Abstract
Purpose
Evaluation of single and double limb support postural balance in patients with Anterior cruciate ligament (ACL)injury and comparison of the postural strategy adopted after ACL injury/deficiency(ACLD) with that of an age-matched healthy individual.
Methods
The study group that included 33 subjects confirming inclusion criteria had undergone postural balance assessment using the HUMAC Balance system. The parameters of the center of pressure excursion were recorded on a force plate and compared with age, BMI matched 66 healthy volunteers of control group. The center of pressure excursions was monitored using dependable variables such as sway path length(cm), the average velocity of sway(cm/sec), and the mean COP stability score(%). The mobility component was recorded as the percentage (%) of time spent on each target.
Result
A decrease in postural balance in the injury group was evidenced by a statistically significant decrease of stability score(p = 0.015), increase in path length(p = 0.002) and decrease on time on target mean score (p= <0.001),. Although, the stability score path length and average sway velocity scores in the sound limb of the ACLD group showed impaired balance, the differences were not statistically significant (p = 0.180, p = 0.561, and p = 0.639 respectively) when compared with the dominant limb of the control group.
Conclusion
HUMAC balance system is an effective and simplified measure for quantifying postural balance. Although overall postural stability in ACL injury is impaired, static postural balance is maintained by the compensatory of strategy of sound limb. However, the quantitative parameters of postural stability for the sound limb, despite of a lower mean value, did not show statistically significant differences from the dominant limb of the controlled group.
Keywords: Anterior cruciate ligament, Postural balance, Centre of pressure, Force plate, Balance
1. Introduction
An anterior cruciate ligament (ACL)is one of the commonly injured ligaments around the knee. The majority of ACL injuries occur through the noncontact mechanism such as cutting and pivoting.1 Complete ACL injury (ACL deficiency-ACLD) not only affects mechanical stability but also impairs motor control.2,3 Hence postural control is significantly impaired in ACL-injured patients.4, 5, 6
Postural control is one's ability to maintain stability by controlling the body's position in space.4 It is a complex integration of visual, vestibular and somatosensory functions. Both the proprioceptive neurophysiological function and mechanical function of ACL are equally important for the maintenance of postural l stability.3 The alteration of the proprioceptive neural feedback mechanism could disrupt coordinated muscle function in ACLD, resulting in knee instability and static postural imbalance.2,3,5, 6, 7 The postural balance in stance could be evaluated more precisely on a force plate and researchers prefer the Center of Pressure (COP) excursions as the key measure.5
It has also been observed that the absence of mechanoreceptors in an ACLD knee could activate other mechanoreceptors and thereby create a compensatory muscle activation,6, 7, 8 to stabilize the knee joint.3 This function can be enhanced by using proprioceptive and neuromuscular exercise protocols after ACL injury.9 Shreds of evidence also highlighted on impairment of postural balance in double as well as single-leg stance on both injured and sound limb.3,10
There is no common consensus, on the extent to which the compensation for postural stability could be observed after an ACL injury. The authors noted that along with other compensatory strategies, the sound limb would also compensate for the loss of postural balance in the affected limb.2 The paucity of literature led us to evaluate the postural compensatory strategy of the sound limb. Since there are no standardize numerical parameters exists for the comparison, the current study included age-sex matched, healthy volunteers in the control group. . Most of the available studies compared the postural balance of the affected limb with the subject's sound limb or affected limb with the dominant limb of healthy volunteers. To the best of our knowledge, no study was found, comparing the impact of ACL deficiency on postural control of sound limb with that of healthy volunteers. Moreover, very few studies described the use of HUMAC balance for a comprehensive assessment of postural balance.
The objective of the current study was to evaluate the double and single limb postural balance in patients having ACLD and to compare their balance parameters with that of age-matched healthy volunteers. We hypothesized that the postural balance, which is expected to be impaired in ACLD, might be compensated by the sound limb.
