Abstract
BACKGROUND
The role of preoperative inflammatory biomarkers (PIBs) in predicting postoperative morbidity has been assessed in colorectal and otorhinolaryngeal surgery. However, data regarding the role that preoperative inflammatory biomarkers have on morbidity after pancreaticoduodenectomiy (PD) are less consistent.
AIM
To assess the utility of PIBs in predicting postoperative complications after pancreaticoduodenectomy.
METHODS
A database of 317 consecutive pancreaticoduodenectomies performed from April 2003 to November 2018 has been retrospectively analyzed. Data regarding preoperative neutrophil-to-lymphocyte ratio (NLR), derived NLR and C-reactive protein (CRP), and postoperative complications of 238 cases have been evaluated. Exclusion criteria were: age < 18-years-old, previous neoadjuvant treatment, absence of data about PIBs, concomitant hematological disorders, and presence of active infections at the moment of the surgery. PIBs were compared using Mann-Whitney’s test and receiver operating characteristic (ROC) analysis was performed to define the cutoffs. The positive predictive value (PPV) was computed to evaluate the probability to develop complication. P-values < 0.05 were considered statistically significant.
RESULTS
According to the literature findings, only four papers have been published reporting the relation between the inflammatory biomarkers and PD postoperative morbidity. A combination of preoperative and postoperative inflammatory biomarkers in predicting complications after PD and the utility of preoperative NLR in the development of postoperative pancreatic fistula (POPF) have been reported. The combination of PIBs and postoperative day-1 drains amylase has been reported to predict the incidence of POPF. According to our results, CRP values were significantly different between patients who had/did not have postoperative complications and abdominal collections (P < 0.05). Notably, patients with preoperative CRP > 8.81 mg/dL were at higher risk of both overall complications and abdominal collections (respectively P = 0.0037, PPV = 0.95, negative predictive value [NPV] = 0.27 and P = 0.016, PPV = 0.59, NPV = 0.68). Preoperative derived neutrophil-to-lymphocyte ratio (dNLR) (cut off > 1.47) was also a predictor of abdominal collection (P = 0.021, PPV = 0.48, NPV = 0.71). Combining CRP and dNLR, PPV increased to 0.67. NLR (cut off > 1.65) was significantly associated with postoperative hemorrhage (P = 0.016, PPV = 0.17, NPV = 0.98).
CONCLUSION
PIBs may predict complications after PD. During postoperative care, PIB levels could influence decisions regarding the timing of drains removal and the selection of patients who might benefit from second level diagnostic exams.
Keywords: Preoperative inflammatory markers, Pancreaticoduodenectomy, Complications, Neutrophil-to-lymphocyte ratio, Derived neutrophil-to-lymphocyte ratio
Core Tip: Inflammatory markers are involved in cancer’s pathogenesis and growth. In addition, their role in predicting post-operative complications in colorectal and otorhinolaryngeal surgery has been reported. Here, the role of preoperative inflammatory biomarkers in predicting postoperative complication after pancreaticoduodenectomy has been investigated.
INTRODUCTION
Periampullary tumors include cancers from the pancreatic head, distal bile duct, ampulla of Vater, and duodenum[1].Pancreaticoduodenectomy (PD) represents the gold standard of treatment for these malignancies. Even though its postoperative mortality is drastically decreased in high-volume centers, postoperative morbidity remains high, affecting approximately 30%-45% of patients[2,3].
The most common complications of PD are postoperative pancreatic fistula (POPF), delayed gastric emptying (DGE), postoperative hemorrhage (PPH), biliary fistula (BF), abdominal collections, and infections[4-6]. POPF is considered the "queen" of these complications since it is often the leading cause of other complications[7].
While factors, such as the presence of a soft pancreas, the small size of the Wirsung, common bile duct stumps, and previous biliary drainage, have been recognized to increase the risk of PD morbidity[8,9], less is known about the role that systemic inflammatory factors play in the development of complications after PD.
Currently, inflammatory biomarkers [e.g., C-reactive protein (CRP), neutrophil count, Glasgow Prognostic Score (GPS), and neutrophil-to-lymphocyte ratio (NLR)], are proven to have an independent prognostic role in the prediction of cancer-specific and postsurgical survival of different malignancies, including periampullary malignancies[10-12].Moreover, their efficacy in predicting postoperative morbidity in colorectal, esophageal, and otorhinolaryngeal surgery has been assessed. Specifically, NLR > 3 is associated with anastomotic failure in colorectal surgery, while decreased levels of albumin and lymphocytes are associated with a higher incidence of complications after esophageal surgery and NLR < 3.5 and platelet-lymphocyte ratio (PLR) < 160 are correlated with impaired wound healing in head and neck surgery[13-16].
