Abstract
Background
Schneiderian membrane thickness may influence the final clinical outcome of sinus augmentation and dental implantation. Mucosal thickening has been regarded as a contributing factor for post-treatment complications. This study aimed to systematically review the available literature on the association between mucosal thickening and potential complications related to sinus augmentation and implant placement.
Methods
An electronic search was carried out in MEDLINE, Embase, and Web of Science by two independent reviewers. It was complemented by manual search of the reference lists of all relevant studies. The studies reporting on sinus augmentation and dental implantation in cases with preoperative mucosal thickening were considered eligible for this study.
Results
The initial search yielded 1032 articles. Five hundred and sixty-four records were screened by title and abstract, and 57 studies succeeded the inclusion criteria for full-text evaluation. Finally, 10 records remained for data extraction. The included studies assessed sinus augmentation and implantation procedures in 765 patients, 324 (42.3%) of them showed mucosal thickening. Increased membrane thickness did not significantly elevate the frequency of sinus augmentation complications. In addition, the overall implant survival rate was 99.03%.
Conclusions
Within the limitations of the present study, the presence of mucosal thickening might not be a risk factor for sinus augmentation and implant survival rate.
Keywords: Dental implant, Sinus floor elevation, Mucosal thickening, Survival rate
Introduction
Dental implants are commonly used to restore oral function and esthetics [1]. The presence of adequate bone volume is necessary for implant stability [2]. Inadequate vertical bone height in edentulous posterior maxilla is a common finding due to alveolar bone resorption and sinus pneumatization, which may jeopardize proper implant placement [3].
Several techniques have been introduced to counter this limitation including tilted implants [4], zygomatic implants [5], short implants [6], and sinus augmentation approaches. Maxillary sinus floor elevation with the use of bone substitutes to increase the vertical bone height was first published by Boyne and James [7]. In this technique, the Schneiderian membrane is elevated to provide adequate space for grafting material. This procedure could be carried out in conjunction with or prior to implant placement according to the residual alveolar bone height for primary implant stability [8].
Different methods and instruments have been developed over the years to increase the implant survival rate and minimize the postoperative problems following sinus augmentation [9]. However, some complications such as membrane perforation still occur and may affect the treatment outcome.
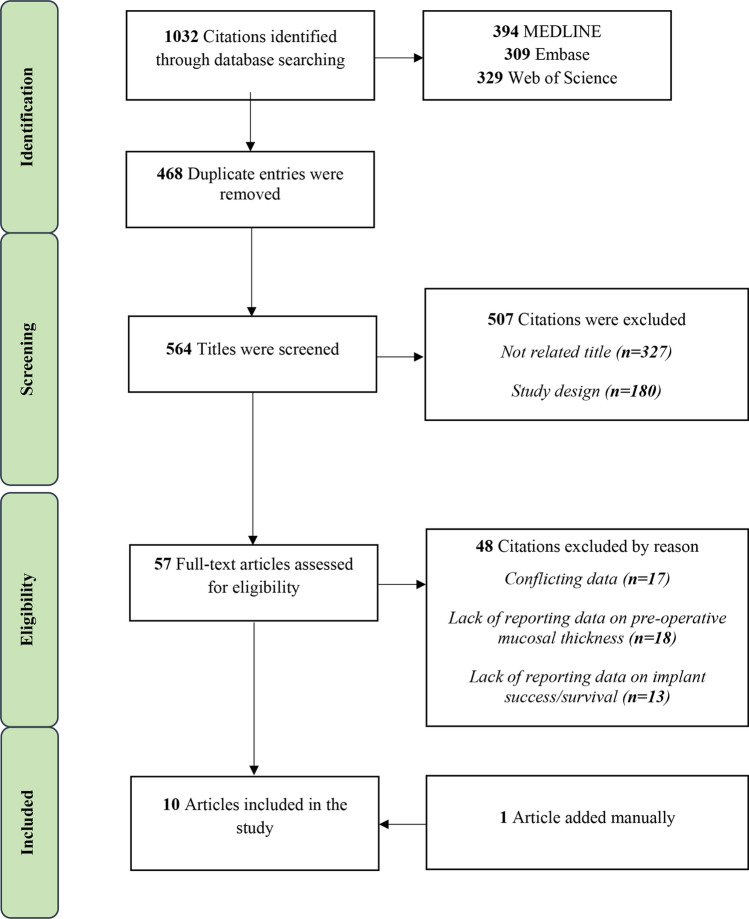
As membrane integrity has been linked to the success of sinus augmentation [10], its meticulous management has been recommended. In addition, any pathology in the maxillary sinus may affect the procedure outcome and the success of implant placement [11]. The overall prevalence of pathologies in the maxillary sinus is reported to be 56.3% [12]. The most frequent abnormality in the sinus cavity is mucosal thickening (Fig. 1), with the prevalence ranging from 25.1 to 66% [13].
Fig. 1.
