Abstract
Clinical genomic testing, analysis of your entire genetic material for healthcare purposes, is a complex topic for various medical specialities. Although Australia is a multicultural society, most genomic resources are produced in English which can make understanding challenging for people from culturally and linguistically diverse (CALD) backgrounds. A mixed methods approach explored the views of healthcare interpreters and people from CALD backgrounds to identify knowledge gaps and inform the provision of more equitable services. Eighteen healthcare interpreters completed a survey from two public hospitals in Melbourne. Descriptive data analysis informed the four pilot interviews with individuals from CALD backgrounds identified through online advertisements. Interpreters revealed variable satisfaction with patient understanding of genomic concepts and suggested that basic training and resources on genomics would help facilitate interpretation. Three themes arose from the pilot interviews: (1) cultural factors; (2) perceptions of genomics; and (3) language barriers and complex terminology. Resources that consider cultural differences and language barriers will help to ensure people from CALD backgrounds are adequately informed about genomic testing. The pilot interviews will inform future in-depth studies of the views of people from the CALD community.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12687-021-00537-0.
Keywords: Clinical genomics, CALD, Healthcare interpreter, Genomic resources, Genomic testing
Introduction
Australia is a multicultural society, with over a quarter of the population born overseas and one-fifth speaking a language other than English at home (Australian Bureau of Statistics 2017). Whilst there are more than 300 different languages spoken in Australia (Australian Bureau of Statistics 2017), the Australian healthcare system predominately caters for English-speaking patients (Phillips 2010). Consequently, a large proportion of the population may face challenges in comprehending health information at the level required for them to engage with health services (Walker 2005). Although individuals from culturally and linguistically diverse (CALD) backgrounds are collectively defined as individuals who were born overseas from a country where English is not the main language spoken, it is important to recognise that this population is not homogeneous and health needs will vary among individuals. The CALD community globally experiences poorer health outcomes (Henderson et al. 2011), including twice the number of hospital admissions for chronic and disabling conditions (Gorman et al. 2003). Despite the high prevalence of health-related issues, individuals from CALD backgrounds are less likely to follow healthcare plans (Gregg and Saha 2007) or access appropriate health services (Comino et al. 2001). This may be due to language barriers (Walker 2005), inadequate cultural understanding and sensitivity of health services and providers (Comino et al. 2001; Cyril et al. 2016; Rao et al. 2006) and a lack of access to appropriate resources (Greenstock 2012; Levy et al. 2011). It is therefore necessary that thoughtful approaches are taken to better understand the health needs of individuals from CALD backgrounds.
Genomic testing, the process of analysing a person’s entire set of genetic material (Roth 2019), is increasingly being implemented into routine healthcare. Despite this, patients from CALD backgrounds are still poorly represented in genetic services (Allford et al. 2014; Armstrong et al. 2005). Research indicates that individuals from CALD backgrounds have a limited understanding of genomics, further compounded by the use of technical language (Cruz-Correa et al. 2017; Lea et al. 2011; Shaw and Hurst 2008). Additionally, concern has been raised over the amount of genomic information available in English compared to other languages, which may prevent CALD communities from providing informed consent to clinical testing or participating in genomic research (Baty et al. 2003; Saleh et al. 2009). It is therefore crucial to address the current disparities of patients from CALD backgrounds in accessing genetic services and understanding genomic information to avoid health inequities in the provision of patient care.
Healthcare interpreters play a vital role in clinical communication between patients and healthcare providers, as they can convey genomic information in a culturally sensitive manner to help improve the quality of patient care (Flores 2005; Gutierrez et al. 2019). However, healthcare interpreters themselves have reported having a limited understanding of basic genomic concepts, with some feeling overwhelmed by the nature and the amount of genomic information that has to be communicated to the patient (Lara-Otero et al. 2018). This can have a profound impact on patient care, as omissions and misinterpretations are more likely to occur when health providers deliver a large amount of information containing technical language (Gutierrez et al. 2017). The result is that the patient may be presented with misleading statements or statements missing crucial clinical information (Simon et al. 2006). Despite the pivotal role of healthcare interpreters in cross-cultural communication between patient and provider, the voice of healthcare interpreters and their role in communicating genomics remains largely absent from the literature.