2. Methods
With approval from the institutional ethical committee, the current cross-sectional study was conducted at a National Rehabilitation Institute of India for a period of 18 months. All the patients reported to Out Patient Department for knee instability, were screened clinically by a senior surgeon and diagnosis of ACLD was confirmed by MRI study.
The patients who fulfilled the eligibility criteria were included in the ACLD group. The inclusion criteria were -i)subjects with unilateral ACL deficiency., ii) Age group of 20–30 years, iii) No evidence of concomitant injury in knee. iv) No history of trauma or surgery of the ipsilateral hip, ankle and contralateral limb. . Exclusion criteria were bilateral ACL injury, previous neurological disease or any other balance issues before ACL injury, visible malalignment of the lower limb, any acute or chronic inflammatory joint disease, any known visual or vestibular problems. Out of 61 patients, reported for ACL reconstruction, 33 subjects, fulfilling the inclusion criteria were taken for the study group. None of them was a professional sportsperson.
Age-matched, 66 healthy volunteers, without any significant orthopedics injury to lower limb or spine, were included in the control group. None of them reported any history of neurological, vestibular, or uncorrected visual disorders. They were not under influence of alcohol, drugs, or medicine that might compromise postural balance. Incidentally, all the participants of the control group were clinically found to be right dominant. The subjects of both the groups were explained about the study and informed consent was taken to authorize their participation. All the participants had undergone a standard procedure for the evaluation of postural balance.
2.1. Balance evaluation
The HUMAC Balance system (HUMAC2015® Version: 15.000.0103 © Computer Sports Medicine, Inc.) (www.csmisolutions.com) was used for postural balance evaluation for our study. It has a force plate and a user-friendly software that gives objective values for both static and dynamic balance of the body. The provision of the display screen provides visual feedback to achieve the maximal performance of the subject. HUMAC balance system was validated by Koltermann et al.11 The absolute error of the HUMAC balance system is consistently under 6.60 mm in contrast to other force plate systems like Kistler and AMTI systems that showed a higher margin of error up to 43.70 mm. It gives consistent & reliable data with an acceptable error of up to 0.18% and shows high reproducibility.11 In this system, evaluation of the center of pressure excursion provides objective numerical values for postural competence, based on ground reaction forces controlling body sway in stance.
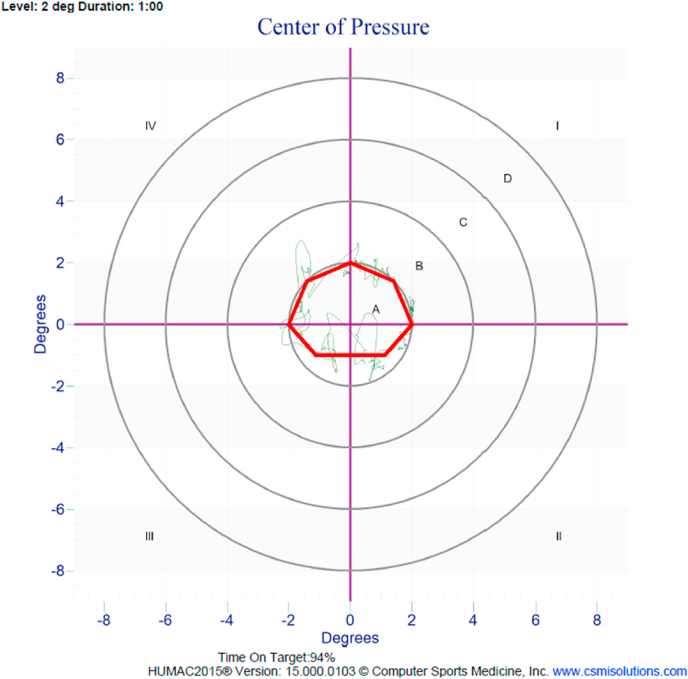
Postural balance was assessed with the subject standing barefoot on the HUMAC Balance force plate, keeping the hand on the waist, and focusing on the visual target, placed approximately 1 m away at eye level. For single-leg stance, subjects were advised to keep the hip and knee of the unsupported limb in a slight flexion position without touching the weight bearing limb [Fig. 1]. All the participants underwent a trial round to familiarize themselves with the procedure. The best score of the remaining three test trials was taken into account. The set parameters were COP (bilateral and unilateral) for 30 s and mobility dimensions at level two for 1 min. The outcome measures for static balance were center of pressure excursions such as sway path length(cm), the average velocity of sway(cm/sec), and the mean COP stability score(%) [Fig. 2]. The dynamic balance was assessed with time on target (%) that is the percentage (%) of time spent on each target [Fig. 3]. The best score among the three trials for both injury and control group were taken into account.