Data regarding the role that preoperative inflammatory biomarkers (PIBs) have on morbidity after PD are less consistent to the best of our knowledge[17].This study aimed to carry out a literature review to analyze and report the role that PIBs have on developing complications after PD. Personal monocentric experience focused on this topic has also been reported.
MATERIALS AND METHODS
Review methods
Literature research was performed, and articles about randomized clinical trials, observational cohort studies, systematic reviews, and original articles focusing on the role of PIBs on postoperative complications after PD were all considered. Only articles written in English with available full text have been analyzed. The last literature review was carried out on December 1st, 2020.
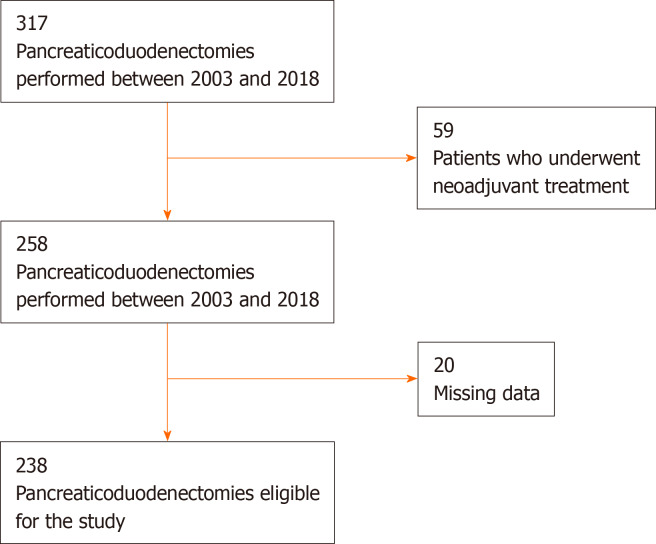
Materials and methods for the center experience analysis
A database of consecutive PDs performed at the Department of General Surgery of the University Campus Bio-Medico of Rome from April 2003 to November 2018 was retrospectively analyzed. The local Ethical Committee approved the study (28/19 OSS ComEt CBM). Inclusion criteria were: Adult patients (≥ 18-years-old) affected by periampullary tumor who underwent PD. Exclusion criteria were: Age < 18-years-old, previous neoadjuvant treatment, absence of data about PIBs, concomitant hematological disorders, or presence of active infections at the moment of the surgery (Figure 1).
Figure 1.
Flow diagram of patients’ selection.
Data regarding preoperative NLR, derived neutrophil-to-lymphocyte ratio (dNLR), platelet-to-lymphocyte ratio (PLR), C-reactive protein (CRP), and postoperative complications have been analyzed. NLR, dNLR and PLR were defined and calculated as previously reported: NLR (neutrophil/Lymphocyte), dNLR (neutrophil count/(White blood cell count- Neutrophil count)), PLR (Platelet count/Lymphocyte count)[18].
CRP was measured by the Dimension Vista® 500 System (Siemens Healthcare Diagnostics, Germany).
POPF, DGE, and PPH have been defined according to the internationally recognized standard[4-6].
Statistical analysis
Continuous variables (Plasmatic levels of NLR, dNLR, PLR, CRP) have been reported as median (95%CI, confidence intervals) according to their distributions, and differences have been tested with the Mann-Whitney's test due to data distribution (i.e. non-parametric according to the Shapiro-Wilks test for Normality). Categorical variables have been reported as numbers and relative frequencies, and differences across groups were tested by the chi-squared test. Receiver operating characteristic (ROC) analysis was performed among independent variables to define the cutoff point for plasma NLR, dNLR, PLR, CRP values to predict postoperative complications. Odds ratios (OR) and their 95%CI were calculated to evaluate the association between patients who underwent neoadjuvant treatment and postoperative complications. Chi-square and Fisher's exact test was used to confirm the statistical significance. All P values < 0.05 were considered statistically significant. Data have been analyzed using Med-Calc 18.11.3 statistical package (MedCalc Software, Mariakerke, Belgium).
RESULTS
To the best of our knowledge, only four papers investigated the role of PIBs, alone or in combination with postoperative inflammatory markers or other clinical parameters, on post-PD morbidity. Solaini et al[17] and, more recently, Zhang et al[19] investigated the combination of preoperative and postoperative inflammatory biomarkers in predicting complications after PD. Kumamoto et al[20] reported the role of preoperative NLR in the development of POPF, while Caputo et al[21] highlighted the utility of combining PIBs together with postoperative day 1-drains amylase (POD1-da) to predict the incidence of POPF.