The National Health Genomics Policy Framework (Australian Health Ministers’ Advisory Council 2017) identified the need for genomic awareness, education and targeted resources for CALD communities. Although the policy framework recognised the development of educational resources for these communities as a national priority, the majority of genomic resources available have been developed for healthcare providers (Slade 2016; Talwar et al. 2017). Patient-targeted resources are varied in content and quality, with information presented mostly in English or requiring navigation through English text (Graves et al. 2020). Targeted genomic testing resources are yet to be developed for the CALD community in Australia, and it is imperative that these communities have a strong voice in the development phase, to ensure that the resource helps improve genomic literacy levels and is culturally sensitive. This study forms part of the Genomics in the Community initiative led by the Australian Genomics Health Alliance, aimed at collating and developing resources to help individuals understand genomics and genomic testing. The aim of this paper is to explore the experiences of interpreters and individuals from CALD backgrounds in understanding genomics and the implications of genomic testing, to then inform the development of culturally appropriate genomic testing resources.
Methods
Participants and recruitment
Survey
The language service departments of four major public hospitals in Melbourne were contacted via email and provided with information about the study. Interested parties were invited to contact the research team directly. The survey study population was purposively sampled and included individuals over 18 years of age and currently employed by a public hospital in Melbourne to provide interpreter services.
Interviews
An online advertisement was posted on the Facebook pages of three multicultural support services, asking interested parties to contact the research team directly. Additionally, an invitation letter was posted by the Australian Genomics Genetic Counsellor to twenty-two patients from CALD backgrounds, who had been involved in a previous research study and had agreed to be contacted about future research opportunities. The interview population was purposively sampled and included individuals over 18 years of age who were born overseas from a country where English is not the main language spoken.
Data collection
Survey
Categorical survey data were collected and managed using REDCap, an electronic data capture tool (Harris et al. 2009, 2019). The survey was reviewed by two interpreter coordinators to check for accuracy and appropriateness and was piloted by the research team. Hard copy surveys and the online link were given to two interpreter coordinators for distribution to staff members.
Interviews
All interviews were audio recorded, with participant consent, and transcribed verbatim with identifiers removed. The transcripts were stored on a secure server and data were organised using QSR International’s NVivo 12 software (2018). All interviews were conducted in English.
Measures
Survey
A 13-question survey consisted of closed and open-ended questions and was developed by the research team to examine the perceptions of healthcare interpreters on the challenges patients face in understanding genomic information and the implications from them, as well as suggestions for improvement (see Supplementary Report 1). More specifically, the survey asked about their demographic characteristics, the utility of genomic resources, satisfaction with patient understanding and suggestions to help improve interpretation of genomics.
Interviews
Semi-structured, in-depth interviews were designed to examine the understanding of genomic testing for individuals from CALD backgrounds and to inform the development of genomic testing resources for these communities. The interview schedule was directly informed by the survey results, and probing questions were used to help guide the conversation (see Supplementary Report 2). A modified version of a critical analysis framework previously developed as part of the larger study, based on established tools and input from experts in the field (Lewit-Mendes et al. 2018; Shoemaker et al. 2014), was incorporated. This framework was utilised to assess the 1, content; 2, language and readability; 3, structure and organisation; and 4, design and decision-making of selected resources. Resources selected for discussion at interviews included one plain language resource and two genomic testing resources (see Supplementary Report 3).
Analysis
Survey
The data were cleaned and analysed using Stata 15 (StataCorp 2017). Categorical variables, including demographic information, were summarised as percentages. The focus of the survey was to inform the development of the interview schedule; therefore, power and sample size calculations were not appropriate.
Interviews
An inductive approach was used to thematically analyse the transcripts, to allow for flexibility and the possibility of generating unanticipated insights from the data (Braun and Clarke 2006). Themes were identified and discussed by the research team through a comparative iterative process as the interviews progressed. Two transcripts were independently coded by two members of the research team (EU and SB) to refine the coding scheme, and EU completed the final two transcripts. Regular discussions were held by the research team to consider any areas of disagreement and allow a consensus to be achieved. Once key themes were identified, quotations that embodied or clarified a key finding were selected.
