identified in Kawasaki disease, and might be relevant to pathogenesis and prognosis76. Additionally, single-nucleotide polymorphisms in cytokine genes, including IL1, KCNN2, TIFAB, P2RY12 and TNF, are associated with Kawasaki disease and with risk of coronary artery lesions, as well as IVIG treatment failure77–82.
Immunological aberrations
Innate and adaptive immune responses both have important roles in the development of Kawasaki disease83. An intense initial response driven by the innate immune system takes the form of neutrophilic leukocytosis, activation of monocytes, natural killer (NK) cells and γδ T cells, and elevation of production of acute-phase reactants and cytokines, especially IL-1β, which contributes to activation of endothelial cells, inducing upregulation of expression of cell-adhesion molecules, IL6 and IL8 (refs76–88). Pro-inflammatory IL-17 produced by type 17 T helper (TH17) cells could activate immune cells such as neutrophils and monocytes, leading to production of other inflammatory cytokines, such as IL-6, TNF and IL-8, thereby contributing to the pathogenesis of many inflammatory disorders89–92. By contrast, CD4+CD25+ regulatory T (Treg) cells contribute to immune tolerance through suppression of the hyperactivation of both innate and adaptive immune cells, via several mutually nonexclusive mechanisms. An imbalance in these pathways could lead to immune dysregulation, which could have a role in the pathogenesis of Kawasaki disease93–96.
Neutrophils are activated in Kawasaki disease and release reactive oxygen species, leading to endothelial cell injury83. Release of neutrophil extracellular traps (NETs) is also implicated in the pathogenesis of Kawasaki disease97. Although NETs have a protective role against infections as components of the innate immune system, they also have pathogenic potential for immune dysregulation and promotion of inflammation and tissue injury98. NETs have been implicated in the development and progression of rheumatic diseases, including systemic lupus erythematosus, rheumatoid arthritis and autoimmune vasculitis99–101. Yoshida et al.97 demonstrated elevation of NET formation in the sera of patients with Kawasaki disease, as well as neutrophil infiltration in the lesions of vasculitis in the coronary arteries and aorta in a mouse model of Kawasaki disease.
Autoimmune antibodies are thought to have a role in the pathogenesis of Kawasaki disease, particularly those against endothelial cell antigens102,103. Anti-endothelial cell antibodies could cause endothelial damage, with release of pro-inflammatory cytokines and a hypercoagulable state leading to vessel-wall injury and intravascular thrombosis104. However, not all results have demonstrated elevation of anti-endothelial cell antibodies in patients with Kawasaki disease105.
Immune complexes might have a role in the development of Kawasaki disease106. They appear in the first 7 days of the disease and peak in the second week before declining107. Elevation of circulating levels of immune complexes in Kawasaki disease is related to adverse outcomes such as coronary artery abnormalities108,109. However, a causal relationship between immune complexes and the pathogenesis of Kawasaki disease has not been definitively established. Activation of the complement system has also been implicated in the pathogenesis of Kawasaki disease, via both the classical and the mannose-binding lectin pathways110,111.
Kawasaki disease is considered by some to be a form of IgA vasculitis. In children with Kawasaki disease, intestinal permeability and levels of secretory IgA in the circulation are greater than in unaffected children, and in mouse models of the disease, elevation of levels of circulating secretory IgA and IgA deposition in the vasculature are observed112,113. Furthermore, pharmacological blockade of zonulin (a modulator of intestinal tight junctions) and administration of IVIG in these mouse models reduce intestinal permeability and cardiovascular inflammation compared with levels in untreated controls114.
Therapeutic strategies
IVIG and acetylsalicylic acid have emerged as first-line therapies for the management of Kawasaki disease20. IVIG therapy leads to rapid improvement in the clinical symptoms of rash, fever and conjunctival injection in most patients. Although the exact mechanism of action of IVIG is not yet known, proposals include inhibition of activation of innate immune cells and inflammatory mediators, expansion of Treg cells and suppression of TH17 cells93,115–118. Evidence indicates that IVIG might target IL-1β+ neutrophils via caspase-independent pathways119. Single-cell RNA sequencing of peripheral blood mononuclear cells in acute Kawasaki disease before and after IVIG therapy has revealed that genes encoding inflammatory mediators (including TNF and IL1B) are highly expressed in monocytes in untreated disease, with reduction of expression following therapy, along with significant enhancement of the plasma-cell population and induction of oligoclonal expansion of T cell receptors and IgG and IgA B cell receptors120. Mining of transcriptomic data by Boolean analysis has identified that several metabolic pathways might contribute to IVIG resistance in Kawasaki disease121. In high-risk patients with acute Kawasaki disease and in those who do not respond to IVIG therapy, steroid treatment can be considered, to prevent the occurrence of coronary artery abnormalities20. Additional therapeutic options for IVIG-resistant Kawasaki disease include infliximab (a monoclonal antibody to TNF), ciclosporin (a calcineurin inhibitor) and anakinra (an IL-1 receptor antagonist)20.
Overview of MIS-C
Since April 2020, many reports have documented a new hyperinflammatory syndrome in children11,12,122. In May 2020, the US Centers for Disease Control and Prevention (CDC) issued an alert identifying MIS-C as a critical illness in children that was associated with SARS‐CoV‐2 infection123. Since then, more than 4,000 cases of MIS-C have been reported in the USA alone124. In 26 studies published in 2020 and 2021, documenting 1,136 cases of MIS-C (mostly occurring in the USA and Europe), the reported median ages of the affected children were 6–11 years, with no significant gender difference14,15,122,125–140 (Table 2).
Table 2.
Demographic features of MIS-C study populations
| Study | Cohort location | N | Median age, years (range or IQR) | Male:female (%) | Race or ethnicity | Ref. |
|---|---|---|---|---|---|---|
| Dufort et al. | USA | 99 |
No median Distribution: 0–5, 31%; 6–12, 42%; 13–20, 26% |
54:46 | Black, 40%; white, 37%; Hispanic, 36%; other, 18%; Asian, 5% | 14 |
| Cheung et al. | USA | 17 | 8 (1.8–16) | 47:53 | Ashkenazi Jewish, 35%; Black, 24%; Hispanic, 24%; white non-Hispanic, 12%; Asian, 6% | 15 |
| Belhadjer et al. | France, Switzerland | 35 | 10 (2–16) | 51:49 | Not reported | 122 |
| Kaushik et al. | USA | 33 | 10 (IQR 6–13) | 61:39 | Hispanic, 45%; Black, 38%; white, 9%; Asian, 3%; other, 3% | 125 |
| Davies et al. | UK | 78 | 11 (IQR 8–14) | 67:33 | Afro-Caribbean, 47%; Asian, 28%; white, 22%; other, 3% | 126 |
| Pouletty et al. | France | 16 | 10 (IQR 4.7–12.5) | 50:50 | Not reported | 127 |
| Toubiana et al. | France | 21 | 7.9 (3.7–16.6) | 43:57 | Sub-Saharan African/Caribbean parentage, 57%; European parentage, 29%; Asian parentage, 10%; Middle Eastern parentage, 5% | 128 |
| Capone et al. | USA | 33 | 8.6 (IQR 4.4–12.6) | 61:39 |
Other, 45%; Black, 24%; Asian, 9%; white, 9%; unknown, 12% (Hispanic, 27%; non-Hispanic, 73%) |
129 |
| Hameed et al. | UK | 35 | 11 (IQR 6–14) | 77:23 | Not reported | 130 |
| Whittaker et al. | UK | 58 | 9 (IQR 5.7–14) | 56:44 | Black, 38%; Asian, 31%; white, 21%; other, 10% | 131 |
| Moraleda et al. | Spain | 31 | 7.6 (IQR 4.5–11.5) | 58:42 | Not reported | 132 |
| Dhanalakshmi et al. | India | 19 | 6 (1.1–16.9) | 42:58 | Not reported | 133 |
| Miller et al. | USA | 44 | 7.3 (0.7–20) | 45:55 | Hispanic, 34%; not reported, 25%; white, 20.5%; Black, 20.5% | 134 |
| Belot et al. | France | 108 | 8 (IQR 5–11) | 49:51 | Not reported | 135 |
| Lee et al. | USA | 28 | 9 (0.1–17) | 57:43 | Hispanic, 43%; white, 36%; Black, 18%; not reported, 3% | 136 |
| Riollano-Cruz et al. | USA | 15 |
No median Mean 12 (3–20) |
73:27 | Hispanic, 66%; non-Hispanic African American, 13%; non-Hispanic white, 13%; other, 8% | 137 |
| Ramcharan et al. | UK | 15 | 8.8 (IQR 6.4–11.2) | 73:27 | African or Afro-Caribbean, 40%; South Asian, 40%; mixed, 13%; other, 7% | 138 |
| Grimaud et al. | France | 20 | 10 (2–16) | 50:50 | Not reported | 139 |
| Perez-Toledo et al. | UK | 8 | 9 (7–14) | 63:37 | Not reported | 140 |
| Jonat et al. | USA | 54 | 7 (0.7–20) | 46:54 | White, 35%; unknown, 31%; other, 19%; African American, 15% | 205 |
| Feldstein et al. | USA | 186 | 8.3 (IQR 3.3–12.5) | 65:35 | Hispanic, 31%; Black, 25%; unknown, 22%; white, 19%; other, 5% | 13 |
| Toubiana et al. | France | 23 | 8.2 | 52:48 | Not reported | 236 |
| García-Salido et al. | Spain | 61 | 9.4 (IQR 5.5–11.8) | 66:34 | Not reported | 145 |
| Shobhavat et al. | India | 21 | 7 (IQR 1.9–12.1) | 47:53 | Not reported | 261 |
| Niño-Taravilla et al. | Chile | 26 | 6.5 (IQR 2–10.5) | 58:42 | Chilean, 73%; Venezuelan, 12%; Peruvian, 8%; Colombian, 4%; Haitian, 4% | 262 |
| Tolunay et al. | Turkey | 52 | 9 (IQR 5–13) | 38:62 | Turkish, 86%; Syrian, 14% | 263 |
IQR, interquartile range; MIS-C, multisystem inflammatory syndrome in children.
Patients with MIS-C have symptoms that resemble those of other hyperinflammatory syndromes, such as Kawasaki disease, toxic-shock syndrome (TSS) and macrophage activation syndrome (MAS), which is a type of secondary haemophagocytic lymphohistiocytosis11,12. To improve clarity and aid diagnosis, the CDC published a case definition, which includes age <21 years, fever, laboratory evidence of inflammation, hospital admission, multisystem (two or more) organ involvement (cardiac, renal, respiratory, haematological, gastrointestinal, dermatological or neurological), either laboratory confirmation of SARS-CoV-2 infection (by PCR with reverse transcription (RT–PCR), serology or antigen test) or known COVID-19 exposure up to 4 weeks before symptom onset, with no alternative plausible diagnosis123. The WHO and the UK Royal College of Paediatrics and Child Health (RCPCH) have also published case definitions, which are largely similar to the CDC definition, except that the RCPCH does not require evidence of prior exposure to SARS-CoV-2 (refs141,142). Despite the broad case definitions, and the considerable overlap with primary COVID-19 and other common childhood febrile illnesses, patients with MIS-C have distinct clinical presentation and levels of biomarkers, which aids in differential diagnosis143–145.
Aetiology
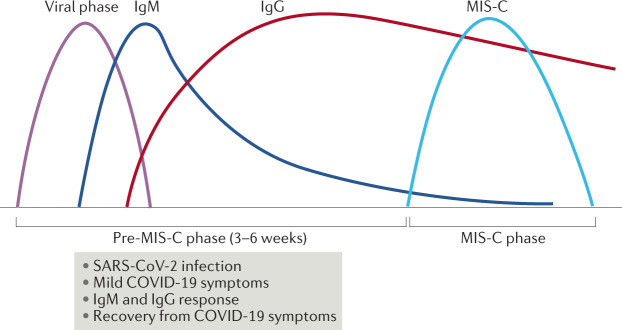
Compared with adults, primary SARS-CoV-2 infection is relatively mild in children146. Evidence indicates that a temporal relationship exists between SARS-CoV-2 exposure and development of MIS-C, as a spike in MIS-C cases occurs 3–6 weeks after the peak of SARS-CoV-2 transmission in a community13,129,147 (Fig. 1). Median intervals of 21 and 25 days have been observed between the occurrence of COVID-19 symptoms and the onset of MIS-C13,14. Although 80–90% of patients with MIS-C have been found to be SARS-CoV-2 seropositive, positivity in PCR testing is only 20–40%, suggesting that the interval to the onset of MIS-C is sufficient for viral RNA levels to fall considerably148,149. Furthermore, nasopharyngeal aspirates from patients with MIS-C have higher SARS-CoV-2 real-time RT–PCR cycle thresholds (indicating lower levels of viral RNA) than those from patients with severe COVID-19 (ref.150). However, autopsy examinations for three individuals who had MIS-C identified SARS-CoV-2 in various tissues, including heart, kidneys, brain and intestine, which is consistent with multisystem organ involvement in MIS-C151. Notably, the prolonged presence of SARS-CoV-2 in children’s intestines might cause zonulin-dependent loss of tight junctions, leading to leakage of viral antigens into the circulation, and to hyperinflammation and MIS-C152. By contrast, single-cell RNA sequencing of peripheral blood mononuclear cells from patients with acute MIS-C have revealed low viral and bacterial signatures in the immune cells, suggesting that active viral or bacterial infectious triggers are not contributing factors153. The accumulated evidence suggests that MIS-C might be the result of a combination of post-infectious immune dysregulation and virus-induced cytopathic effects and inflammation in multiple organ systems.
Fig. 1. The temporal relationship between SARS-CoV-2 infection and development of MIS-C.
Evidence suggests that a relationship exists between the timing of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and development of multisystem inflammatory syndrome in children (MIS-C). Cases of MIS-C tend to be seen 3–6 weeks after the peak of SARS-CoV-2 transmission in a community. Because of this time lag, MIS-C is associated with a strong anti-spike protein IgG response, but a weak IgM response. It should be noted that implication of SARS-CoV-2 as a triggering factor for the development of MIS-C has yet to be firmly established.