Fig. 1.

Postural balance evaluation on HUMAC Balance system.
Fig. 2.
Assessment of COP parameters on HUMAC balance.
Fig. 3.
Time on Target assessment on HUMAC balance.
2.2. Statistical analysis
The data were entered into Microsoft Excel Worksheet and analyzed using SPSS Version 18.0. Mean & Standard Deviation was calculated for parametric variables. Homogeneity of raw scores in the demographic data set, for both the groups, were assessed by computing Z score. 95% of scores fall within ±2 standard deviations of normal distribution. Independent samples t-test was used to compare the bilateral stance of both the groups and between the sound limb of the ACL deficiency group with the dominant limb of the control group.
3. Results
The basic demographic features of the study participants are given in Table 1. Male subjects constituted 75% in ACLDand 45% in the control group. 52% of ACLD group patients had a right knee ACL injury and 48% involved the left knee. The Mean age for both ACLD and control groups were 24.48 and 23.83 respectively and there was no significant difference in the age of both groups(p = 0.174). The Mean body mass index(BMI) of participants for both the groups were 24.97 and 24.54 and the difference was statistically not significant(p = 0.641).
Table 1.
Comparison of demographic data.
| group | N | Mean | Std. Deviation | Std. Error Mean | t-test for Equality of Means | Sig. (2-tailed) | 95% Confidence Interval of the Difference Lower-- Upper | |
|---|---|---|---|---|---|---|---|---|
| Age | 1∗ 2# |
33 66 |
24.48 23.83 |
3.650 .938 |
.635 .115 |
1.369 | 0.174 | −0.293–1.596 |
| height | 1 2 |
33 66 |
165.82 159.77 |
8.225 8.864 |
1.432 1.091 |
3.358 | 0.001 | 2.454–9.637 |
| weight | 1 2 |
33 66 |
68.39 62.80 |
11.300 13.167 |
1.967 1.621 |
2.194 | 0.031 | 0.512–10.670 |
| BMI | 1 2 |
33 66 |
24.9785 24.5421 |
4.35909 4.38581 |
.75882 .53986 |
0.469 | 0.641 | −1.423–2.296 |
1∗ = Anterior Cruciate Ligament Deficiency(ACLD) group, 2# = Control group, N = number of subjects.
In comparison of stability score between the groups, the Mean score appeared less in the ACLD group. However, the difference was statistically significant(p = 0.015). The body sway COP path length and the average sway velocity are inversely related to postural balance.11 The Mean path length in the ACLD group was significantly higher than the control (p = 0.002) which could imply lower postural stability in these subjects. Although the sway velocity in the ACLD group was higher, the difference was statistically not significant(p = 0.070). The dynamic balance in the ACLD group was significantly less as compared to volunteers(p = 0.000) as indicated by a decrease in the Mean of the time on target score (Table 2).
Table 2.
