Abstract
Aim
The objective of this study was to correlate the preoperative radiological findings and intraoperative surgical findings during removal of impacted mandibular 3rd molar with respect to the inferior alveolar canal.
Materials and Method
The prospective study design included 100 patients between the age group of 20 years and 50 years who visited the Department of Oral and Maxillofacial Surgery at Vydehi Institute of Dental Sciences and Research Centre, Whitefield, Bengaluru. A preoperative panoramic radiograph was taken and the parameters were assessed and a normal surgical protocol was followed to extract the impacted mandibular 3rd molar with intra-operative assessment as well.
Results
Out of the 100 patients with definitive radiological signs showing close relation of the third molar to the mandibular canal who underwent surgical removal, only 12 patients presented with definitive clinical findings of the association.
Conclusion
A true close relationship between the third molars and mandibular canal increases the risk of inferior alveolar nerve injury, and accurate evaluation of the relationship is essential to avoid the risk of surgery. The accuracy of the plain radiographs to diagnose an intimate relationship between the neurovascular bundle and the third molar root has its limitations, since only 12 of the 100 patients with positive radiological signs showed clinical evidence of involvement. Surgeons should be aware of the limitations of the radiographic markers of panoramic radiography and should consider more detailed imaging in more specific cases in which one or more radiographic marker is present.
Keywords: Inferior alveolar canal, Mandibular 3rd molar, Panoramic radiograph
Introduction
The extraction of an impacted or erupted third molar is regarded to be the most common dentoalveolar procedure performed in oral and maxillofacial surgery. The principal teeth that present as impaction is either third molars or canines. Mandibular third molars are considered to be the most commonly impacted teeth [1, 2].
The inferior alveolar nerve runs in a canal within the mandible usually near the apices of the third molar and if the molar is impacted, a close relationship of the roots to the nerve is likely. Some times during the surgical removal of mandibular third molar, the inferior alveolar nerve is damaged leading to impairment of sensation in the lower lip [2]. The reported frequency of IAN injury associated with mandibular third molar ranges from 0.6 to 5.3%. The risk of permanent IAN injury is less than 1% [3].
Preoperative assessment must be carried out radiologically in an attempt to identify the proximity of the impacted tooth to the inferior alveolar canal. An inherent risk of mandibular third molar odontectomy is damage to inferior alveolar nerve, which generally lies in a position buccal and inferior to the roots. The major risk factors associated with IAN injury include advanced patient age, depth of impaction, tooth angulation, need for tooth sectioning and bone removal, surgeon experience and radiographic predictors [4].
Inferior alveolar nerve injury can result from a number of different actions which include the use of elevators, pressure directly or indirectly on the nerve or the use of burs if drilling reaches the nerve. Direct visualization of an intact IAN bundle during third molar indicates that the third molar was intimately associated with the IAN and poses 20% risk of subsequent paresthesia. On the other hand, intraoperative hemorrhage within the socket and postoperative swelling can cause an IAN damage [5, 6].
The dental panoramic tomograph (DPT) is the most common primary radiographic investigation of choice in the preoperative assessment of mandibular third molar teeth. It is useful to assess the position, depth and type of impaction, as well as texture of investing bone. However, there is difference between the preoperative radiological assessment of the anatomy of the third molar and their relation to the inferior alveolar neurovascular bundle on DPT, and the findings during surgery [7].
Materials and Method
This prospective study was carried out in the department of oral and maxillofacial surgery at Vydehi Institute of Dental Sciences and Research Centre, Bangalore, India. A total number of 100 subjects, both males and females in the age group of 20–50 years were included in the study. Since this study involved human subjects, all Helsinki guidelines were complied with.
Inclusion Criteria
Subjects having impacted mandibular 3rd molars requiring extraction.
Subjects having impacted mandibular 3rd molar in which preoperative radiological assessment showed intimate relationship with inferior alveolar canal.
Subjects between the age group of 20–50 years.
Subjects having impacted mandibular 3rd molar in which root formation is complete.
Subjects in good health (ASA1 or 2).
Exclusion Criteria
Subjects less than 20 years of age or more than 50 years of age.
Subjects having impacted mandibular 3rd molar in which root formation is not complete.
Preoperative radiograph showing the distance between the root of the tooth and the inferior alveolar canal is more than 1 mm.
Subjects under ASA 3 and greater.