Mucosal thickening is the most common sinus abnormality
Schneiderian membrane thickening may increase the probability of the sinus membrane perforation. Membrane thickness more than 2 mm is considered pathologic [14] and is defined as a hyperplastic inflammatory reaction of the maxillary sinus membrane [15]. This finding could be a result of trauma, infection, chemical agents, foreign body reaction, neoplasm, or airway conditions such as allergies, rhinitis, or asthma [16]. Sinus membrane thickness could also be influenced by some factors including gingival biotype, periodontal diseases, smoking, or certain seasonal changes [17].
Although mucosal thickening is the most common abnormality in the sinus cavity, the evidence regarding its effects on the outcomes of dental implant treatment is still limited. Therefore, this systematic review aimed to investigate the effect of sinus membrane thickness on the outcomes of sinus floor elevation and implant placement.
Methods
The present systematic review was performed in accordance with the “Preferred Reporting Items for Systematic Review and Meta-Analysis” protocol (PRISMA) [18].
PICO question (Participant, Intervention, Comparison, Outcome):
Participants (P): Partially or completely edentulous patients in need of the posterior maxillary implants.
Intervention (I): Sinus floor augmentation and dental implants in patients with mucosal thickening.
Comparison (C): Sinus floor augmentation and dental implants in patients without mucosal thickening.
Outcomes (O): Sinus floor elevation outcome and implant success and/or survival rates.
Search Strategy
An exhaustive search of the literature was carried out by two reviewers (R. A, A. M) in MEDLINE, Embase, and Web of Science up to April 2020. Search terms included the following keywords, which were modified appropriately for each database:
(implant) AND (sinus augmentation OR sinus lift OR sinus elevation OR sinus floor augmentation OR sinus floor elevation) AND (mucosal thickening OR mucosal thickness OR membrane thickness OR schneiderian membrane OR mucosal thickening pathology).
(edentulous jaw OR edentulous mouth OR partially edentulous jaw) AND (alveolar resorption OR alveolar bone atrophy OR alveolar bone loss) AND (sinus augmentation therapy OR maxillary sinus floor augmentation) AND (Schneiderian membrane OR sinus membrane).
(sinus lift OR sinus floor elevation OR bone augmentation) AND sinus AND mucosal thickening AND dental implant.
We did not limit our search strategy regarding the study design, as doing so could have excluded some pertinent publications [19]. No publication status, language or time restrictions were applied. The electronic search was complemented by manual search of the reference lists of all relevant articles. Any disagreements during the process were resolved by discussion with a third reviewer (M. K).
Inclusion Criteria
Titles and abstracts of the retrieved articles were screened independently by two independent authors (A. M, M, N) based on the predetermined inclusion criteria.
The inclusion criteria were as follows:
Prospective or retrospective human studies with ≥ 10 participants
Full text availability
Reporting on preoperative sinus membrane thickness
Reporting on implant survival and/or success rates
Sinus floor elevation outcomes
The exclusion criteria were as follows:
Without proper follow-up information.
Review, case reports, expert opinions, in vitro studies, and animal studies
The procedure success could not be clearly derived from the presented data
Data extraction was performed by two independent authors (A. M, M, N) using a predefined data extraction table. Any disagreements was resolved by a third author (M. K).
Qualitative Assessment
Two reviewers (R. A, M, K) independently assessed the quality of the identified studies and resolved any disagreements through discussion.
For non-randomized clinical trials, qualitative assessment was performed using Newcastle–Ottawa Quality Assessment Scale (NOS) [20]. Quality assessment for one randomized controlled clinical trial was assessed based on The Cochrane risk of bias tool for randomized trials [21].
Statistical Analysis
To carry out the present systematic review the Microsoft Excel was used for calculations. Furthermore, Comprehensive Meta-Analysis 2.2.064 was used for meta-analysis and the corresponding forest plot.
Results
A total of 1032 articles were retrieved through all three search strategies. After exclusion of 468 duplicate entries, 564 records were remained for further screening. Excluding articles based on titles and abstracts, 57 studies were remained for full text assessment. One article was added by manual search of the reference lists of all relevant articles. Finally, 10 records [22–30] were included for the final evaluation (Fig. 2).
Fig. 2.
Flowchart of the screening process
The qualitative assessment for non-randomized studies is presented in Supplementary Table. The only randomized clinical trial [14] was evaluated as “moderate potential risk’ of bias based on the Cochrane risk of bias tool for randomized trials.
In order to evaluate the effects of mucosal thickening on the outcomes of sinus grafting and implant placement success, increased mucosal thickness of more than 2 mm was considered pathologic (regardless of the reason for the thickening), in accordance with some previous studies [31–33].
The included studies assessed sinus augmentation procedures in 765 patients aged between 18 and 94 years (351 females, 414 males), with the mean follow-up duration of 39.3 months. They received 865 implants, considering 4 studies did not report their implant numbers [22, 23, 27, 30] (Table 1). The mean smoking rate was 25.7%, while three studies did not report on smoking status of their participants [23, 24, 27].