Paediatric patients with COVID-19 or MIS-C have strong IgG, but weak IgM antibody responses to the trimeric S glycoprotein of SARS-CoV-2, and weak responses to the nucleocapsid protein N, which is implicated in viral replication140,154–158. By contrast, adult COVID-19 patients have higher levels of anti-S antibodies, broader immunoglobulin response to SARS-CoV-2 with respect to specificity and isotype distribution (including IgG, IgM and IgA isotypes) and higher virus-neutralizing capacity140,155,156,158. The mild or asymptomatic nature of COVID-19 in children might be related to the extent of the antibody response. Nevertheless, IgG antibodies to S protein provide an important diagnostic criterion for MIS-C. Low IgM titres in MIS-C are consistent with its appearance several weeks after SARS-CoV-2 exposure.
Analyses from geographically diverse cohorts have demonstrated that 20–50% of people with no previous exposure to the virus have T cell reactivity against peptides corresponding to SARS-CoV-2 sequences159, which might be related to CD4+ T cell cross-reactivity with circulating seasonal human ‘common cold’ coronavirus (HCoV)160. Although this phenomenon has implications for the development of herd-immunity models and vaccine candidates, it is currently unclear whether the presence of prior cross-reactive CD4+ T cells is protective or harmful in the pathogenesis of MIS-C. When tested for serological evidence of prior seasonal coronavirus infection, children with MIS-C and those hospitalized for non-COVID reasons had similar prevalence and levels of antibodies to HCoV161. Additionally, HCoV antibody levels did not correlate with the levels of SARS-CoV-2 antibodies, suggesting that prior HCoV infection neither provides protection nor worsens the course of paediatric SARS-CoV-2 infection or MIS-C.
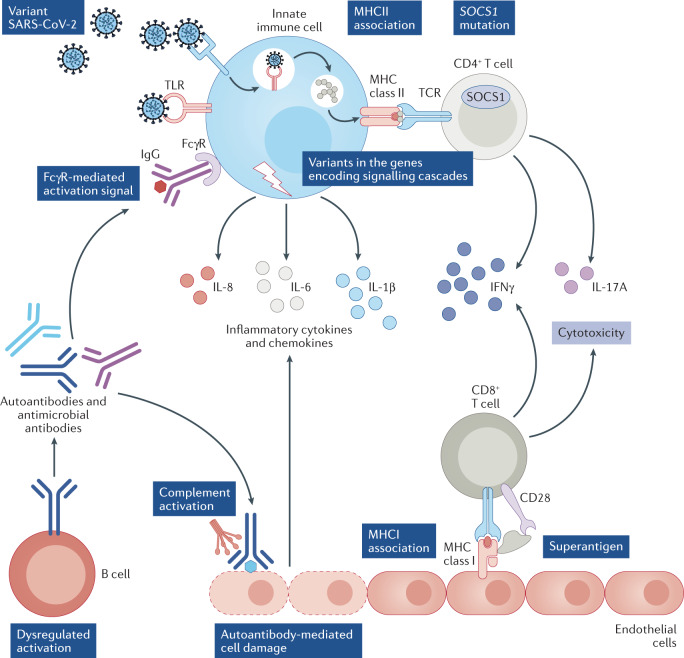
SARS-CoV-2 S protein as a superantigen
SARS-CoV-2 viral S protein might behave like a superantigen, triggering a cytokine storm that results in the development of the TSS-like presentation of MIS-C162 (Fig. 2). The S protein has a high-affinity motif for binding TCR, which is similar in structure to the staphylococcal enterotoxin B, a superantigen that mediates TSS by interacting with both TCR and MHC class II molecules. Computational modelling has shown that SARS-CoV-2 encodes a superantigen motif near the S1/S2 cleavage site, which interacts with both the TCR and CD28 (ref.163). TCR repertoire analysis of T cells in a small number of patients with MIS-C has identified skewing of TCR Vβ towards TRBV11-2 (Vβ21.3), which is associated with HLA class I alleles A02, B35 and C04 (refs163,164). The CDR3-independent nature of TCR Vβ skewing suggested superantigen-mediated activation of T cells in MIS-C. Further evidence supports the enrichment of TRBV11-2 among T cells153,165, although notably it has been observed in the absence of differential expression of a set of ‘superantigen genes’153. Also, MIS-C is usually observed several weeks after primary SARS-CoV-2 exposure, in contrast to the acute illness and cytokine storm observed in TSS166. In most cases, SARS-CoV-2 is undetectable in patients with MIS-C during the acute phase of inflammation. Thus, the superantigenic property of SARS-CoV-2 S protein and its implication in MIS-C is not yet confirmed. As an RNA virus, SARS-CoV-2 undergoes constant mutation, and whether any particular variant of the virus contributes to MIS-C by triggering strong inflammatory signalling in the immune cells and endothelial cells of children with COVID-19 requires further exploration. Notably, the use of in silico techniques has demonstrated that mutations in the binding region of SARS-CoV-2 S protein could influence the interaction with MHC class II molecules and TCR163.
Fig. 2. Possible mechanisms implicated in aberrant activation of immune cells in MIS-C.
Clinical signs of multisystem inflammatory syndrome in children (MIS-C) mostly appear several weeks after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. MIS-C might be triggered by dysregulation of immune responses following viral infection. Aberrant activation of immune cells in patients with MIS-C could result from several factors. Infection with particular variants of SARS-CoV-2 might trigger hyperinflammatory responses. Genetic predisposition resulting from variants in the genes that encode pattern recognition receptors, Fcγ receptors and components of the signalling cascades of immune response, as well as mutations in genes such as SOCS1, which regulate inflammatory responses, could all contribute to enhancement of inflammatory responses to infection. Dysregulated activation of lymphocytes, with production of IgG corresponding to microbial pathogens or autoantigens, could cause immune-complex-mediated innate-cell activation by signalling via Fcγ receptors. Production of autoantibodies could also lead to complement activation and autoantibody-mediated endothelial damage. SARS-CoV-2 spike (S) protein might function as a superantigen, contributing to activation of T cells. SOCS1, suppressor of cytokine signalling 1; TLR, Toll-like receptor.
Involvement of nutritional disorders
Nutritional factors such as vitamin D deficiency might have a role in the development of MIS-C. Adults with vitamin D deficiency were noted to have a more severe form of COVID-19 with an increased risk of death than those without this deficiency167. Vitamin D supplementation has proved to be of some benefit in infections with other viruses, such as influenza A168. Whether a similar benefit could accrue in MIS-C has not been elucidated.
The role of microbiota
Another contributing factor in the development of MIS-C that warrants investigation is the role of gut and respiratory tract microbiota. Gastrointestinal microbes are important regulators of the gut immune system and inflammation, and influence the balance between TH17 cells and Treg cells169. Adult patients with COVID-19 display alteration of gut and upper respiratory microbiomes, and gut dysbiosis persists beyond the nasal clearance of SARS-CoV-2 (refs170–173). Notably, faecal SARS-CoV-2 load is inversely correlated with the abundance of bacteria of the Bacteroidetes phylum, which suppress ACE2 in the mouse gut173. Preliminary data from peer reviewed and non-peer reviewed reports also suggest the persistence of microbiome dysbiosis in the upper respiratory tract and the gut in paediatric COVID-19 (refs174,175).
Genetic susceptibility
The low incidence of MIS-C relative to COVID-19, and the similarity in antibody response to SARS-CoV-2 in paediatric patients with MIS-C and with COVID-19 (irrespective of the subsequent development of MIS-C) suggest that SARS-CoV-2 infection causes dysregulation of immune responses in a subgroup of predisposed children with particular genetic backgrounds176. Specifically, predisposition might be related to mutations and polymorphisms in the genes that encode pattern recognition molecules such as Toll-like receptors, components of the signalling cascades of the immune response and Fcγ receptors (Fig. 2). The incidence of MIS-C is higher in children of African and Hispanic heritage than in those of other ethnicities, although attribution of this finding to genetic differences is confounded by the contribution of socioeconomic factors to the risks of SARS-CoV-2 infection177–180. Among 145 HLA-A, HLA-B and HLA-C genotypes, HLA-B*46:01 was associated with in silico prediction of the fewest SARS-CoV-2-binding peptides (suggesting particular vulnerability to COVID-19), whereas HLA-B*15:03 was predicted to have the greatest capacity for coronavirus peptide presentation (suggesting protective T cell-based immunity)181. Monogenic loss-of-function variants affecting immunity in the type I interferon signalling pathway might confer a predisposition to severe COVID-19 manifestations182,183. In a study of two unrelated patients with infection-associated immune thrombocytopenia and autoimmune haemolytic anaemia, both had SOCS1 haploinsufficiency and exhibited T cell activation and high levels of interferon signalling, and one developed MIS-C after SARS-CoV-2 infection. SOCS are negative regulators of interferon signalling, and silencing mutations might predispose the individuals to infection-associated hyperinflammatory states such as MIS-C184 (Fig. 2). However, a clear genetic basis that explains why some children develop MIS-C after SARS-CoV-2 exposure is currently undetermined. Additional factors, such as epigenetic effects at the level of histones, DNA or microRNA might also contribute to the development of MIS-C.
Immunological aberrations
In general, the signatures of immune cells and inflammatory parameters of MIS-C closely overlap with those of adults with moderate-to-severe COVID-19 rather than with paediatric COVID-19, which is mostly mild or asymptomatic. Also, immune activation in MIS-C is transient and tends to reduce during recovery154,185,186.
Pro-inflammatory mediators
Elevation of levels of pro-inflammatory cytokines such as IL-6, IL-10 and IL-17A, and chemokines such as CXCL5, CXCL11, CXCL1 and CXCL6 in MIS-C distinguishes it from paediatric COVID-19 (refs136,153,154,187). In various cohorts, elevation of TNF, IL-1β, IFNγ, soluble IL-2R, CCL2, CCL3, CCL4, CXCL8 (IL-8) or IFNγ-induced chemokines CXCL9 and CXCL10 has been reported in the serum of patients with MIS-C relative to those with paediatric COVID-19 or healthy controls136,150,153,165,186–189. Overall, enhancement of these pro-inflammatory molecules in the circulation indicates inflammatory responses of myeloid and lymphoid cells. Endothelial cells could also contribute innate inflammatory mediators, as E-selectin, a marker of inflamed endothelial cells, shows elevation in the serum of patients with MIS-C153. The reasons for the absence of some pro-inflammatory mediators in particular cohorts of patients are not known. The mediators that were analysed could have differed from study to study, but also, the levels of inflammatory mediators might vary depending on the patients’ genetic and epigenetic backgrounds, severity of the disease, geographical location and timing of the analyses. Results from a study of plasma proteomics in children with SARS-CoV-2 infection, which have not yet undergone peer review, suggest that IFNγ expression is heterogeneous among patients with MIS-C, and that patients have dysregulated response to IFNγ190. As the pandemic progresses, it will be important to have a consensus regarding the panel of cytokines and chemokines that should be analysed in relation to MIS-C, to facilitate our understanding of the molecular pathogenesis and heterogeneity of this complex disease, and to enable accurate prognosis and effective treatment.
Immune-cell profiles
Immune-cell profiling of children with MIS-C or primary COVID-19 infection reveals similarities as well as differences in their immune signatures185. They have similar proportions of eosinophils, immature granulocytes, monocytes and classic dendritic cells, but patients with MIS-C have elevation of neutrophils and reduction of plasmacytoid dendritic cells153,185,188, which might contribute to the low levels of IFNα that are observed in the blood of patients with MIS-C relative to those with paediatric COVID-19 (ref.188).
Neutrophils and monocytes are activated in patients with MIS-C186 and show upregulation of alarmin signatures (in particular S100A genes) and reduction of expression of antigen-presenting, antigen-processing and co-stimulatory molecules153,165,186. Compared with healthy children, those with MIS-C have greater expression of cytotoxicity genes and CCL4 in NK cells, which might contribute to the occurrence of tissue damage153. Preliminary results suggest that plasma levels of IFNγ correlate with levels of NCR1 and IL-2RA, which are the soluble markers of activated NK and T cells, respectively190.
MIS-C could have a common pathophysiology with Kawasaki disease involving NET formation, which has been described in the sera of adults with COVID-19 and with endothelial injuries or a prothrombotic state191–193. However, plasma levels of NETs and release of NETs from neutrophils are similar in children with mild or moderate COVID-19 or MIS-C and in healthy children194. Despite similarities between disorders associated with pathogenic NETs and MIS-C, the role of NETosis in the pathogenesis of MIS-C remains uncertain because of a lack of definitive evidence, and hence further studies are warranted.
Both MIS-C and paediatric COVID-19 present with general lymphopenia (affecting cells that include mucosa-associated invariant T cells, γδ T lymphocytes and CD8+ T lymphocytes)136,150,154,185–188. Compared with paediatric COVID-19, in MIS-C there is more-pronounced CD4+ T cell-biased lymphopenia, which is similar to the situation in severely ill adults with COVID-19 (ref.185). However, results from single-cell RNA sequencing analysis have revealed enhanced proliferation of CD4+ T cells in patients with MIS-C compared with healthy individuals153, suggesting that lymphopenia might be the result of homing of T cells to the inflamed tissues. Despite showing T cell lymphopenia, the relative distribution of various T cell subsets such as naive, central memory and effector memory cells in patients with MIS-C is similar to that in age-matched healthy individuals, indicating a pan-CD4+/CD8+ T cell lymphopenia, rather than a subset-specific effect154,185.
A distinct feature of MIS-C compared with paediatric COVID-19 is the activation of CX3CR1+CD8+ T cells (CD8+ T cells that express vascular endothelium-homing CX3CR1, also known as fractalkine receptor), which could have implications for development of vascular abnormalities and cardiovascular abnormalities185. This immunological phenotype is correlated with elevation of D-dimer, reduction of platelets and with the requirement for vasoactive medication. Although not as prominent as in NK cells, CD8+ T cells in MIS-C also show increases in signatures of cytotoxicity compared with those in healthy children153. RNA sequencing in blood from children with MIS-C revealed aberrant NK and CD8+ T cell regulation, with depletion of NK cells and an absence of NK cell-dependent exhaustion of effector CD8+ T cells, which can lead to sustained inflammation195. Notably, the proportion of activated CX3CR1+CD8+ T cells in patients with MIS-C decreases as the clinical status improves185. Thus, there seems to be a sustained activation and dysregulation of CD8+ T cells, particularly those that express CX3CR1.
