Introduction
Radical neck dissection (RND) was initially described by Crile in 1906 and was shown to improve the outcomes of neck metastasis treatment. The modified RND (MRND) is functional neck dissection method that preserves the internal jugular vein (IJV) and/or accessory nerve and/or sternocleidomastoid muscle (SCM), allowing improved function. The principal advantages of MRND incision are the provision of adequate surgical access, the good healing potential, and the production of an acceptable cosmetic result. An ideal skin incision for MRND should maintain adequate skin viability, provide coverage of the carotid artery to lessen the risk of rupture, provide adequate exposure for the procedure, produce good cosmetic results, and allow the transfer of appropriate flaps to the head and neck region for reconstruction [1].
The Y incision introduced by Ward in 1950 can provide adequate surgical access, but the vertical incision does not match the neck wrinkle line, producing an ugly scar (Fig. 1a). The modified MacFee double-incision pattern using separate horizontal lines on the upper and lower neck was proposed to avoid the use of three-point suture line junctions that may compromise healing in important areas of the irradiated neck. The lower incision scar eventually lies below the collar line in most patients. Therefore, the MacFee incision creates a balance between cosmesis and exposure [2–5]. This technical note proposes a modified MacFee double-incision pattern to produce more aesthetic results following MRND to treat oral cancer.
Fig. 1.
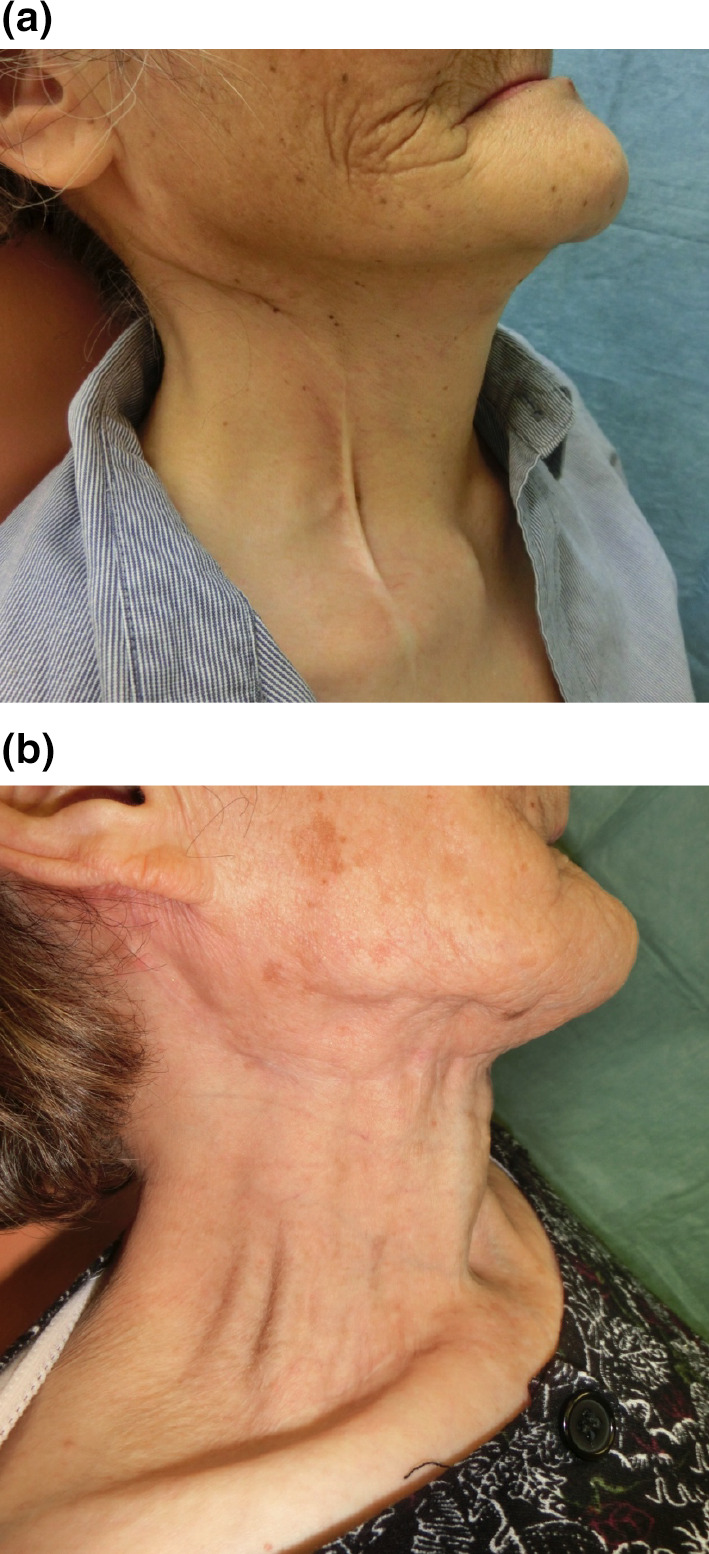
Comparison of a wound with radical neck dissection. a The scar from a Y incision. b The scar after a modified MacFee incision
Surgical Technique