Comparison of bilateral stance postural stability parameters between ACLD and control group.
| Variable | ACLD (B/L stance) n = 33 (Mean ± S.D.) | Control (B/L stance) n = 66 (Mean ± S.D.) | Mean Difference | Std. Error Difference | 95% Confidence Interval | t | P |
|---|---|---|---|---|---|---|---|
| Stability score (%) | 90.15 ± 9.78 | 93.35 ± 2.72 | −3.197 | 1.289 | −5.756–0.638 | - 2.480 | 0.015 |
| Path length (cm) | 33.39 ± 22.12 | 23.61 ± 8.48 | 9.784 | 3.087 | 3.656–15.913 | 3.169 | 0.002 |
| Average velocity (cm/second) | 0.97 ± 0.55 | 0.78 ± 0.28 | 0.191 | 0.103 | −0.016 – 0.399 | 1.862 | 0.070 |
| Time on target | 90.94 ± 7.73 | 95.36 ± 3.49 | - 4.424 | 1.127 | −6.660 – −2.188 |
−3.927 | 0.000 |
| (%) |
ACLD: Anterior cruciate ligament Deficiency(Injury), B/L: Bilateral, SD: Standard deviation.
Comparison of Postural balance parameters between the sound limb in the ACLD group and dominant limb in the control group is shown in Table 3. Although the Mean difference of stability score was −1.00, the value was statistically insignificant(p = 0.180). Similarly, the Mean score for both path length and average velocity was marginally higher in the sound limb of the ACLD group, but the difference was statistically not significant (p = 0.561 and p = 0.639 respectively) (Table 3).
Table 3.
Comparison of single leg stance postural stability parameters between sound limb of ACLD and dominant limb of control group.
| Variables | ACLD group (Sound limb single leg stance) n = 33 (Mean ± S.D.) | Control group (Dominant single leg stance) n = 66 (Mean ± S.D.) | Mean Difference | Std. Error Difference | 95% Confidence Interval | t | p |
|---|---|---|---|---|---|---|---|
| Stability score (%) | 86.52 ± 4.42 | 87.52 ± 2.90 | −1.000 | 0.741 | −2.471–0.471 | - 1.349 | 0.180 |
| Path length (cm) | 97.32 ± 24.12 | 94.28 ± 25.06 | 3.047 | 5.210 | −7.354 – 13.449 | 0.585 | 0.561 |
| Average velocity (cm/Second) | 3.22 ± 0.78 | 3.14 ± 0.83 | 0.080 | 0.171 | −0.260 – 0.422 | 0.472 | 0.639 |
ACLD: Anterior cruciate ligament Deficiency(Injury), SD: Standard deviation.
4. Discussion
Our study result showed an overall reduction of postural stability in the ACLD group and both static and dynamic parameters showed statistically significant differences, as compared to the control group. But, while comparing the sound limb of the ACL deficient group with the dominant limb of the volunteer group, the Mean differences were marginally lower, and statistically insignificant. It implies that the sound limb of unilateral ACLD patients probably undergo a compensatory strategy, in order to substitute the postural deficits that would have arisen in the affected limb.
Many methods have been used to quantify postural balance disorders for enabling a better rehabilitation plan for such kinds of patients. Stabilometric assessment using a force plate has been conducted to investigate impairment of proprioception in an ACLD knee,12, 13, 14, 15 but the use of HUMAC balance for a comprehensive assessment of postural balance after ACL deficiency in our study, is the first one of its kind.
Although homogeneity of the baseline data set was maintained between the groups, there was a significant difference in gender ratio. Ageberg et al.16 reported that there was no significant influence of activity level on the result, but age and gender should be accounted for. In contrast, the role of gender in the variance of COP measurement was found to be insignificant by some studies.17,18 We chose young individuals within the age group of 20–30years for both the groups so that we could avoid bias such as balance abnormalities due to other causes or greater body sway in the elderly population.19
Hernikson et al.20 eliminated the visual component of the balance system and challenged the somatosensory component by using a moving platform. They found a better postural balance in the control group. In our study, the evaluation was done with the eye open, so that the impairment of somatosensory component after ACLdeficiency could be assessed keeping the other components of balance such as visual and vestibular components intact. Several other studies also assessed postural stability with open eye conditions.20, 21, 22, 23
COP is calculated from the horizontal moment and vertical force data generated by the force platform. It measures the center of distribution of the total force applied to the supporting surface over a definite time interval.24 It is the most commonly used parameter for evaluating postural balance on a force plate.25 In the HUMAC balance system, forces along the z-axis are taken for calculation of COP.11
Researchers have shown significant differences in all postural parameters between ACLD and the healthy control group on double leg stance.12,13,26 Whereas, a study by O’ Connell et al.27 did not find any difference between such groups. In our study, all the COP parameters except average sway velocity showed a significant difference in postural balance, between the groups. The balance deficit in the ACLD group could be explained by a lack of mechanical restrain and proprioceptive impairment after the ACL injury.