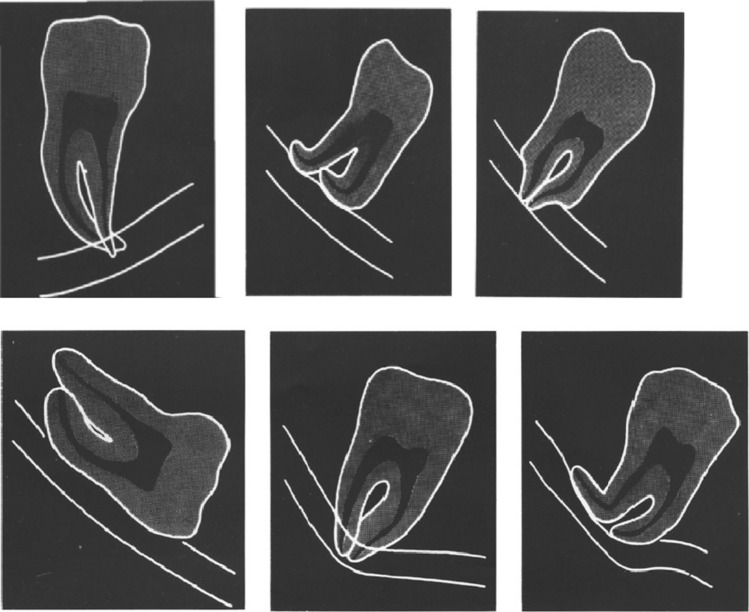
Preoperative radiological assessment was done by using panoramic radiograph (Fig. 1). Normal surgical protocols were followed to extract the impacted mandibular 3rd molar. All the surgical procedures were performed by a single operator. Intraoperative assessment of the extraction socket and the extracted tooth was done by using the clinical parameters. The radiological parameters for preoperative radiological assessment were: darkening of the root, deflection of the roots, narrowing of the root, dark and bifid apex of the root, interruption of white lines of the canal, diversion of the inferior alveolar canal, narrowing of the inferior alveolar canal, root of tooth just touching the upper outline of the neurovascular bundle and root of tooth superimposed on the neurovascular bundle. The parameters for the clinical assessment were: grooving of root of the extracted tooth (Fig. 2), oozing of blood from the socket (Fig. 3), presence of inferior alveolar canal in the empty socket when the socket is examined after irrigation (Fig. 4).
Fig. 1.
OPG
Fig. 2.

Grooving of root
Fig. 3.

Oozing from socket
Fig. 4.
Relationship of tooth root and inferior alveolar canal
Results
Out of 100 patients, 64 patients (64%) were male and 36 patients (36%) were female. Among the various preoperative radiological signs, interruption of white line of the canal was found in 44 (44%) patients, root of the tooth superimposed on the neurovascular bundle was found in 24 (24%) patients, narrowing of the canal was found in 10 (10%) patients, darkening of the root was found in 2 (2%) patients, deflection of the root was found in 1 (1%) patient, diversion of the canal was found in 2 (2%) patients, root of the tooth just touching the upper outline of the neurovascular bundle was found in 1 (1%) patient, darkening of root and interruption of white line was found in 1 (1%) patient, interruption of white line and narrowing of canal was found in 3 (3%) patients, interruption of white line and root of the tooth superimposed on the neurovascular bundle was found in 8 (8%) patients, narrowing of the canal and root of the tooth superimposed on the neurovascular bundle was found in 1 (1%) patient, deflection of the root and interruption of white line of the canal was found in 2 (2%) patients, interruption of white line of the canal and diversion of the canal was found in 1 (1%) patient.
The most common intraoperative clinical sign was oozing of blood from socket which was found in 7 patients (7%) followed by grooving of root of the extracted tooth (3%), presence of inferior alveolar canal in the empty socket when socket was examined after irrigation (1%), grooving of root of the extracted tooth and oozing of blood from socket (1%), oozing of blood from socket and presence of inferior alveolar canal in the empty socket (1%).
A Chi-square and Fisher’s Exact test was conducted to assess the relationship between the radiological signs and intraoperative clinical assessment features. Among the 44 patients who showed interruption of the white line of the canal, 1 patient (2.3%) showed grooving of root of the extracted tooth and 3 patients (6.8%) showed oozing of blood from the socket (x2 = 0.143 p = 0.71). Among the 2 patients who showed diversion of the canal, 1 patient (50%) showed grooving of root of the extracted tooth (x2 = 15.492 p = < 0.001 statistically significant). Among the 10 patients who showed narrowing of the canal, 1 patient (10%) showed oozing of blood from the socket (x2 = 0.154 p = 0.70). The patient who showed root of the tooth just touching the upper outline of the neurovascular bundle (100%), showed presence of inferior alveolar canal in the empty socket when socket was examined after irrigation (x2 = 75.854 p = < 0.001 statistically significant). Among the 24 patients who showed root of the tooth superimposed on the neurovascular bundle, 1 patient (4.2%) showed grooving of root of the extracted tooth, 2 patients (8.3%) showed oozing of blood from the socket and 1 patient (4.2%) showed oozing of blood from socket and presence of inferior alveolar canal in the empty socket (x2 = 0.086 p = 0.77). The patient who showed darkening of root and interruption of white line (100%) showed oozing of blood from the socket (x2 = 13.420 p = < 0.001 statistically significant). Among the 3 patients who showed interruption of white line and narrowing of canal, 1 patient (33.3%) showed grooving of root of the extracted tooth and oozing of blood from socket (x2 = 32.660 p = < 0.001 statistically significant) (Tables 1, 2).
