Abstract
Objective
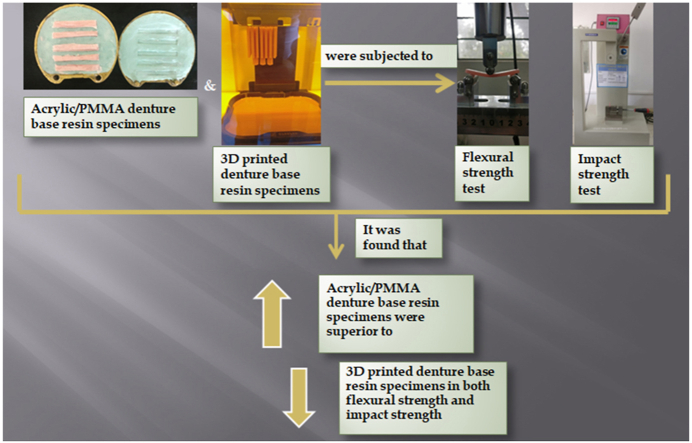
The present study aimed to evaluate and compare the flexural strength and impact strength of heat-cured acrylic/Polymethyl methacrylate (PMMA) denture base resin and 3D printed denture base resin.
Methods
60 rectangular specimens were fabricated from conventional heat-cured acrylic and 3D-printed denture base resins. 15 specimens each of heat-cured acrylic and 3D printed denture base resin were tested for flexural strength and impact strength. The flexural strength was assessed using three point bend test while impact strength was assessed by Izod impact test.
Results
The mean flexural strength of heat-cured acrylic resin was 92.01 ± 12.14 MPa and 3D printed denture base resin was 69.78 ± 7.54 MPa. The mean impact strength of heat-cured acrylic resin was 1.67 ± 0.79 kJ/m2 and 3D printed denture base resin was 1.15 ± 0.40 kJ/m2.The differences in mean impact and flexural strength between heat-cured acrylic and 3D printed denture base resins were statistically significant.
Conclusion
Heat-cured acrylic denture base resin (DPI heat-cure) had greater flexural and impact strength than 3D printed denture base resin (Next Dent denture 3D+).
Keywords: Acrylic resin, Denture base resin, 3D printed denture base resin, Flexural strength
Graphical abstract
1. Introduction
Edentulism has been a constant companion of human race since time immemorial. Many individuals experience either complete or partial loss of dentition in their life span and in order to rehabilitate their oral condition, dentures have been the most sought after solution. The need for complete dentures is set to rise from 53.8 million in 1991 to 61.0 million in 2020.1 The American College of Prosthodontists, has provided facts and figures which validate the need of dentures even today and for days to come.2
Acrylic resin/Polymethyl methacrylate (PMMA) is the most widely used denture base material till date and has undergone various modifications in order to enhance its physical and mechanical properties. Even after the modifications acrylic resin is far from an ideal material for dentures and requires more research and breakthroughs to provide a better material.3
A denture in an intraoral environment is subjected to various complex forces, which can initiate flexural and impact stresses. Since acrylic resin is less resistant to impact, flexure and fatigue stresses it is very common for dentures to fracture when subjected to these stresses.4,5
To address the problem of fractures in dentures, dentures procured either by subtractive manufacturing (CAD-CAM) or additive manufacturing (3D Printing) technology has been introduced as alternatives to the conventional dentures. Many studies have already been conducted on milled dentures but 3D printed dentures are new and hence, demand research which test their overall properties and compare it to its milled or conventional counterparts.
Thus, the purpose of this study was to compare the flexural and impact strength of conventional heat-cured acrylic denture base resin with the 3D printed denture base resin. The research hypothesis of this study was that the flexural and impact strength of 3D printed denture base resin is better than conventional heat-cured acrylic denture base resin.
2. Materials and methods
The materials chosen for this study were a conventional heat-cured acrylic denture base resin (DPI heat cure, Dental Products of India, Mumbai, India) and a 3D printed denture base resin (Next Dent Denture 3D+, 3D Systems, USA).
A total of 60 specimens were fabricated for the study. 15 specimens each of heat-cured acrylic and 3D printed denture base resin were tested for flexural strength test and 15 specimens each for impact strength.
2.1. Evaluation of flexural strength & impact strength
Heat-cured acrylic denture base resin specimen fabrication.