Several studies have shown an increase in sway frequency in the affected side of ACLD subjects during the unilateral stance test[15–17]. A systematic review by Negahban et al.28 compared postural balance between sound limb of the ACLD group with that of the control group. Out of their eight reviewed papers, six studies showed larger postural sway in the sound leg compared to the control leg. Conflicting results with smaller postural sway of the sound limb were shown by Ageberg16 and O Connel et al.27 In our study, we also observed low stability scores and higher body sway parameters in the sound limb of the ACLD group as compared to the dominant limb of the control group. This finding implies that the impaired postural control mechanism is not only found in the deficient leg but also in the sound leg. However, a small mean difference between the group suggests that the postural balance of the sound limb is less affected than the injured side. Hoffman et al.15 have explained in a theoretical way that balance asymmetry due to ACLD could be compensated by sound limb. By decreasing the balance of the sound leg, re-establishment of the symmetry between the injured and the sound leg could be possible.14 We recommend, equal attention to be given also to the sound limb while planning the preoperative as well as postoperative management. Moreover, assessment of balance dysfunction and appropriate remedial measures are critical in ACLD subjects.29 The importance of psychological preparedness along with good postural balance and better agonist-antagonist ratio for return to sports are highlighted by Albano et al.30 If balance issues are not addressed during the rehabilitation phase, then, they might continue to persist and increase the risk of re-injury.31
Limitations of the study: Remarkable gender difference between stydy and control group might have created a gender bias in this study. Future reference should aim to maintain the gender ratio in both the groups and a large comparable sample size to increase the power of the study.
5. Conclusion
The over-all postural stability was reduced in patients with unilateral ACL deficiency. The sound limb of ACLD subjects also showed impairment of postural stability in comparison to a healthy volunteers, hence a second thought should be given while considering it as the ‘control’ during postural assessments. However, the quantitative parameters of postural stability for the sound limb did not show statistically significant differences from the dominant limb of the controlled group. Thus, generalization of this result is limited and further studies are recommended to address the issue The HUMAC balance system is an effective alternative for the evaluation of Postural balance in individuals with an ACL deficiency. Assessment of postural balance and appropriate remedial measures is critical for the strategic planning of a comprehensive rehabilitation protocol.
Funding
No funds received for this study purpose.
Ethical Approval
The current study being a part of the ongoing research project, has got approval from the ethical committee.
Consent to Participate and Publish
Informed consent has been taken from participants of both groups.
Disclosure
Nothing to declare.
Availability of data and material
Nothing to submit.
Authors contribution
Pabitra Kumar Sahoo designed and supervised the study, interpreted the results of the study, prepared an initial draft of the manuscript, and agrees to be accountable for all aspects of the work and to take the responsibility of the corresponding author. Mamata Manjari Sahu collected the data, statistically analyzed it, revised the manuscript critically by providing important intellectual inputs, approved the final version of the manuscript to be published. All authors have critically reviewed and approved the final version of the manuscript.
Declaration of Competing Interest
No conflict of interest to declare.
Acknowledgments
We express our sincere gratitude to all the student volunteers who kindly participated in the study.