Table 1.
Relationship between the radiological signs and the intraoperative clinical assessment features
| Radiological signs | Overall | Grooving of root of the extracted tooth | Oozing of blood from the socket | Presence of inferior alveolar canal in the empty socket when socket is examined after irrigation | Grooving of root of the extracted tooth + oozing of blood from the socket | Oozing of blood from the socket + presence of inferior alveolar canal in the empty socket when socket is examined after irrigation | x2 value | p value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n | % | n | % | n | % | N | % | n | % | |||
| Interruption of white lines of the canal | 44 | 1 | 2.3 | 3 | 6.8 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0.143 | 0.71 |
| Diversion of the inferior alveolar canal | 2 | 1 | 50.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 15.492 | < 0.001* |
| Narrowing of the inferior alveolar canal | 10 | 0 | 0.0 | 1 | 10.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0.154 | 0.70 |
| Root of the tooth just touching the upper outline of the neurovascular bundle | 1 | 0 | 0.0 | 0 | 0.0 | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 | 75.854 | < 0.001* |
| Root of the tooth superimposed on the neurovascular bundle | 24 | 1 | 4.2 | 2 | 8.3 | 0 | 0.0 | 0 | 0.0 | 1 | 4.2 | 0.086 | 0.77 |
| Darkening of the root + interruption of white lines of the canal | 1 | 0 | 0.0 | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 13.420 | < 0.001* |
| Interruption of white lines of the canal + narrowing of the inferior alveolar canal | 3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 33.3 | 0 | 0.0 | 32.660 | < 0.001* |
Asterisk signifies p value
Table 2.
Intraoperative clinical assessment features
| Sl. no. | Feature | n | % |
|---|---|---|---|
| 1 | Grooving of root of the extracted tooth | 3 | 3.0 |
| 2 | Oozing of blood from the socket | 7 | 7.0 |
| 3 | Presence of inferior alveolar canal in the empty socket when socket is examined after irrigation | 1 | 1.0 |
| 4 | Grooving of root of the extracted tooth + oozing of blood from the socket | 1 | 1.0 |
| 5 | Oozing of blood from the socket + presence of inferior alveolar canal in the empty socket when socket is examined after irrigation | 1 | 1.0 |
Thus, it was found that out of the 100 patients showing definitive radiological signs of involvement of the third molar with the mandibular canal, only 12 had definitive clinical evidence of involvement.
Discussion
Surgical removal of impacted third molar is one of the most frequently performed oral surgical procedure. Most of the complications associated with this procedure are mild and reversible such as pain, swelling and trismus. Injury to the inferior alveolar canal is one of the most serious complications of this procedure which may lead to traumatic injuries, fibromas, scar tissue and mucocele formation on the mucosa [8]. Preoperative radiological assessment gives the surgeon an idea regarding the anatomic relationship of the canal and root of the impacted tooth, so that he can plan his surgery accordingly and if required he can modify the technique. It also allows the surgeon to inform the patient regarding the complications associated with the procedure [4].
The mandibular canal runs in the mandibular ramus and the body from mandibular foramen. It contains inferior alveolar artery, vein and nerve which supplies the root of the lower teeth. The nerve, artery and vein travel anteriorly in the mandibular canal up to mental foramen, below the root of the second premolar where the nerve divides into its terminal branches: the incisive and mental nerve [9]. In majority of the cases, the canal is symmetrical in both sides and single canal will be seen in each side. Sometimes supplemental canals can be present and if it is large enough, it can be seen in panoramic radiographs. These occur in three different configurations, the most common being duplicate canals commencing from a single mandibular foramen and the least common arising from two distinctly separate foramina [10].
The risk of inferior alveolar nerve injury associated with surgical extraction of mandibular third molar depends upon the anatomic proximity of the canal to the root of the tooth. Orthopantomographs are used routinely for the preoperative assessment of the impacted third molars. Several authors have identified high-risk radiological signs which may denote a close relationship between the canal and the tooth. The presence of one or more high-risk radiological signs in a patient increases the risk of inferior alveolar nerve injury. Conversely in the absence of any of these radiological signs, the chance of nerve injury is negligible. If one or more radiological signs are present in an orthopantomograph, the surgeon should advice additional imaging such as computed tomography which is more accurate in defining the proximity of the canal to the root. More accurate risk assessment may help the surgeon and patient in making the decision for or against removal of the tooth in question and in discussing alternative management strategies [11].