Results
Survey
Participant demographics
Of the 34 interpreters who were approached, 18 interpreters completed the survey (53%). Descriptive statistics are summarised in Table 1. The sample was predominately female (N = 11, 61%), aged between 55 and 64 years old (N = 6, 33%), with 1–5 years of experience as an interpreter (N = 7, 39%). Seven different languages were interpreted: Arabic (N = 3, 15%), Cantonese (N = 3, 15%), Greek (N = 3, 15%), Italian (N = 6, 30%), Mandarin (N = 3, 15%), Persian (N = 1, 5%) and Vietnamese (N = 1, 5%) with three participants interpreting more than one language.
Table 1.
Survey participant characteristics
| ID | Gender | Age group | Languages interpreted | Years of experience as an interpreter |
| 1 | F | 45–54 | Italian | 11–19 |
| 2 | M | 55–64 | Arabic | 11–19 |
| 3 | F | 35–44 | Vietnamese | 1–5 |
| 4 | F | 65 or older | Italian | 20 + |
| 5 | F | 35–44 | Italian | 1–5 |
| 6 | F | 45–54 | Not specified | 1–5 |
| 7 | F | 25–34 | Mandarin and Cantonese | 1–5 |
| 8 | M | 55–64 | Arabic | 6–10 |
| 9 | F | 45–54 | Mandarin and Cantonese | 6–10 |
| 10 | F | 35–44 | Italian | 1–5 |
| 11 | M | 55–64 | Greek | 1–5 |
| 12 | F | 45–54 | Greek | 11–19 |
| 13 | M | 55–64 | Mandarin and Cantonese | 6–10 |
| 14 | M | 35–44 | Persian | < 1 |
| 15 | M | 55–64 | Italian | 11–19 |
| 16 | F | 65 or older | Italian | 20 + |
| 17 | F | 55–64 | Greek | 20 + |
| 18 | M | 25–34 | Arabic | 1–5 |
Interpreters’ satisfaction with patients’ understanding of genomics
The majority of participants felt very satisfied or somewhat satisfied with patient understanding of genomics (N = 8, 61%); however, there was still a large minority who felt neutral (N = 4, 31%). In the free text, participants noted the essential role of clinicians in ensuring patient understanding of genomics with one participant identifying that the clinician can also negatively influence patient understanding if complicated terminology is used (see Supplementary Report 4). The notion of complicated terminology was commonly discussed as a barrier for patient understanding (N = 4, 31%).
Improving interpretation of genomic information to patients
The majority of participants encountered genomic information between once a month to once every 6 months (N = 13/17, 72%) with genomic testing options being the most common information interpreted (N = 6/18, 33%). Participants’ suggestions to help improve interpreter understanding to assist in the correct interpretation of genomics included having access to genomic resources and basic training in genomics (see Supplementary Report 5).
Interviews
Participant demographics
A total of 4 individuals participated in an interview. Descriptive statistics are summarised in Table 2. Although the most common language interpreted by the healthcare interpreters was Italian, we did not receive any interest from individuals with an Italian background to participate in an interview. Interviews were conducted in person and lasted between 30–50 min. There was an even number of male (N = 2, 50%) and female (N = 2, 50%) participants. The majority were aged between 35 and 44 years old (N = 3, 75%), had been living in Australia for 1–5 years (N = 3, 75%) and had a bachelor’s degree (N = 3, 75%). First languages spoken were Arabic, Armenian, Tamil and Persian.
Table 2.