Nonspecific activation of B cell clones and expansion of plasmablasts occurs in MIS-C150,153,185,186. Plasmablast elevation also occurs in children with COVID-19 (ref.185). However, the specificity of expanded B cells and plasmablasts might vary between the two conditions. Patients with MIS-C display pronounced autoreactivity signatures of plasma immunoglobulins compared with healthy children or adults and children with COVID-19 (refs103,153,154). Also, patients with MIS-C have evidence of extrafollicular responses, as indicated by high frequencies of plasmablasts expressing the T box transcription factor T-bet185. Future research should aim to uncover the reasons for this B cell activation, and should compare the characteristics of expanded B cells and plasmablasts, and the specificities of immunoglobulins, in MIS-C and paediatric COVID-19. As both conditions are associated with nonspecific B cell activation and elevation of plasmablast frequencies196, molecular mimicry between self-antigens and SARS-CoV-2 antigens (as described in a paper that has not yet been peer reviewed197) might not be entirely responsible for the appearance of autoreactivity in MIS-C, and instead a combination of molecular mimicry and dysfunctional immunoregulatory machinery could be involved.
Humoral features
Analysis of IgG by systems serology has identified that humoral features in patients with MIS-C, such as complement deposition and neutrophil phagocytosis, overlap with those in convalescent adults with COVID-19 (ref.158). However, patients with severe MIS-C have persistent levels of FcγR binding (and in particular activating FcγRIIA) and inflammatory monocyte/macrophage-activating IgG158. Although hypergammaglobulinaemia is not observed in patients with MIS-C, a selective expansion of the IgG repertoire to react not only to SARS-CoV-2, but also to other bacterial and viral pathogens, some of which are implicated in the triggering of Kawasaki disease, has been observed. The underlying reason for the enrichment of particular IgG specificities is not yet known, but many of the microbes have been identified in the respiratory tracts of patients with MIS-C198, suggesting a role for an immune-complex-driven inflammatory response in the pathogenesis of MIS-C. IgG and IgA autoantibodies occur in patients with MIS-C, and recognize gastrointestinal, mucosal, immune-cell and endothelial antigens153,154. Although the functionality of these autoantibodies and their roles in the pathogenesis of MIS-C should be investigated, these results might explain at least in part the involvement of multiple organ systems in MIS-C and provide a pointer towards dysregulated activation of B lymphocytes, enhanced autoreactivity and immune-complex-mediated inflammatory responses (Fig. 2). Enhanced expression of CD64 (FcγR1), a high-affinity receptor for the Fc fragment of IgG, has been observed on neutrophils and monocytes of patients with MIS-C154,186. Furthermore, most of these patients respond to IVIG therapy11,15,122,129,131, which provides additional indirect support for the implication of FcγR-mediated activation of innate immune cells by immune complexes formed by these IgGs.
A role for the complement system in the pathogenesis of MIS-C has been suggested. Patients with MIS-C or paediatric COVID-19 have elevated plasma levels of soluble C5b-9 compared with healthy controls150,199. Soluble C5b-9 is a biomarker to monitor the activity of the terminal pathway of complement, and elevated levels suggest complement activation and endothelial dysfunction. Notably, although patients with MIS-C and paediatric COVID-19 have similar levels of complement-activating IgG antibodies to S protein of SARS-CoV-2 (refs140,154–158), those with MIS-C have enhanced autoreactive signatures of IgG103,153,154. As patients with MIS-C typically have minimal or no SARS-CoV-2 at the time of development of the disease, enhanced autoreactivity and immune-complex formation might contribute to the elevated levels of C5b-9. Consistent with complement activation, MIS-C is associated with clinical criteria for complement-mediated thrombotic microangiopathy, such as microangiopathic haemolytic anaemia, hypertension, thrombocytopenia, proteinuria and evidence of organ damage on the basis of lactate dehydrogenase elevation199. Compared with paediatric COVID-19, patients with MIS-C have higher incidence of thrombotic events200. Results from proteomics analyses of plasma samples, which have not yet been peer reviewed, suggest that phospholipase A2 (PLA2G2A) could be a biomarker for diagnosis of thrombotic microangiopathy in MIS-C190. The lectin complement pathway might also have an important role in the pathogenesis of diseases associated with SARS-CoV-2, as a result of the carbohydrate-residue-rich surface structures of the virus201–203.
Therapeutic strategies
Treatment approaches to MIS-C aim to mute the exaggerated inflammatory response. Multiple approaches, borrowed from Kawasaki disease and other hyperinflammatory syndromes, have been considered, ranging from IVIG to glucocorticoids and immunotherapy204,205. MIS-C treatment regimens described in 24 studies, involving 1,020 individuals, are summarized in Table 3, highlighting the many variations on the theme of attempting to calm overactive inflammatory responses6,17,20,94,100–114,164. In most studies, most (70–100%) of the patients were treated with IVIG as the first-line agent, with satisfactory results. Steroids were the second most common treatment employed for patients with MIS-C.
Table 3.
Treatment of MIS-C
| Study | Cohort location | N | IVIG (%) | Glucocorticoids (%) | Other treatments | Ref. |
|---|---|---|---|---|---|---|
| Dufort et al. | USA | 99 | 70 | 64 | NR | 14 |
| Cheung et al. | USA | 17 | 77 | 82 | Tocilizumab, 6% | 15 |
| Belhadjer et al. | France, Switzerland | 35 | 72 | 34 | Anakinra, 9% | 122 |
| Kaushik et al. | USA | 33 | 54 | 51 | Tocilizumab, 36%; remdesivir, 21%; anakinra, 12%; convalescent plasma therapy, 3% | 125 |
| Davies et al. | UK | 78 | 76 | 73 | Tocilizumab, 4%; anakinra, 10%; infliximab, 9%; rituximab, 1% | 126 |
| Pouletty et al. | France | 16 | 94 | 18.8 | Tocilizumab, 6%; anakinra, 6%; hydroxychloroquine, 6% | 127 |
| Toubiana et al. | France | 21 | 100 | 33 | NR | 128 |
| Capone et al. | USA | 33 | 100 | 70 | Tocilizumab, 9%; anakinra, 12%; infliximab, 3% | 129 |
| Hameed et al. | UK | 35 | 100 | 100 | NR | 130 |
| Whittaker et al. | UK | 58 | 71 | 64 | Anakinra, 5%; infliximab, 14% | 131 |
| Moraleda et al. | Spain | 31 | 65 | 68 | Remdesivir, 6% | 132 |
| Dhanalakshmi et al. | India | 19 | 79 | 58 | Tocilizumab, 5% | 133 |
| Miller et al. | USA | 44 | 82 | 96 | Anakinra, 18% | 134 |
| Lee et al. | USA | 28 | 71 | 61 | Anakinra, 18% | 136 |
| Riollano-Cruz et al. | USA | 15 | 80 | 20 | Tocilizumab, 80%; remdesivir, 13%; anakinra, 13%; convalescent plasma therapy, 6% | 137 |
| Ramcharan et al. | UK | 15 | 66 | 33 | NR | 138 |
| Grimaud et al. | France | 20 | 100 | 10 | Tocilizumab, 10%; anakinra, 10% | 139 |
| Jonat et al. | USA | 54 | 83 | 79 | NR | 205 |
| Feldstein et al. | USA | 186 | 77 | 49 | Anakinra, 13% | 13 |
| Toubiana et al. | France | 23 | 100 | 61 | NR | 236 |
| García-Salido et al. | Spain | 61 | 45 | 80 | Tocilizumab, 24%; hydroxychloroquine, 55% | 145 |
| Shobhavat et al. | India | 21 | 52 | 86 | Tocilizumab, 10% | 261 |
| Niño-Taravilla et al. | Chile | 26 | 77 | 88 | Tocilizumab, 12%; infliximab, 4% | 262 |
| Tolunay et al. | Turkey | 52 | 93 | 71 | Anakinra, 4% | 263 |
IVIG, intravenous immunoglobulin; MIS-C, multisystem inflammatory syndrome in children; NR, not reported.
Shock and cardiovascular manifestations comprise a predominant mode of presentation of MIS-C, and high-dose glucocorticoids have been advocated for, and used successfully in, patients with shock. Widely followed guidance from the ACR recommends IVIG as first-line therapy in hospitalized patients with MIS-C, with addition of glucocorticoids in the presence of shock, organ-threatening disease or refractory disease149. In a study of 181 children with suspected MIS-C, IVIG alone had a higher failure rate than the use of IVIG with methylprednisolone (OR 0.25; 95% CI 0.09–0.70)206. By contrast, results from a multinational observational cohort study that involved 615 children with suspected MIS-C identified no difference in acute outcomes between primary treatment with IVIG alone, IVIG with steroids or steroids alone207. In view of the apparently important role of IL-1β in the pathogenesis of MIS-C, anakinra (an IL-1 receptor antagonist) has been used in MIS-C that is refractory to therapy with IVIG or steroids, extrapolating from its success in small groups of patients with IVIG-resistant Kawasaki disease122,148,208,209.
Zonulin-dependent loss of intestinal mucosal permeability is implicated in mediation of the hyperinflammation observed in MIS-C, and accordingly, a patient who did not respond to anti-inflammatory therapies was treated with the zonulin antagonist larazotide, with a satisfactory outcome152. In a pooled meta-analysis, D-dimer was found to be elevated in 92% of patients (330 out of 356)210. Because of the associated risk of hypercoagulability, and extrapolating from the management of Kawasaki disease, the use of anticoagulants such as acetylsalicylic acid and/or enoxaparin has been reported211,212.
MIS-C: distinct from Kawasaki disease?
Both Kawasaki disease and MIS-C have temporal associations with infectious diseases and are associated with immune-system alteration, systemic inflammation and cytokine storm. Myocardial dysfunction, which is seen in both pathologies, might be a consequence of systemic inflammation213,214. An artificial intelligence computational analysis based on viral pandemics and disease-severity gene signatures, and in particular induction of IL15–IL15RA genes, has placed Kawasaki disease and MIS-C on the same host-immune-response continuum (although these results have not yet been peer reviewed)215. Consistently, patients with MIS-C have significantly higher levels of IL-15 than paediatric patients with COVID-19 (ref.189). However, the intensity of the immune response is high in MIS-C, which places it further along the severity spectrum than Kawasaki disease215.
A quarter to half of patients with MIS-C meet the full criteria for diagnosis of Kawasaki disease17,148,149,212,216. Without evidence of prior SARS-CoV-2 exposure in these patients, it might not be possible to differentiate them from those with classic Kawasaki disease. Commonly reported clinical features of MIS-C include fever, mucocutaneous findings, myocardial dysfunction with cardiogenic or vasoplegic shock, gastrointestinal symptoms and neurological features including headache and altered mental status (Table 4). Like Kawasaki disease, these clinical manifestations are not specific to MIS-C, and they could occur in other infectious or inflammatory conditions20.
Table 4.
Reported clinical features of multisystem inflammatory syndrome in children
| Affected organ system | Symptoms | Frequency of involvement (%) | Refs |
|---|---|---|---|
| Cardiovascular | Shock | 40–80 | 210,234–236 |
| Cardiac arrhythmias | 2 | 235 | |
| Abnormal ST- or T-wave segment | 22 | 235 | |
| Prolonged QT interval | 2 | 235 | |
| Pericardial effusion | 13–28 | 235,246 | |
| Decreased LVEF by echo | 31–58 | 234,235 | |
| Increased troponin | 68–95 | 234,235 | |
| Myocarditis | 36–87 | 210,236,246 | |
| Coronary artery dilation on CT | 27 | 235 | |
|
Coronary artery aneurysm Mild Moderate Giant |
14–48 22 7 1 |
||
| Gastrointestinal | Gastrointestinal symptoms | 60–100 | 234–236 |
| Diarrhoea | 38–72 | 210,235 | |
| Vomiting | 51–68 | 210,246 | |
| Abdominal pain | 19–71 | 210,235 | |
| Ascites | 21 | 235 | |
| Ileitis | 9 | 235 | |
| Colitis | 4 | 235 | |
| Ophthalmological | Conjunctivitis | 32–83 | 234–236,246,264 |
| Periorbital erythema and oedema | 20 | 264 | |
| Nervous system | Neurological symptoms | 13–35 | 210,235,236,249 |
| Severe symptoms, including encephalopathy, stroke, central nervous system infection/demyelination, Guillain–Barré syndrome and acute cerebral oedema | 3 | 249 | |
| Integumentary | Rash | 50–70 | 234,236,246 |
| Erythematous skin rash | 62 | 235 | |
| Hyperaemia, oedema or desquamation of extremities | 26–51 | 235,264 | |
| Malar erythema | 17 | 264 | |
| Skin eruptions | 9–14 | 264 | |
| Desquamation in groin | 26 | 236 | |
| Respiratory | Upper respiratory tract infection | 34 | 235 |
| Lower respiratory tract infection | 22 | 235 | |
| Pleural effusion on CT | 20 | 235 | |
| Lung involvement on CT (bilateral pulmonary consolidation and ground-glass opacity) | 13 | 235 | |
| Mucosal | Oral mucosa hyperaemia | 41 | 235 |
| Red and/or cracked lips | 37–49 | 246,264 | |
| Strawberry tongue | 11–23 | 246,264 | |
| Lips and oral-cavity changes | 74 | 234,236 | |
| Other | Lymphadenopathy (cervical) | 19–61 | 235,236,246 |
| Extremity changes | 8–52 | 234,236,246 |
LVEF, left ventricular ejection fraction.
Epidemiological and clinical differences
Despite the apparent similarities between MIS-C and Kawasaki disease, there are important epidemiological and clinical differences20,122,127. Kawasaki disease is typically a disease of young children <5 years old, whereas MIS-C has been reported in a wide age range from 1.6 to 20 years, with a median age of 6–11 years20,217,218 (Table 2). In sharp contrast to Kawasaki disease, there is a surprising lack of reports of MIS-C from Japan and East Asian countries219,220. In fact, published data from the USA and Europe suggest that MIS-C is most commonly encountered in children of African and Hispanic heritage177,180. These epidemiological differences suggest that although MIS-C has phenotypic similarities to Kawasaki disease, they are essentially distinct syndromes.