Specifically, Solaini and colleagues, using a cohort of 378 patients who underwent to PD, demonstrated the role of preoperative white blood cell count (cut-off > 8.5 × 103/mL, AUC 0.591, 95%CI: 10.53-0.64, P = 0.02), postoperative day 2 NLR (cut-off > 12.3, AUC 0.605, 95%CI: 0.55-0.66, P = 0.005) and CRP dosed on postoperative day 4 (cut-off > 188 mg/L, AUC 0.645, 95%CI: 0.58-0.7, P = 0.004) in predicting postoperative complications. The authors reported a higher accuracy and positive predictive value (PPV) (76.8% and 71.4%) combining the above-mentioned inflammatory markers. Nonetheless, according to this study's findings, increased NLR on postoperative day 2 and CRP > 272 mg/L on postoperative day 3 were significantly associated with POPF.
Zhang et al[19] analyzed the development of sepsis in 31 out of 138 PDs. The Authors studied inflammatory markers (IL-6, IL-2, IL-1, IL-10, tumor necrosis factor (TNF), and CRP) preoperatively and in POD1 in those who developed the complication and compared marker's levels with the group without sepsis. Preoperative IL-6, at the cutoff value of 5.26 pg/mL, resulted in an independent risk factor for sepsis, and was the only PIB significantly associated with a 3-fold higher risk of developing sepsis after PD (OR = 3.31, 95%CI :1.37-12.89, P = 0.044).
Kumamoto et al[20] reported the association between PIBs and post-PD Clavien-Dindo grade ≥ III complications. On a series of 84 PDs, 39 (46%) patients developed major postoperative complications. Higher neutrophil count (P < 0.05) and NLR (P < 0.01) were significantly able to predict complications as well as body mass index (BMI) (P < 0.01) did. The optimal cutoff values detected were neutrophil count 2.727/µL, NLR > 2.0 and BMI > 23.0 kg/m2. Using multivariate logistic regression analysis, independent risk factors for major postoperative complications were NLR > 2.0 (OR = 6.77, 95.0%CI: 2.4421.13; P < 0.001) and BMI > 23.0 kg/m2 (OR = 3.83, 95.0%CI: 1.3511.83; P = 0.011).
In Caputo et al[3,18,21], even though POD1-da levels were confirmed to be the main factor able to predict the risk of POPF, the combinations of PIBs with POD1-da levels allowed to improve POPF's PPV. Specifically, NLR > 3.2, dNLR > 3 and PLR > 137 increased up to 89% the POD1-da levels PPV for POPF development.
Centre experience results
Baseline demographic characteristics of the 238 PDs included in the study are reported in Table 1. The median age was 68 years (interquartile range [IQR] = 61-75 years). Male patients represented 57% of the cases and the median BMI was 24.1 kg/m2 (IQR = 22.23-27.71 kg/m2). At least one postoperative complication was observed in 78% of the cases. The main postoperative complications were: POPF 50.8% (121/238), DGE 30.6% (73/238), PPH 14.2% (34/238), abdominal collection 39.5% (94/238), and biliary fistula 14.2% (34/238). A biochemical leak occurred in 30.6% of POPF, while clinically relevant Grade B-C fistula was detected in 20% of these patients. PIBs values are listed in Table 2.
Table 1.
Demographic characteristics of the study population median value and postsurgical infections characteristics
|
Demographic characteristics (n = 238) and postoperative complications
| |
| Age | 68 (59-74) |
| Median (IQR) | |
| Sex, n (%) | |
| Male | 141 (59.2) |
| Female | 97 (40.8) |
| BMI | |
| Median (kg/m2) | 24.9 (22.2-27.7) |
| Postoperative complications, n (%) | |
| Overall complications | 191 (80.2) |
| Pancreatic fistula | 121(50.8) |
| Pancreatic fistula Grade A | 73 (30.6) |
| Pancreatic fistula Grade B-C | 48 (20) |
| Hemorrhage | 34 (14.2) |
| DGE | 73 (30.6) |
| Abdominal collection | 94 (39.5) |
| Biliary fistula | 35 (14.7) |
| Sepsis | 21 (8.8) |
| Infection of wound | 23 (9.6) |
BMI: Body mass index; DGE: Delayed gastric emptying; IQR: Interquartile range, 25th percentile to 75th percentile.
