Abstract
Objective:
To assess quality of antenatal care-linked to HIV counseling and testing as an intervention for prevention of mother-to-child transmission at government health facilities in Harar Town, Eastern Ethiopia, 2020.
Methods:
Institutional-based cross-sectional study was done from 1 February to 30 February 2020 by applying quantitative method conducting in government health facilities in Harar town, Eastern, Ethiopia. A total of 422 participants were recruited from four governmental hospitals in Harar Town. Simple random sampling method was used to select the participants. Data were collected by three nurses selected from prospected hospitals. The collected data were cleaned, checked for quality, coded, and analyzed using “Software package Social Science, version 20” computer program.
Result:
From a total of 422 participants, 348 (82.5%) were satisfied with the counseling room’s privacy, and having pre-test and post-test counseling by the same person provided comfort for 357 (98.9%) of clients. Three hundred eighty-nine (92.2%) felt comfortable with the counselors’ client handling/respect; 386 (91.5%) were satisfied with technical competence of the counselors. About a quarter (25.4%) of clients had no discussion of prevention of mother-to-child transmission at all, and the majority (68.2%) comprehended that HIV counseling and testing could benefit prevention of mother-to-child transmission.
Conclusion:
Exit interview revealed that the basic topics were covered in most of the pre- and/or post-test sessions, and the majority of those counseled comprehended the information; however, nearly a quarter of the clients did not understand why they were offered HIV counseling and testing particularly during their pregnancy time.
Keywords: Prevention of mother-to-child transmission of HIV
Introduction
Antenatal care (ANC) is a vital component of the continuum of care for mothers and babies and provides an opportunity for the timely diagnosis of obstetric conditions, educating women about the danger signs of pregnancy, the advantages of breastfeeding, and the importance of family planning. It has been estimated that increased coverage and quality of maternal healthcare could avert 71% of neonatal deaths, 33% of stillbirths, and 54% of maternal deaths in low-and-middle-income countries. Quality of ANC given to eligible women and was determined by four dimensions, namely: (1) skilled healthcare (ANC provided by doctors, auxiliary nurse midwives, nurses, midwives or lady health visitors), (2) timeliness (first ANC visit and registration during the first trimester of pregnancy), (3) sufficiency (at least four ANC visits completed during the pregnancy), and (4) appropriateness in content (processes of care provided during antenatal check-up, e.g., blood sample taken to test for possible morbidities). 1
Quality of ANC with HCT (HIV counseling and testing) has great value to PMTCT (prevention of mother-to-child transmission) of HIV (human immunodeficiency virus) entails transmission of HIV from an infected mother to her child. Also called “vertical” or “perinatal” transmission, MTCT (mother-to-child transmission) can occur during pregnancy, labor, delivery, and breastfeeding. Over 90% of pediatric AIDS cases are from MTCT. Measuring the quality of HCT in PMTCT programs has been divided into two common elements-competence or counseling quality (which includes interpersonal relationship, gathering information, giving information, and dealing with special circumstances) and content (which includes pre-test, post-test, and HIV diagnostic procedure counseling). The purpose of pre-test counseling in all PMTCT settings is to provide clients or couples with adequate information to make an informed decision on HIV testing. The pre-test counseling session should take approximately 10–20 min for the group or individual sessions in the ANC setting. The purpose of post-test session is to provide women or couples with the HIV test result; to help them understand the meaning of the result; to encourage disclosure and partner testing; to offer counseling and prevention education including risk-reduction messages as well as support and referrals to services. The post-test session for the woman or couple who tests HIV-negative typically lasts about 5–10 min, and for the HIV-positive generally takes 15–30 min or longer, depending on the need for support. 2
The clients are given pre-test information in a group or individually on HIV/AIDS and PMTCT and are told that their routine antenatal laboratory tests will include HIV test. The provider also must inform the client that she has the right to say “no” (to opt-out), and this decision by no means affects the services she will get from the health facility. Ethiopia has started human capacity development and rolling out the revised PMTCT guidelines at a larger scale in early 2007. 3
Due to a number of barriers for the implementation of PMTCT program, in 2010, it was estimated that only 45% of HIV-positive pregnant women in the Sub-Saharan Africa (SSA) had access to PMTCT program. 4 MTCT rates remain high in developing nations, particularly SSA countries where the majority of HIV-infected women of childbearing age live. Such high rates persist mostly due to lack of access to existing prevention interventions, lack of male involvement, and women not disclosing their status to their partners. MTCT of HIV remains as one of the biggest concerns that needs to be dealt with in taking effective preventive measures and maximizing treatment, care, and support for needy HIV-positive pregnant mothers in order to save the life of large number of innocents in our developing country. 5
In Ethiopia, PMTCT program was started in 2001 and comprehensive national guideline was developed in 2007. 6 In 2013, Ethiopia has introduced option B+ in accordance with World Health Organization (WHO) guideline. In 2014, in Ethiopia, 2495 health facilities were providing PMTCT service and the proportion of pregnant women counseled and tested for PMTCT of HIV was 57.0%. Although the number of health facilities providing PMTCT service has increased dramatically in Ethiopia, MTCT of HIV still remains to be a challenge for the country due to high missed opportunities and dropout rates in addition to low coverage and quality of services. 7