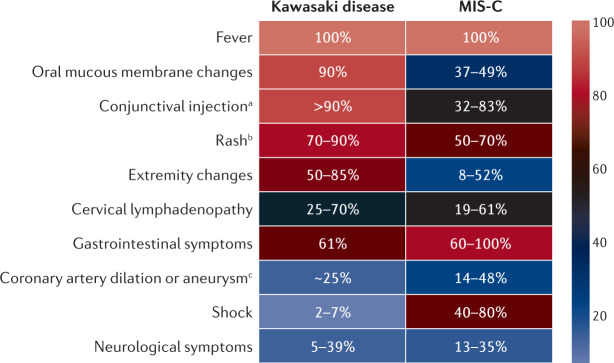
Cardiac involvement is more prevalent and severe in MIS-C than in Kawasaki disease. Although a quarter of untreated patients with Kawasaki disease will develop coronary artery abnormalities, in the current era with a high level of clinical suspicion as well as early diagnosis and treatment, the incidence of coronary artery abnormalities in Kawasaki disease is <10%216,221–224. By contrast, our understanding of coronary artery dilation in MIS-C is still evolving, and incidence rates of 14–48% have been reported in various patient populations180,191,192 (Fig. 3). However, the adoption of standardized MIS-C management protocols has begun to reduce the rate of coronary artery involvement149. Cardiac MRI in MIS-C has demonstrated high signal intensity on T1-weighted and T2-weighted imaging, consistent with diffuse myocardial oedema, with no enhancement on late gadolinium imaging to suggest fibrosis225. Results from echocardiographic studies have demonstrated that global left ventricular longitudinal strain is significantly lower in individuals with MIS-C than in those with Kawasaki disease226. A longitudinal, single-centre study involving 15 children with MIS-C has demonstrated significant improvement towards normalization of both ventricular function and coronary artery size over a 30-day follow-up period227.
Fig. 3. Comparative incidence of clinical signs in MIS-C and Kawasaki disease.
Percentage incidence of particular symptoms in patients with multisystem inflammatory syndrome in children (MIS-C) or Kawasaki disease is shown, with the values derived from published reports210,231,232,234–236,246,249,250,264–270. Although some clinical signs, such as fever and cervical lymphadenopathy are equally prevalent in both MIS-C and Kawasaki disease, the incidence of other symptoms, including shock, coronary artery involvement and gastrointestinal symptoms (vomiting, diarrhoea or abdominal pain), are characteristic of MIS-C. a‘Conjunctival injection’ refers to bilateral non-exudative conjunctivitis in Kawasaki disease. b‘Rash’ refers to polymorphous rash in Kawasaki disease. c‘Coronary artery dilation of aneurysm’ refers to incidence in untreated cases of Kawasaki disease.
Fewer than 10% of cases of Kawasaki disease manifest as Kawasaki disease-shock syndrome (KDSS), which requires the use of intravascular fluid resuscitation and vasoactive medication228–231. Patients with KDSS tend to be older, have longer duration of fever and higher levels of inflammatory markers, and have a higher incidence of IVIG resistance as well as coronary abnormalities than those without KDSS232,233. By contrast, shock and depressed left ventricular systolic function are more frequent with MIS-C, for which reports indicate that 40–80% of patients present with shock210,234–236 (Fig. 3). In a retrospective comparison of a cohort of patients with KDSS with published data relating to MIS-C, individuals with KDSS were more likely than those with MIS-C to fulfil the diagnostic criteria for complete Kawasaki disease, with higher incidence of coronary artery aneurysms237.
Kawasaki disease has been reported to occur with MAS238,239. In a retrospective analysis of 638 patients with Kawasaki disease, the incidence of MAS was <2%240. However, this figure is likely to be an underestimation of the true incidence, as a result of an absence of sensitive diagnostic criteria and a lack of awareness among health-care providers241. Patients with Kawasaki disease and MAS tend to have elevation of levels of IFNγ, TNF, serum neopterin, IL-18 and sTNFR-II242. A retrospective comparison of patients with MAS (as a complication of systemic-onset juvenile idiopathic arthritis) and MIS-C revealed that MAS was associated with lower levels of haemoglobin and fibrinogen, and higher ferritin and lactate dehydrogenase, whereas patients with MIS-C tended to have signs of shock and need of intensive care management243. Results that have not yet been peer reviewed, based on analyses of IFNγ and CXCL9 signalling characteristics, suggest that >50% of patients with MIS-C have a MAS-like cytokine phenotype190, along with elevation of CD163, IL-2RA and ferritin (during the early period) in the plasma. However, although MAS has an association with neutropenia, patients with MIS-C, including those who meet the criteria for MAS, display neutrophilia. Thus, although KDSS and Kawasaki disease with MAS have overlapping clinical features with MIS-C, there are subtle differences that are likely to reflect the different cytokine profiles in these conditions.
Gastrointestinal and neurological symptoms are also more commonly encountered in MIS-C than in Kawasaki disease134,235,236,244–247. The gastrointestinal manifestations include abdominal pain, vomiting and diarrhoea210,235,246, with rare presentations that resemble appendicitis requiring surgical exploration248. In a national US registry consisting of 1,695 children and adolescents with active COVID-19 infections including MIS-C (n = 616), neurological symptoms were noted in 22% of the patient population (n = 365), with most of those affected having transient symptoms249. Among these 365 patients, 126 met the criteria for MIS-C. In the patients with neurological involvement (n = 365), 43 (12%) had life-threatening neurological involvement (including encephalopathy, stroke, central nervous system infection and/or demyelination, Guillain–Barré syndrome and acute cerebral oedema) and among which 20 (47%) met the criteria for MIS-C. In a study of 286 children with MIS-C located in 55 centres in 17 European countries, neurological involvement was identified in 43 individuals (15%)235. In a pooled meta-analysis of data from 370 children with MIS-C, 133 (35.9%) had neurological symptoms210 (Table 4). Neurological involvement in Kawasaki disease is variable, reportedly affecting 5–39% of patients250,251.
In contrast to those with Kawasaki disease, patients with MIS-C tend to have a worse acute clinical course and multisystem involvement, as illustrated by an increased requirement forintensive care management. A large study of >1,000 patients with Kawasaki disease revealed that 2.4% of these children required intensive care252. In stark contrast, an analysis of 783 cases of MIS-C determined that 68% of patients required intensive care admission, 63% needed inotropic support, 28% had some form of respiratory support and 4% of patients required extra-corporeal membrane oxygenation253. Among 1,080 patients with MIS-C, intensive care admission was more likely in children aged >5 years old than in younger children, and in non-Hispanic Black patients than in non-Hispanic white patients, and coronary artery abnormalities were more common in boys than in girls254. Elevated acute-phase inflammatory markers, troponin, B-type natriuretic peptide and D-dimer levels also identified patents at risk of severe disease254. In a study evaluating 29 children with MIS-C in France, severe disease occurred in 52% of them and was associated with high persistent fever and high levels of inflammatory markers255. Although the reason for a more critical illness in the acute phase of MIS-C than in Kawasaki disease is unclear, it is thought to be linked to the cytokine storm in MIS-C256,257.
Immunological differences
In several small studies, comparative immune profiling of children with MIS-C and Kawasaki disease has been performed, to differentiate between these two disease entities. MIS-C is associated with lymphopenia, lower white blood cell and naive CD4+ T cell counts, and increased central and effector memory T cell subpopulations, compared with Kawasaki disease103. IL-17 is a mediator of inflammation in Kawasaki disease, but is less prominent in MIS-C103. In a comparison of cytokine profiles, levels of circulating IFNγ were significantly higher in patients with severe forms of MIS-C than in those with milder MIS-C or Kawasaki disease258.
In a study of the immunological profiles of paediatric patients, 75% of those with MIS-C, but none with Kawasaki disease, TSS or COVID-19, displayed non-HLA-biased, SARS-CoV-2 non-reactive, polyclonal expansion of TCR Vβ 21.3+ activated CD4+ and CD8+ T cells165. Notably, these Vβ 21.3+ T cells had high expression of CX3CR1, a marker previously identified on the activated CD8+ T cells of patients with MIS-C185. The remarkable specificity of Vβ 21.3+ T cell subset expansion noted in MIS-C is consistent with superantigen-mediated activation of the immune system163, whereas in Kawasaki disease, evidence of a role of superantigens in pathogenesis is lacking50.
Autoantibody profiles have been compared in patients with MIS-C and Kawasaki disease103. Levels of antibodies to some vascular endothelial cell proteins, such as endoglin, were higher in both groups of patients than in healthy controls, whereas some autoantibodies (such as that to EGF-like repeat and discoidin I-like domain-containing protein 3) were overexpressed in Kawasaki disease compared with MIS-C. To confound matters, plasma levels of endoglin were elevated in both sets of patients compared with healthy children, raising the possibility that antibodies to endothelial cells were the result, rather than the cause, of vascular damage. Another possibility is that the S protein superantigen of SARS-CoV-2 might cause aberrant activation of B cells162.
Some laboratory parameters are important differentiators between Kawasaki disease and MIS-C. Although both syndromes involve a diffuse hyperinflammatory response, patients with MIS-C tend to have a lower platelet count, lower absolute lymphocyte count and higher levels of C-reactive protein, N-terminal pro-B-type natriuretic peptide, troponin and ferritin16,17,20,94,100–114,164. Additionally, coagulation abnormalities are common, including elevation of D-dimer and fibrinogen levels11,12,257,259. Hyponatraemia is another common laboratory finding in patients with MIS-C127. The presence of burr cells and neutrophils with toxic granulation can also discriminate MIS-C from severe COVID-19 (ref.150). Finally, evidence of recent SARS-CoV-2 infection, particularly by positive serology, is a diagnostic indicator of MIS-C148,149.
Conclusion
Epidemiological and clinical differences reveal that although MIS-C has phenotypic similarities to Kawasaki disease, they are different syndromes. They have varying degrees of hyperinflammation and dysregulated immune responses131. Children with MIS-C are, in general, more critically ill, with prominent gastrointestinal symptoms, cardiac involvement with shock, haematological abnormalities and elevated acute-phase reactants. They have positive SARS-CoV-2 serology, suggesting a link to prior clinical or subclinical infection or exposure. It is likely that a combination of pathogen and host factors is involved in the genesis of an intense aberrant activation of both innate and adaptive immune responses and subsequent cytokine storm16,18. Some of the pathogen-related factors include antigen mimicry of host antigens, and superantigen properties of viral proteins. Potential host factors include age and immune-system immaturity, altered intestinal microbiota, nutritional deficiencies and genetic (including inborn errors of immunity) and epigenetic predisposition13. However, to what extent each of these factors contributes, and how they interact to cause the clinical syndrome, are relative unknowns that need further exploration. Various lines of evidence based on inflammatory parameters, clinical signs or gene analyses have evoked the possibility that MIS-C is a heterogeneous complex disorder. Current data on the immune signatures in patients with MIS-C are based on small sample size, non-homogeneous cohorts. Hence, analysis of dynamic changes in the immune signatures of patients with MIS-C and their comparison with those with Kawasaki disease in a large homogeneous cohort is needed, to accurately determine the similarities and distinct features of the two disease entities. Nevertheless, with the evidence of elevation of signatures of autoimmunity in MIS-C, and reports of various post-COVID-19 conditions in adults, long-term follow-up of patients with MIS-C might be advisable, because of the possibility of relapse. Notably, however, relapse is rare in Kawasaki disease, which might suggest that recurrence is also unlikely in MIS-C.
While researchers and clinicians navigate the possibilities and evaluate the best treatment options for patients affected by COVID-19-related illnesses, it is imperative to establish registries and dedicated multidisciplinary research teams to investigate the pathogenesis and specific therapeutic strategies in MIS-C. An important step towards this end was the workshop that was convened by the NIH in June 2020, which aimed to bring together the experts on the subject, to initiate dialogue leading to future studies260. In conclusion, MIS-C has important epidemiological, clinical and immunological differences from Kawasaki disease, enabling its classification as a separate syndrome. Study of MIS-C will continue to enhance our understanding of these conditions that are related by their association with the cytokine storm phenomenon.
Acknowledgements
The work of J.B. is supported by Agence Nationale de la Recherche, France (Flash COVID-19; ANR-20-COVI-0093-COVIMUNE).
Author contributions
C.S., M.G. and J.B. researched data for the article. C.S., M.G. and J.B. wrote the article. All authors provided substantial contribution to discussion of the content, and reviewed and approved the text before submission.
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information
Nature Reviews Rheumatology thanks H. Bassiri, who co-reviewed with A. Blatz (ECR), and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Chetan Sharma, Madhusudan Ganigara.
Contributor Information
Chetan Sharma, Email: Chetan.Sharma@bcm.edu.
Jagadeesh Bayry, Email: bayry@iitpkd.ac.in.