Table 2.
Median levels of pre-operative inflammatory biomarkers
|
Preoperative inflammatory biomarkers
|
Median value
|
| NLR (IQR) | 227 (164-306) |
| dNLR (IQR) | 1635 (117-21) |
| CRP (IQR) | 53 mg/L (25-1633) |
CRP: C-reactive protein; dNLR: Derived neutrophil-to-lymphocyte ratio; IQR: Interquartile range, 25th percentile to 75th percentile; NLR: Neutrophil-to-lymphocyte ratio.
According to the Mann-Whitney's test, no relationship between PIBs and POPF occurrence was found. On the contrary, significant associations have been found between preoperative CRP and overall complications (P = 0.01) and between preoperative NLR and PPH (P = 0.03). Moreover, preoperative dNLR and CRP were significantly associated with abdominal collection (P = 0.026 and P = 0.017, respectively).
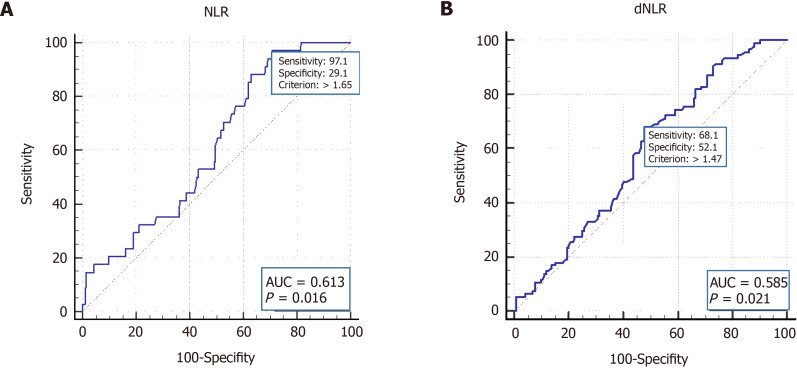
By ROC curve analysis, optimal cutoffs for PIBs and post-PD complications have been calculated. In detail, preoperative NLR at the cut off of > 1.65 was significantly associated with PPH (P = 0.016, PPV = 0.17, negative predictive value [NPV] = 0.98) (Figure 2A).
Figure 2.
Receiver operating characteristic curves of preoperative neutrophil-to-lymphocyte ratio in postoperative hemorrhage and derived neutrophil-to-lymphocyte ratio in abdominal collections. A: Preoperative neutrophil-to-lymphocyte ratio in postoperative hemorrhage; B: Derived neutrophil-to-lymphocyte ratio in abdominal collections. AUC: Area under the curve; d-NLR: Derived neutrophil-to-lymphocyte ratio; NLR: Neutrophil-to-lymphocyte ratio;.
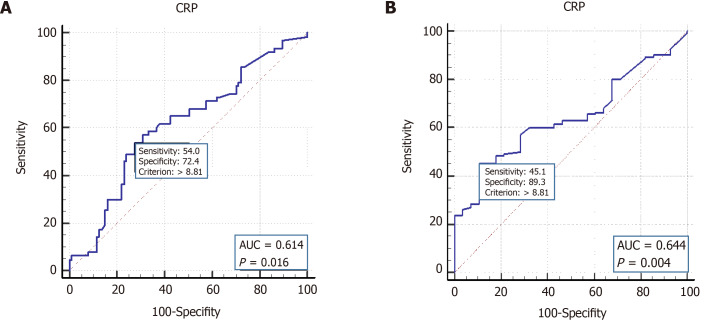
Preoperative CRP levels > 8.81 mg/dL have been found associated with higher rate of overall postoperative complications (P = 0.0037, PPV = 0.95, NPV = 0.27) and abdominal collections (P = 0.016, PPV = 0.59, NPV = 0.68) (Figure 3, Table 3). Preoperative levels of dNLR at the cut off of > 1.47 resulted significantly associated with abdominal collections (P = 0.021, PPV = 0.48, NPV = 0.71) (Figure 2B). Combining CRP and dNLR, PPV increased to 0.67.
Figure 3.
Receiver operating characteristic curves of preoperative C-reactive protein in abdominal collections and overall complications. A: C-reactive protein in abdominal collections; B: Overall complications. AUC: Area under the curve; CRP: C-reactive protein.
Table 3.