Globally, approximately 37.6 million people across the globe living with HIV in 2020 and of these about 59% were in SSA, and more than 30 million have died due to AIDS worldwide.1,8 According to United Nation’s Children Fund (UNICEF), estimated that about 1.8 million HIV-infected women are pregnant every year; and in case of low uptake of PMTCT, they deliver roughly 70,000–170,000 HIV-infected infants annually, around 310,000–650,000 children acquired HIV infection mainly from mother-to-child transmission and of these more than 80% were not receiving HCT during pregnancy session, about 200,000 to 350,000 infants are infected by HIV through breastfeeding each year; and 1000 children under 15 years become infected with HIV every day; 90% of them through mother-to-child HIV transmission and of that, 2 million children (6% of the 33.4 million people living with HIV (PLWHA)) are living with HIV and the majority of these children (90%) live in SSA. In the absence of these critical interventions, the risk ranges from 20% to 45%. 9
There were approximately 84,000 AIDS-related deaths in 2017 and about 9.7 million AIDS orphans in the same year in SSA. 9 Besides the dominant heterosexual transmission in Ethiopia, vertical transmission from mother to child accounts for more than 90% of pediatric AIDS. A report from Federal HIV/AIDS Prevention and Control Office indicates that, daily 65 peoples infected with HIV/AIDS and 30 peoples are died because of HIV/AIDS and currently the MTCT of HIV/AIDS increased by 11% (60%–71%). The rate of transmission of HIV/AIDS were 1.2% in female and 0.5% in male. The availability of HCT services in Ethiopia has been uneven, and even when available, uptake has been relatively low. 10
As far as our knowledge there is few published information on this subject in Ethiopia, especially in the context of this study areas. Therefore, this study will try to assess quality of ANC-linked to HIV counseling’s and testing as an intervention of PMTCT provided to pregnant mothers.
Materials and methods
Study setting and population
Institutional-based cross-sectional study was done from February 1-30/2020 by applying quantitative methods which were used for study in Harari region. Harari region is one of the historical regions and located 525 km away from Addis Ababa to the eastern part of the country. Based on the 2007 Census conducted by the Central Statistical Agency of Ethiopia (CSA), Harari has a total population of 246,000 of whom 124,000 were men and 122,000 were women. 6 In the region, there are 3 governmental hospitals, 1 private hospitals, 1 fistula hospital, 8 health center (HC), 27 health posts, and 1 regional laboratory were found. 11 From these facilities, this study will be conducted on selected four government health facilities those are Hiwotfana Specialized University Hospital (HFSUH), Jugal Hospital, Aratega HC, and Aboker HC. The hospitals and the HC serve for dwellers of the town and for patients coming from different Woredas and Kebeles surrounding the town. They have maternal and child healthcare units which provide ANC, delivery service, family planning, HCT service, counseling on infant feeding options and safer sex practices, and ART (antiretroviral therapy) for PMTCT of HIV for pregnant women.
Sample size estimation and sampling technique
The exit interview of the pregnant women regarding the service in the PMTCT sites and 422 ANC attendants were involved in the study. From seven government health facilities which found in Harar Town, four government health facilities was selected based on simple random sampling method. The sample size was determined by 3-month ANC clients flow on each health facilities and the total 3-month ANC flow of four health facilities are 847. The total sample size (n = 422) was allocated proportionally to four health facilities.
The exit interview of the pregnant women regarding the service in the PMTCT sites, and based on the following assumptions for a single population proportion
where n is the maximum sample size; Z1 − α/2 is the confidence level, taking 95%; d is the margin of tolerable sampling error, taking d = 5% (0.05); P is the proportion which is 48% (based on the study done in Addis Ababa on quality of ANC linked with HCT). 10
Thus, it gives n = (1.96)2 × 0.48 (1 − 0.48) / (0.05)2≈384. Considering 10% non-response rate, it will give a sample size of 422.
Eligibility criteria
All pregnant women who attended the HCs and received HCT were included in this study. All pregnant women, PMTCT counselors, and coordinators participated in this study voluntarily. Pregnant women who attended an ANC visit but did not receive HCT were excluded
Data collection tool and procedure
All questionnaires are adapted from the United Nations Program on HIV/AIDS (UNAIDS) Best Practice Collection KEY Material (UNAIDS/00.09E (English original)) for evaluating quality of ANC-linked HCT for PMTCT. 12 Based upon the expected content found in this tool and final adjustment are made after pre-test was carried out to fit to our local situation.
The tool has three parts: questionnaire for exit PMTCT client interview; questionnaire for PMTCT site coordinators and counselor’s. Four days of training were given for data collectors and supervisors. They were health professionals, who had the skills of the local languages. The data collection was supervised, reported, and managed by the investigators.
Data quality control
The quality of data was ensured using various strategies like pre-testing the questionnaire, training of the data collectors and supervisors, supervision, and checking the questionnaire. The data collectors and supervisors were trained on the data collection technique for 2 days prior to data collection processes. Pre-test were carried out in 5% of the study participants at Federal police hospital before the actual data collection period which is not selected for the study.