References
- 1.Boden B.P., Sheehan F.T., Torg J.S., Hewett T.E. Non-contact ACL injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520–527. doi: 10.5435/00124635-201009000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howells B.E., Ardern C.L., Webster K.E. Is postural control restored following anterior cruciate ligament reconstruction? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1168–1177. doi: 10.1007/s00167-011-1444-x. [DOI] [PubMed] [Google Scholar]
- 3.Johansson H., Sjölander P., Sojka P. Receptors in the knee joint ligaments and their role in the biomechanics of the joint. Crit Rev Biomed Eng. 1991;18(5):341–368. [PubMed] [Google Scholar]
- 4.Williams G.N., Chmielewski T., Rudolph K.S., Buchanan T.S., Snyder-Mackler L. Dynamic knee stability: current theory and implications for clinicians and scientists. J Orthop Sports Phys Ther. 2001;31(10):546–566. doi: 10.2519/jospt.2001.31.10.546. [DOI] [PubMed] [Google Scholar]
- 5.Lee J., Webb G., Shortland A.P., Edwards R., Wilce C., Jones G.D. Reliability and feasibility of gait initiation centre-of-pressure excursions using a Wii® Balance Board in older adults at risk of falling. Aging Clin Exp Res. 2019;31(2):257–263. doi: 10.1007/s40520-018-0945-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zimny M.L., Schutte M., Dabezies E. Mechanoreceptors in the human anterior cruciate ligament. Anat Rec. 1986;214(2):204–209. doi: 10.1002/ar.1092140216. [DOI] [PubMed] [Google Scholar]
- 7.Schutte M.J., Dabezies E.J., Zimny M.L., Happel L.T. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am. 1987;69(2):243–247. [PubMed] [Google Scholar]
- 8.Fulton J., Wright K., Kelly M. Injury risk is altered by previous injury: a systematic review of the literature and presentation of causative neuromuscular factors. Int J Sports Phys Ther. 2014;9(5):583–595. [PMC free article] [PubMed] [Google Scholar]
- 9.Akbari A., Ghiasi F., Mir M., Hosseinifar M. The effects of balance training on static and dynamic postural stability indices after acute ACL reconstruction. Global J Health Sci. 2016;8(4):68–81. doi: 10.5539/gjhs.v8n4p68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonfim T.R., Grossi D.B., Paccola C.A.J., Barela J.A. Additional sensory information reduces body sway of individuals with anterior cruciate ligament injury. Neurosci Lett. 2008;441(3):257–260. doi: 10.1016/j.neulet.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 11.Koltermann J., Gerber M., Beck H., Beck M. Validation of the HUMAC balance system in comparison with conventional force plates. Technologies. 2017;5:44. doi: 10.3390/technologies5030044. [DOI] [Google Scholar]
- 12.Lysholm M., Ledin T., Odkvist L.M., Good L. Postural control--a comparison between patients with chronic anterior cruciate ligament insufficiency and healthy individuals. Scand J Med Sci Sports. 1998;8(6):432–438. doi: 10.1111/j.1600-0838.1998.tb00464.x. [DOI] [PubMed] [Google Scholar]
- 13.Zätterström R., Fridén T., Lindstrand A., Moritz U. The effect of physiotherapy on standing balance in chronic anterior cruciate ligament insufficiency. Am J Sports Med. 1994;22(4):531–536. doi: 10.1177/036354659402200416. [DOI] [PubMed] [Google Scholar]
- 14.Gauffin H., Pettersson G., Tegner Y., Tropp H. Function testing in patients with old rupture of the anterior cruciate ligament. Int J Sports Med. 1990;11:73–77. doi: 10.1055/s-2007-1024766. [DOI] [PubMed] [Google Scholar]
- 15.Hoffman M., Schrader J., Koceja D. An investigation of postural control in postoperative anterior cruciate ligament reconstruction patients. J Athl Train. 1999;34(2):130–136. [PMC free article] [PubMed] [Google Scholar]