The upper incision of the conventional MacFee incision begins approximately 25 mm below and 25 mm behind the tip of the mastoid process. It is formed downward and anteriorly, about 25 mm below the angle of the mandible, and then forward along a line approximately parallel to the lower margin of the mandible. The incision crosses the midline at the level of the hyoid bone and ends on the opposite side of the neck, approximately at the point where the intermediate tendon of the digastric muscle passes over the hyoid bone. The lower incision is made approximately 35 mm above and parallel to the clavicle. Anteriorly, the incision extends over the medial border of the sternocleidomastoid muscle; posteriorly, it ends about 25 mm beyond the anterior margin of the trapezius muscle (Fig. 2, Red line) [5].
Fig. 2.
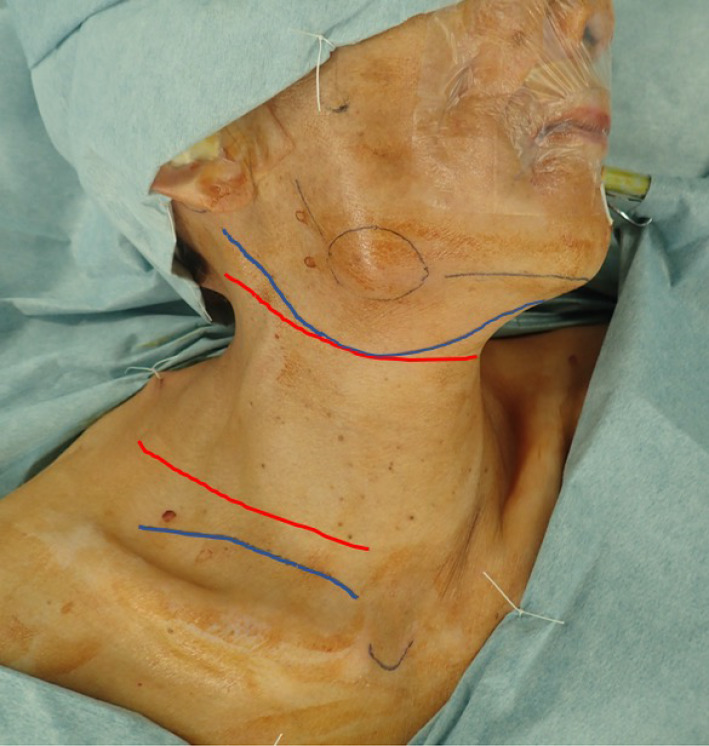
The modified MacFee incision (blue line). The upper incision run connects the mastoid process, approximately 25 mm below mandibular notch of lower margin to the midline of mandible. The lower incision is made approximately 15 mm above the clavicle. The conventional MacFee incision (Red line)
We modified the upper incision to connect the mastoid process approximately 25 mm below mandibular notch of lower margin to the midline of mandible. In this method, the incision does not cross the level of hyoid bone and runs above the hyoid bone to the submental space to hide the incision by the mandible and more aesthetic than conventional MacFee incision. The lower curved incision is made approximately 15 mm above the clavicle, allowing the scar to be hidden more than conventional MacFee incision with clothing. These changes improve the wound esthetic compared with the conventional MacFee incision (Figs. 1b, 2 Blue line).