Ethical consideration
Initially letter of cooperation and permission was obtained from Harar Health Science College Ethical Review Committee with an approval number of CRPO/HHSC-NMBU/007/21. Information about the study was explained with local languages (Amharic and Afan Oromo), and written consent was taken from adult participants (age greater than 18 years old) and for minor group those less than 18 years participants, we obtained written consent from guardians and ascent from the minor group before commencement of the study. All the participants were reassured of the anonymity, and personal identifiers are not used. Then, after obtaining written consent from every participant, the data collectors continue the job by giving due respect to the norms, values, beliefs, culture, and ensuring the confidentiality of the data they collects
Operational definition
Client/customer satisfaction: the state of being pleased or contented by clients/customer about the overall services (they received or the specific attributes of the interpersonal relationships, technical competencies, and outcomes of the care). 13
Counseling duration: it will be considered as the time taken for all counseling sessions. 13
Confidentiality: it is a situation in which you trust someone not to tell secret or private information to anyone else. 13
MTCT: a transmission of HIV from infected mothers to unborn babies which may occur during pregnancy, delivery, or during breastfeeding. 13
Post-test counseling: it is the counseling provided when an individual receives his or her HIV test results as well as giving moral support immediately after the client has received the result. 13
Pre-test counseling: it is the counseling given to an individual before an HIV test is performed to make sure that the individual has sufficient information to make an informed decision about having an HIV test. 13
Privacy in counseling rooms: for adequate privacy in counseling rooms, the door and walls need to be closed to the roof. Only the counselor and the client are expected in the room, and sessions may not be interrupted. 13
HCT counselor: a person who has received special training in client centered HCT. 13
Data processing and analysis
The collected data were cleaned, check for quality, coded, and analyzed using SPSS version 20 computer program. Binary and multiple logistic regressions were used to observe the association (p-value < 0.2 for binary and p-value < 0.05 for multiple) between independent variables and dependent variable. Odds ratio with 95% confidence interval (CI) was calculated using multiple logistic regression models to control confounders. Quality of the PMTCT program was analyzed by the content of client’s feedback. The findings were presented by text tables and graphs.
Results
This study tried to assess the quality of PMTCT services given in four health facilities. The data were collected from key informants (PMTCT site coordinators and PMTCT counselors), and 422 exit clients.
Operational aspect of the PMTCT sites
Four PMTCT coordinators at four health facilities were interviewed. All the coordinators responded to the questionnaire. Regarding trained human power working on PMTCT, the maximum number of trained human power found in the health facilities was six and the minimum number was one. Two health facilities had two trained PMTCT counselors, and the rest two health facilities had three or more trained counselors. Some of the PMTCT site coordinators reported that they had shortage of trained human power and that the problem affected the performance and/or quality of the services. They added also that other additional health workers need to be trained and refreshment courses be given to those who were already trained. All health facilities had an appointment system for their clients. Again all the health facilities had a referral system for a better service. The HCs refer their clients to Hospitals, ART Centers, and to Care and Support Groups for a better management.
According to the responses of the PMTCT coordinators, all of the health facilities offer both pre-test and post-test counseling services for the pregnant women. In addition, two of them also reported that they offer an ongoing counseling for their clients. The types of the counseling the health facilities offer were group and individual (pre-test) counseling. All the health facilities offered group pre-test information by HIV-positive mothers or by health professionals and later individual pre- and post-test counseling delivered by PMTCT trained nurses. Tree of the health facilities had a separate room for individual counseling. Regarding the uptake rates, three of the HCs reported to have an HCT uptake rate of 100% (all ANC clients underwent HCT), one health facility were in the range of 90%–99%. Regarding the ANC clients’ return rates to collect their blood test results, two health facilities reported a return rate of 90%–99% and the rest health facilities reported a return rate of 70%–89%.
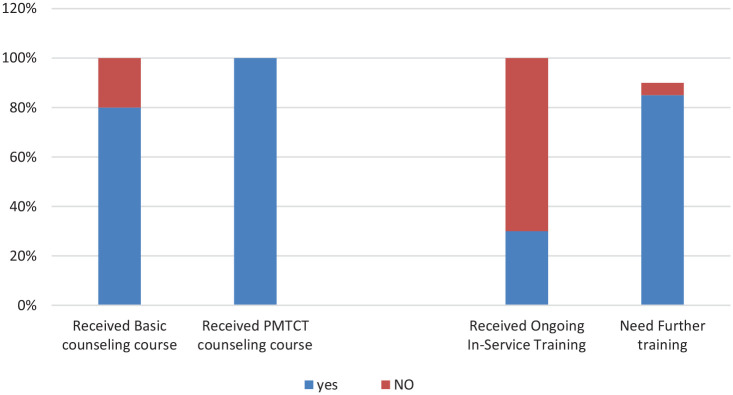
Regarding interview with counselors working on PMTCT at the time of survey, nine of the counselors responded to the questionnaire (Figure 1). All the interviewed PMTCT counselors were found to be nurses, and all were appointed to become PMTCT counselors by their heads.
Figure 1.
Survey response of counselors regarding need for further training in Harar, Ethiopia, 2020.
Seven of the nine PMTCT counselors had taken the basic Voluntary Counseling and Testing (VCT) courses, and all had attended the additional PMTCT training. Only three of them had taken refreshment training in the past 5 years. Eight of them believed that they need further training. Regarding specific areas of further training, six of them would like to get in-service training on “HIV and PMTCT”; the rest three required an in-service training on “counseling of HIV, PMTCT, and Group Counseling.”