Statistical significance of preoperative inflammatory biomarkers
|
|
Overall complications
|
Abdominal collection
|
PPH
|
| NLR > 1.65 | Ns | Ns | P = 0.016 |
| dNLR > 1.47 | Ns | P = 0.021 | |
| CRP > 881 mg/L | P = 0.0037 | P = 0.016 | Ns |
CRP: C-reactive protein; dNLR: Derived neutrophil-to-lymphocyte ratio; NLR: Neutrophil-to-lymphocyte ratio; Ns: Not significant; PPH: Postoperative hemorrhage.
DISCUSSION
Different studies demonstrated the role that inflammation plays in carcinogenesis. For example, the role of inflammation in pancreatic cancer patients has been investigated as well, and the association between inflammatory biomarkers and the prognosis of these patients was reported[22]. Cytokines and proangiogenic factors, whose production is regulated by white blood cells and platelets, have been mainly investigated[23].
The role that serum inflammatory biomarkers can play in the development of postoperative complications has been reported for surgery performed for different solid tumors. However, there is still a lack of data about the role that inflammation can play in developing complications after PD. Nonetheless, most of the literature on this topic focuses on inflammatory biomarkers dosed and calculated postoperatively[24].
The papers found in our literature research mainly reported data underlining the relationship between pre-operative and/or postoperative inflammatory markers and oncological outcomes, such as disease-free survival and overall survival in patients affected by periampullary tumors. Postoperative complications after PD were mainly related to postoperative inflammatory markers instead of PIBs.
According to Solaini et al[17], the combination of preoperative and postoperative levels of white blood cells, NLR, and CRP predict the development of postoperative complications after PD with particular regard to POPF. The association between preoperative NLR and the higher risk of POPF has also been reported by Kumamoto et al[20]. Zhang et al[19] has proposed preoperative IL-6 and postoperative PCT and CRP levels in a model to estimate the risk of sepsis after PD. Therefore, on this basis and considering the strong association between IL-6 and intestinal lipopolysaccharide, the authors suggested using preoperative immunonutrition to decrease the levels of IL-6 and, consequently, the risk of sepsis[21].
Even though POD1-da levels still represent the main indicator of the risk of POPF when compared to PIBs as reported by Caputo, the combination of preoperative NLR, NLR, and PLR with POD1-da levels was effective in predicting the increased risk of grade C POPF[21].
In our present study, PIBs such as CRP, NLR, and dNLR was significantly associated with the development of surgical complications after PD, particularly abdominal collections and postoperative bleeding. Specifically, higher CRP levels significantly predict overall complications, while lower values of NLR and dNLR were associated with a lower risk of PPH and abdominal collection, respectively.
These findings are in part in agreement with Uchida and colleagues, who reported postoperative CRP's role in the prediction of the hemorrhage post PD. According to Uchida, patients with high CRP in POD3 are at higher risk of PPH since at higher risk of grade C POPF[25,26].From the literature and our findings, it is possible to establish the role of PIBs in predicting the development of complications after PD. However, as already highlighted by other authors, the rationale behind the association between preoperative inflammation and PD postoperative complications has yet to be fully defined.
Elevated NLR and PLR can distinguish spontaneous subarachnoid hemorrhage from acute headache[27] and were associated with gastrointestinal bleeding in patients with cerebral hemorrhage[28].
Moreover, an increased inflammatory state would generate a cytokine storm with consequent microvascular alterations responsible for impaired wound and anastomotic healing[29].
Nonetheless, according to Nakanishi, the systemic inflammatory response determines a dysfunction of the endothelium that loses its ability to produce prostacyclin and nitric oxide with a consequent decrease of dilatation and antithrombotic function inhibiting wound healing[30]
Based on what was highlighted in the literature and our findings, the routine use of anti-inflammatory drugs could be considered in patients with altered inflammatory status before PD, just as was done to prevent pancreatitis after endoscopic retrograde cholangiopancreatography (ERCP)[31,32].
The present work is not without limitations. Our experience is retrospective, and there is a lack of direct evidence confirming the role of preoperative inflammatory status in PD complications development. Therefore, as already suggested by others, these findings must be interpreted with caution.
Our study's strengths are the homogeneity of the series; since we excluded patients who underwent neoadjuvant treatments that may have altered the inflammatory status and the analysis of only preoperative inflammatory biomarkers allowing to exclude the effect of the surgical trauma and of not yet clinically evident complications.