A total of 15 rectangular specimens of the dimension 64 mm × 10 mm x 3.3 mm as per ISO 1567:1999 for flexural strength testing and 15 rectangular specimens of the dimension 50 mm × 06 mm x 04 mm with a 1.2 mm notch in the middle as per ISO 1567:1999 for impact strength testing were fabricated.6,7 Templates made of wax were invested with dental stone (Kaldent, Kalabhai KarsoPvt Ltd) in brass flasks following the conventional two pour technique. After the dental stone set completely, dewaxing was done.The flasks were opened flushed with hot water and separating medium was coated over the mold. Heat-cure acrylic denture base resin was packed in the mold cavity. The flasks were then placed in a hydraulic press under 1500 psi pressure. The heat-polymerized acrylic specimens were prepared by placing the flaks in the polymerization unit. The standard processing cycle of the ADA specified short curing cycle was followed. The whole processing was carried out for 90 min at 74 °C and then raised to 100 °C for 30 min. After the curing cycle was completed, the flasks were bench cooled until they reached the room temperature before deflasking. Finally, the rectangular acrylic blocks were retrieved from the flask and were finished and polished.7
2.2. 3D printed denture base resin specimen fabrication
15 rectangular specimen each for flexural and impact strength testing similar to the dimensions of heat-cured acrylic resin specimen were designed (Materialise Magics, Belgium) and saved as a standard tessellation language (STL) file. A total of 15 3D-printed samples were prepared according to the STL file which was designed and programmed into the 3D printer unit (NextDent 5100 3D printer, 3D Systems, USA). After initial printing, the specimens were cleaned according to the manufacturer's instructions in an isopropyl alcohol bath (FormWash, Formlabs,USA). Post polymerization was carried in a UV light curing unit (FormCure,Formlabs, USA) and specimens were then finished and polished before testing.
2.3. Testing
Flexural strength test was carried out in accordance with ISO 1567:1999. 7Prior to flexural strength testing, length, width and thickness of each specimen were measured with a digital vernier caliper (Aerospace, China) with a measuring accuracy of ±0.1 mm. A Universal Testing Machine (International Equipments, India), was used to determine the flexural strength. The device consisted of a pair of adjustable supporting wedges placed at 50 mm apart and a loading wedge.
The specimen was centred on the device in such a way that the loading wedge, set to travel at a crosshead speed of 5 mm/min, engaged the centre of the upper surface of the specimen. The specimens were loaded until fracture occurred. The peak load (fracture load) was recorded in chart recorder. The formula to calculate flexural Strength is: S = 3PL/2bd,2 where S= Flexural strength (N/mm2 or MPa), P = load at fracture, L = distance between jig supports/span length (50 mm), b = specimen width (10 mm), d = specimen thickness (3.3 mm).
For Impact strength, the specimens from each group were subjected to testing using digital Izod/Charpy type impact testing machine (International Equipments, India). The specimen was kept on the jig in such a way that notch was facing towards the pendulum hammer. A 5.4 J pendulum hammer was used to impart the energy at the center of the specimen from the notched side. The specimens were subjected to the impact by the pendulum from an angle of 150° and the energy absorbed by the specimen up to the point of fracture was displayed on the digital display of the machine. The Impact strength was measured using the formula: IS = (Energy absorbed/[effective width × thickness]) × 1000, where IS = impact strength (kJ/m2), Energy absorbed is net energy absorbed in Joule, Effective width = total width - notch depth (6mm–1.2 mm = 4.8 mm) and Thickness = 4 mm.8
After the data collection, the results were tabulated and statistically analyzed. Descriptive statistics was used to obtain mean and the standard deviation among the test results. Unpaired ‘t’ test was used to compare the mean between the two denture base resins. Data was analyzed using SPSS software for Windows version 25.
3. Results
Mean flexural strength of heat-cured acrylic denture base resin was higher (92.01 ± 12.14 MPa) as compared to 3D printed denture base resin (69.78 ± 7.54 MPa). Unpaired/Independent ‘t’ test showed highly significant difference between the groups (p = 0.000). (Table 1).
Table 1.
Comparison of the flexural strength between heat-cured acrylic denture base resin and 3D printed denture base resin.
| GROUPS | N | Minimum | Maximum | Mean | SD | Mean difference | t- value | P value |
|---|---|---|---|---|---|---|---|---|
| Heat-cured acrylic denture base resin | 15 | 71.91 | 109.97 | 92.01 | 12.14 | 22.23 | 6.024 | 0.001 HS |
| 3D printed denture base resin | 15 | 56.82 | 82.96 | 69.78 | 7.54 |
Mean impact strength of heat-cured acrylic denture base resin was higher (1.67 ± 0.79 kJ/m2) as compared to 3D printed denture base resin (1.15 ± 0.40 kJ/m2). Statistically significant differences between the groups (p = 0.031) were observed (Table 2).
Table 2.