Exit interviews with mothers
Socio-demographic characteristics
In the exit interview, 422 ANC clients from four health facilities were interviewed at exit points. Accordingly, almost all (95.0%) were residents of Harar city (Table 1). Majority (54.0%) of them were in the age group of 16–24 years, followed by age group of 25–34 years, which accounted for 178 (42.2%) and the rest (3.8%) were in the age group of 35–40 years. The mean age of the respondents was 24.6 (+4.67) years (the youngest being 16 and the oldest 40). Nearly 2/3 (63.7%) of the respondents were Orthodox Christian by religion followed by Muslim (25.9%). Protestants accounted for 42 (10.0%) and Catholics 2 (0.2%). About 1/3 (34.0%) of the clients were Amhara by ethnicity, followed by Oromo (29.5%) and Gurage (20.7%). Harari and Tigres accounted for 30 (7.0%) and 20 (4.8%), respectively, and other ethnic groups accounted for 17 (4.0%). Majority of the respondents (88.1%) were married, 34 (8.1%) single, 13 (3.1%) cohabiting, and 3 (0.7%) divorced. Concerning the educational background, about half of mothers (50.4%) were in grades 7–12 (or 10 + 2), and college or university levels accounted only for 12 (2.9%). Nearly 1/3 (29.9%) were in the grade levels of 1–6, and the rest were either illiterate (14.5%) or only able to read/write (2.3%). Occupationally, 238 (56.5%) were housewives, 53 (12.6%) were employed in different private agencies, 40 (9.5%) were merchants, and 31 (7.4%) were unemployed/jobless. Government employees, daily laborers and students accounted for 20 (4.7%), 18 (4.3%), and 12 (2.9%), respectively; and others 9 (2.1%). More than half (55.3%) were first gravid, 186 (44.2%) were gravida 2–5 and the rest 2 were above gravida 5. One hundred ninety-six (46.4%) of the clients were in their third trimester, 180 (42.7%) in second trimester, and the rest 46 (10.9%) were in the first trimester. Majority 352 (83.4%) of the clients were first visit clients, 64 (15.2%) were second visit, and the rest 6 (1.4%) were third visit who came for different services.
Table 1.
Socio-demographic characteristics of PMTCT attendees, Harar, Ethiopia, 2020.
| Socio-demographic variables of the PMTCT clients | Number | % |
|---|---|---|
| Place of residence(n = 422) | ||
| HARAR | 401 | 95.0 |
| Out of HARAR | 21 | 5.0 |
| Age (completed years) | ||
| 16–24 | 228 | 54.0 |
| 25–34 | 178 | 42.2 |
| 35–40 | 16 | 3.8 |
| Religion | ||
| Orthodox | 268 | 63.7 |
| Muslim | 109 | 25.9 |
| Protestant | 42 | 10.0 |
| Catholic | 2 | 0.4 |
| Ethnicity | ||
| Amhara | 143 | 34.0 |
| Gurage | 124 | 29.5 |
| Oromo | 87 | 20.7 |
| Tigre | 30 | 7.0 |
| Siltie | 20 | 4.8 |
| Others | 12 | 4.0 |
| Marital status | ||
| Married | 371 | 88.1 |
| Single | 34 | 8.1 |
| Widowed | 13 | 3.1 |
| Divorced | 3 | 0.7 |
| Occupation (n = 421) | ||
| Housewife | 238 | 56.5 |
| Private | 53 | 12.6 |
| Merchant | 40 | 9.5 |
| Jobless | 31 | 7.4 |
| Daily laborer | 20 | 4.7 |
| Government employee | 18 | 4.3 |
| Student | 12 | 2.9 |
| Other | 9 | 2.1 |
| Gravidity | ||
| 1 | 233 | 55.3 |
| 2–5 | 186 | 44.2 |
| ⩾5 | 2 | 0.5 |
| Current gestational age | ||
| First trimester | 46 | 10.6 |
| Second trimester | 180 | 42.7 |
| Third trimester | 196 | 46.4 |
PMTCT: prevention of mother-to-child transmission.
Among 422 pregnant mothers, 393 (93.12%) were either counseled or simply requested to have HIV blood test, 390 (92.4%) had discussed about receiving their test results, and 319 (75.6%) were also counseled about issues associated with having been tested some time ago; but only 288 (68.4%) of the 422 clients were counseled about HIV/AIDS and 133 (31.5%) were not counseled on HIV/AIDS (Table 2). Of those 393 clients who were requested to have blood test, only 266 (67.7%) were counseled about HIV/AIDS and 366 (93.1%) were also counseled about receiving their test results (not tabulated here). Concerning MTCT/PMTCT, in 314 (74.6%) of the sessions the discussion was held. With regard to the infants’ health and feeding options, only 245 (58.1%) clients were counseled about the health of their babies and only 178 (42.3%) of the mothers were counseled about infant feeding options.
Table 2.
Counseling offered to PMTCT clients as reported by the clients at exit interview, Harar, Ethiopia, 2020.
| Major counseling topics | Clients received counseling | |||||
|---|---|---|---|---|---|---|
| Yes | No | Total | ||||
| Number | % | Number | % | Number | % | |
| About having an HIV test | 393 | 93.1 | 29 | 6.9 | 422 | 100 |
| About receiving the test result | 390 | 92.4 | 32 | 7.6 | 422 | 100 |
| Issues associated with having been tested some time ago | 319 | 75.6 | 103 | 24.4 | 422 | 100 |
| About HIV | 288 | 68.4 | 133 | 31.6 | 421 | 100 |
| About MTCT/PMTCT | 314 | 74.6 | 107 | 25.4 | 421 | 100 |
| About the health of the baby | 245 | 58.1 | 177 | 41.9 | 422 | 100 |
| About the child’s feeding options | 178 | 42.3 | 243 | 57.6 | 421 | 100 |
MTCT: mother-to-child transmission; PMTCT: prevention of mother-to-child transmission.