References
- 1.Lai C-C, et al. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int. J. Antimicrob. Agents. 2020;55:105946. doi: 10.1016/j.ijantimicag.2020.105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Med. Atenei Parm. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bikdeli B, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Montalvan V, Lee J, Bueso T, De Toledo J, Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin. Neurol. Neurosurg. 2020;194:105921. doi: 10.1016/j.clineuro.2020.105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clerkin KJ, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman JIE, Kaplan S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002;39:1890–1900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 7.Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor. Rev. 2020;53:25–32. doi: 10.1016/j.cytogfr.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ou X, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat. Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffmann M, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and Is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu J, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020;55:102763. doi: 10.1016/j.ebiom.2020.102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verdoni L, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395:1771–1778. doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feldstein LR, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N. Engl. J. Med. 2020;383:334–346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dufort EM, et al. Multisystem inflammatory syndrome in children in New York State. N. Engl. J. Med. 2020;383:347–358. doi: 10.1056/NEJMoa2021756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheung EW, et al. Multisystem inflammatory syndrome related to COVID-19 in previously healthy children and adolescents in New York City. JAMA. 2020;324:294–296. doi: 10.1001/jama.2020.10374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galeotti C, Bayry J. Autoimmune and inflammatory diseases following COVID-19. Nat. Rev. Rheumatol. 2020;16:413–414. doi: 10.1038/s41584-020-0448-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simpson JM, Newburger JW. Multi-system inflammatory syndrome in children in association with COVID-19. Circulation. 2020;142:437–440. doi: 10.1161/CIRCULATIONAHA.120.048726. [DOI] [PubMed] [Google Scholar]
- 18.Levin M. Childhood multisystem inflammatory syndrome — a new challenge in the pandemic. N. Engl. J. Med. 2020;383:393–395. doi: 10.1056/NEJMe2023158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi. 1967;16:178–222. [PubMed] [Google Scholar]
- 20.McCrindle Brian W, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–e999. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 21.Burns JC, et al. Genetic variations in the receptor-ligand pair CCR5 and CCL3L1 are important determinants of susceptibility to Kawasaki disease. J. Infect. Dis. 2005;192:344–349. doi: 10.1086/430953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burgner D, et al. A genome-wide association study identifies novel and functionally related susceptibility loci for Kawasaki disease. PLoS Genet. 2009;5:e1000319. doi: 10.1371/journal.pgen.1000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burgner D, Harnden A. Kawasaki disease: what is the epidemiology telling us about the etiology? Int. J. Infect. Dis. 2005;9:185–194. doi: 10.1016/j.ijid.2005.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Son MBF, Newburger JW. Kawasaki disease. Pediatr. Rev. 2018;39:78–90. doi: 10.1542/pir.2016-0182. [DOI] [PubMed] [Google Scholar]
- 25.Burns JC. The riddle of Kawasaki disease. N. Engl. J. Med. 2007;356:659–661. doi: 10.1056/NEJMp068268. [DOI] [PubMed] [Google Scholar]
- 26.Holman RC, Curns AT, Belay ED, Steiner CA, Schonberger LB. Kawasaki syndrome hospitalizations in the United States, 1997 and 2000. Pediatrics. 2003;112:495–501. doi: 10.1542/peds.112.3.495. [DOI] [PubMed] [Google Scholar]
- 27.Kuijpers TW, et al. Kawasaki disease: a maturational defect in immune responsiveness. J. Infect. Dis. 1999;180:1869–1877. doi: 10.1086/315111. [DOI] [PubMed] [Google Scholar]
- 28.Green MS. The male predominance in the incidence of infectious diseases in children: a postulated explanation for disparities in the literature. Int. J. Epidemiol. 1992;21:381–386. doi: 10.1093/ije/21.2.381. [DOI] [PubMed] [Google Scholar]
- 29.Burgner D, Levin M. Genetic susceptibility to infectious diseases. Pediatr. Infect. Dis. J. 2003;22:1–6. doi: 10.1097/00006454-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Harnden A, Alves B, Sheikh A. Rising incidence of Kawasaki disease in England: analysis of hospital admission data. BMJ. 2002;324:1424–1425. doi: 10.1136/bmj.324.7351.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bell DM, Morens DM, Holman RC, Hurwitz ES, Hunter MK. Kawasaki syndrome in the United States 1976 to 1980. Am. J. Dis. Child. 1983;137:211–214. doi: 10.1001/archpedi.1983.02140290003001. [DOI] [PubMed] [Google Scholar]
- 32.Chang R-KR. Hospitalizations for Kawasaki disease among children in the United States, 1988–1997. Pediatrics. 2002;109:e87. doi: 10.1542/peds.109.6.e87. [DOI] [PubMed] [Google Scholar]
- 33.Du Z-D, et al. Epidemiologic picture of Kawasaki disease in Beijing from 1995 through 1999. Pediatr. Infect. Dis. J. 2002;21:103–107. doi: 10.1097/00006454-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Park Y-W, et al. Epidemiologic study of Kawasaki disease in Korea, 1997-1999: comparison with previous studies during 1991-1996. J. Korean Med. Sci. 2002;17:453–456. doi: 10.3346/jkms.2002.17.4.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uehara R, Belay ED. Epidemiology of Kawasaki disease in Asia, Europe, and the United States. J. Epidemiol. 2012;22:79–85. doi: 10.2188/jea.JE20110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yanagawa H, Yashiro M, Nakamura Y, Kawasaki T, Kato H. Results of 12 nationwide epidemiological incidence surveys of Kawasaki disease in Japan. Arch. Pediatr. Adolesc. Med. 1995;149:779–783. doi: 10.1001/archpedi.1995.02170200069011. [DOI] [PubMed] [Google Scholar]
- 37.Burns JC, et al. Seasonality and temporal clustering of Kawasaki syndrome. Epidemiology. 2005;16:220–225. doi: 10.1097/01.ede.0000152901.06689.d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakamura Y, Yanagawa I, Kawasaki T. Temporal and geographical clustering of Kawasaki disease in Japan. Prog. Clin. Biol. Res. 1987;250:19–32. [PubMed] [Google Scholar]
- 39.Yanagawa H, Nakamura Y, Kawasaki T, Shigematsu I. Nationwide epidemic of Kawasaki disease in Japan during winter of 1985-86. Lancet. 1986;2:1138–1139. doi: 10.1016/s0140-6736(86)90541-6. [DOI] [PubMed] [Google Scholar]
- 40.Chang L-Y, et al. Viral infections associated with Kawasaki disease. J. Formos. Med. Assoc. 2014;113:148–154. doi: 10.1016/j.jfma.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Benseler SM, et al. Infections and Kawasaki disease: implications for coronary artery outcome. Pediatrics. 2005;116:e760–e766. doi: 10.1542/peds.2005-0559. [DOI] [PubMed] [Google Scholar]
- 42.Esper F, et al. Association between a novel human coronavirus and Kawasaki disease. J. Infect. Dis. 2005;191:499–502. doi: 10.1086/428291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rowley AH, et al. Detection of antigen in bronchial epithelium and macrophages in acute Kawasaki disease by use of synthetic antibody. J. Infect. Dis. 2004;190:856–865. doi: 10.1086/422648. [DOI] [PubMed] [Google Scholar]
- 44.Cohen E, Sundel R. Kawasaki disease at 50 years. JAMA Pediatr. 2016;170:1093–1099. doi: 10.1001/jamapediatrics.2016.1446. [DOI] [PubMed] [Google Scholar]
- 45.Rowley AH. Is Kawasaki disease an infectious disorder? Int. J. Rheum. Dis. 2018;21:20–25. doi: 10.1111/1756-185X.13213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abe J, et al. Selective expansion of T cells expressing T-cell receptor variable regions Vβ2 and Vβ 8 in Kawasaki disease. Proc. Natl Acad. Sci. USA. 1992;89:4066–4070. doi: 10.1073/pnas.89.9.4066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abe J, et al. Characterization of T cell repertoire changes in acute Kawasaki disease. J. Exp. Med. 1993;177:791–796. doi: 10.1084/jem.177.3.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Curtis N, Zheng R, Lamb JR, Levin M. Evidence for a superantigen mediated process in Kawasaki disease. Arch. Dis. Child. 1995;72:308–311. doi: 10.1136/adc.72.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nagata S, et al. Heat shock proteins and superantigenic properties of bacteria from the gastrointestinal tract of patients with Kawasaki disease. Immunology. 2009;128:511–520. doi: 10.1111/j.1365-2567.2009.03135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pietra BA, Inocencio JD, Giannini EH, Hirsch R. TCR Vβ family repertoire and T cell activation markers in Kawasaki disease. J. Immunol. 1994;153:1881–1888. [PubMed] [Google Scholar]
- 51.Mancia L, et al. Characterization of the T-cell receptor V-β repertoire in Kawasaki disease. Scand. J. Immunol. 1998;48:443–449. doi: 10.1046/j.1365-3083.1998.00415.x. [DOI] [PubMed] [Google Scholar]
- 52.Jun JS, Jung YK, Lee DW. Relationship between vitamin D levels and intravenous immunoglobulin resistance in Kawasaki disease. Korean J. Pediatr. 2017;60:216–220. doi: 10.3345/kjp.2017.60.7.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Canning MO, Grotenhuis K, de Wit H, Ruwhof C, Drexhage HA. 1-α,25-Dihydroxyvitamin D3 (1,25(OH)(2)D(3)) hampers the maturation of fully active immature dendritic cells from monocytes. Eur. J. Endocrinol. 2001;145:351–357. doi: 10.1530/eje.0.1450351. [DOI] [PubMed] [Google Scholar]
- 54.Ben-Shoshan M, et al. 1α,25-dihydroxyvitamin D3 (Calcitriol) inhibits hypoxia-inducible factor-1/vascular endothelial growth factor pathway in human cancer cells. Mol. Cancer Ther. 2007;6:1433–1439. doi: 10.1158/1535-7163.MCT-06-0677. [DOI] [PubMed] [Google Scholar]
- 55.Meyer K, et al. Breastfeeding and vitamin D supplementation reduce the risk of Kawasaki disease in a German population-based case-control study. BMC Pediatr. 2019;19:66. doi: 10.1186/s12887-019-1438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stagi S, Rigante D, Lepri G, Matucci Cerinic M, Falcini F. Severe vitamin D deficiency in patients with Kawasaki disease: a potential role in the risk to develop heart vascular abnormalities? Clin. Rheumatol. 2016;35:1865–1872. doi: 10.1007/s10067-015-2970-6. [DOI] [PubMed] [Google Scholar]
- 57.Chen Y-L, Wang J-L, Li W-Q. Prediction of the risk of coronary arterial lesions in Kawasaki disease by serum 25-hydroxyvitamin D3. Eur. J. Pediatr. 2014;173:1467–1471. doi: 10.1007/s00431-014-2346-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim S, Eun LY. Iron deficiency anemia as a predictor of coronary artery abnormalities in Kawasaki disease. Korean J. Pediatr. 2019;62:301–306. doi: 10.3345/kjp.2018.06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Belkaid Y, Hand T. Role of the microbiota in immunity and inflammation. Cell. 2014;157:121–141. doi: 10.1016/j.cell.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kaneko K, Akagawa S, Akagawa Y, Kimata T, Tsuji S. Our evolving understanding of Kawasaki disease pathogenesis: role of the gut microbiota. Front. Immunol. 2020;11:1616. doi: 10.3389/fimmu.2020.01616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yamashiro Y, Nagata S, Ohtsuka Y, Oguchi S, Shimizu T. Microbiologic studies on the small intestine in Kawasaki disease. Pediatr. Res. 1996;39:622–624. doi: 10.1203/00006450-199604000-00010. [DOI] [PubMed] [Google Scholar]
- 62.Takeshita S, Kobayashi I, Kawamura Y, Tokutomi T, Sekine I. Characteristic profile of intestinal microflora in Kawasaki disease. Acta Paediatr. 2002;91:783–788. doi: 10.1080/08035250213221. [DOI] [PubMed] [Google Scholar]
- 63.Chen J, et al. Altered gut microbiota correlated with systemic inflammation in children with Kawasaki disease. Sci. Rep. 2020;10:14525. doi: 10.1038/s41598-020-71371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumrah R, Vignesh P, Rawat A, Singh S. Immunogenetics of Kawasaki disease. Clin. Rev. Allergy Immunol. 2020;59:122–139. doi: 10.1007/s12016-020-08783-9. [DOI] [PubMed] [Google Scholar]
- 65.Holman RC, et al. Kawasaki syndrome in Hawaii. Pediatr. Infect. Dis. J. 2005;24:429–433. doi: 10.1097/01.inf.0000160946.05295.91. [DOI] [PubMed] [Google Scholar]
- 66.Fujita Y, et al. Kawasaki disease in families. Pediatrics. 1989;84:666–669. [PubMed] [Google Scholar]
- 67.Onouchi Y, et al. Common variants in CASP3 confer susceptibility to Kawasaki disease. Hum. Mol. Genet. 2010;19:2898–2906. doi: 10.1093/hmg/ddq176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shimizu C, et al. Transforming growth factor-beta signaling pathway in patients with Kawasaki disease. Circ. Cardiovasc. Genet. 2011;4:16–25. doi: 10.1161/CIRCGENETICS.110.940858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chang L, Yang H-W, Lin T-Y, Yang KD. Perspective of immunopathogenesis and immunotherapies for Kawasaki disease. Front. Pediatr. 2021;9:697632. doi: 10.3389/fped.2021.697632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alphonse MP, et al. Inositol-triphosphate 3-kinase c mediates inflammasome activation and treatment response in Kawasaki disease. J. Immunol. 2016;197:3481–3489. doi: 10.4049/jimmunol.1600388. [DOI] [PubMed] [Google Scholar]
- 71.Onouchi Y. Molecular genetics of Kawasaki disease. Pediatr. Res. 2009;65:46R–54R. doi: 10.1203/PDR.0b013e31819dba60. [DOI] [PubMed] [Google Scholar]
- 72.Burns JC. Cyclosporine and coronary outcomes in Kawasaki disease. J. Pediatr. 2019;210:239–242. doi: 10.1016/j.jpeds.2019.04.044. [DOI] [PubMed] [Google Scholar]
- 73.Matsuda I, Hattori S, Nagata N, Fruse A, Nambu H. HLA antigens in mucocutaneous lymph node syndrome. Am. J. Dis. Child. 1977;131:1417–1418. doi: 10.1001/archpedi.1977.02120250099033. [DOI] [PubMed] [Google Scholar]
- 74.Kato S, et al. HLA antigens in Kawasaki disease. Pediatrics. 1978;61:252–255. [PubMed] [Google Scholar]
- 75.Krensky AM, Berenberg W, Shanley K, Yunis EJ. HLA antigens in mucocutaneous lymph node syndrome in New England. Pediatrics. 1981;67:741–743. [PubMed] [Google Scholar]
- 76.Sharma K, et al. Epigenetics in Kawasaki disease. Front. Pediatr. 2021;9:626. doi: 10.3389/fped.2021.673294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Assari R, et al. Pro-inflammatory cytokine single nucleotide polymorphisms in Kawasaki disease. Int. J. Rheum. Dis. 2018;21:1120–1126. doi: 10.1111/1756-185X.12911. [DOI] [PubMed] [Google Scholar]