Table 1.
Characteristic of the participants in the included studies
| Author/year | Study design | Participants (n) | Age (Y) | Gender | Smoking | |
|---|---|---|---|---|---|---|
| Overall | MT | |||||
| Ritter et al./2020 [30] | Retrospective | 145 sinuses |
55 MT (> 2 mm) 19 Cyst/Polyp 5 Sinus opacification 10 Ostium obstruction |
18–94 |
82 F 63 M |
31 (21%) |
| Küçükkurt/2019 [26] | Retrospective |
88 115 sinuses (27 bilateral, 61 unilateral) |
43 27 MT (≥ 3 mm) 35 sinuses\ 16 Peseudocyst (17 sinuses) |
30–73 |
34 F 54 M |
47 (53.4%) |
| Gong et al./2019 [23] | Retrospective | 92 | 19 MT (> 2 mm) | 44–48 |
38 F 54 M |
NR |
| Najm et al./2018 [28] | Retrospective |
13 14 sinuses |
2 MT (> 2 mm) 1 in a smoker | 38–69 | 13 F | 2 (15%) |
| Chen et al./2017 [22] | Prospective | 84 |
19 Solitary polyps or cysts 17 MT 6 Fluid accumulation 1 Near-total opacification 2 Calcification spots |
Average: 48.8 |
29 F 55 M |
16 (19%) |
| Qin et al./2017 [29] | Prospective | 100 |
28 13 Flat thickening 15 Pseudocyst |
20–80 |
47 F 53 M |
19 (19%) |
| Maska et al./2017 [27] | Retrospective | 29 |
6.9% Minimal thickening (> 1 mm but ≤ 2 mm) 20.7% Moderate thickening (> 2 mm but ≤ 5 mm) 65.5% Severe thickening (> 5 mm) |
NR |
11 F 18 M |
NR |
| Kfir et al./2014 [25] | Retrospective | 16 | 16 | 26–64 |
7 F 9 M |
4 (25%) |
| Kayabasoglu et al./2014 [24] | Retrospective |
94 145 sinuses (51 bilateral, 43 unilateral) |
94 | 29–71 |
32 F 62 M |
NR |
| Garcia et al./2013 [14] | RCT | 104 (135 sinuses) |
58 (> 2 mm) 3 mucosal cyst |
39–81 |
58 F 46 M |
30 (27.8%) |
MT Mucosal thickening, F Female, M Male, Y Years, NR Not reported
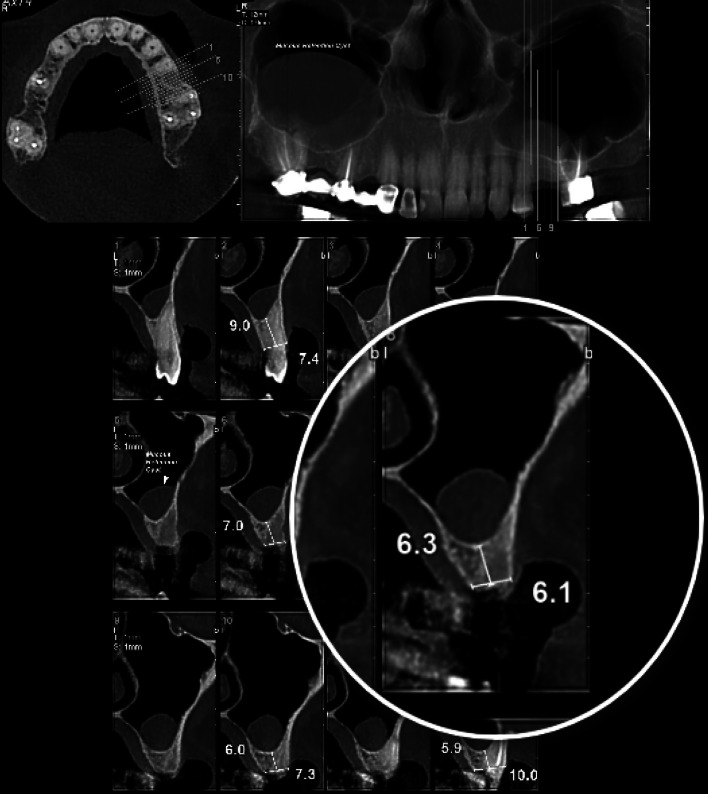
The most common method used for evaluation of the mucosal thickness was cone-beam computed tomography (CBCT) (61.5%) (Table 2). Two studies [14, 30] used computed tomography (CT) scans to measure mucosal thickness, while one study [24] used CT only for cases with sinusitis. The reported cases of mucosal thickening reached 324 patients (excluding pseudocysts, polyps, and opacification), and its prevalence among articles that had not excluded cases with normal mucosa was 30.6% [14, 22, 23, 26–30, 34, 35]. Five studies used lateral window approach for sinus floor augmentation [14, 24, 26, 28, 30], four studies applied transcrestal technique [23, 25, 29, 30] (two studies with bone substitute [23, 29]), and two studies did not report on their surgical approach [22, 27]. Ritter et al. [30] applied both approaches (79% Lateral window and 21% transcrestal sinus grafting).