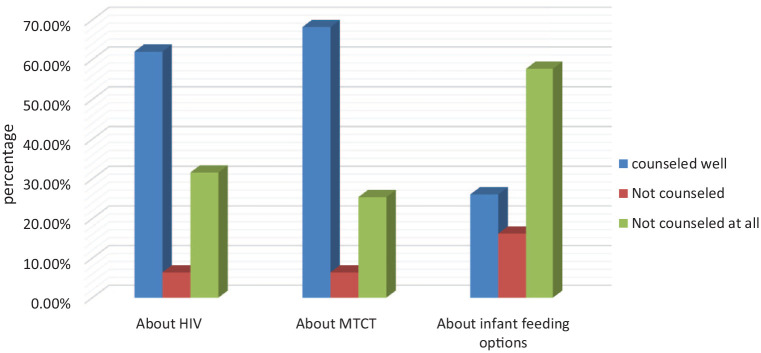
Regarding comprehension/understanding levels of the PMTCT counseling topics among the clients, 261 (62.0%) of the respondents said that they had understood well the counseling on HIV/AIDS, 27 (6.4%) had discussed on the topic, but the discussion was not clear enough to understand, and 133 (31.6%) said that they had not discussed the topic at all (Figure 2). Among the points the clients reported to have gained new knowledge as a result of the counseling on HIV/AIDS were that HIV can pass from a positive mother to the fetus during pregnancy, delivery process, and by breast feeding; the need for HIV testing during pregnancy; the need for partners testing; and counseling on how to live with the virus if I they have turned positive; about HIV transmission and prevention. Of the 314 clients counseled about issues related to MT and prevention of HIV, 287 (68.2%) reported to have comprehended the information, 27 (6.4%) had discussed about the issue, but could not grasp the information, and 107 (25.4%) did not discuss about PMTCT at all. The main points the clients reported to have grasped were that HIV can pass from mother to their children; the need for HIV testing during pregnancy; and that it is possible to protect the children or to minimize the chance of transmission by use of drugs if the mothers are positive.
Figure 2.
Level of major counseling topics comprehended by the PMTCT clients as reported at exit interview, Harar, Ethiopia, 2020.
Concerning infant feeding options, 110 (26.1%) reported to have benefited from the counseling, 68 (16.2%) did not understand well the discussion, and the rest 243 (57.7%) reported that there was no such discussion at all. Among the information the clients reported to have grasped from the counseling was that it is possible to protect or decrease the chance of transmission of HIV from a positive mother through drugs given to the mother and the infant, and that an HIV-positive mother may breastfeed her infant exclusively. Almost all (99.5%) the clients believed that HCT during pregnancy was necessary for the mother; however, only 332 (78.7%) of them correctly answered that HCT is offered during pregnancy for the purpose of PMTCT, the rest (21.3%) did not know the main reason why they were offered HCT at the HCs particularly when they were pregnant.
The majority (61.6%) of the clients were served same day without an appointment, 147 (34.8%) were appointed for up to a week, and the rest (3.6%) were appointed for 2–3 weeks to get the service. The vast majority (86.7%) of the clients stayed in the health facilities up to 1.5 h to get the service they wanted, 41 (9.7%) waited 1.5–3 h, and the rest 15 (3.6%) waited for the service more than 3 h in the HCs. Average waiting time was 39.75 min.
A bit greater than two-third (67.5%) of the clients spent 5–15 min both on pre- and post-test discussions altogether. Forty-two (10.0%) clients spent a time less than 5 min both for pre- and post-test discussion, and 95 (22.5%) discussed for more than 15 min in the pre- and post-test sessions altogether with the counselors (Table 3). The mean duration of counseling was 14 min for both the pre- and post-test sessions’ altogether.
Table 3.
Time spent by the PMTCT clients to get the services from governmental health facilities in Harar town, Harar, Ethiopia, 2020.
| Time variables | Frequency | |
|---|---|---|
| Number | % | |
| First appointment to get service served same day | 260 | 61.6 |
| 1–7 days | 147 | 34.8 |
| 8–14 days | 8 | 1.9 |
| 15–22 days | 7 | 1.7 |
| Waiting time to get service | ||
| <1.5 h | 366 | 86.7 |
| 1.5–3 h | 41 | 9.7 |
| >3 h | 15 | 3.6 |
| Time spent with the counselor | ||
| <5 min | 42 | 10.0 |
| 5–15 min (pre- and post-test sessions altogether) | 285 | 67.5 |
| >15 min | 95 | 22.5 |
PMTCT: prevention of mother-to-child transmission.
Concerning clients’ satisfaction with the services, 348 (82.5%) of the clients said that the counseling room’s privacy was maintained, and 357 (98.9%) of the clients were counseled by the same counselor both in the pre-test and post-test sessions. Three hundred eighty-nine (92.2%) felt comfortable with the counselors’ client handling/respect; 386 (91.5%) were satisfied with technical competence of the counselors; and if they were given an option to see another counselor, 324 (76.8%) would not like to see another counselor at that time. Most (91.9%) of the clients believed that they benefited from the counseling discussions; generally 379 (89.8%) of the clients reported being satisfied with the pre-test and/or post-test counseling discussions; and 388 (92.2%) of them would recommend the HCs to their relatives or friends who would like to use the service (Table 4).