- 78.Weng K-P, et al. IL-1B polymorphism in association with initial intravenous immunoglobulin treatment failure in Taiwanese children with Kawasaki disease. Circ. J. 2010;74:544–551. doi: 10.1253/circj.cj-09-0664. [DOI] [PubMed] [Google Scholar]
- 79.Kim J-J, et al. Identification of KCNN2 as a susceptibility locus for coronary artery aneurysms in Kawasaki disease using genome-wide association analysis. J. Hum. Genet. 2013;58:521–525. doi: 10.1038/jhg.2013.43. [DOI] [PubMed] [Google Scholar]
- 80.Kwon Y-C, et al. Identification of the TIFAB gene as a susceptibility locus for coronary artery aneurysm in patients with Kawasaki disease. Pediatr. Cardiol. 2019;40:483–488. doi: 10.1007/s00246-018-1992-7. [DOI] [PubMed] [Google Scholar]
- 81.Lu Z, et al. P2RY12:rs7637803 TT variant genotype increases coronary artery aneurysm risk in Kawasaki disease in a southern Chinese population. J. Gene Med. 2019;21:e3066. doi: 10.1002/jgm.3066. [DOI] [PubMed] [Google Scholar]
- 82.Fu LY, et al. The IL-1B gene polymorphisms rs16944 and rs1143627 contribute to an increased risk of coronary artery lesions in southern Chinese children with Kawasaki disease. J. Immunol. Res. 2019;2019:4730507. doi: 10.1155/2019/4730507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hara T, et al. Kawasaki disease: a matter of innate immunity. Clin. Exp. Immunol. 2016;186:134–143. doi: 10.1111/cei.12832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee NH, Choi HJ, Kim YH. Clinical usefulness of serum procalcitonin level in distinguishing between Kawasaki disease and other infections in febrile children. Korean J. Pediatr. 2017;60:112–117. doi: 10.3345/kjp.2017.60.4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tremoulet AH, et al. Increased incidence and severity of Kawasaki disease among Filipino-Americans in San Diego county. Pediatr. Infect. Dis. J. 2011;30:909–911. doi: 10.1097/INF.0b013e31821e52c6. [DOI] [PubMed] [Google Scholar]
- 86.Burns JC, Glodé MP. Kawasaki syndrome. Lancet. 2004;364:533–544. doi: 10.1016/S0140-6736(04)16814-1. [DOI] [PubMed] [Google Scholar]
- 87.Ikeda K, et al. Unique activation status of peripheral blood mononuclear cells at acute phase of Kawasaki disease. Clin. Exp. Immunol. 2010;160:246–255. doi: 10.1111/j.1365-2249.2009.04073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Armaroli G, et al. Monocyte-derived interleukin-1β as the driver of S100A12-induced sterile inflammatory activation of human coronary artery endothelial cells: implications for the pathogenesis of Kawasaki disease. Arthritis Rheumatol. 2019;71:792–804. doi: 10.1002/art.40784. [DOI] [PubMed] [Google Scholar]
- 89.Zhang K, et al. Increase in T helper type 17 cells in children with Kawasaki disease is NR4A2 dependent. Eur. J. Inflamm. 2018;16:2058739218760945. [Google Scholar]
- 90.Wu Y, et al. Interleukin-6 is prone to be a candidate biomarker for predicting incomplete and IVIG nonresponsive Kawasaki disease rather than coronary artery aneurysm. Clin. Exp. Med. 2019;19:173–181. doi: 10.1007/s10238-018-00544-5. [DOI] [PubMed] [Google Scholar]
- 91.Oharaseki T, et al. The role of TNF-α in a murine model of Kawasaki disease arteritis induced with a Candida albicans cell wall polysaccharide. Mod. Rheumatol. 2014;24:120–128. doi: 10.3109/14397595.2013.854061. [DOI] [PubMed] [Google Scholar]
- 92.Lin CY, Lin CC, Hwang B, Chiang B. Serial changes of serum interleukin-6, interleukin-8, and tumor necrosis factor alpha among patients with Kawasaki disease. J. Pediatr. 1992;121:924–926. doi: 10.1016/s0022-3476(05)80343-9. [DOI] [PubMed] [Google Scholar]
- 93.Guo MM-H, et al. Th17- and Treg-related cytokine and mRNA expression are associated with acute and resolving Kawasaki disease. Allergy. 2015;70:310–318. doi: 10.1111/all.12558. [DOI] [PubMed] [Google Scholar]
- 94.Lin C-Y, Lin C-C, Hwang B, Chiang BN. Cytokines predict coronary aneurysm formation in Kawasaki disease patients. Eur. J. Pediatr. 1993;152:309–312. doi: 10.1007/BF01956740. [DOI] [PubMed] [Google Scholar]
- 95.Rahmani F, et al. Interleukin 10 and and transforming growth factor β polymorphisms as risk factors for Kawasaki disease: a case-control study and meta-analysis. Avicenna J. Med. Biotechnol. 2019;11:325–333. [PMC free article] [PubMed] [Google Scholar]
- 96.Jia S, Li C, Wang G, Yang J, Zu Y. The T helper type 17/regulatory T cell imbalance in patients with acute Kawasaki disease. Clin. Exp. Immunol. 2010;162:131–137. doi: 10.1111/j.1365-2249.2010.04236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yoshida Y, et al. Enhanced formation of neutrophil extracellular traps in Kawasaki disease. Pediatr. Res. 2020;87:998–1004. doi: 10.1038/s41390-019-0710-3. [DOI] [PubMed] [Google Scholar]
- 98.Papayannopoulos V. Neutrophil extracellular traps in immunity and disease. Nat. Rev. Immunol. 2018;18:134–147. doi: 10.1038/nri.2017.105. [DOI] [PubMed] [Google Scholar]
- 99.Garcia-Romo GS, et al. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci. Transl. Med. 2011;3:73ra20. doi: 10.1126/scitranslmed.3001201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kessenbrock K, et al. Netting neutrophils in autoimmune small-vessel vasculitis. Nat. Med. 2009;15:623–625. doi: 10.1038/nm.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Corsiero E, Pratesi F, Prediletto E, Bombardieri M, Migliorini P. NETosis as source of autoantigens in rheumatoid arthritis. Front. Immunol. 2016;7:485. doi: 10.3389/fimmu.2016.00485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Grunebaum E, et al. The role of anti-endothelial cell antibodies in Kawasaki disease – in vitro and in vivo studies. Clin. Exp. Immunol. 2002;130:233–240. doi: 10.1046/j.1365-2249.2002.02000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Consiglio CR, et al. The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell. 2020;183:968–981.e7. doi: 10.1016/j.cell.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sakurai Y. Autoimmune aspects of Kawasaki disease. J. Investig. Allergol. Clin. Immunol. 2019;29:251–261. doi: 10.18176/jiaci.0300. [DOI] [PubMed] [Google Scholar]
- 105.Nash MC, Shah V, Reader JA, Dillon MJ. Anti-neutrophil cytoplasmic antibodies and anti-endothelial cell antibodies are not increased in Kawasaki disease. Rheumatology. 1995;34:882–887. doi: 10.1093/rheumatology/34.9.882. [DOI] [PubMed] [Google Scholar]
- 106.Li CR, Yang XQ, Shen J, Li YB, Jiang LP. Immunoglobulin G subclasses in serum and circulating immune complexes in patients with Kawasaki syndrome. Pediatr. Infect. Dis. J. 1990;9:544–547. doi: 10.1097/00006454-199008000-00003. [DOI] [PubMed] [Google Scholar]
- 107.Levin M, et al. Platelet immune complex interaction in pathogenesis of Kawasaki disease and childhood polyarteritis. Br. Med. J. Clin. Res. Ed. 1985;290:1456–1460. doi: 10.1136/bmj.290.6480.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Miyata K, et al. Circulation immune complexes and granulocytes chemotaxis in Kawasaki disease: the 8th conference on prevention for rheumatic fever and rheumatic heart disease. Jpn. Circ. J. 1984;48:1350–1353. doi: 10.1253/jcj.48.1350. [DOI] [PubMed] [Google Scholar]
- 109.Ono S, Onimaru T, Kawakami K, Hokonohara M, Miyata K. Impaired granulocyte chemotaxis and increased circulating immune complexes in Kawasaki disease. J. Pediatr. 1985;106:567–570. doi: 10.1016/s0022-3476(85)80073-1. [DOI] [PubMed] [Google Scholar]
- 110.Kohsaka T, Abe J, Asahina T, Kobayashi N. Classical pathway complement activation in Kawasaki syndrome. J. Allergy Clin. Immunol. 1994;93:520–525. doi: 10.1016/0091-6749(94)90362-x. [DOI] [PubMed] [Google Scholar]
- 111.Biezeveld MH, et al. Polymorphisms in the mannose-binding lectin gene as determinants of age-defined risk of coronary artery lesions in Kawasaki disease. Arthritis Rheum. 2006;54:369–376. doi: 10.1002/art.21529. [DOI] [PubMed] [Google Scholar]
- 112.Ohshio G, et al. High levels of IgA-containing circulating immune complex and secretory IgA in Kawasaki disease. Microbiol. Immunol. 1987;31:891–898. doi: 10.1111/j.1348-0421.1987.tb03150.x. [DOI] [PubMed] [Google Scholar]
- 113.Noval Rivas M, Arditi M. Kawasaki disease: pathophysiology and insights from mouse models. Nat. Rev. Rheumatol. 2020;16:391–405. doi: 10.1038/s41584-020-0426-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Noval Rivas M, et al. Intestinal permeability and IgA provoke immune vasculitis linked to cardiovascular inflammation. Immunity. 2019;51:508–521.e6. doi: 10.1016/j.immuni.2019.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Olivito B, et al. Defective FOXP3 expression in patients with acute Kawasaki disease and restoration by intravenous immunoglobulin therapy. Clin. Exp. Rheumatol. 2010;28:93–97. [PubMed] [Google Scholar]
- 116.Abe J, et al. Gene expression profiling of the effect of high-dose intravenous Ig in patients with Kawasaki disease. J. Immunol. 2005;174:5837–5845. doi: 10.4049/jimmunol.174.9.5837. [DOI] [PubMed] [Google Scholar]
- 117.Yoshimura K, et al. Increased nitric oxide production by neutrophils in early stage of Kawasaki disease. Eur. J. Pediatr. 2009;168:1037–1041. doi: 10.1007/s00431-008-0872-1. [DOI] [PubMed] [Google Scholar]
- 118.Wang Y, et al. Evaluation of intravenous immunoglobulin resistance and coronary artery lesions in relation to Th1/Th2 cytokine profiles in patients with Kawasaki disease. Arthritis Rheum. 2013;65:805–814. doi: 10.1002/art.37815. [DOI] [PubMed] [Google Scholar]
- 119.Zhu YP, et al. Immune response to intravenous immunoglobulin in patients with Kawasaki disease and MIS-C. J. Clin. Invest. 2021 doi: 10.1172/JCI147076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang Z, et al. Single-cell RNA sequencing of peripheral blood mononuclear cells from acute Kawasaki disease patients. Nat. Commun. 2021;12:5444. doi: 10.1038/s41467-021-25771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rambabu N, Mathew MJ, Kaveri SV, Bayry J. Boolean analysis of the transcriptomic data to identify novel biomarkers of IVIG response. Autoimmun. Rev. 2021;20:102850. doi: 10.1016/j.autrev.2021.102850. [DOI] [PubMed] [Google Scholar]
- 122.Belhadjer Z, et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation. 2020;142:429–436. doi: 10.1161/CIRCULATIONAHA.120.048360. [DOI] [PubMed] [Google Scholar]
- 123.CDC. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). Health Alert Networkhttps://emergency.cdc.gov/han/2020/han00432.asp (2020).
- 124.CDC. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker (2020).
- 125.Kaushik S, et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): a multi-institutional study from New York City. J. Pediatr. 2020;224:24–29. doi: 10.1016/j.jpeds.2020.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Davies P, et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: a multicentre observational study. Lancet Child Adolesc. Health. 2020;4:669–677. doi: 10.1016/S2352-4642(20)30215-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pouletty M, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann. Rheum. Dis. 2020;79:999–1006. doi: 10.1136/annrheumdis-2020-217960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Toubiana J, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094. doi: 10.1136/bmj.m2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Capone CA, et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 Infection. J. Pediatr. 2020;224:141–145. doi: 10.1016/j.jpeds.2020.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hameed S, et al. Spectrum of imaging findings on chest radiographs, US, CT, and MRI images in multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19. Radiology. 2020;298:E1–E10. doi: 10.1148/radiol.2020202543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Whittaker E, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324:259–269. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Moraleda C, et al. Multi-inflammatory syndrome in children related to SARS-CoV-2 in Spain. Clin. Infect. Dis. 2020;72:e397–e401. doi: 10.1093/cid/ciaa1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Dhanalakshmi K, et al. Epidemiological and clinical profile of pediatric inflammatory multisystem syndrome — temporally associated with SARS-CoV-2 (PIMS-TS) in Indian children. Indian. Pediatr. 2020;57:1010–1014. doi: 10.1007/s13312-020-2025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Miller J, et al. Gastrointestinal symptoms as a major presentation component of a novel multisystem inflammatory syndrome in children that is related to coronavirus disease 2019: a single center experience of 44 cases. Gastroenterology. 2020;159:1571–1574.e2. doi: 10.1053/j.gastro.2020.05.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Belot A, et al. SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020. Eurosurveillance. 2020;25:2001010. doi: 10.2807/1560-7917.ES.2020.25.22.2001010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lee PY, et al. Distinct clinical and immunological features of SARS–CoV-2–induced multisystem inflammatory syndrome in children. J. Clin. Invest. 2020;130:5942–5950. doi: 10.1172/JCI141113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Riollano-Cruz M, et al. Multisystem inflammatory syndrome in children related to COVID-19: a New York City experience. J. Med. Virol. 2021;93:424–433. doi: 10.1002/jmv.26224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ramcharan T, et al. Paediatric inflammatory multisystem syndrome: temporally associated with SARS-CoV-2 (PIMS-TS): cardiac features, management and short-term outcomes at a UK tertiary paediatric hospital. Pediatr. Cardiol. 2020;41:1391–1401. doi: 10.1007/s00246-020-02391-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Grimaud M, et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann. Intensive Care. 2020;10:69. doi: 10.1186/s13613-020-00690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Perez-Toledo M, et al. SARS-CoV-2-specific IgG1/IgG3 but not IgM in children with pediatric inflammatory multi-system syndrome. Pediatr. Allergy Immunol. 2021;32:1125–1129. doi: 10.1111/pai.13504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.RCPCH. Paediatric multisystem inflammatory syndrome temporally associated with COVID-19. https://www.rcpch.ac.uk/resources/guidance-paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19 (2020).
- 142.WHO. Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19. https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (2020).