Interview participant characteristics
| ID | Gender | Age group | First language | Country of birth | Years living in Australia | Highest level of education |
|---|---|---|---|---|---|---|
| 1 | M | 25–34 | Persian | Iran | 1–5 | Bachelor degree |
| 2 | M | 35–44 | Arabic | Syria | 1–5 | High school degree or equivalent |
| 3 | F | 35–44 | Tamil Sinhalese (3rd language) | Sri Lanka | 1–5 | Postgraduate degree |
| 4 | F | 35–44 | Armenian | Iran | 20 + | Bachelor degree |
Interview themes
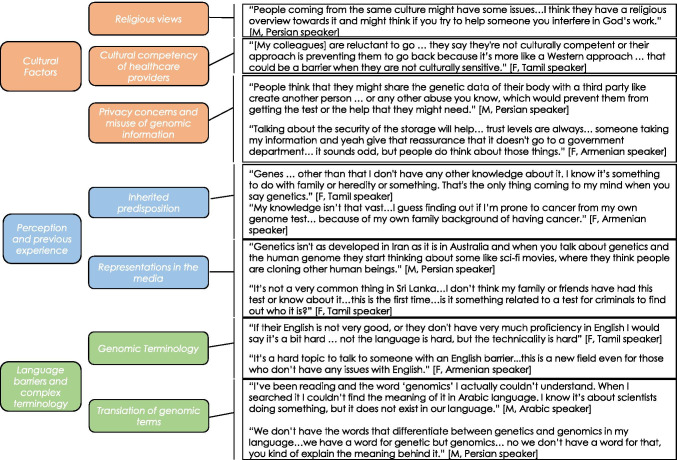
Three themes were identified that influenced participants’ understanding of genomic testing, as illustrated in Fig. 1.
Fig. 1.
Themes and subthemes identified from interviews with people from CALD backgrounds, with exemplar quotes
Theme 1: cultural factors
All participants discussed the influence of their cultures on understanding genomic testing, which encompassed religious views, privacy concerns and the cultural competency of health services and professionals. Religious views could impact how individuals perceived genomic testing, its utility and whether individuals accessed genetic services. Another factor discussed that could influence understanding of genomic testing was the ‘Western’ approach to presenting health information, which could negatively impact CALD community participation in genetic services. Key barriers identified were the mistrust of authorities, privacy concerns and fear of misuse of their genomic information that could result in individuals from their culture being reluctant to have genomic testing. Cultural concerns were raised regarding the storage and usage of samples and personal genomic information. Conversely, some participants were content to go ahead with genomic testing based on the doctor’s recommendation and the ability to benefit research.
Theme 2: perception and previous experience
Participants had a limited understanding of genomic testing and its implications. The majority of participants had no prior experience with genomics and their awareness was focused around heredity. Participants’ perception of genomic testing and its implications were often shaped by representations in the media.
Theme 3: language barriers and complex terminology
All participants believed that the most challenging aspect of comprehending genomic health information was the terminology used. Participants referred to genomic terms as confusing, foreign and not very clear in their explanation. Participants also stated the importance of using a dictionary or the Internet to help overcome language barriers; however, participants struggled to locate a translation in their own language for terms such as ‘genomics’ or ‘genome’.
Developing culturally sensitive resources
A number of suggestions for the development of culturally sensitive resources were generated from the survey and interview data and are summarised in Table 3.
Table 3.
Resource considerations
| Cultural considerations | |
| • To ensure the resource is culturally sensitive, co-develop the resource in discussion with target communities, translation experts and genetic professionals | |
| • Consider translated or bilingual material | |
| • Personalise the information so that it is of cultural relevance to the target population | |
| • Ensure graphics used are representative of diverse populations | |
| Resource considerations | |
| • Provide adequate information on the benefits, risks and outcomes of genomic testing as well as implications for family members | |
| • Provide explanations of genomic concepts and be consistent in language used | |
| • Consider a format that can be easily printed and taken to and from a consultation such as a booklet | |
| • Keep technical detail to a minimum | |
| • Use of organisational logo |
Discussion
The major barriers for understanding genomic health information included cultural differences, limited genomic literacy unless previously exposed to genetics and a lack of linguistic equivalent of new terminology in other languages. This study also identified practical considerations for the development of a genomic testing resource, including the importance of detailed explanations of concepts and using appropriate terminology whilst ensuring cultural relevance to the target population.
This study highlights that cultural beliefs can deeply influence understanding of genomic testing, particularly in the absence of a biological understanding of genetic disease. In Australia, genomic information is usually presented from a Western perspective, and the effects of religion and spirituality on how individuals understand their health are not always respected. The interviews identified that the term ‘genetics’ is often synonymous with genetic manipulation which can be considered unnatural and interfering with what God intended, negatively impacting understanding of genomic testing. This perception has been cited elsewhere in the literature as a key concern regarding the utility of genomic technologies in non-Western communities (Catz et al. 2005). These interviews indicate that a lack of cultural competency can prevent individuals from CALD backgrounds seeking information about genomic testing and services. To provide an inclusive service, healthcare professionals need to respond to these needs and consider the role that religion and spiritualty may have on disease causality and perceptions of health.