Table 4.
Clients’ satisfaction with the PMTCT sites services in govrnmental health facilities in Harari Region, Ethiopia, 2020.
| Satisfaction issues | Yes | No | Total | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Was there enough privacy during the counseling? | 348 | 82.5 | 74 | 17.5 | 422 |
| Did you see same counselor before and after the test? | 357 | 98.94 | 1.1 | 361 | |
| Felt comfortable with counselor’s respect/handling | 389 | 92.2 | 33 | 7.8 | 422 |
| Satisfied with technical competence of the counselor? | 386 | 91.5 | 36 | 8.5 | 422 |
| Do you want to see another counselor just this time? | 98 | 23.2 | 324 | 76.8 | 422 |
| Generally have you benefited any from the pre- and/or post-test | |||||
| Counseling? | 388 | 91.9 | 34 | 8.1 | 422 |
| Generally are you satisfied with the pre- and/or post-test | |||||
| Counseling discussions? | 379 | 89.8 | 43 | 10.2 | 422 |
| Do you recommend this health center to others? | 388 | 92.2 | 33 | 7.8 | 421 |
PMTCT: prevention of mother-to-child transmission.
Discussion
This study is among the first attempts to evaluate the quality of ANC-linked HCT service as an intervention for PMTCT. But it may not have appropriate comparison due to the lack of similar studies with similar objectives using similar methods and target population in our country.
According to the reports of PMTCT coordinators of the HCs, all sites offered pre-test counseling, either as group or individually, and individual post-test counseling after blood test. All of the HCs had an HCT uptake rate of 90%–100% by ANC attendees. And HCs had a post-test client return rate of 90%–100% (for their results). This is in line with the findings of a retrospective study done in Addis Ababa among ANC attendees in five government HCs from 2002 to 2006, 14 which indicated that overall PMTCT utilization rate was 92.6% among PMTCT counseled ANC attendees. This may be as a result of an opt-out strategy being carried out throughout the country currently.
Availability of separate room for counseling is one of the minimum prerequisites in establishing HCT services. The counseling room should provide audiovisual privacy; conversations between clients and counselors should not be seen or overheard by others and the UNAIDS also specifically recommends a separate room for counseling which is at least 9 m2 wide. In this study, however, one of the health facilities had no a separate room dedicated for counseling to maintain privacy. This violates client rights to confidentiality during counseling, in that counseling information should remain between the counselor and counselee only. Moreover, the clients may become reluctant to openly/freely discuss personal issues, and may not be benefited from the service as expected.
All surveyed health facility had three or more trained PMTCT counselors; and all the counselors found in the health facility were nurses in their backgrounds before they become counselors. This may be an advantage since relatively nurses are expected to have better knowledge of health matters than non-health background counselors, and as a result, they would be more confident and skilled/experienced in counseling their clients better.
Poor quality counseling can result in misunderstanding and even resistance to behavior change. Counselors need adequate training and ongoing support and supervision to ensure that they give good quality counseling and can cope with their work load but this study indicated that two of the nine counselors had not taken the basic VCT training, six of the nine also never had a refreshment training, and all, but one counselor believed that they would need further refreshment training to be equipped with recent information about HIV and PMTCT, and how to conduct group counseling. Some PMTCT coordinators also shared the counselors’ idea and believed the compromise of the quality of their services as a result of shortage of trained human power and lack of refreshment training for their counselors. This finding may seem to be better than the finding of a study done in 2006 in Addis Ababa which indicated that 83.1% of the general VCT counselors had never been given an ongoing training. The lack of training, particularly an ongoing training and technical support of counselors working for the PMTCT program, could lead to burnout of counselors or to a decline in the quality of counseling services with time.15,16 Furthermore, it could be an important contributory factor in the low coverage of antiretroviral (ARV) among HIV-positive pregnant women if seropositive women do not receive adequate ongoing counseling to reinforce the importance of adherence.
Exit point interviews with the mothers revealed that 93.1% of the clients were addressed or urged about having an HIV blood test. However, only 68.4% of the pregnant mothers were counseled about HIV/AIDS. This indicates that a significant number of the clients were simply ordered to give blood sample for the test without the clients’ written consent and without being counseled about the topic. This initial experience may negatively influence subsequent attendance as the mere HIV testing averts little MTCT.17,18 The majority (90.6%) of those counseled about HIV/AIDS, however, reported to have comprehended the information. This is in line with the results of a study done in Thailand. 15
Almost three-fourth (74.6%) of the clients reported to have been counseled about issues associated with MTCT/PMTCT, but only less than half (42.4%) of the clients were counseled on infant feeding options. Of those clients who reported having been counseled on infant feeding options, only 61.8% reported to have comprehended/understood the counseling. A similar finding was observed in Kenya. 19
MTCT/PMTCT knowledge was inadequate as clients could not recall information given during counseling. This study indicated that there was statistically significant association between clients’ comprehension level of major discussion topics and a counseling duration that lasted for 5 min or more. This may indicate that the counseling time was inadequate for the clients to grasp the information.