- 143.Carlin RF, et al. Discriminating multisystem inflammatory syndrome in children requiring treatment from common febrile conditions in outpatient settings. J. Pediatr. 2021;229:26–32.e2. doi: 10.1016/j.jpeds.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Roberts JE, et al. Differentiating multisystem inflammatory syndrome in children: a single-centre retrospective cohort study. Arch. Dis. Child. 2021 doi: 10.1136/archdischild-2021-322290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.García-Salido A, et al. Severe manifestations of SARS-CoV-2 in children and adolescents: from COVID-19 pneumonia to multisystem inflammatory syndrome: a multicentre study in pediatric intensive care units in Spain. Crit. Care. 2020;24:666. doi: 10.1186/s13054-020-03332-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hoang A, et al. COVID-19 in 7780 pediatric patients: a systematic review. EClinicalMedicine. 2020;24:100433. doi: 10.1016/j.eclinm.2020.100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mahase E. Covid-19: cases of inflammatory syndrome in children surge after urgent alert. BMJ. 2020;369:m1990. doi: 10.1136/bmj.m1990. [DOI] [PubMed] [Google Scholar]
- 148.Henderson LA, et al. American College of Rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS–CoV-2 and Hyperinflammation in pediatric COVID-19: Version 1. Arthritis Rheumatol. 2020;72:1791–1805. doi: 10.1002/art.41454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Henderson LA, et al. American College of Rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19: Version 2. Arthritis Rheumatol. 2021;73:e13–e29. doi: 10.1002/art.41616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Diorio C, et al. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS–CoV-2. J. Clin. Invest. 2020;130:5967–5975. doi: 10.1172/JCI140970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Duarte-Neto AN, et al. An autopsy study of the spectrum of severe COVID-19 in children: from SARS to different phenotypes of MIS-C. EclinicalMed. 2021;35:100850. doi: 10.1016/j.eclinm.2021.100850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Yonker LM, et al. Multisystem inflammatory syndrome in children is driven by zonulin-dependent loss of gut mucosal barrier. J. Clin. Invest. 2021;131:149633. doi: 10.1172/JCI149633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ramaswamy A, et al. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity. 2021;54:1083–1095.e7. doi: 10.1016/j.immuni.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Gruber CN, et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C) Cell. 2020;183:982–995.e14. doi: 10.1016/j.cell.2020.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Rostad CA, et al. Quantitative SARS-CoV-2 serology in children with multisystem inflammatory syndrome (MIS-C) Pediatrics. 2020;146:e2020018242. doi: 10.1542/peds.2020-018242. [DOI] [PubMed] [Google Scholar]
- 156.Weisberg SP, et al. Distinct antibody responses to SARS-CoV-2 in children and adults across the COVID-19 clinical spectrum. Nat. Immunol. 2021;22:25–31. doi: 10.1038/s41590-020-00826-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Anderson EM, et al. SARS-CoV-2 antibody responses in children with MIS-C and mild and severe COVID-19. J. Pediatr. Infect. Dis. Soc. 2020;10:669–673. doi: 10.1093/jpids/piaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bartsch YC, et al. Humoral signatures of protective and pathological SARS-CoV-2 infection in children. Nat. Med. 2021;27:454–462. doi: 10.1038/s41591-021-01263-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mateus J, et al. Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science. 2020;370:89–94. doi: 10.1126/science.abd3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Grifoni A, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181:1489–1501.e15. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Sermet-Gaudelus I, et al. Prior infection by seasonal coronaviruses, as assessed by serology, does not prevent SARS-CoV-2 infection and disease in children, France, April to June 2020. Eur. Surveill. 2021;26:2001782. doi: 10.2807/1560-7917.ES.2021.26.13.2001782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Rivas MN, Porritt RA, Cheng MH, Bahar I, Arditi M. COVID-19–associated multisystem inflammatory syndrome in children (MIS-C): a novel disease that mimics toxic shock syndrome — the superantigen hypothesis. J. Allergy Clin. Immunol. 2021;147:57–59. doi: 10.1016/j.jaci.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Cheng MH, et al. Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation. Proc. Natl Acad. Sci. USA. 2020;117:25254–25262. doi: 10.1073/pnas.2010722117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Porritt RA, et al. HLA class I-associated expansion of TRBV11-2 T cells in multisystem inflammatory syndrome in children. J. Clin. Invest. 2021;131:e146614. doi: 10.1172/JCI146614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Moreews M, et al. Polyclonal expansion of TCR Vβ 21.3+ CD4+ and CD8+ T cells is a hallmark of multisystem inflammatory syndrome in children. Sci. Immunol. 2021;6:eabh1516. doi: 10.1126/sciimmunol.abh1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.McCormick JK, Yarwood JM, Schlievert PM. Toxic shock syndrome and bacterial superantigens: an update. Annu. Rev. Microbiol. 2001;55:77–104. doi: 10.1146/annurev.micro.55.1.77. [DOI] [PubMed] [Google Scholar]
- 167.Radujkovic A, et al. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients. 2020;12:2757. doi: 10.3390/nu12123643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Urashima M, et al. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am. J. Clin. Nutr. 2010;91:1255–1260. doi: 10.3945/ajcn.2009.29094. [DOI] [PubMed] [Google Scholar]
- 169.Omenetti S, Pizarro TT. The Treg/TH17 axis: a dynamic balance regulated by the gut microbiome. Front. Immunol. 2015;6:639. doi: 10.3389/fimmu.2015.00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Yeoh YK, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut. 2021;70:698–706. doi: 10.1136/gutjnl-2020-323020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Zuo T, et al. Alterations in fecal fungal microbiome of patients with COVID-19 during time of hospitalization until discharge. Gastroenterology. 2020;159:1302–1310.e5. doi: 10.1053/j.gastro.2020.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Merenstein C, et al. Signatures of COVID-19 severity and immune response in the respiratory tract microbiome. mBio. 2021;12:e0177721. doi: 10.1128/mBio.01777-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zuo T, et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology. 2020;159:944–955.e8. doi: 10.1053/j.gastro.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Xu R, et al. Progressive deterioration of the upper respiratory tract and the gut microbiomes in children during the early infection stages of COVID-19. J. Genet. Genomics. 2021 doi: 10.1016/j.jgg.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Hurst, J. H. et al. Age-related changes in the upper respiratory microbiome are associated with SARS-CoV-2 susceptibility and illness severity. Preprint at medRxivhttps://www.medrxiv.org/content/10.1101/2021.03.20.21252680v1 (2021).
- 176.Chou J, et al. Mechanisms underlying genetic susceptibility to multisystem inflammatory syndrome in children (MIS-C) J. Allergy Clin. Immunol. 2021;148:732–738.e1. doi: 10.1016/j.jaci.2021.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Belay ED, et al. Trends in geographic and temporal distribution of US children with multisystem inflammatory syndrome during the COVID-19 pandemic. JAMA Pediatr. 2021;175:837–845. doi: 10.1001/jamapediatrics.2021.0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Krishnan L, Ogunwole SM, Cooper LA. Historical insights on coronavirus disease 2019 (COVID-19), the 1918 influenza pandemic, and racial disparities: illuminating a path forward. Ann. Intern. Med. 2020;173:474–481. doi: 10.7326/M20-2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J. Clin. Med. 2020;9:2442. doi: 10.3390/jcm9082442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Rafferty MS, et al. Multisystem inflammatory syndrome in children (MIS-C) and the coronavirus pandemic: current knowledge and implications for public health. J. Infect. Public Health. 2021;14:484–494. doi: 10.1016/j.jiph.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Nguyen A, et al. Human leukocyte antigen susceptibility map for severe acute respiratory syndrome coronavirus 2. J. Virol. 2020;94:e00510–e00520. doi: 10.1128/JVI.00510-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zhang Q, et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370:eabd4570v. doi: 10.1126/science.abd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Bastard P, et al. Insufficient type I IFN immunity underlies life-threatening COVID-19 pneumonia. C. R. Biol. 2021;344:19–25. doi: 10.5802/crbiol.36. [DOI] [PubMed] [Google Scholar]
- 184.Lee PY, et al. Immune dysregulation and multisystem inflammatory syndrome in children (MIS-C) in individuals with haploinsufficiency of SOCS1. J. Allergy Clin. Immunol. 2020;146:1194–1200.e1. doi: 10.1016/j.jaci.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Vella LA, et al. Deep immune profiling of MIS-C demonstrates marked but transient immune activation compared to adult and pediatric COVID-19. Sci. Immunol. 2021;6:eabf7570. doi: 10.1126/sciimmunol.abf7570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Carter MJ, et al. Peripheral immunophenotypes in children with multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Nat. Med. 2020;26:1701–1707. doi: 10.1038/s41591-020-1054-6. [DOI] [PubMed] [Google Scholar]
- 187.Pierce CA, et al. Immune responses to SARS-CoV-2 infection in hospitalized pediatric and adult patients. Sci. Transl. Med. 2020;12:eabd5487. doi: 10.1126/scitranslmed.abd5487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Caldarale F, et al. Plasmacytoid dendritic cells depletion and elevation of IFN-γ dependent chemokines CXCL9 and CXCL10 in children with multisystem inflammatory syndrome. Front. Immunol. 2021;12:654587. doi: 10.3389/fimmu.2021.654587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Peart Akindele N, et al. Distinct cytokine and chemokine dysregulation in hospitalized children with acute COVID-19 and multisystem inflammatory syndrome with similar levels of nasopharyngeal SARS-CoV-2 shedding. J. Infect. Dis. 2021;224:606–615. doi: 10.1093/infdis/jiab285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Diorio, C. et al. Proteomic profiling of MIS-C patients reveals heterogeneity relating to interferon gamma dysregulation and vascular endothelial dysfunction. Preprint at medRxivhttps://www.medrxiv.org/content/10.1101/2021.04.13.21255439v1 (2021). [DOI] [PMC free article] [PubMed]
- 191.Zuo Y, et al. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020;5:e138999. doi: 10.1172/jci.insight.138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Middleton EA, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Yamashita K, Takaori-Kondo A, Mizugishi K. Exaggerated neutrophil extracellular trap formation in Kawasaki disease: a key phenomenon behind the outbreak in western countries? Ann. Rheum. Dis. 2020 doi: 10.1136/annrheumdis-2020-218593. [DOI] [PubMed] [Google Scholar]
- 194.Seery V, et al. Blood neutrophils from children with COVID-19 exhibit both inflammatory and anti-inflammatory markers. EBioMedicine. 2021;67:103357. doi: 10.1016/j.ebiom.2021.103357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Beckmann ND, et al. Downregulation of exhausted cytotoxic T cells in gene expression networks of multisystem inflammatory syndrome in children. Nat. Commun. 2021;12:4854. doi: 10.1038/s41467-021-24981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Vojdani A, Vojdani E, Kharrazian D. Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: implications for autoimmune diseases. Front. Immunol. 2020;11:617089. doi: 10.3389/fimmu.2020.617089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.An, H. & Park, J. Molecular mimicry map (3M) of SARS-CoV-2: prediction of potentially immunopathogenic SARS-CoV-2 epitopes via a novel immunoinformatic approach. Preprint at bioRxivhttps://www.biorxiv.org/content/10.1101/2020.11.12.344424v1 (2020).
- 198.European Centre for Disease Prevention and Control. Rapid risk assessment: paediatric inflammatory multisystem syndrome and SARS-CoV-2 infection in children. https://www.ecdc.europa.eu/en/publications-data/paediatric-inflammatory-multisystem-syndrome-and-sars-cov-2-rapid-risk-assessment (2020).
- 199.Diorio C, et al. Evidence of thrombotic microangiopathy in children with SARS-CoV-2 across the spectrum of clinical presentations. Blood Adv. 2020;4:6051–6063. doi: 10.1182/bloodadvances.2020003471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Whitworth HB, et al. Rate of thrombosis in children and adolescents hospitalized with COVID-19 or MIS-C. Blood. 2021;138:190–198. doi: 10.1182/blood.2020010218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Endo Y, Takahashi M, Fujita T. Lectin complement system and pattern recognition. Immunobiology. 2006;211:283–293. doi: 10.1016/j.imbio.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 202.Watanabe Y, Allen JD, Wrapp D, McLellan JS, Crispin M. Site-specific glycan analysis of the SARS-CoV-2 spike. Science. 2020;369:330–333. doi: 10.1126/science.abb9983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Polycarpou A, Grigoriadou S, Klavinskis L, Sacks S. Does the lectin complement pathway link Kawasaki disease and SARS-CoV-2? Front. Immunol. 2020;11:604512. doi: 10.3389/fimmu.2020.604512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Dove ML, et al. Multisystem inflammatory syndrome in children: survey of protocols for early hospital evaluation and management. J. Pediatr. 2021;229:33–40. doi: 10.1016/j.jpeds.2020.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Jonat B, et al. Multisystem inflammatory syndrome in children associated with coronavirus disease 2019 in a children’s hospital in New York City: patient characteristics and an institutional protocol for evaluation, management, and follow-up. Pediatr. Crit. Care Med. 2021;22:e178–e191. doi: 10.1097/PCC.0000000000002598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ouldali N, et al. Association of intravenous immunoglobulins plus methylprednisolone vs immunoglobulins alone with course of fever in multisystem inflammatory syndrome in children. JAMA. 2021;325:855–864. doi: 10.1001/jama.2021.0694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.McArdle AJ, et al. Treatment of multisystem inflammatory syndrome in children. N. Engl. J. Med. 2021;385:11–22. doi: 10.1056/NEJMoa2102968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Guillaume M-P, Reumaux H, Dubos F. Usefulness and safety of anakinra in refractory Kawasaki disease complicated by coronary artery aneurysm. Cardiol. Young. 2018;28:739–742. doi: 10.1017/S1047951117002864. [DOI] [PubMed] [Google Scholar]
- 209.Kone-Paut I, et al. The use of interleukin 1 receptor antagonist (anakinra) in Kawasaki disease: a retrospective cases series. Autoimmun. Rev. 2018;17:768–774. doi: 10.1016/j.autrev.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 210.Jiang L, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect. Dis. 2020;20:e276–e288. doi: 10.1016/S1473-3099(20)30651-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Feldstein LR, et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA. 2021;325:1074–1087. doi: 10.1001/jama.2021.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Hoste L, Van Paemel R, Haerynck F. Multisystem inflammatory syndrome in children related to COVID-19: a systematic review. Eur. J. Pediatr. 2021;180:2019–2034. doi: 10.1007/s00431-021-03993-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Xu Q-Q, et al. Evaluation of left ventricular systolic strain in children with Kawasaki disease. Pediatr. Cardiol. 2014;35:1191–1197. doi: 10.1007/s00246-014-0915-5. [DOI] [PubMed] [Google Scholar]
- 214.Surve, S. V., Joseph, S., Gajbhiye, R. K., Mahale, S. D. & Modi, D. N. A systematic review on multisystem inflammatory syndrome in children (MIS-C) with COVID-19: development of a scoring system for clinical diagnosis. Preprint at medRxivhttps://www.medrxiv.org/content/10.1101/2021.04.23.21255879v1 (2021).