- 16.Ageberg E., Roberts D., Holmström E., Fridén T. Balance in single-limb stance in healthy subjects--reliability of testing procedure and the effect of short-duration sub-maximal cycling. BMC Muscoskel Disord. 2003;4:14. doi: 10.1186/1471-2474-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nordahl S.H., Aasen T., Dyrkorn B.M., Eidsvik S., Molvaer O.I. Static stabilometry and repeated testing in a normal population. Aviat Space Environ Med. 2000;71(9):889–893. [PubMed] [Google Scholar]
- 18.Tookuni K.S., Bolliger Neto R., Pereira C.A.M., Souza DR de, Greve J.M.D.A., Ayala A.D.A. Comparative analysis of postural control in individuals with and without lesions on the anterior cruciate ligament of the knee. Acta Ortopédica Bras. 2005;13(3):115–119. doi: 10.1590/S1413-78522005000300003. [DOI] [Google Scholar]
- 19.Kollegger H., Baumgartner C., Wöber C., Oder W., Deecke L. Spontaneous body sway as a function of sex, age, and vision: posturographic study in 30 healthy adults. Eur Neurol. 1992;32(5):253–259. doi: 10.1159/000116836. [DOI] [PubMed] [Google Scholar]
- 20.Henriksson M., Ledin T., Good L. Postural control after anterior cruciate ligament reconstruction and functional rehabilitation. Am J Sports Med. 2001;29(3):359–366. doi: 10.1177/03635465010290031801. [DOI] [PubMed] [Google Scholar]
- 21.Chmielewski T.L., Wilk K.E., Snyder-Mackler L. Changes in weight-bearing following injury or surgical reconstruction of the ACL: relationship to quadriceps strength and function. Gait Posture. 2002;16(1):87–95. doi: 10.1016/s0966-6362(01)00202-8. [DOI] [PubMed] [Google Scholar]
- 22.Zouita Ben Moussa A., Zouita S., Dziri C., Ben Salah F.Z. Single-leg assessment of postural stability and knee functional outcome two years after anterior cruciate ligament reconstruction. Ann Phys Rehabil Med. 2009;52(6):475–484. doi: 10.1016/j.rehab.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Harrison E.L., Duenkel N., Dunlop R., Russell G. Evaluation of single-leg standing following anterior cruciate ligament surgery and rehabilitation. Phys Ther. 1994;74(3):245–252. doi: 10.1093/ptj/74.3.245. [DOI] [PubMed] [Google Scholar]
- 24.Guskiewicz K.M., Perrin D.H. Research and clinical applications of assessing balance. J Sport Rehabil. 1996;5(1):45–63. doi: 10.1123/jsr.5.1.45. [DOI] [Google Scholar]
- 25.Harrison N. The Influence of HUMAC Training on Balance and Range of Motion in an Achilles Tendon. :46.
- 26.Fridén T., Zätterström R., Lindstrand A., Moritz U. Disability in anterior cruciate ligament insufficiency. An analysis of 19 untreated patients. Acta Orthop Scand. 1990;61(2):131–135. doi: 10.3109/17453679009006504. [DOI] [PubMed] [Google Scholar]
- 27.null O'Connell, George null, Stock null. Postural sway and balance testing: a comparison of normal and anterior cruciate ligament deficient knees. Gait Posture. 1998;8(2):136–142. doi: 10.1016/s0966-6362(98)00023-x. [DOI] [PubMed] [Google Scholar]
- 28.Negahban H., Mazaheri M., Kingma I., van Dieën J.H. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1491–1504. doi: 10.1007/s00167-013-2501-4. [DOI] [PubMed] [Google Scholar]
- 29.Ferdowsi F., Rezaeian Z.S. Evaluating equilibrium in anterior cruciate ligament reconstruction. J Phys Ther Sci. 2018;30(5):726–729. doi: 10.1589/jpts.30.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Albano T.R., Rodrigues C.A.S., Melo A.K.P., de Paula P.O., Almeida G.P.L. Clinical decision algorithm associated with return to sport after anterior cruciate ligament reconstruction. J Athl Train. 2020;55(7):691–698. doi: 10.4085/1062-6050-82-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paterno M.V., Schmitt L.C., Ford K.R. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Nothing to submit.