Comparison of the impact strength between heat-cured acrylic denture base resin and 3D printed denture base resins.
| GROUPS | N | Minimum | Maximum | Mean | SD | Mean difference | t-value | P value |
|---|---|---|---|---|---|---|---|---|
| Heat-cured acrylic denture base resin | 15 | 1.04 | 2.60 | 1.67 | 0.79 | 0.52 | 2.269 | 0.031 sig |
| 3D printed denture base resin | 15 | 1.04 | 2.60 | 1.15 | 0.40 |
4. Discussion
In this study, DPI heat cure resin was chosen over the other resins as it is easily available and is the most commonly used denture base resin in India. The emphasis was more on 3D printing technology as it is recent and demands to be researched upon, owing to low numbers of studies. The dimensions of the specimen and the experimental set up was in accordance with the ISO standards to evaluate flexural strength and impact strength of conventional heat-cured acrylic denture base resin and 3D printed denture base resin. The resins were not tested for the ISO compliance, as the rationale behind the cut-off values provided for mechanical properties were considered less evidenced.9
A denture is prone to fracture when subjected to sudden impact and flexural stresses.10 Heat-cured acrylic as denture base resin material has managed to fulfill the expectations of both the dentist and the patient for a long time, but, its low flexural and impact strength is still an issue. Reinforcements like addition of nanoparticles and modification to create high impact denture base materials have been successful to some extent, but they leave room for improvement as well as trial of new materials like 3D printed denture base resin.11, 12, 13
The specimens in the present study were subjected to three point bending. Chinchumnong et al. (1989) compared 3-point bending with 4-point bending flexural test for various polymers. The flexural strength values were statistically higher and more reliable for three point bending than four point bending according to the authors. Hence, three point bending was used in this study.14
The mean flexural strength of heat-cured acrylic denture base resin was 92.01 MPa whereas, the mean flexural strength of 3D printed denture base resin was 69.78 MPa. The ‘t’ value between the two was 6.024 with ‘p’ = 0.000 which suggested that results were highly significant. These findings were in accordance with a study conducted by Prpic’ et al. where 3D printed denture base resin was found to have least flexural strength when compared to conventional and milled denture base materials.15
Impact strength is another important property for a denture base resin. According to a study by AmitV.Naik, the most common cause of mandibular denture fracture and the 2nd most common cause of maxillary denture fracture was accidental dropping of denture while cleaning, insertion or removal.16 Flexural strength test gives the estimate of material performance under static loading whereas, impact strength test involves dynamic loading conditions and also computes the value of energy absorbed before the material fractures.17 In our study Izod method of impact testing was adopted as it is a common test used to check impact strength of plastic materials.17
The mean impact strength of heat-cured acrylic denture base resin was 1.67 kJ/m2 whereas, the mean impact strength of 3D printed denture base material was 1.15 kJ/m2. The ‘t’ value between the two was 2.269 with ‘p’ = 0.031 which suggested that the difference between the impact strength of the two resins was significant. These findings are contradictory to a research by Lee et al. where the impact strength of 3D printed denture base resin was more than the conventional heat cured denture base resins. The different brands of materials being tested could have been a possible reason for the contrasting results obtained in our research.18
The clinical implication of this study is that the 3D printed dentures can be valuable option apart from conventionally fabricated dentures with acceptable flexural and impact properties. Less chair side time and ease of fabrication of the dentures are additional advantages when using 3D printed denture base resin. Numerous research are in progress for improving the mechanical properties of 3 D printed denture base resins which may initiate the availability of better 3D printed resins compared to the conventional resins in the market.
4.1. Limitations
The materials were tested in laboratory conditions. The properties of both resin materials in the clinical setting would differ from the laboratory setting. So, further investigation should include closely simulated clinical conditions. Only conventional and 3D printed denture base resins were included. Resins fabricated by other techniques like CAD-CAM could also have been used in the study. Though DPI resin is not a high impact strength resin material it was included in the study. One brand of each type of denture base resin was used. Future research should involve many brands of acrylic and 3D printed denture base resins in testing and comparing the mechanical properties.
5. Conclusion
Within the confines of this study, it can be concluded that the flexural and impact strength of heat-cured acrylic denture base resin was greater than 3D printed denture base resin. Since high flexural and impact strength are desirable properties for denture base, 3D printed denture base resins are required to improve as the conventional heat-cured acrylic denture base resin showed better results.
Funding
This work was supported by JSSAHER Research Grants under Grant REG/DIR(R)/URG/54/2011–12/12,237.
Declaration of competing interest
No conflict of interest.
Acknowledgement
We sincerely thank Dr. Shiva Shankar Mahadevan for guiding and helping with all the aspects of additive manufacturing employed in this study.
Contributor Information
Mayank Chhabra, Email: chhabramayank961@gmail.com.
M. Nanditha Kumar, Email: dr.nandithakumarm@jssuni.edu.in.
K N RaghavendraSwamy, Email: knrswamy27@gmail.com.
H.M. Thippeswamy, Email: dentisttips@gmail.com.