- 215.Sahoo, D. et al. An AI-guided invariant signature places MIS-C with Kawasaki disease in a continuum of host immune responses. Preprint at bioRxivhttps://www.biorxiv.org/content/10.1101/2021.04.11.439347v2 (2021).
- 216.Newburger JW, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N. Engl. J. Med. 1991;324:1633–1639. doi: 10.1056/NEJM199106063242305. [DOI] [PubMed] [Google Scholar]
- 217.Abrams JY, et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2: a systematic review. J. Pediatr. 2020;226:45–54.e1. doi: 10.1016/j.jpeds.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ouldali N, et al. Emergence of Kawasaki disease related to SARS-CoV-2 infection in an epicentre of the French COVID-19 epidemic: a time-series analysis. Lancet Child. Adolesc. Health. 2020;4:662–668. doi: 10.1016/S2352-4642(20)30175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Choe YJ, et al. Surveillance of COVID-19-associated multisystem inflammatory syndrome in children, South Korea. Emerg. Infect. Dis. 2021;27:1196–1200. doi: 10.3201/eid2704.210026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Li W, Tang Y, Shi Y, Chen Y, Liu E. Why multisystem inflammatory syndrome in children has been less commonly described in Asia? Transl. Pediatr. 2020;9:873–875. doi: 10.21037/tp-20-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Son MBF, et al. Treatment of Kawasaki disease: analysis of 27 US pediatric hospitals from 2001 to 2006. Pediatrics. 2009;124:1–8. doi: 10.1542/peds.2008-0730. [DOI] [PubMed] [Google Scholar]
- 222.Coon ER, Wilkes J, Bratton SL, Srivastava R. Paediatric overdiagnosis modelled by coronary abnormality trends in Kawasaki disease. Arch. Dis. Child. 2018;103:937–941. doi: 10.1136/archdischild-2017-313694. [DOI] [PubMed] [Google Scholar]
- 223.Ghelani SJ, Kwatra NS, Spurney CF. Can coronary artery involvement in Kawasaki disease be predicted? Diagnostics. 2013;3:232–243. doi: 10.3390/diagnostics3020232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Gong GWK, McCrindle BW, Ching JC, Yeung RSM. Arthritis presenting during the acute phase of Kawasaki disease. J. Pediatr. 2006;148:800–805. doi: 10.1016/j.jpeds.2006.01.039. [DOI] [PubMed] [Google Scholar]
- 225.Blondiaux E, et al. Cardiac MRI in children with multisystem inflammatory syndrome associated with COVID-19. Radiology. 2020;297:E283–E288. doi: 10.1148/radiol.2020202288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Gaitonde M, et al. COVID-19-related multisystem inflammatory syndrome in children affects left ventricular function and global strain compared with Kawasaki disease. J. Am. Soc. Echocardiogr. 2020;33:1285–1287. doi: 10.1016/j.echo.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Jhaveri S, et al. Longitudinal echocardiographic assessment of coronary arteries and left ventricular function following multisystem inflammatory syndrome in children. J. Pediatr. 2020;228:290–293. doi: 10.1016/j.jpeds.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Gamez-Gonzalez LB, et al. Kawasaki disease shock syndrome: unique and severe subtype of Kawasaki disease. Pediatr. Int. 2018;60:781–790. doi: 10.1111/ped.13614. [DOI] [PubMed] [Google Scholar]
- 229.Tsuda E, et al. Changes in causes of sudden deaths by decade in patients with coronary arterial lesions due to Kawasaki disease. Cardiol. Young. 2005;15:481–488. doi: 10.1017/S1047951105001344. [DOI] [PubMed] [Google Scholar]
- 230.Gatterre P, et al. Kawasaki disease: an unexpected etiology of shock and multiple organ dysfunction syndrome. Intensive Care Med. 2012;38:872–878. doi: 10.1007/s00134-012-2473-8. [DOI] [PubMed] [Google Scholar]
- 231.Kanegaye JT, et al. Recognition of a Kawasaki disease shock syndrome. Pediatrics. 2009;123:e783–e789. doi: 10.1542/peds.2008-1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Li Y, et al. Kawasaki disease shock syndrome: clinical characteristics and possible use of IL-6, IL-10 and IFN-γ as biomarkers for early recognition. Pediatr. Rheumatol. 2019;17:1. doi: 10.1186/s12969-018-0303-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Ma L, Zhang Y-Y, Yu H-G. Clinical manifestations of Kawasaki disease shock syndrome. Clin. Pediatr. 2018;57:428–435. doi: 10.1177/0009922817729483. [DOI] [PubMed] [Google Scholar]
- 234.Alsaied T, et al. Review of cardiac involvement in multisystem inflammatory syndrome in children. Circulation. 2021;143:78–88. doi: 10.1161/CIRCULATIONAHA.120.049836. [DOI] [PubMed] [Google Scholar]
- 235.Valverde I, et al. Acute cardiovascular manifestations in 286 children with multisystem inflammatory syndrome associated with COVID-19 infection in Europe. Circulation. 2021;143:21–32. doi: 10.1161/CIRCULATIONAHA.120.050065. [DOI] [PubMed] [Google Scholar]
- 236.Toubiana J, et al. Distinctive features of Kawasaki disease following SARS-CoV-2 infection: a controlled study in Paris, France. J. Clin. Immunol. 2021;41:526–535. doi: 10.1007/s10875-020-00941-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Suzuki J, et al. Kawasaki disease shock syndrome in Japan and comparison with multisystem inflammatory syndrome in children in European countries. Front. Pediatr. 2021;9:625456. doi: 10.3389/fped.2021.625456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Kaneko K, Takahashi K, Fujiwara S, Maruyama T, Obinata K. Kawasaki disease followed by haemophagocytic syndrome. Eur. J. Pediatr. 1998;157:610–611. doi: 10.1007/s004310050893. [DOI] [PubMed] [Google Scholar]
- 239.Cummings C, McCarthy P, van Hoff J, Porter G. Kawasaki disease associated with reactive hemophagocytic lymphohistiocytosis. Pediatr. Infect. Dis. J. 2008;27:1116–1118. doi: 10.1097/INF.0b013e31817ecb6d. [DOI] [PubMed] [Google Scholar]
- 240.Latino GA, Manlhiot C, Yeung RSM, Chahal N, McCrindle BW. Macrophage activation syndrome in the acute phase of Kawasaki disease. J. Pediatr. Hematol. Oncol. 2010;32:527–531. doi: 10.1097/MPH.0b013e3181dccbf4. [DOI] [PubMed] [Google Scholar]
- 241.Natoli V, Rosina S, Ravelli A. Is macrophage activation syndrome in Kawasaki disease underrecognized? J. Rheumatol. 2021;48:162–164. doi: 10.3899/jrheum.200361. [DOI] [PubMed] [Google Scholar]
- 242.Jinkawa A, et al. Cytokine profile of macrophage activation syndrome associated with Kawasaki disease. Cytokine. 2019;119:52–56. doi: 10.1016/j.cyto.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 243.Aydın F, et al. Comparison of baseline laboratory findings of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis and multisystem inflammatory syndrome in children. Int. J. Rheum. Dis. 2021;24:542–547. doi: 10.1111/1756-185X.14078. [DOI] [PubMed] [Google Scholar]
- 244.Zulian F, et al. Acute surgical abdomen as presenting manifestation of Kawasaki disease. J. Pediatr. 2003;142:731–735. doi: 10.1067/mpd.2003.232. [DOI] [PubMed] [Google Scholar]
- 245.Miyake T, et al. Small bowel pseudo-obstruction in Kawasaki disease. Pediatr. Radiol. 1987;17:383–386. doi: 10.1007/BF02396613. [DOI] [PubMed] [Google Scholar]
- 246.Halepas S, et al. Oral manifestations of COVID-2019-related multisystem inflammatory syndrome in children: a review of 47 pediatric patients. J. Am. Dent. Assoc. 2021;152:202–208. doi: 10.1016/j.adaj.2020.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Saguil A, Fargo M, Grogan S. Diagnosis and management of Kawasaki disease. Am. Fam. Physician. 2015;91:365–371. [PubMed] [Google Scholar]
- 248.Chen T-H, Kao W-T, Tseng Y-H. Gastrointestinal involvements in children with COVID-related multisystem inflammatory syndrome. Gastroenterology. 2020;160:1887–1888. doi: 10.1053/j.gastro.2020.06.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.LaRovere KL, et al. Neurologic involvement in children and adolescents hospitalized in the United States for COVID-19 or multisystem inflammatory syndrome. JAMA Neurol. 2021;78:536–547. doi: 10.1001/jamaneurol.2021.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Dengler LD, et al. Cerebrospinal fluid profile in patients with acute Kawasaki disease. Pediatr. Infect. Dis. J. 1998;17:478–481. doi: 10.1097/00006454-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 251.Liu X, et al. Neurological involvement in Kawasaki disease: a retrospective study. Pediatr. Rheumatol. Online J. 2020;18:61. doi: 10.1186/s12969-020-00452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Kuo C-C, et al. Characteristics of children with Kawasaki disease requiring intensive care: 10 years’ experience at a tertiary pediatric hospital. J. Microbiol. Immunol. Infect. 2018;51:184–190. doi: 10.1016/j.jmii.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 253.Radia T, et al. Multi-system inflammatory syndrome in children & adolescents (MIS-C): a systematic review of clinical features and presentation. Paediatr. Respir. Rev. 2020;38:51–57. doi: 10.1016/j.prrv.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Abrams JY, et al. Factors linked to severe outcomes in multisystem inflammatory syndrome in children (MIS-C) in the USA: a retrospective surveillance study. Lancet Child. Adolesc. Health. 2021;5:323–331. doi: 10.1016/S2352-4642(21)00050-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Ouldali N, et al. Factors associated with severe SARS-CoV-2 infection. Pediatrics. 2021;147:e2020023432. doi: 10.1542/peds.2020-023432. [DOI] [PubMed] [Google Scholar]
- 256.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘cytokine storm’ in COVID-19. J. Infect. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Dolinger MT, et al. Pediatric Crohn disease and multisystem inflammatory syndrome in children (MIS-C) and COVID-19 treated with infliximab. J. Pediatr. Gastroenterol. Nutr. 2020;71:153–155. doi: 10.1097/MPG.0000000000002809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Esteve-Sole A, et al. Similarities and differences between the immunopathogenesis of COVID-19-related pediatric multisystem inflammatory syndrome and Kawasaki disease. J. Clin. Invest. 2021;131:e144554. doi: 10.1172/JCI144554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Al-Ghafry M, et al. Multisystem inflammatory syndrome in children (MIS-C) and the prothrombotic state: coagulation profiles and rotational thromboelastometry in a MIS-C cohort. J. Thromb. Haemost. 2021;19:1764–1770. doi: 10.1111/jth.15340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Martinez OM, Bridges ND, Goldmuntz E, Pascual V. The immune roadmap for understanding multi-system inflammatory syndrome in children: opportunities and challenges. Nat. Med. 2020;26:1819–1824. doi: 10.1038/s41591-020-1140-9. [DOI] [PubMed] [Google Scholar]
- 261.Shobhavat L, et al. Multisystem inflammatory syndrome in children: clinical features and management-intensive care experience from a pediatric public hospital in western India. Indian. J. Crit. Care Med. Peer Rev. 2020;24:1089–1094. doi: 10.5005/jp-journals-10071-23658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Niño-Taravilla C, Otaola-Arca H, Lara-Aguilera N, Zuleta-Morales Y, Ortiz-Fritz P. Multisystem inflammatory syndrome in children, Chile, May-August 2020. Emerg. Infect. Dis. 2021;27:1457–1461. doi: 10.3201/eid2705.204591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Tolunay O, et al. Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19: a case series experience in a tertiary care hospital of southern Turkey. J. Trop. Pediatr. 2021;67:fmab050. doi: 10.1093/tropej/fmab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Young TK, et al. Mucocutaneous manifestations of multisystem inflammatory syndrome in children during the COVID-19 pandemic. JAMA Dermatol. 2021;157:207–212. doi: 10.1001/jamadermatol.2020.4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Newburger Jane W, et al. Diagnosis, treatment, and long-term management of Kawasaki disease. Circulation. 2004;110:2747–2771. doi: 10.1161/01.CIR.0000145143.19711.78. [DOI] [PubMed] [Google Scholar]
- 266.Ozdemir H, et al. Clinical and epidemiological characteristics of children with Kawasaki disease in Turkey. J. Trop. Pediatr. 2010;56:260–262. doi: 10.1093/tropej/fmp110. [DOI] [PubMed] [Google Scholar]
- 267.Fukushige J, Takahashi N, Ueda Y, Ueda K. Incidence and clinical features of incomplete Kawasaki disease. Acta Paediatr. Oslo. Nor. 1994;83:1057–1060. doi: 10.1111/j.1651-2227.1994.tb12985.x. [DOI] [PubMed] [Google Scholar]
- 268.Sung RYT, et al. Lack of association of cervical lymphadenopathy and coronary artery complications in Kawasaki disease. Pediatr. Infect. Dis. J. 2006;25:521–525. doi: 10.1097/01.inf.0000215263.96289.1c. [DOI] [PubMed] [Google Scholar]
- 269.Smith LB, Newburger JW, Burns JC. Kawasaki syndrome and the eye. Pediatr. Infect. Dis. J. 1989;8:116–118. [PubMed] [Google Scholar]
- 270.Baker AL, et al. Associated symptoms in the ten days before diagnosis of Kawasaki disease. J. Pediatr. 2009;154:592–595.e2. doi: 10.1016/j.jpeds.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]