HCT is a critical component of PMTCT programs and has been a recommended practice in overall HIV/AIDS prevention and care programs, with a high level of scientific evidence. Even though almost all the clients believed that HCT was helpful for the mother during pregnancy, only 78.7% correctly understood the purpose why HCT is needed particularly during pregnancy. This may be because of the short counseling time spent on counseling, as evidenced by association of longer (5–15 min) counseling time and correct knowledge why pregnant mothers undergo HCT particularly during their pregnancy time; or it may due to the hustle the counselors were making against time with the clients load. Knowledge why pregnant mothers undergo HCT during pregnancy was also found to be higher among residents of Harar, those who attended school up to grade 12, and among those clients who were in their third trimester. This may be due to the fact that these groups of clients relatively have access to information as a result of their schooling or repeated ANC attendance.
Even though the majority of the clients were served the same day without an appointment, a significant number (38.4%) of the clients reported to have been appointed to come back other days for the service. This is likely to discourage potential clients from utilizing the services, resulting in low uptake since this initial experience negatively influences subsequent attendance. Recall bias is a limitation of reporting on waiting time and could lead to misclassification bias. Ninety min is regarded as the acceptable waiting time. The vast majority (86.7%) of the clients stayed in the HCs up to 1.5 h, which is regarded as acceptable waiting time to get the services they wanted, and average waiting time was 39.75 min (±60.5). This is much better than the finding obtained from a study done in Kenya, 19 in which only 3.9% waited less than 90 min. This may encourage the clients to utilize the service and eventually improve the service outcome.
Assessing client satisfaction helps to identify service gaps which once addressed will improve the quality of services and hence utilization. Clients’ satisfaction may be considered to be one of the desired outcomes of care. An expression of satisfaction or dissatisfaction is also the client’s judgment on the quality of care in all its aspects, but particularly pertaining to the interpersonal process. However, it should be remembered that, unless special precautions are taken, clients may be reluctant to reveal their opinions for fear of alienating their attendants. 20 Concerning clients’ satisfaction with the services in this study, 92.2% felt comfortable with the counselors’ client handling/respect; 91.5% were satisfied with technical competence of the counselors; and 91.9% of the clients believed that they had benefited from the counseling discussions. Generally, 89.8% of the clients reported being satisfied with the pre-test and/or post-testing counseling discussions. This finding is similar to that done in Thailand. 15 Satisfaction with the service was associated with the duration of counseling.
Even though the overall quality of the counseling services in terms of content of the counseling, duration of the counseling and counselors’ competence (interpersonal relationships, gathering and giving information) of the surveyed HCs was more or less comparable to different studies done elsewhere, there still remains a lot to be improved to avert MTCT of HIV.
Generalizability may be limited by the small number of interview, especially with the counseling of HIV-positive cases. Even though the interview were made unobtrusive and sit through multiple sessions, performance bias may be present and also some limitation to describe medical words coordinators and counselors may deviate from their actual practice in interview sessions because of the presence of the interview.
The strength of this study was used (adapted) standardized UNAIDS Best Practice Collection Key Material to evaluate the quality of ANC-linked HCT. The limitation of the study was that generalizability may be limited by the small number of interview, especially with the counseling of HIV-positive cases and even though the interview was made unobtrusive and sit through multiple sessions, performance bias may be present and also some limitation to describe medical words coordinators and counselors may deviate from their actual practice in interview sessions because of the presence of the interview.
Conclusion
All the health facilities offered pre-test and post-test counseling, either as group or individually. Most of the health facilities had a separate room for counseling and mostly, the counseling and testing was performed on the day they come without further appointments. The uptake of HCT and a return rate to collect their test results among the ANC client was very high. Majority of the surveyed health facilities had more than two trained PMTCT counselors; however, most of the counselors complained that they lacked refreshment training. Some of the site coordinators also shared this idea and urged training of additional counselors and refreshment courses for those who are on job to improve the service quality.
Exit interview revealed that the basic topics were covered in most of the pre- and/or post-test sessions, and majority of those counseled comprehended the information; however, nearly a quarter of the clients did not understand why they were offered HCT particularly during their pregnancy time. The vast majority (86.7%) of the clients stayed in the health facilities up to 1.5 h, which is regarded as acceptable waiting time to get the services they wanted. Most of the exit clients also indicated to have spent unreasonably short counseling sessions; however, the vast majority of the women interviewed were satisfied with the counseling and counselor interactions, and believed to have gained new things they did not know.
All clients who had undergone HIV blood test had also undergone post-test individual counseling. However, even though the basic topics were covered, there were significant shortcomings in the comprehensiveness/depth of the information given, coverage of the clients, and in the time allotted for the counseling session.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211047757 for Assessment of quality antenatal care-linked HIV counseling and testing as an intervention for prevention of mother-to-child transmission of HIV at government health facilities in Harari region, Eastern Ethiopia by Masresha Leta, Siraj Adem and Biniyam Daniel in SAGE Open Medicine
Acknowledgments
We acknowledge Harar health science college and our special gratitude goes to collectors and study participants for their unreserved commitment and support. We are grateful to Harar Health Science College, as well as collectors and study participants, for their unwavering commitment and support.
Footnotes
Author contributions: All authors contributed significantly to the work reported, whether it was in the conception, study design, execution, data acquisition, analysis, and interpretation, or all of these areas; participated in the drafting, revising, or critical review of the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Research Ethics review committee of Harar Health Science College prior to the study, with an ethical approval number of CRPO/HHSC-NMBU/007/21.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by Harar Health Science College for data collection.