Table 2.
Membrane thickness, residual bone height, and surgical approach in the included studies
| Author/year | Method of evaluation | Preoperative membrane thickness (mm) | Average residual bone height (mm) | Surgical approach | Implant (n) | Implant placement |
|---|---|---|---|---|---|---|
| Ritter et al./2020[30] | CT | 8.9 ± 4.6 mm | NR | 79% Lateral window 21% Transcrestal | NR | 97 Simultaneous (67%) 48 Delayed (33%) |
| Küçükkurt/2019 [26] | CBCT | 7.97 ± 2.82 mm 12,6 ± 4.47 mm Pseudocyst | 3.1 ± 1.40 mm Control group 4.5 ± 1.70 mm MT group | Lateral window | 168 | Simultaneous |
| Gong et al./2019 [23] | CBCT | > 2 mm | 5.36 ± 1.28 mm Control group 5.15 ± 1.34 mm MT group | Transcrestal Bone substitute | NR | Simultaneous |
| Najm et al./2018 [28] | CBCT | > 2 mm | 5.6 ± 1.9 mm | Lateral window | 21 | Simultaneous |
| Chen et al./2017 [22] | CBCT | > 2 mm | NR | NR | NR | Delayed |
| Qin et al./2017 [29] | CBCT | > 2 mm | 7.21 ± 1.12 mm | Transcrestal Bone substitute | 100 | Simultaneous (non-submerged) |
| Maska et al./2017 [27] | CBCT | > 2 mm | NR | NR | NR | NR |
| Kfir et al./2014 [25] | CT | 15 ± 4.8 mm | NR | Transcrestal with balloon elevation | 30 | Simultaneous |
| Kayabasoglu et al./2014 [24] | OPG CT in patients with sinusitis | ≥ 5 | NR | Lateral window | 268 | Simultaneous |
| Garcia et al./2013 [14] | CT | > 2 | NR | Lateral window | 278 | 61 Simultaneous 74 Delayed |
MT Mucosal thickening, CBCT Cone-beam computed tomography, CT Computed tomography, OPG Orthopantomograph, NR Not reported
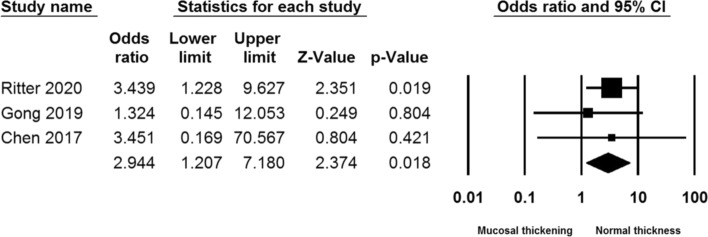
Eight studies installed implants simultaneously with sinus augmentation [14, 23–26, 28–30], three studies used a delayed implant installation protocol [14, 22, 30], and one study [27] did not report the implant placement approach (two studies [14, 30] applied both protocols). The overall implant survival rate was 99.03%, which was not significantly different in sinuses with and without mucosal thickening. One study even reported separate survival rates in cases with and without mucosal thickening (98.7% vs. 94.1%) [26]. In addition, the survival rate showed no relationship with the implant placement protocol (simultaneous/delayed or one stage/two stage) (p > 0.05). Three studies [22, 23, 30] reported distinct sinus membrane perforation rates in cases with and without mucosal thickening, which shows that this finding was less frequent in sinuses with increased membrane thickness (Fig. 3).
Fig. 3.
Cumulative odds ratio of sinus membrane perforation in sinuses with and without mucosal thickening
Discussion
Previous studies have reported that the mucosal thickness is ≥ 2 mm in 23–55% [36] and ≥ 3 mm in 10–12% [36, 37] of population. It has also been reported that 56.3% of the maxillary sinuses have pathologies [12], the most common of which is mucosal thickening, with prevalence ranging from 25.1 to 56.5% [13]. The studies included in this review reported mucosal thickening in 324 (42%) cases. The prevalence of mucosal thickening in articles that had not excluded cases with normal mucosa was 30.6%.
Most of the included studies reported the thickness of > 2 mm as mucosal thickening, which is consistent with other studies reporting the normal sinus membrane thickness ranging from 0.8 to 1.99 mm [27, 38], and the thickness of > 2 mm as pathologic mucosal thickening (regardless of the underlying etiology) [31–33]. However, some investigations [26, 27] considered other criteria as abnormal membrane thickness. This could be explained by the authors’ definition of mucosal thickening and its consequences on the postoperative complications such as ostium obstruction [31, 32].