Skin Incision and Elevation of Subplatysmal Flaps
The skin incision is completed through the platysma with a No. 10 scalpel. The subplatysmal flaps are elevated in a subplatysmal plane above the superficial layer of the deep cervical facia with a scalpel or thermal scalpel system (Hemostatix Medical Technologies, LLC, Memphis, TN, USA). As the platysma muscle terminates anteriorly and posteriorly, the dissection is completed in a subcutaneous plane. In the posterior area, the external jugular vein, great auricular nerve, and SCM serve as excellent guides to maintain this dissection at the appropriate level because the dissection should be superficial to it. Good traction is created by keeping the flaps under good tension perpendicular to the neck to aid in their elevation. The lower incision is made approximately 15 mm above the clavicle, and the flap is elevated in a subplatysmal plane above the superficial layer of the deep cervical facia. A tunnel should be made by elevating the flap between upper and lower and anterior and posterior areas to allow good access (Fig. 3a, b). This lower incision has better access to level IV and V than single upper incision, especially for long-neck patients.
Fig. 3.
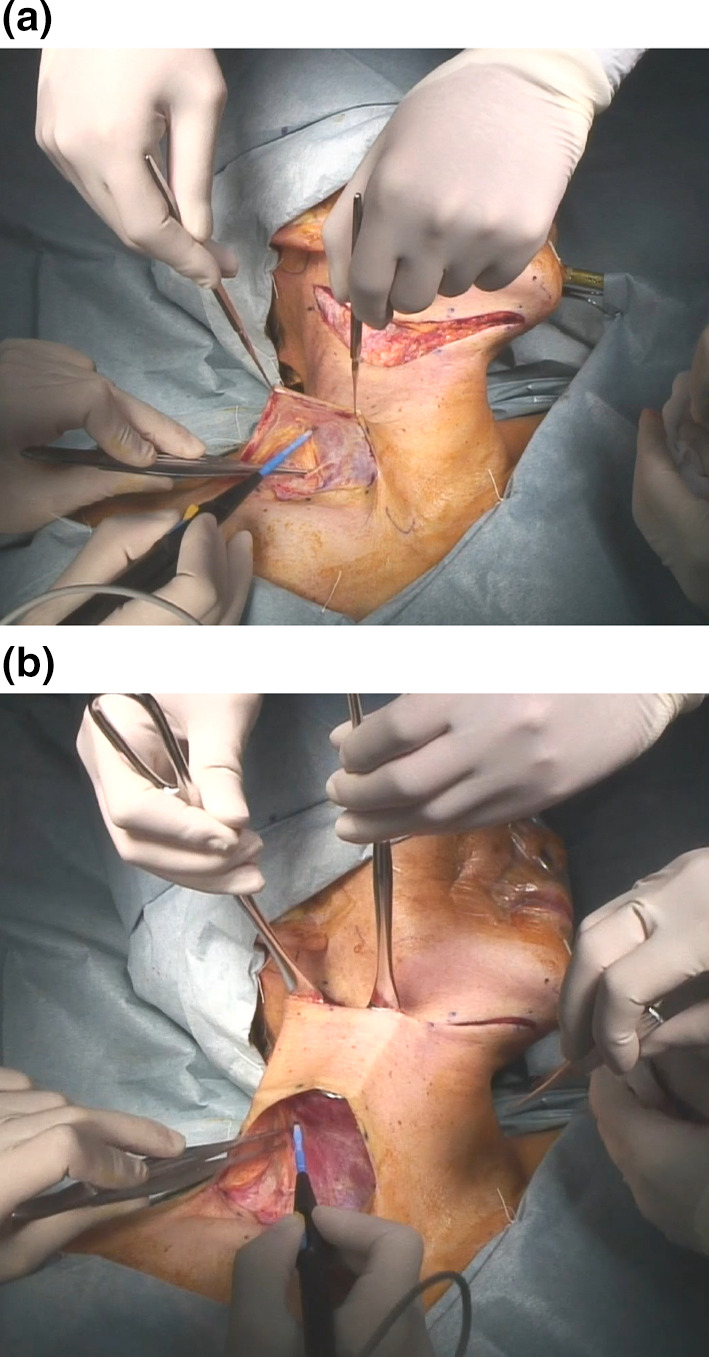
a The flap elevated from the supraclavicle region with a subplatysmal plane above the superficial layer of the deep cervical fascia. b A tunnel should be made by elevating the flap between the upper and lower and anterior and posterior regions to allow good access
Approach from the Supraclavicle Region
The SCM is resected with monopolarcautery at the sternal and clavicular head (Fig. 4a). The carotid artery and vagus nerve are identified in front of the IJV(Fig. 4b). The lower resection area is 10 mm above the clavicle, which is the inferior border of the dissection.