CONCLUSION
Although the role of inflammatory biomarkers has been assessed in predicting oncological outcomes of patients affected by periampullary tumors who underwent PD, the efficacy of PIBs in predicting postoperative morbidity has been marginally investigated. Despite the limited experiences published in the literature, the available data and results of our experience show that preoperative NLR, d-NLR, and CRP could predict the risk of complications after PD with particular regard to abdominal collections and hemorrhage. On this basis, PIBs may represent simple, cheap, and valuable tools to predict the risk of complications after PD and promote early interventions to reduce postoperative morbidity.
ARTICLE HIGHLIGHTS
Research background
Role of preoperative inflammatory biomarkers (PIBs) in predicting postoperative morbidity has been widely assessed in colorectal and otorhinolaryngeal surgery.
Research motivation
To date, little is known about the role of PIBs in predicting pancreaticoduodenectomy (PD) postoperative complications.
Research objectives
To exploit the utility of PIBs in predicting the postoperative course after PD.
Research methods
A literature research and a retrospective analysis of data from a prospective collected database of 317 consecutive pancreaticoduodenectomies have been performed. Data regarding preoperative neutrophil-to-lymphocyte ratio (NLR), derived NLR (dNLR), platelet-lymphocyte ratio, C-reactive protein (CRP) and postoperative complications of 238 cases have been analyzed. PIBs were compared using MannWhitney’s test and receiver operating characteristic (ROC) analysis was performed to define the cutoffs.
Research results
Patients with preoperative CRP > 8.81 mg/dL were at higher risk of both overall complications and abdominal collections (respectively P = 0.0037, PPV = 0.95, NPV = 0.27 and P = 0.016, PPV = 0.59, NPV = 0.68). _Preoperative dNLR (cut off > 1.47) was also predictor of abdominal collection (P = 0.021, PPV = 0.48, NPV = 0.71). Combining CRP and dNLR, PPV increased to 0.67. NLR (cut off > 1.65) was significantly associated with postoperative hemorrhage (P = 0.016, PPV = 0.17, NPV = 0.98).
Research conclusions
PIBS are cost-effective tools that may predict complications after pancreaticoduodenectomy and could be useful in the postoperative management.
Research perspectives
In clinical practice, PIBs could be used during the postoperative course of PD decisions regarding timing of drains removal and selection of patients who can benefit from second level diagnostic exams (e.g., CT scan).
Footnotes
Institutional review board statement: The local Ethical Committee approved the study (28/19 OSS ComEt CBM).
Informed consent statement: Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement: All authors declare that they do not have any conflict of interest.
Data sharing statement: Dataset will be available from the corresponding author at d.caputo@unicampus.it according to local laws.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Peer-review started: January 25, 2021
First decision: May 3, 2021
Article in press: July 13, 2021
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: do Monte Junior ES S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Wu RR
Contributor Information
Alessandro Coppola, Department of Surgery, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Vincenzo La Vaccara, Department of General Surgery, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Lorenza Caggiati, Department of General Surgery, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Ludovico Carbone, Department of General Surgery, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Silvia Spoto, Department of Internal Medicine, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Massimo Ciccozzi, Medical Statistics and Epidemiology Unit, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Silvia Angeletti, Unit of Clinical Laboratory Science, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Roberto Coppola, Department of General Surgery, University Campus Bio-Medico di Roma, Rome 00128, Italy.
Damiano Caputo, Department of General Surgery, University Campus Bio-Medico di Roma, Rome 00128, Italy. d.caputo@unicampus.it.