Higher prevalence of mucosal thickening was reported in patients with a history of periodontitis [27], which might be due to pro-inflammatory reactions involved in such circumstances. No association was found in terms of age [26], gender [26, 27], systemic factors, alveolar ridge height, endodontic treatment or other dental history issues [27]. However, previous systematic reviews concluded that periodontitis, smoking [39], male gender, and apical pathology [33] may result in the thickening of the sinus membrane. Such heterogeneous results could be rooted in differences in populations, sample sizes, and diagnostic thresholds for sinus membrane thickening (Table 3).
Table 3.
Follow up duration, implant outcome, and complications in the included studies
| Author/year | Follow-up (months) | Survival rate/success rate (%) | Perforation rate (%) | Complication |
|---|---|---|---|---|
| Ritter et al./2020[30] | 6–107 | 98.5% success rate |
11% of cases with increased thickness 29% of cases with normal thickness |
32 Mucosal perforation 10 Local infection 4 Postoperative bleeding 3 Flap dehiscence 2 Oroantral fistula |
| Küçükkurt/2019 [26] |
25.1 ± 10 Control group 27.8 ± 9.5 MT group |
96.4% 94.1% Survival rate (control group) 98.7% Survival rate (Pathology group) |
NR | NR |
| Gong et al./2019 [23] | 4–6 | 100% Survival rate |
6.5% Normal thickness 5% MT |
6 Mucosal perforation |
| Najm et al./2018 [28] | 120 | 100% Survival rate | 21.40% | 3 Mucosal perforations |
| Chen et al./2017 [22] | 3 | 100 Survival rate |
7.1% Normal thickness No perforation in cases with thickening |
1 Perforation |
| Qin et al./2017 [29] | 7.82 ± 2.02 | 100% Survival rate | 2.33% | 3 Mucosal perforations |
| Maska et al./2017 [27] | 12–94 |
100% Survival rate 100% Success rate |
NR | NR |
| Kfir et al./2014 [25] | 6–50 | 100% Success rate | None | None |
| Kayabasoglu et al./2014 [24] | 5–47 | 99.6% Survival rate | 8.5% (none of them developed sinusitis) | 4 Postoperative sinusitis |
| Garcia et al./ 2013 [14] | 12 | 95.3% Survival rate | 7.50% |
3 Postoperative pain 8 Perforations |
MT Mucosal thickening, NR Not reported
The overall 3-year survival rate of implants installed in conjunction or after sinus augmentation was reported to be 90.1% in a previous systematic review [40]. The present review concluded an overall sinus floor elevation success rate of 97.1%. The survival rate associated with implants placed in the sinus augmentation regions with preoperative mucosal thickening (324 cases) was 99.3%. It could be concluded that the presence of mucosal thickening might not have any association with the sinus augmentation and implant survival rate. This finding is in accordance with another study [41] showing that sinus pathologies including sinus membrane thickening does not have any association with sinus augmentation and implant success rate [27, 42].
Physiologic mucosal thickening does not seem to contribute to implant failure [27]. However, no clear conclusions can be made on the association between mucosal thickening as a result of sinusitis and implant survival. Hence, it could be suggested that if sinusitis is suspected, clinicians should consult the appropriate medical specialists prior to implant placement. It has also been concluded that only patients with complete sinus opacification need to be referred to an otolaryngologist prior to surgery [30]. These are in agreement with other studies reporting that mucosal thickening might be a concern if it is associated or accompanied by other pathologies including large cysts, polyps and sinus opacifications (Fig. 4); such subjects have been suggested to be referred before sinus floor augmentation [22].
Fig. 4.
Large cysts are suggested to be referred to an otolaryngologist before sinus augmentation
A noteworthy complication, which should be considered while evaluating the presence of mucosal thickening in sinus augmentation, is postoperative ostium obstruction. It seems that sinus augmentation for healthy sinuses has no risk of ostium obstruction, but mucosal thickening could be an obstacle during sinus elevation and may lead to failure or complications. It can also lead to ostium blockage when the sinus membrane is elevated and the graft material is placed under it, which in turn could lead to drainage disturbances and sinusitis [31]. Although this complication might not affect the implant survival rate, it should be considered preoperatively. Preoperative ostium obstruction was only reported in 10 cases in one study in this review [30], but it was not correlated to more frequent complications in asymptomatic patients.
Sinus membrane perforation is considered the most common complication during sinus augmentation procedure and the sinus membrane thickness has been studied as a risk factor for perforation [31]. If perforations have any effects on the implant survival rate, and membrane thickness has an effect on the rate of perforations, then it could be expected that sinus membrane thickness should have an effect on the implant survival rate. The association between sinus membrane thickness and membrane perforation has been studied with some conflicting results. A significant correlation has been identified between membrane thickness and perforation rate in transcrestal approach [43], and the perforation rate was lowest when the thickness was 1.5–2 mm, which increased two to threefold in both thinner or thicker Schneiderian membranes. The studies included in this review reported the overall perforation rate of 8.62%, which was less common in sinuses with increased mucosal thickness (4.9% vs. 11.2%). It may postulated that a thin membrane might be perforated due to the lack of sufficient mechanical support to resist elevation force or bone graft insertion. In addition, some novel instruments have recently been introduced to prevent membrane perforation using transcrestal approach; these methods are, however, technique sensitive and inadvertent execution may lead to a higher rate of membrane perforation. Thicker membranes could resist stronger forces, allowing more compaction of the bone substitute material and consequently better osseointegration and higher implant survival rate [44].
