Abstract
Background
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common malignancy in the world, and it is extremely rare that HNSCC occurs with salivary gland tumor(s). Here, we presented a rare case that squamous cell carcinoma of floor of mouth occurred simultaneously with Warthin’s tumor in the submandibular gland.
Case Presentation
A 65-year-old Chinese male presented with a 6-month history of an ulcer on the floor of the mouth and preoperative biopsy pathological examination demonstrated it was squamous cell carcinoma. Postoperative microscopic examination unexpectedly found the carcinoma occurred simultaneously with two Warthin’s tumors in the right submandibular gland.
Conclusion
This case serves as a reminder to oral surgeons that in head and neck carcinomas, enlarged lump may be caused by inflammation or secondary primary focus rather than lymph node metastasis. Recognition and implication of the unexpected pathologic findings in patients with head and neck cancer are thus worth of studying.
Keywords: Multiple primary tumors (MPTs), Warthin’s tumor, Head and neck squamous cell carcinoma (HNSCC), Submandibular gland
Introduction
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common malignancy in the world, and on unusual occasions, it may occur with other tumors [1, 2]. The incidence and implications of multiple tumors remain relatively unknown. It is extremely rare that HNSCC occurs with salivary gland tumor(s) [1, 3, 4]. Warthin’s tumor is the second most common benign salivary gland tumors more common in males with a mean age between the fifth and seventh decades; besides, it is closely related to smoking [5, 6]. Warthin’s tumors are common in the parotid gland, but in a few cases, they may also occur in “extra-parotid” sites, such as cervical lymph nodes or other salivary gland tissues [7]. In addition, lesions can be seen in unilateral, bilateral or multifocal lesions with a higher frequency than other benign salivary gland lesions [5].
Some reports have presented “extra-parotid” Warthin’s tumor lesions in lymph nodes and soft tissue which are often mistaken as metastatic tumors [5]. Here, we report a case of Warthin’s tumor of submandibular gland unexpectedly detected in postoperative neck dissection specimen in a patient suffered from carcinoma of floor of mouth. Until now, only a few cases with the same combination of histology have been reported [1, 3, 4].
Case Report
A 65-year-old Chinese male was referred to the Department of Oral and Maxillofacial Surgery with a 6-month history of ulceration on the right floor of the mouth with no pain and other symptoms. There was no contributory past medical history besides a 30-year smoking history. On intraoral examination, an irregular ulcerating mass measuring 30 × 15 mm was found on the right floor of mouth with the anterior front encroaching on the contralateral region (Fig. 1). There was no sign of metastases in the regional lymph nodes or any other organs. The biopsy was performed under local anesthesia, and the pathological examination confirmed clearly the lesion was squamous cell carcinoma (Fig. 2).
Fig. 1.

An examination of the mouth revealed an irregular ulcer measuring 30 × 15 mm on the right floor of mouth with the anterior front encroaching on the contralateral region
Fig. 2.
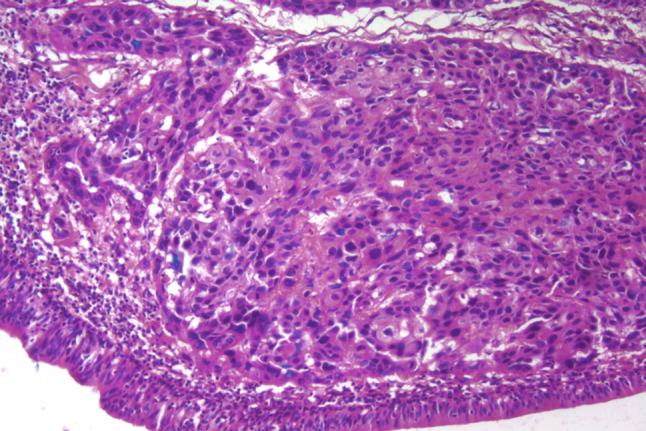
The preoperative pathological examination confirmed clearly the lesion was squamous cell carcinoma (H&E stain; original magnification × 200)
One week later, extensive primary tumor resection and radical neck dissection (I–II–III–IV–V levels in right side and I–II–III levels in left side) were undertaken under general anesthesia. Postoperative macroscopic examination found two indurating nodules measuring 0.6 cm in diameter within the right submandibular gland which the pathologist first thought they were just metastasis foci. Unexpectedly, microscopic examination showed these were Warthin’s tumors (Fig. 3). Pathological microscopic examination also showed one lymph node metastasis on the right submandibular region (Fig. 4). Radiotherapy to the oral floor and the neck was performed 2 weeks. There was no evidence of recurrence of the two types of tumors or carcinoma metastasis after 3-year follow-up.