Trust issues relating to privacy of genetic information featured highly in the interviews, suggesting some level of genomic literacy. As established in the literature, historical malpractice has fostered mistrust by the CALD community with healthcare providers and research (Baty et al. 2003; Catz et al. 2005; George et al. 2014). The use, and possible storage, of human tissue often required for genomic testing can be considered a culturally significant activity; therefore, there is a level of trust that has to be given to researchers and clinicians during this process (Hudson et al. 2016). Whilst some participants in this study would not hesitate to undergo genomic testing if recommended by a health professional, other participants were more cautious and discussed how trust issues may create a negative attitude towards genomic testing. Therefore, steps need to be taken to help build trust and address any misconceptions of genomics within these communities.
Cultural differences in family structures may influence understanding of genomic testing and its implications. Study participants indicated knowledge of genomics in the context of heredity and family, consistent with published findings (Condit 2010; Molster et al. 2009; Sandberg et al. 2017). Additionally, some healthcare interpreters discussed the role of cultural differences regarding consent influencing understanding of genomics. Previous literature has outlined how differing family structures and kinship systems can influence understanding of genetic health, and decisions surrounding consent and testing may involve the input of other family members (Saleh et al. 2009; Zhong et al. 2018). Therefore, the model of client autonomy utilised in genetic services may not be an appropriate approach in some cultures (Saleh et al. 2009). It is important that these family nuances are understood when offering genomic testing in a clinical setting, as testing can impose implications extending beyond the individual.
This study identified low awareness and understanding of genomics and implications of genomic testing by the majority of interview participants. Low genomic literacy is not specific to members of the CALD community, and low literacy levels among the general public have been widely reported elsewhere in the literature (Allford et al. 2014; Catz et al. 2005; Condit 2010; Molster et al. 2009). Additionally, the role of the media in shaping perceptions of genomics was acknowledged. These findings compare to previous studies, tracing low genomic literacy to weaknesses in representations of genetics in the media and on the Internet (Dougherty et al. 2014; Lea et al. 2011). Furthermore, the illusion of perceived knowledge due to the media may be problematic if it creates a false sense of reassurance and prevents individuals from seeking information from health professionals (Haga et al. 2013). Therefore, educating the CALD community and the wider public on genomic testing and its implications is essential, particularly because of the predictive nature of genomic information and the possibility of variants of uncertain significance and incidental findings from genomic testing (Samuel et al. 2017).
Whilst genomic literacy has been observed to be low among all populations, this study demonstrates that CALD communities face the additional challenge of language barriers. Participants struggled to identify a translation for certain genomic terms, creating further confusion about the topic. Healthcare interpreters also discussed the impact of complex terminology on interpreter and patient understanding, advocating for resources to assist them. Whilst it is perhaps unsurprising that recently developed technical terms such as ‘genomics’ may not have a linguistic equivalent in languages other than English, this finding suggests that a potential language gap exists between genetic professionals and patients, which could influence an individual’s comprehension of genomic testing and the potential outcomes. Moreover, previous research suggests that patients are unlikely to ask a healthcare professional or interpreter for an explanation of medical terminology to clarify understanding (Watermeyer et al. 2020).
The healthcare interpreters who participated in this study indicated that training on basic genetic concepts could assist in their ability to interpret more effectively as the majority only encountered genomic information once every 1 to 6 months. Previous studies have discussed this challenge (Komaric 2012; Krieger et al. 2018), with one recent study observing 11% of misinterpretations and 13% omitted words when interpreting genomic concepts to patients (Gutierrez et al. 2017). Similarly, previous studies have identified the demand for genetics training for interpreters in an attempt to alleviate these challenges (Krieger et al. 2018; Lara-Otero et al. 2018). The findings from this study reinforce the challenges that arise when delivering a specialty service without ensuring specialised training of technical terminology for interpreters.