The studies conducted on the association between sinus membrane perforation and implant survival rate have conflicting results, as well. A meta-analysis conducted in 2018 showed that an intraoperative sinus membrane perforation could increase the risk of implant failure after the sinus floor elevation [45]. This association may be explained by spreading of the grafting material in large perforations and consequent inflammation, which may lead to the failure of immediate bone grafting and implant loss. However, some other studies have concluded that sinus membrane perforation has no detrimental effect upon the implant survival rate [46], which is in agreement with the results of our included studies.
One of the main limitations of this review is that histologic studies have shown that 3-D imaging might overestimate mucosal thickness and lead to measurement inaccuracies. In addition, most of the included investigations did not follow a consistent and standardized method to measure membrane thickness, as it has shown that sinus membrane thickness is not homogeneous throughout the sinus cavity [47]. These limitations should be considered as a source of bias and be kept in mind during interpretation.
Conclusion
Within the limitations of the present study, it seems that the presence of physiologic mucosal thickening does not contribute to implant failure and sinus augmentation complications. However, more prospective studies are needed to conclude regarding the effect of pathologic increased mucosal thickness on implant survival.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
Not applicable.
Declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12663-021-01551-y.
References
- 1.Cho-Lee GY, Naval-Gias L, Castrejon-Castrejon S, Capote-Moreno AL, Gonzalez-Garcia R, Sastre-Perez J, Munoz-Guerra MF. A 12-year retrospective analytic study of the implant survival rate in 177 consecutive maxillary sinus augmentation procedures. Int J Oral Maxillofac Implant. 2010;25(5):1019–1027. [PubMed] [Google Scholar]
- 2.Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, Belser UC, Lang NP. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implant Res. 1997;8(3):161–172. doi: 10.1034/j.1600-0501.1997.080302.x. [DOI] [PubMed] [Google Scholar]
- 3.Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology-eleven years of surgical experience (1979–1990) J Oral Implantol. 1990;16(3):199–209. [PubMed] [Google Scholar]
- 4.Del Fabbro M, Bellini CM, Romeo D, Francetti L. Tilted implants for the rehabilitation of edentulous jaws: a systematic review. Clin Implant Dent Relat Res. 2012;14(4):612–621. doi: 10.1111/j.1708-8208.2010.00288.x. [DOI] [PubMed] [Google Scholar]
- 5.Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and complications of zygomatic implants: an updated systematic review. J Oral Maxillofac Surg. 2016;74(10):1949–1964. doi: 10.1016/j.joms.2016.06.166. [DOI] [PubMed] [Google Scholar]
- 6.Esposito M, Barausse C, Pistilli R, Sammartino G, Grandi G, Felice P. Short implants versus bone augmentation for placing longer implants in atrophic maxillae: One-year post-loading results of a pilot randomised controlled trial. Eur J Oral Implantol. 2015;8(3):257–268. [PubMed] [Google Scholar]
- 7.Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38(8):613–616. [PubMed] [Google Scholar]
- 8.Kaufman E. Maxillary sinus elevation surgery an overview. J Esthet Restor Dent. 2003;15(5):272–282. doi: 10.1111/j.1708-8240.2003.tb00298.x. [DOI] [PubMed] [Google Scholar]
- 9.Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;8(1):328–343. doi: 10.1902/annals.2003.8.1.328. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004;75(4):511–516. doi: 10.1902/jop.2004.75.4.511. [DOI] [PubMed] [Google Scholar]
- 11.Manji A, Faucher J, Resnik RR, Suzuki JB. Prevalence of maxillary sinus pathology in patients considered for sinus augmentation procedures for dental implants. Implant Dent. 2013;22(4):428–435. doi: 10.1097/ID.0b013e31829d1a20. [DOI] [PubMed] [Google Scholar]