Fig. 3.
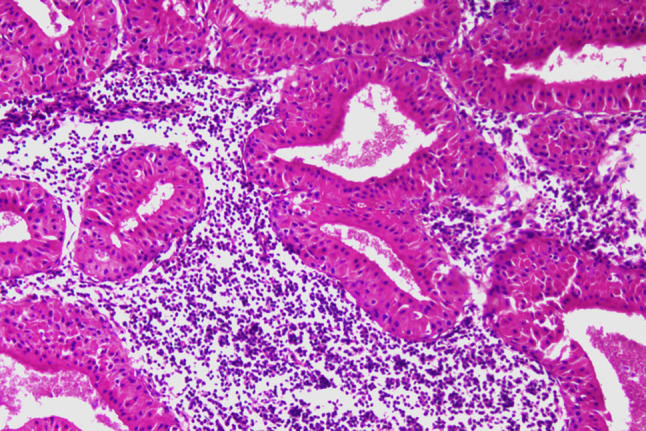
Postoperative microscopic findings detected Warthin’s tumor in the submandibular gland showing double-layered epithelium with tall columnar, eosinophilic and granular epithelial cells lining cystic cavities and forming papillary projections (H&E stain; original magnification × 200)
Fig. 4.
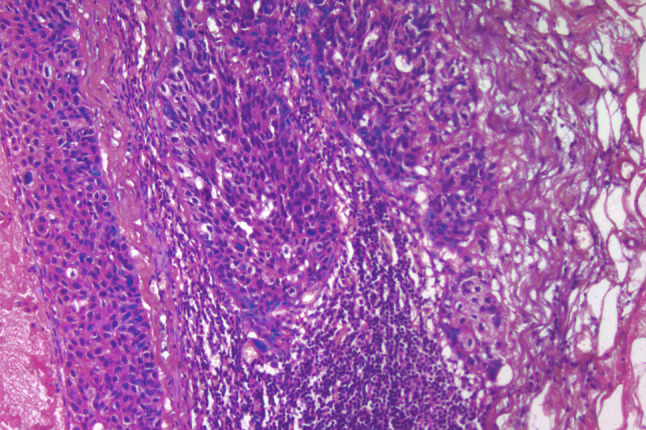
A lymph node metastasis in the right submandibular region (H&E stain; original magnification × 200)
Discussion
The risk of multiple primary tumors (MPTs) in the head and neck area is higher than that in other areas of the body [1]. In recent years, the reports of MPTs increased. This may be due to improved patient survival of primary tumors, as well as an increased recognition of multiple primary tumors by clinicians. However, oral squamous cell carcinoma simultaneously with Warthin’s tumor in the submandibular gland is extremely rare [1, 3, 4].
It is reported that “extra-parotid” Warthin’s tumor occurs in 2.7–12% of cases with the neck and surrounding parotid gland being the most common tumors can also be found in the oral cavity, oropharynx and larynx [8–10]. Histologically, the envelope of Warthin’s tumor is complete and consists of eosinophilic cells and lymphoid stroma. Embryonic development of the parotid gland may explain the causes of the “extra-parotid” disease. The parotid gland encapsulates late in embryonic development; therefore, the components of the salivary glands may be mixed with the developing lymphoid tissues inside or outside the parotid gland. These heterotopically salivary components are thought to be the origin of “extra-parotid” Warthin’s tumor [10], and immunohistochemical study of the epithelial and mesenchymal components of Warthin’s tumor confirmed the hypothesis that it originated from regional lymph nodes [9]. However, some authors suggest that they may also develop from branchial cleft remnants, especially in the larynx [8].
Squamous cell carcinoma (SCC) is the most common malignant neoplasm of the oral cavity. In rare cases, it can occur with other benign or malignant tumors simultaneously [1]. Floor of mouth is one site which SCC involves frequently with a high incidence of regional lymphatic metastasis, especially to the submandibular region. Lymphatic metastasis is one of the most important factors influencing the prognosis and choice of treatment. On occasion, lymphatic node enlargement may be due to inflammation or the second primary tumor rather than metastasis [9]. So, a decision whether or not to treat the lymph nodes of the neck is of utmost importance.