References
- 1.Kamarajah SK. Pancreaticoduodenectomy for periampullary tumours: a review article based on Surveillance, End Results and Epidemiology (SEER) database. Clin Transl Oncol. 2018;20:1153–1160. doi: 10.1007/s12094-018-1832-5. [DOI] [PubMed] [Google Scholar]
- 2.Giuliano K, Ejaz A, He J. Technical aspects of pancreaticoduodenectomy and their outcomes. Chin Clin Oncol. 2017;6:64. doi: 10.21037/cco.2017.09.01. [DOI] [PubMed] [Google Scholar]
- 3.Caputo D, Angeletti S, Ciccozzi M, Cartillone M, Cascone C, La Vaccara V, Coppola A, Coppola R. Role of drain amylase levels assay and routinary postoperative day 3 abdominal CT scan in prevention of complications and management of surgical drains after pancreaticoduodenectomy. Updates Surg. 2020;72:727–741. doi: 10.1007/s13304-020-00784-9. [DOI] [PubMed] [Google Scholar]
- 4.Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M International Study Group on Pancreatic Surgery (ISGPS) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584–591. doi: 10.1016/j.surg.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Surgery. 2007;142:761–768. doi: 10.1016/j.surg.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–25. doi: 10.1016/j.surg.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Nahm CB, Connor SJ, Samra JS, Mittal A. Postoperative pancreatic fistula: a review of traditional and emerging concepts. Clin Exp Gastroenterol. 2018;11:105–118. doi: 10.2147/CEG.S120217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu QY, Zhang WZ, Xia HT, Leng JJ, Wan T, Liang B, Yang T, Dong JH. Analysis of risk factors for postoperative pancreatic fistula following pancreaticoduodenectomy. World J Gastroenterol. 2014;20:17491–17497. doi: 10.3748/wjg.v20.i46.17491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malgras B, Duron S, Gaujoux S, Dokmak S, Aussilhou B, Rebours V, Palazzo M, Belghiti J, Sauvanet A. Early biliary complications following pancreaticoduodenectomy: prevalence and risk factors. HPB (Oxford) 2016;18:367–374. doi: 10.1016/j.hpb.2015.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng H, Luo G, Lu Y, Jin K, Guo M, Xu J, Long J, Liu L, Yu X, Liu C. The combination of systemic inflammation-based marker NLR and circulating regulatory T cells predicts the prognosis of resectable pancreatic cancer patients. Pancreatology. 2016;16:1080–1084. doi: 10.1016/j.pan.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 11.Dolan RD, McSorley ST, Horgan PG, Laird B, McMillan DC. The role of the systemic inflammatory response in predicting outcomes in patients with advanced inoperable cancer: Systematic review and meta-analysis. Crit Rev Oncol Hematol. 2017;116:134–146. doi: 10.1016/j.critrevonc.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Garcea G, Cairns V, Berry DP, Neal CP, Metcalfe MS, Dennison AR. Improving the diagnostic yield from staging laparoscopy for periampullary malignancies: the value of preoperative inflammatory markers and radiological tumor size. Pancreas. 2012;41:233–237. doi: 10.1097/MPA.0b013e31822432ee. [DOI] [PubMed] [Google Scholar]
- 13.Josse JM, Cleghorn MC, Ramji KM, Jiang H, Elnahas A, Jackson TD, Okrainec A, Quereshy FA. The neutrophil-to-lymphocyte ratio predicts major perioperative complications in patients undergoing colorectal surgery. Colorectal Dis. 2016;18:O236–O242. doi: 10.1111/codi.13373. [DOI] [PubMed] [Google Scholar]
- 14.Kang WM, Zhu CZ, Yang XX, Yu JC, Ma ZQ, Ye X, Li K, Liu D. Application of the Onodera prognostic nutrition index and neutrophil-to-lymphocyte ratio in risk evaluation of postoperative complications in Crohn's disease. Sci Rep. 2017;7:8481. doi: 10.1038/s41598-017-09265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maruyama Y, Inoue K, Mori K, Gorai K, Shimamoto R, Onitsuka T, Iguchi H, Okazaki M, Nakagawa M. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as predictors of wound healing failure in head and neck reconstruction. Acta Otolaryngol. 2017;137:106–110. doi: 10.1080/00016489.2016.1218047. [DOI] [PubMed] [Google Scholar]
- 16.Nozoe T, Kimura Y, Ishida M, Saeki H, Korenaga D, Sugimachi K. Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol. 2002;28:396–400. doi: 10.1053/ejso.2002.1257. [DOI] [PubMed] [Google Scholar]
- 17.Solaini L, Atmaja BT, Watt J, Arumugam P, Hutchins RR, Abraham AT, Bhattacharya S, Kocher HM. Limited utility of inflammatory markers in the early detection of postoperative inflammatory complications after pancreatic resection: Cohort study and meta-analyses. Int J Surg. 2015;17:41–47. doi: 10.1016/j.ijsu.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Caputo D, Caricato M, Coppola A, La Vaccara V, Fiore M, Coppola R. Neutrophil to Lymphocyte Ratio (NLR) and Derived Neutrophil to Lymphocyte Ratio (d-NLR) Predict Non-Responders and Postoperative Complications in Patients Undergoing Radical Surgery After Neo-Adjuvant Radio-Chemotherapy for Rectal Adenocarcinoma. Cancer Invest. 2016;34:440–451. doi: 10.1080/07357907.2016.1229332. [DOI] [PubMed] [Google Scholar]