- 12.Gracco A, Incerti Parenti S, Ioele C, Alessandri Bonetti G, Stellini E. Prevalence of incidental maxillary sinus findings in Italian orthodontic patients: a retrospective cone-beam computed tomography study. Korean J Orthod. 2012;42(6):329–334. doi: 10.4041/kjod.2012.42.6.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drumond JP, Allegro BB, Novo NF, de Miranda SL, Sendyk WR. Evaluation of the prevalence of maxillary sinuses abnormalities through spiral computed tomography (CT) Int Arch Otorhinolaryngol. 2017;21(2):126–133. doi: 10.1055/s-0036-1593834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia-Denche JT, Wu X, Martinez PP, Eimar H, Ikbal DJ, Hernandez G, López-Cabarcos E, Fernandez-Tresguerres I, Tamimi F. Membranes over the lateral window in sinus augmentation procedures: a two-arm and split-mouth randomized clinical trials. J Clin Periodontol. 2013;40(11):1043–1051. doi: 10.1111/jcpe.12153. [DOI] [PubMed] [Google Scholar]
- 15.Van Dis ML, Miles DA. Disorders of the maxillary sinus. Dent Clin North Am. 1994;38(1):155–166. [PubMed] [Google Scholar]
- 16.White SC, Pharoah MJ. Oral Radiology Principles and Interpretation. 7. Mosby Elsevier; 2014. [Google Scholar]
- 17.Bornstein MM, Wasmer J, Sendi P, Janner SF, Buser D, von Arx T. Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: a comparative radiographic analysis using limited cone beam computed tomography. J Endod. 2012;38(1):51–57. doi: 10.1016/j.joen.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed) 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harden A, Peersman G, Oliver S, Mauthner M, Oakley A. A systematic review of the effectiveness of health promotion interventions in the workplace. Occup Med (Lond) 1999;49(8):540–548. doi: 10.1093/occmed/49.8.540. [DOI] [PubMed] [Google Scholar]
- 20.Wells G, Brodsky L, O'Connell D, Shea B, Henry D, Mayank S, Tugwell P (2009) The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed 19 Oct 2009
- 21.Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. London: The Cochrane Collaboration
- 22.Chen YW, Lee FY, Chang PH, Huang CC, Fu CH, Huang CC. Lee TJ A paradigm for evaluation and management of the maxillary sinus before dental implantation. Laryngoscope. 2018;128(6):1261–1267. doi: 10.1002/lary.26856. [DOI] [PubMed] [Google Scholar]
- 23.Gong T, Hu C, Chen Y, Zhou N, Wu H, Man Y. Raising the transcrestal sinus floor in the presence of antral pseudocysts, and in sinus floors with a normal Schneiderian membrane: a retrospective cohort study. Clin Oral Implant Res. 2019;57(5):466–472. doi: 10.1016/j.bjoms.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 24.Kayabasoglu G, Nacar A, Altundag A, Cayonu M, Muhtarogullari M, Cingi C. A retrospective analysis of the relationship between rhinosinusitis and sinus lift dental implantation. Head Face Med. 2014;10:53. doi: 10.1186/1746-160X-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kfir E, Goldstein M, Abramovitz I, Kfir V, Mazor Z, Kaluski E. The effects of sinus membrane pathology on bone augmentation and procedural outcome using minimal invasive antral membrane balloon elevation. J Oral Implantol. 2014;40(3):285–293. doi: 10.1563/AAID-JOI-D-11-00253. [DOI] [PubMed] [Google Scholar]
- 26.Küçükkurt S. Evaluation of the survival of implant placement simultaneously with sinus augmentation: relationship in maxillary sinus pathologies. Oral Radiol. 2020;36(3):225–237. doi: 10.1007/s11282-019-00399-w. [DOI] [PubMed] [Google Scholar]
- 27.Maska B, Lin GH, Othman A, Behdin S, Travan S, Benavides E, Kapila Y. Dental implants and grafting success remain high despite large variations in maxillary sinus mucosal thickening. Int J Implant Dent. 2017;3(1):1–8. doi: 10.1186/s40729-017-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Najm SA, Nurdin N, El Hage M, Bischof M, Nedir R. Osteotome sinus floor elevation without grafting: a 10-year clinical and cone-beam sinus assessment. Implant Dent. 2018;27(4):439–444. doi: 10.1097/ID.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 29.Qin L, Lin SX, Guo ZZ, Zhao N, Song YL, Xie C, Li DH. Influences of Schneiderian membrane conditions on the early outcomes of osteotome sinus floor elevation technique: a prospective cohort study in the healing period. Clin Oral Implant Res. 2017;28(9):1074–1081. doi: 10.1111/clr.12920. [DOI] [PubMed] [Google Scholar]
- 30.Ritter A, Rozendorn N, Avishai G, Rosenfeld E, Koren I, Soudry E. Preoperative maxillary sinus imaging and the outcome of sinus floor augmentation and dental implants in asymptomatic patients. Ann Otol Rhinol Laryngol. 2020;129(3):209–215. doi: 10.1177/0003489419883292. [DOI] [PubMed] [Google Scholar]
- 31.Carmeli G, Artzi Z, Kozlovsky A, Segev Y, Landsberg R. Antral computerized tomography preoperative evaluation: relationship between mucosal thickening and maxillary sinus function. Clin Oral Implant Res. 2011;22(1):78–82. doi: 10.1111/j.1600-0501.2010.01986.x. [DOI] [PubMed] [Google Scholar]