Fig. 4.

a Resection of SCM with the sternal and clavicular head b Vagus nerve and IJV from inferior part. c Lateral approach with a No. 15 blade from superior part of IJV
Approach from the Submandible Region
The superior approach is possible after the supraclavicular approach has undergone about 1/4–1/3 resection. The superior border is the mandibular lower border and the line connecting the mandibular angle and mastoid process. The inferior part of the parotid gland is ligated and dissection done after separating the marginal mandibular branch of the facial nerve. The SCM is resected at the mastoid process. The posterior belly of the digastric muscle appears and this muscle is retracted upward so the superior part of IJV is visible.
Lateral Approach
After the approach from supraclavicle and submandible, deep cervical fascia overlying the splenius capitus, levator scapulae, and scalene muscles should be preserved from the posterior limit of the dissection. No. 15 blade dissection combined with good traction on the specimen and countertraction on the IJV is helpful here (Fig. 4c) [6]. The common carotid artery and vagus nerve are separated from the specimen. The phrenic nerve, superior thyroid artery, and hypoglossal nerve is identified and preserved. Finally, the duct of submandibular gland is ligated and the transected attachments of lingual nerve, which allows the specimen to be delivered.
Before closure, the wound should be well irrigated with saline. The bleeding and lymph drainage should be checked (Fig. 5a,b). Two continuous suction drains are inserted anteriorly and posteriorly into the neck and fixed with 2-0 silk. A two-layer closure is employed using 3-0 vicryl for the approximation of the platysma muscle and subcutaneous tissue and 5-0 black nylon for the skin (Fig. 5c).
Fig. 5.

Completion of dissection: a Inferior part from the supraclavicular view, b Superior part from the submandibular view, and c Wound closure with two suction drains
Surgical Results
The 101 patients were treated with modified MacFee incision from 2009 to 2019 in our hospital. Although all patients were satisfied with wound, two patients had delay of wound healing. One patient was post irradiated 70 Gy, and another had diabetes mellitus (HbA1c 7.1%). The significant advantage of modified MacFee incision is more aesthetic than Y and MacFee incision. The incision runs above the hyoid bone to the submental space to hide the incision by the mandible and more esthetic than conventional MacFee incision. The lower incision is made approximately 15 mm above the clavicle, allowing the scar to be hidden more than conventional MacFee incision with clothing. The disadvantage of this incision is the slight difficulty in surgically accessing the middle neck region. But the dissection area is same to Y incision and possible with combination approach from the supraclavicle and submandible.
Conclusion
The advantage of modified MacFee incision is more aesthetic than Y and MacFee incision. Accessibility is almost same to conventional incision with combination of the supraclavicle and submandible approach.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.White K, Mosdell DM, Morris D. MacFee incision: a safe approach to the neck. South Med J. 1993;86:871–874. doi: 10.1097/00007611-199308000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Shaw HJ. A modification of the MacFee incisions for neck dissection. J Laryngol Otol. 1988;102:1124–1126. doi: 10.1017/S0022215100107509. [DOI] [PubMed] [Google Scholar]
- 3.Roy S, Shetty V, Sherigar V, Hegde P, Prasad R. Evaluation of four incisions used for radical neck dissection—a comparative study. Asian Pac J Cancer Prev. 2019;20:575–580. doi: 10.31557/APJCP.2019.20.2.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kudva A, Hemavathi U, Patil BR. Modification of MacFee incision: a balance between cosmesis and accessibility. J Maxillofac Oral Surg. 2014;13:349–350. doi: 10.1007/s12663-013-0530-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacFee WF. Transverse incisions for neck dissection. Ann Surg. 1960;151:79–284. doi: 10.1097/00000658-196002000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmes JD. Neck dissection: nomenclature, classification, and technique. Oral Maxillofac Surg Clin North Am. 2008;20:459–475. doi: 10.1016/j.coms.2008.02.005. [DOI] [PubMed] [Google Scholar]