Informed consent: Participants were provided information about the study prior to data collection, and adult participants gave their informed consent (age greater than 18 years old). We got written agreement from guardians and assent from the minor group of participants who were under the age of 18.
ORCID iD: Masresha Leta  https://orcid.org/0000-0002-5788-0737
https://orcid.org/0000-0002-5788-0737
Data availability: The data used to support the findings of this study are available from the corresponding author upon request. The data used to support the findings of this study are included within the article. The data used to support the findings of this study were supplied by the authors under license and so cannot be made freely available. Requests for access to these data should be made to contacting the authors.
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Health Organization (WHO). WHO child growth standards and the identification of severe acute malnutrition in infants and children. Geneva: World Health Organization; Joint United Nations Children’s Fund (UNICEF) Universal, 2009. [PubMed] [Google Scholar]
- 2. WHO, HHS/CDC, UNICEF and USAID. “Protect yourself, your baby and your family from HIV/AIDS.” Testing and counseling for prevention of mother-to-child transmission of HIV (TC for PMTCT) support tools (Reference guide 2006). Geneva: WHO, HHS/CDC, http://www.womenchildrenhiv.org/wchiv?page=vc-10-00> (2006, accessed 3 July 2008). [Google Scholar]
- 3. MOH guidelines for prevention of mother-to-child transmission of HIV in Ethiopia . Addis Ababa, Ethiopia: Federal HIV/AIDS Prevention and Control Office, Federal Ministry of Health, 2007. [Google Scholar]
- 4. WHO. Towards universal access: scaling up priority HIV/ AIDS interventions in the health sector. Progress report, WHO, Geneva, 2010. [Google Scholar]
- 5. Hardon A, Vernooij E, Bongololo-Mbera G, et al. Women’s views on consent, counseling and confidentiality in PMTCT: a mixed-methods study in four African countries. BMC Public Health 2012; 12: Article 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Federal Democratic Republic of Ethiopia. Population and Housing Census of 2007 Ethiopia, Central Statistical Agency, Addis Ababa, Ethiopia, 2007. [Google Scholar]
- 7. Ministry of Health of Federal Democratic Republic of Ethiopia. Health sector development program IV. Annual performance report, Ministry of Health of Federal Democratic Republic of Ethiopia, Addis Ababa, Ethiopia, 2014. [Google Scholar]
- 8. UNAIDS. Global HIV and AIDS statistics. Geneva: UNAIDS, 2019 [Google Scholar]
- 9. UNICEF. State of the world’s children. New York: UNICEF, 2017. [Google Scholar]
- 10. Federal Democratic Republic of Ethiopia HIV Prevention and Control Office, Country Progress Report on the HIV Response, Federal Democratic Republic of Ethiopia HIV Prevention and Control Office, Addis Ababa, Ethiopia, 2011-2014. https://www.google.com/url?esrc=s&q=&rct=j&sa=U&url=https://www.unaids.org/sites/default/files/country/documents/ETH_narrative_report_2014 [Google Scholar]
- 11. Harari Regional Health Bureau. Harari regional health Bureau yearly bulletin report, 2011.
- 12. UNAIDS. Tools for evaluating HIV counseling and testing (UNAIDS BEST PRACTICE COLLECTION). Geneva: UNAIDS, 2000. [Google Scholar]
- 13. UNAIDS. AIDS epidemic update: Dec 2007. Geneva: UNAIDS, www.unaids.org (2007, accessed 9 July 2008). [Google Scholar]
- 14. Guidelines for assessing the utility of data from prevention of mother-to-child transmission (PMTCT) programmes for HIV sentinel surveillance among pregnant women . Geneva: UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance, 2013. [PubMed] [Google Scholar]
- 15. Department of Health, Ministry of Public Health Thailand. Evaluation of VCT in the National PMTCT Program. Nonthaburi, Thailand: Department of Health, Ministry of Public Health Thailand, 2012. [Google Scholar]
- 16. Bachore BB, Tafese F, Gebissa F, et al. Quality of prevention of mother to child transmission (PMTCT) of HIV services in public hospitals of Hadiya zone, Southern Ethiopia. Health Syst Policy Res 2018; 5(2): 72. [Google Scholar]
- 17. Stringer J. Nevirapine to prevent mother-to-child transmission of HIV-1 among women of unknown serostatus. Lancet 2003; 362: 1850–1853. [DOI] [PubMed] [Google Scholar]
- 18. Chopra M, Doherty T, Jackson D, et al. Preventing HIV transmission to children: quality of counseling of mothers in South Africa. Act Pediatric 2010; 94: 357–363. [DOI] [PubMed] [Google Scholar]
- 19. Delva W, Mutunga L, Quaghebeur A, et al. Quality and quantity of antenatal HIV counseling in a PMTCT programme in Mombasa, Kenya. AIDS Care 2013; 18(3): 189–193. [DOI] [PubMed] [Google Scholar]
- 20. Addis Ababa Health Bureau (AAHB). VCT service guideline. Addis Ababa, Ethiopia: Addis Ababa Health Bureau, 2004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211047757 for Assessment of quality antenatal care-linked HIV counseling and testing as an intervention for prevention of mother-to-child transmission of HIV at government health facilities in Harari region, Eastern Ethiopia by Masresha Leta, Siraj Adem and Biniyam Daniel in SAGE Open Medicine