Limitations
The interviews may not represent the views of the larger population as only a small number of participants were interviewed, and the majority were highly educated. Additionally, two of the participants had the same country of birth. This limits the opportunity for diverse opinions to be captured. Transferability may be limited as participants were recruited from the same metropolitan region. Furthermore, by limiting interviews to English, the study may have missed important insights from members of the CALD community who have limited or no English proficiency. However, these pilot interviews will inform future in-depth studies of the views of people from the CALD community.
Future research
The next steps will be to expand the sample for the qualitative interviews to include a wider spectrum of languages and cultural communities and to develop a broader understanding of the challenges faced by these communities in understanding genomic testing and its implications. Future research should include further consultations with members of CALD communities to refine any cultural sensitivities that require consideration when developing targeted genomic testing resources. Additional research is needed to inform development of educational tools to assist interpreters in gaining basic genetic knowledge.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study was completed in partial fulfilment of the requirements for the Master of Genomics and Health, the University of Melbourne, Victoria, Australia. This work was supported by the Victorian Government’s Operational Infrastructure Support (OIS) Programme.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Declarations
Ethics approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). The study was approved by the Royal Children’s Hospital Melbourne Human Research Ethics Committee (HREC 38264).
Consent to participate
Informed consent was obtained for all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Allford A, Qureshi N, Barwell J, Lewis C, Kai J. What hinders minority ethnic access to cancer genetics services and what may help? Eur J Hum Genet. 2014;22(7):866–874. doi: 10.1038/ejhg.2013.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729–1736. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics (2017) Census of population and housing: reflecting Australia - stories from the census 2016 (No. 2071.0). Retrieved from https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2071.0Main+Features100012016?OpenDocument
- Australian Health Ministers’ Advisory Council. (2017). National Health Genomics Policy Framework 2018–2021. Retrieved from http://www.coaghealthcouncil.gov.au/Publications/Reports
- Baty BJ, Kinney AY, Ellis SM. Developing culturally sensitive cancer genetics communication aids for African Americans. Am J Med Genet A. 2003;118a(2):146–155. doi: 10.1002/ajmg.a.10150. [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Catz DS, Green NS, Tobin JN, Lloyd-Puryear MA, Kyler P, Umemoto A, Wolman F. Attitudes about genetics in underserved, culturally diverse populations. Community Genet. 2005;8(3):161–172. doi: 10.1159/000086759. [DOI] [PubMed] [Google Scholar]
- Comino EJ, Silove D, Manicavasagar V, Harris E, Harris MF. Agreement in symptoms of anxiety and depression between patients and GPs: the influence of ethnicity. Fam Pract. 2001;18(1):71–77. doi: 10.1093/fampra/18.1.71. [DOI] [PubMed] [Google Scholar]
- Condit CM. Public understandings of genetics and health. Clin Genet. 2010;77(1):1–9. doi: 10.1111/j.1399-0004.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- Cruz-Correa M, Perez-Mayoral J, Dutil J, Echenique M, Mosquera R, Rivera-Roman K, Pardo S. Clinical cancer genetics disparities among Latinos. J Genet Couns. 2017;26(3):379–386. doi: 10.1007/s10897-016-0051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyril S, Green J, Nicholson JM, Agho K, Renzaho AM. Exploring service providers’ perspectives in improving childhood obesity prevention among CALD communities in Victoria Australia. Plos One. 2016;11(10):e0162184. doi: 10.1371/journal.pone.0162184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty MJ, Lontok KS, Donigan K, McInerney JD. The critical challenge of educating the public about genetics. Curr Genet Med Rep. 2014;2(2):48–55. doi: 10.1007/s40142-014-0037-7. [DOI] [Google Scholar]
- Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16–31. doi: 10.2105/ajph.2013.301706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman D, Brough M, Elvia R. How young people from culturally and linguistically diverse backgrounds experience mental health: some insights for mental health nurses. Int J Ment Health Nurs. 2003;12(3):194–202. doi: 10.1046/j.1440-0979.2003.00289.x. [DOI] [PubMed] [Google Scholar]
- Graves JM, Moore M, Gonzalez C, Ramos J, Nguyen L, Vavilala MS. Too little information: accessibility of information about language services on hospital websites. J Immigr Minor Health. 2020;22(3):433–438. doi: 10.1007/s10903-020-00978-8. [DOI] [PubMed] [Google Scholar]
- Greenstock L, Woodward-Kron R, Fraser C, Bingham A, Naccarella L, Elliott K, Morris M (2012) Telecommunications as a means to access health information: an exploratory study of migrants in Australia. J Public Health Res 1(3):216–221. 10.4081/jphr.2012.e34 [DOI] [PMC free article] [PubMed]
- Gregg J, Saha S (2007) Communicative competence: a framework for understanding language barriers in health care. J Gen Intern Med 22(Suppl 2):368–370. Retrieved from https://ezp.lib.unimelb.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=17957428&site=eds-live&scope=site [DOI] [PMC free article] [PubMed]
- Gutierrez AM, Robinson JO, Statham EE, Scollon S, Bergstrom KL, Slashinski MJ, Street RL. Portero versus portador: Spanish interpretation of genomic terminology during whole exome sequencing results disclosure. Per Med. 2017;14(6):503–514. doi: 10.2217/pme-2017-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez AM, Statham EE, Robinson JO, Slashinski MJ, Scollon S, Bergstrom KL, McGuire AL. Agents of empathy: How medical interpreters bridge sociocultural gaps in genomic sequencing disclosures with Spanish-speaking families. Patient Educ Couns. 2019;102(5):895–901. doi: 10.1016/j.pec.2018.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haga SB, Barry WT, Mills R, Ginsburg GS, Svetkey L, Sullivan J, Willard HF. Public knowledge of and attitudes toward genetics and genetic testing. Genet Test Mol Biomarkers. 2013;17(4):327–335. doi: 10.1089/gtmb.2012.0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P, Taylor R, Minor B, Elliott V, Fernandez M, O’Neal L, Duda S (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed]
- Henderson S, Kendall E, See L. The effectiveness of culturally appropriate interventions to manage or prevent chronic disease in culturally and linguistically diverse communities: a systematic literature review. Health Soc Care Community. 2011;19(3):225–249. doi: 10.1111/j.1365-2524.2010.00972.x. [DOI] [PubMed] [Google Scholar]
- Hudson M, Beaton A, Milne M, Port W, Russell K, Smith B, Toki V, Uerata L, Wilcox P (2016) Te Mata Ira: guidelines for genomic research with Māori. Retrieved from http://researcharchive.wintec.ac.nz/5640/
- Komaric N, Bedford S, van Driel ML (2012) Two sides of the coin: patient and provider perceptions of health care delivery to patients from culturally and linguistically diverse backgrounds. BMC Health Serv Res 18(12):322. 10.1186/1472-6963-12-322 [DOI] [PMC free article] [PubMed]
- Krieger M, Reiser CA, Petty EM, Agather A, Douglass K. Working with the Hmong population in a genetics setting: an interpreter perspective. J Genet Couns. 2018;27(3):565–573. doi: 10.1007/s10897-017-0153-0. [DOI] [PubMed] [Google Scholar]
- Lara-Otero K, Weil J, Guerra C, Cheng JKY, Youngblom J, Joseph G (2018) Genetic counselor and healthcare interpreter perspectives on the role of interpreters in cancer genetic counseling. Health Commun 1–11.10.1080/10410236.2018.1514684 [DOI] [PubMed]
- Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW. Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genomics. 2011;14(4–5):279–289. doi: 10.1159/000294191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DE, Byfield SD, Comstock CB, Garber JE, Syngal S, Crown WH, Shields AE. Underutilization of BRCA1/2 testing to guide breast cancer treatment: black and Hispanic women particularly at risk. Genet Med. 2011;13(4):349–355. doi: 10.1097/GIM.0b013e3182091ba4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewit-Mendes M, Pereira K, Dunlop K, Boughtwood T (2018) Australian genomics: genomics in the community project landscape analysis report. Retrieved from https://www.australiangenomics.org.au/resources/for-patients/genomics-in-the-community/