- 19.Zhang H, Meng F, Lu S. Risk factors of sepsis following pancreaticoduodenectomy based on inflammation markers and clinical characteristics. ANZ J Surg. 2020;90:1428–1433. doi: 10.1111/ans.15791. [DOI] [PubMed] [Google Scholar]
- 20.Kumamoto Y, Kaizu T, Tajima H, Nishizawa N, Ei S, Igarashi K, Watanabe M. Neutrophil-to-lymphocyte ratio as a predictor of postoperative morbidity in patients with distal cholangiocarcinoma. Mol Clin Oncol. 2018;9:362–368. doi: 10.3892/mco.2018.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caputo D, Coppola A, Cascone C, Angeletti S, Ciccozzi M, La Vaccara V, Coppola R. Preoperative systemic inflammatory biomarkers and postoperative day 1 drain amylase value predict grade C pancreatic fistula after pancreaticoduodenectomy. Ann Med Surg (Lond) 2020;57:56–61. doi: 10.1016/j.amsu.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanjay P, de Figueiredo RS, Leaver H, Ogston S, Kulli C, Polignano FM, Tait IS. Preoperative serum C-reactive protein levels and post-operative lymph node ratio are important predictors of survival after pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. JOP. 2012;13:199–204. [PubMed] [Google Scholar]
- 23.Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005;91:181–184. doi: 10.1002/jso.20329. [DOI] [PubMed] [Google Scholar]
- 24.Warschkow R, Ukegjini K, Tarantino I, Steffen T, Müller SA, Schmied BM, Marti L. Diagnostic study and meta-analysis of C-reactive protein as a predictor of postoperative inflammatory complications after pancreatic surgery. J Hepatobiliary Pancreat Sci. 2012;19:492–500. doi: 10.1007/s00534-011-0462-x. [DOI] [PubMed] [Google Scholar]
- 25.Aosasa S, Mochizuki H, Yamamoto T, Ono S, Ichikura T. A clinical study of the effectiveness of oral glutamine supplementation during total parenteral nutrition: influence on mesenteric mononuclear cells. JPEN J Parenter Enteral Nutr. 1999;23:S41–S44. doi: 10.1177/014860719902300511. [DOI] [PubMed] [Google Scholar]
- 26.Uchida Y, Masui T, Hashida K, Machimoto T, Nakano K, Yogo A, Sato A, Nagai K, Anazawa T, Takaori K, Uemoto S. Impact of vascular abnormality on contrast-enhanced CT and high C-reactive protein levels on postoperative pancreatic hemorrhage after pancreaticoduodenectomy: A multi-institutional, retrospective analysis of 590 consecutive cases. Pancreatology. 2021;21:263–268. doi: 10.1016/j.pan.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Yang P, Gu B, Wang J. Comparison of the Diagnostic Values of Neutrophil, Neutrophil to Lymphocyte Ratio, and Platelet to Lymphocyte Ratio in Distinguishing Spontaneous Subarachnoid Hemorrhage from Nontraumatic Acute Headache. Clin Lab. 2019;65 doi: 10.7754/Clin.Lab.2019.190301. [DOI] [PubMed] [Google Scholar]
- 28.Zou Y, Zhang W, Huang C, Zhu Y. Clinical significance of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in acute cerebral hemorrhage with gastrointestinal hemorrhage, and logistic regression analysis of risk factors. Exp Ther Med. 2019;18:1533–1538. doi: 10.3892/etm.2019.7778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yao C, Zhang Z, Yao Y, Xu X, Jiang Q, Shi D. Predictive value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio for acute deep vein thrombosis after total joint arthroplasty: a retrospective study. J Orthop Surg Res. 2018;13:40. doi: 10.1186/s13018-018-0745-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakanishi N, Sato M, Shirai K, Suzuki K, Tatara K. White blood cell count as a risk factor for hypertension; a study of Japanese male office workers. J Hypertens. 2002;20:851–857. doi: 10.1097/00004872-200205000-00018. [DOI] [PubMed] [Google Scholar]
- 31.Patai Á, Solymosi N, Mohácsi L, Patai ÁV. Indomethacin and diclofenac in the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis of prospective controlled trials. Gastrointest Endosc. 2017;85:1144–1156.e1. doi: 10.1016/j.gie.2017.01.033. [DOI] [PubMed] [Google Scholar]
- 32.Serrano JPR, de Moura DTH, Bernardo WM, Ribeiro IB, Franzini TP, de Moura ETH, Brunaldi VO, Salesse MT, Sakai P, De Moura EGH. Nonsteroidal anti-inflammatory drugs vs placebo for post-endoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and meta-analysis. Endosc Int Open. 2019;7:E477–E486. doi: 10.1055/a-0862-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]