References
- 1.Douglass C.W., Shih A., Ostry L. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 2002 Jan 1;87(1):5–8. doi: 10.1067/mpr.2002.121203. [DOI] [PubMed] [Google Scholar]
- 2.2020. Gotoapro.org.https://www.gotoapro.org/facts-figures/> Facts & Figures | American College of Prosthodontists. [online] Available at: Accessed. [Google Scholar]
- 3.Figuerôa R.M., Conterno B., Arrais C.A., Sugio C.Y., Urban V.M., Neppelenbroek K.H. Porosity, water sorption and solubility of denture base acrylic resins polymerized conventionally or in microwave. J Appl Oral Sci. 2018;26 doi: 10.1590/1678-7757-2017-0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanie T., Fujii K., Arikawa H., Inoue K. Flexural properties and impact strength of denture base polymer reinforced with woven glass fibers. Dent Mater. 2000 Mar 1;16(2):150–158. doi: 10.1016/s0109-5641(99)00097-4. [DOI] [PubMed] [Google Scholar]
- 5.Al‐Dwairi Z.N., Tahboub K.Y., Baba N.Z., Goodacre C.J. A comparison of the flexural and impact strengths and flexural modulus of CAD/CAM and conventional heat‐cured polymethyl methacrylate (PMMA) J Prosthodont. 2020 Apr;29(4):341–349. doi: 10.1111/jopr.12926. [DOI] [PubMed] [Google Scholar]
- 6.Standard International. International Organization for Standardization; Geneva, Switzerland: 1999. ISO 1567 for Dentistry—Denture Base Polymers. [Google Scholar]
- 7.Nitanda J., Wakasa K., Matsui H., Kasahara Y., Yamaki M., Matsui A. Fibre reinforcement in heat-cured, microwave-cured and visible light-cured base resins. J Mater Sci Mater Med. 1991 Apr 1;2(2):101–105. [Google Scholar]
- 8.Choksi R.H., Mody P.V. Flexural properties and impact strength of denture base resins reinforced with micronized glass flakes. J Indian Prosthodont Soc. 2016 Jul;16(3):264. doi: 10.4103/0972-4052.176532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinmassl O., Offermanns V., Stöckl W., Dumfahrt H., Grunert I., Steinmassl P.A. In vitro analysis of the fracture resistance of CAD/CAM denture base resins. Materials. 2018 Mar;11(3):401. doi: 10.3390/ma11030401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al‐Harbi F.A., Abdel‐Halim M.S., Gad M.M. Effect of nanodiamond addition on flexural strength, impact strength, and surface roughness of PMMA denture base. J Prosthodont. 2019 Jan;28(1):e417–e425. doi: 10.1111/jopr.12969. [DOI] [PubMed] [Google Scholar]
- 11.Khindria S.K., Mittal S., Sukhija U. Evolution of denture base materials. J Indian Prosthodont Soc. 2009 Apr 1;9(2):64. [Google Scholar]
- 12.John J., Gangadhar S.A., Shah I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J Prosthet Dent. 2001 Oct 1;86(4):424–427. doi: 10.1067/mpr.2001.118564. [DOI] [PubMed] [Google Scholar]
- 13.Archadian N., Kawano F., Ohguri T., Ichikawa T., Matsumoto N. Flexural strength of rebased denture polymers. J Oral Rehabil. 2000 Aug;27(8):690–696. doi: 10.1046/j.1365-2842.2000.00552.x. [DOI] [PubMed] [Google Scholar]
- 14.Chinchumnong P., Brooks S.C., Stafford Comparison of three and four- point flexural strength testing of denture base polymers. Dent Mater. 1989;5:2–5. doi: 10.1016/0109-5641(89)90082-1. [DOI] [PubMed] [Google Scholar]
- 15.Prpić V., Schauperl Z., Ćatić A., Dulčić N., Čimić S. Comparison of mechanical properties of 3D‐printed, CAD/CAM, and conventional denture base materials. J Prosthodont. 2020 Jul;29(6):524–528. doi: 10.1111/jopr.13175. [DOI] [PubMed] [Google Scholar]
- 16.Naik A.V. Complete denture fractures: a clinical study. J Indian Prosthodont Soc. 2009 Jul 1;9(3):148. [Google Scholar]
- 17.Abidin N.M., Sultan M.T., Shah A.U., Safri S.N. vol. 670. IOP Publishing; 2019 Nov. Charpy and Izod impact properties of natural fibre composites. (InIOP Conference Series: Materials Science and Engineering). 1. [Google Scholar]
- 18.Lee J., Belles D., Gonzalez M., Kiat-Amnuay S., Dugarte A., Ontiveros J. Impact strength of 3D printed and conventional heat-cured and cold-cured denture base acrylics. Int J Prosthodont (IJP) 2021 Feb 26 doi: 10.11607/ijp.7246. Epub ahead of print. PMID: 33651031. [DOI] [PubMed] [Google Scholar]