- QSR International Pty Ltd. (2018) NVivo (Version 12). https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Molster C, Charles T, Samanek A, O’Leary P (2009) Australian study on public knowledge of human genetics and health. Public Health Genomics 12(2):84–91. 10.1159/000164684 [DOI] [PubMed]
- Phillips C (2010) Using interpreters a guide for GPs. Aust Fam Phys 39:188–195. Retrieved from http://www.racgp.org.au/afp/2010/april/using-interpreters-–-a-guide-for-gps/ [PubMed]
- Rao DV, Warburton J, Bartlett H. Health and social needs of older Australians from culturally and linguistically diverse backgrounds: issues and implications. Australas J Ageing. 2006;25(4):174–179. doi: 10.1111/j.1741-6612.2006.00181.x. [DOI] [Google Scholar]
- Roth SC. What is genomic medicine? J Med Libr Assoc. 2019;107(3):442–448. doi: 10.5195/jmla.2019.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh M, Barlow-Stewart K, Meiser B, Muchamore I. Challenges faced by genetics service providers’ practicing in a culturally and linguistically diverse population: an Australian experience. J Genet Couns. 2009;18(5):436–446. doi: 10.1007/s10897-009-9234-z. [DOI] [PubMed] [Google Scholar]
- Samuel GN, Dheensa S, Farsides B, Fenwick A, Lucassen A. Healthcare professionals’ and patients’ perspectives on consent to clinical genetic testing: moving towards a more relational approach. BMC Med Ethics. 2017;18(1):47. doi: 10.1186/s12910-017-0207-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg JC, Rodriguez G, Howard TD, Quandt SA, Arcury TA. “He beat you in the blood”: knowledge and beliefs about the transmission of traits among Latinos from Mexico and Central America. J Immigr Minor Health. 2017;19(1):170–178. doi: 10.1007/s10903-015-0311-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A, Hurst JA (2008) ‘What is this genetics, anyway?’ Understandings of genetics, illness causality and inheritance among British Pakistani users of genetic services. J Genet Counsel (4):373. Retrieved from https://ezp.lib.unimelb.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=edsgao&AN=edsgcl.233071098&site=eds-live&scope=site [DOI] [PubMed]
- Shoemaker SJ, Wolf MS, Brach C (2014) Development of the patient education materials assessment tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. (3):395. Retrieved from https://ezp.lib.unimelb.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=edsbl&AN=RN359036175&site=eds-live&scope=site [DOI] [PMC free article] [PubMed]
- Simon CM, Zyzanski SJ, Durand E, Jimenez X, Kodish ED. Interpreter accuracy and informed consent among Spanish-speaking families with cancer. J Health Commun. 2006;11(5):509–522. doi: 10.1080/10810730600752043. [DOI] [PubMed] [Google Scholar]
- Slade I, Subramanian DN, Burton H (2016) Genomics education for medical professionals - the current UK landscape. Clin Med (Lond) 16(4):347–352. 10.7861/clinmedicine.16-4-347 [DOI] [PMC free article] [PubMed]
- StataCorp . Stata Statistical software: release 15. College Station: StataCorp LLC; 2017. [Google Scholar]
- Talwar D, Tseng TS, Foster M, Xu L, Chen LS. Genetics/genomics education for nongenetic health professionals: a systematic literature review. Genet Med. 2017;19(7):725–732. doi: 10.1038/gim.2016.156. [DOI] [PubMed] [Google Scholar]
- Walker C, Weeks A, McAvoy B, Demetriou E (2005) Exploring the role of self-management programmes in caring for people from culturally and linguistically diverse backgrounds in Melbourne, Australia. Health Expect 8(4):315–323. 10.1111/j.1369-7625.2005.00343.x [DOI] [PMC free article] [PubMed]
- Watermeyer J, Thwala Z, Beukes J (2020) Medical terminology in intercultural health interactions. Health Commun 1–10.10.1080/10410236.2020.1735700 [DOI] [PubMed]
- Zhong A, Darren B, Loiseau B, He LQB, Chang T, Hill J, Dimaras H. Ethical, social, and cultural issues related to clinical genetic testing and counseling in low- and middle-income countries: a systematic review. Genet Med. 2018 doi: 10.1038/s41436-018-0090-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Not applicable.