- 32.Shanbhag S, Karnik P, Shirke P, Shanbhag V. Cone-beam computed tomographic analysis of sinus membrane thickness, ostium patency, and residual ridge heights in the posterior maxilla: implications for sinus floor elevation. Clin Oral Implant Res. 2014;25(6):755–760. doi: 10.1111/clr.12168. [DOI] [PubMed] [Google Scholar]
- 33.Vogiatzi T, Kloukos D, Scarfe WC, Bornstein MM. Incidence of anatomical variations and disease of the maxillary sinuses as identified by cone beam computed tomography: a systematic review. Int J Oral Maxillofac Implant. 2014;29(6):1301–1314. doi: 10.11607/jomi.3644. [DOI] [PubMed] [Google Scholar]
- 34.Cortes AR, Cortes DN, Arita ES. Effectiveness of piezoelectric surgery in preparing the lateral window for maxillary sinus augmentation in patients with sinus anatomical variations: a case series. Int J Oral Maxillofac Implant. 2012;27(5):1211–1215. [PubMed] [Google Scholar]
- 35.Lundgren S, Johansson AS, Cricchio G, Lundgren S. Clinical outcome and factors determining new bone formation in lateral sinus membrane elevation with simultaneous implant placement without grafting material: a cross-sectional, 3–17 year follow-up study. Clin Implant Dent Relat Res. 2019;21(5):827–834. doi: 10.1111/cid.12758. [DOI] [PubMed] [Google Scholar]
- 36.Janner SFM, Caversaccio MD, Dubach P, Sendi P, Buser D, Bornstein MM. Characteristics and dimensions of the Schneiderian membrane: a radiographic analysis using cone beam computed tomography in patients referred for dental implant surgery in the posterior maxilla. Clin Oral Implant Res. 2011;22(12):1446–1453. doi: 10.1111/j.1600-0501.2010.02140.x. [DOI] [PubMed] [Google Scholar]
- 37.Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):e80–87. doi: 10.1016/j.tripleo.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 38.Yilmaz HG, Tozum TF. Are gingival phenotype, residual ridge height, and membrane thickness critical for the perforation of maxillary sinus? J Periodontol. 2012;83(4):420–425. doi: 10.1902/jop.2011.110110. [DOI] [PubMed] [Google Scholar]
- 39.Monje A, Diaz KT, Aranda L, Insua A, Garcia-Nogales A, Wang HL. Schneiderian membrane thickness and clinical implications for sinus augmentation: a systematic review and meta-regression analyses. J Periodontol. 2016;87(8):888–899. doi: 10.1902/jop.2016.160041. [DOI] [PubMed] [Google Scholar]
- 40.Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35(8 Suppl):216–240. doi: 10.1111/j.1600-051X.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 41.Lim HC, Nam JY, Cha JK, Lee JS, Lee DW, Jung UW, Choi SH. Retrospective analysis of sinus membrane thickening: profile, causal factors, and its influence on complications. Implant Dent. 2017;26(6):868–874. doi: 10.1097/ID.0000000000000667. [DOI] [PubMed] [Google Scholar]
- 42.Jungner M, Legrell PE, Lundgren S. Follow-up study of implants with turned or oxidized surfaces placed after sinus augmentation. Int J Oral Maxillofac Implant. 2014;29(6):1380–1387. doi: 10.11607/jomi.3629. [DOI] [PubMed] [Google Scholar]
- 43.Wen SC, Lin YH, Yang YC, Wang HL. The influence of sinus membrane thickness upon membrane perforation during transcrestal sinus lift procedure. Clin Oral Implant Res. 2015;26(10):1158–1164. doi: 10.1111/clr.12429. [DOI] [PubMed] [Google Scholar]
- 44.Antonaya-Mira R, Barona-Dorado C, Martinez-Rodriguez N, Caceres-Madrono E, Martinez-Gonzalez JM. Meta-analysis of the increase in height in maxillary sinus elevations with osteotome. Med Oral Patol Oral Cir Bucal. 2012;17(1):e146–152. doi: 10.4317/medoral.16921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al-Moraissi E, Elsharkawy A, Abotaleb B, Alkebsi K, Al-Motwakel H. Does intraoperative perforation of Schneiderian membrane during sinus lift surgery causes an increased the risk of implants failure?: a systematic review and meta regression analysis. Clin Implant Dent Relat Res. 2018;20(5):882–889. doi: 10.1111/cid.12660. [DOI] [PubMed] [Google Scholar]
- 46.Froum SJ, Khouly I, Favero G, Cho SC. Effect of maxillary sinus membrane perforation on vital bone formation and implant survival: a retrospective study. J Periodontol. 2013;84(8):1094–1099. doi: 10.1902/jop.2012.120458. [DOI] [PubMed] [Google Scholar]
- 47.Aimetti M, Massei G, Morra M, Cardesi E, Romano F. Correlation between gingival phenotype and Schneiderian membrane thickness. Int J Oral Maxillofac Implant. 2008;23(6):1128–1132. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.