In this patient, one lymphatic node enlargement microscopically proved to be carcinoma metastasis, whereas the other two nodes be multicentric Warthin’s tumors. Until now, only a few cases with the same combination of histology have been reported previously. Sheahan reviewed 274 SCC patients who underwent neck dissection and found one patient had a benign Warthin’s tumor within a lymph node close to the submandibular gland [2].
It is difficult to explain the simultaneous occurrence of carcinoma of the floor of mouth and Warthin’s tumor. Some researchers proposed that the development of MPTs be linked to etiologic factors such as smoking, alcohol consumption, heredity and occupational exposure. Our patient had a 30-year smoking history, which might be a co-etiological factor for the tumors in the patient.
For oral surgeons, the diagnosis of “extra-parotid” Warthin’s tumor remains a challenge. This case prompts clinical surgeons of the need to include this condition in the differential diagnosis of suspected metastatic upper cervical lymphadenopathy.
Conclusion
This case serves as a reminder to oral surgeons that in the case of head and neck tumors, enlarged lymph nodes may be caused by inflammation or secondary primary focus rather than lymph node metastasis. Recognition and implication of the unexpected pathologic findings in patients with head and neck cancer are thus worth studying. Failure to recognize and treat an unexpected pathology may have adverse effects on the outcome. Furthermore, unexpected pathology may masquerade as metastases from the original SCC. For these reasons, the potential for unexpected pathology during neck dissection should be always borne in mind by the pathologist and oral surgeon alike.
Acknowledgments
We are grateful to the patient who contributed to this study.
Funding
The authors declare no funding from institution or commercial company with regard to this case report.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sheahan P, Hafidh M, Toner M, Timon C. Unexpected findings in neck dissection for squamous cell carcinoma: incidence and implications. Head Neck. 2005;27:28–35. doi: 10.1002/hed.20110. [DOI] [PubMed] [Google Scholar]
- 2.Meikle D, Yarington CT. Synchronous parotid tumors of different histiological types in association with metastasizing hypopharyngeal carcinoma. J Laryngol Otol. 1985;99:1261–1267. doi: 10.1017/S0022215100098509. [DOI] [PubMed] [Google Scholar]
- 3.Maiorano E, Muzio LL, Favia G, Piattelli A. Warthin’s tumour: a study of 78 cases with emphasis on bilaterality, multifocality and association with other malignancies. Oral Oncol. 2002;38:35–40. doi: 10.1016/S1368-8375(01)00019-7. [DOI] [PubMed] [Google Scholar]
- 4.Sato T, Ishibashi K. Multicentric Warthin tumor of the paraparotid region mimicking lymph node metastases of homolateral oral and oropharyngeal squamous cell carcinoma: reports of two cases. J Oral Maxillofac Surg. 1998;56:75–80. doi: 10.1016/S0278-2391(98)90920-X. [DOI] [PubMed] [Google Scholar]
- 5.Eveson JW, Cawson RA. Salivary gland tumours. A review of 2410 cases with particular reference to histological types, site, age and sex distribution. J Pathol. 1985;146:51–58. doi: 10.1002/path.1711460106. [DOI] [PubMed] [Google Scholar]
- 6.Orabona GDA, Abbate V, Piombino P. Warthin’s tumour: aetiopathogenesis dilemma, ten years of our experience. J Craniomaxillofac Surg. 2015;43:427–431. doi: 10.1016/j.jcms.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Yoo GH, Eisele DW, Driben JS, Driben JS. Johns ME (1994) Warthin’s tumor: a 40-year experience at the johns hopkins hospital. Laryngoscope. 1994;104:799–803. doi: 10.1288/00005537-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 8.van der Wal JE, Davids JJ, van der Waal I. Extraparotid Warthin’s tumours-report of 10 cases. Br J Oral Maxillofac Surg. 1993;31:43–44. doi: 10.1016/0266-4356(93)90098-H. [DOI] [PubMed] [Google Scholar]
- 9.Demir Y, Aktepe F, Yílmaz MD, Altuntaş A. Warthin’s tumor of the cervical lymph node: an incidental finding. Ann Plast Surg. 2002;48:110–111. doi: 10.1097/00000637-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Fantozzi RD, Bone RC, Fox R. Extraglandular Warthin’s tumors. Laryngoscope. 1985;95:682–688. doi: 10.1288/00005537-198506000-00010. [DOI] [PubMed] [Google Scholar]