Seven radiological signs had been suggested as indicative of a close relationship between the mandibular third molar tooth and the inferior alveolar canal [2]. Four of these signs are seen on the root of the tooth and the other three are changes in the appearance of the inferior alveolar canal. The signs related to root are: (1) darkening of the root, (2) deflected roots, (3) narrowing of the root and (4) dark and bifid root. The signs related to canal are: (1) interruption of the white line, (2) diversion of the canal and (3) narrowing of the canal.
In a study done by Bell [5], it was found that based on surgical observations, 12% teeth had an intimate relation with the inferior alveolar nerve. This finding was similar to our study where 13% teeth showed intimate relation with the inferior alveolar canal clinically. Leung and Cheung [6] also found that the incidence of inferior alveolar nerve exposure was 13.5% after third molar surgery. Bell et al. [4] concluded that there is a significant difference between the preoperative radiologic assessments with a panoramic radiograph of the anatomy of third molars and their relationship with the neurovascular bundle and the findings at surgery which was similar to our study. According to Gomes et al. [7], the presence of a radiological sign of a close relationship with the mandibular canal was recorded in 159 of the 260 cases analysed. Nine (3.5%) of the 260 cases presented sensory complications, this percentage being higher among those in which there was judged to be a radiological sign of a close relationship with the mandibular canal than in those without such a sign. However, no significant association was shown to exist between the occurrence of the radiological sign and presence of changes in the inferior alveolar nerve (p = 0.94).
According to Bell [5], the most common radiological sign was superimposition (37%). Szalma et al. [8] found that the most common radiological sign was interruption of the superior cortical line (14%) followed by diversion of the canal (5.8%). Gomes et al. [7] found that the most common radiographic sign was darkening of the root (33.3%) followed by interruption of the white line (10.7%). In our study, the most common radiological sign was interruption of white line of the canal and it was found in 44 (44%) patients followed by root of the tooth superimposed on the neurovascular bundle (24%). The mandibular nerve was visualized in 6.5% of cases in the study done by Bundy et al. [12]. The frequency was much lower in our study (2%).
Szalma et al. [13] found that when darkening of root was present, it resulted in inferior alveolar nerve exposure in 45.8% cases. In our study, none of the cases showed signs of inferior alveolar nerve exposure when darkening was shown radiologically. The patient who showed darkening of root and interruption of white line (100%) showed oozing of blood from the socket (x2 = 13.420 p = < 0.001 statistically significant). According to Szalma et al. [12], 61% patients were female and inferior alveolar nerve injury was more in female patients. According to Gomes et al. [7], 73.8% patients were female. In our study, 64% patients were male and out of 13 patients who showed signs of inferior alveolar canal injury, 7 patients were female.
Leung and Cheung [6] found that 117 (65.7%) of the 178 third molars had only 1 of the 5 radiographic signs, 49 (27.5%) had 2 signs, 9 (5.1%) had 3 signs and 3 (1.7%) had 4 signs. No teeth presented with all 5 radiographic signs. In our study, out of 100 patients 84 patients had only 1 radiographic sign (84%), 16 patients had 2 radiographic signs (16%). No patients showed more than two radiographic signs.
According to Rood and Shehab [2], the most significant sign which related to nerve injury was diversion of the inferior alveolar canal (p < 0.001) followed by darkening of the root (p ~ 0.001); then interruption of the white line (p < 0.001). However, in our study the radiographic signs related to inferior alveolar nerve were root of the tooth just touching the upper outline of the neurovascular bundle (x2 = 75.854 p = < 0.001), interruption of white line and narrowing of canal together (x2 = 32.660 p = < 0.001), diversion of the canal (x2 = 15.492 p = < 0.001), darkening of root and interruption of white line together (x2 = 13.420 p = < 0.001).
de Almeida Barros et al. [14] in their study demonstrated in their study association between impacted third molars and position of the mandibular canal: a morphological analysis using cone—beam computed tomography that most third molars tilted mesially (n = 33), while the mandibular canal was positioned below the roots of the third molar in most cases (n = 73). Contact between the two was most likely when the mandibular canal was between (RR = 1.49; 95% CI 1.27–1.75, p < 0.001), or to the lingual side (RR = 1.49; 95% CI 1.27–1.75, p < 0.001) of the roots of the tooth. These outcomes indicate greater likelihood of contact between the canal and the roots when the canal is between and to the lingual side of the roots.
In a study done by Bozkurt and Gorurgoz [15] titled Detecting direct inferior alveolar nerve—Third molar contact and canal decorticalization by cone-beam computed tomography to predict postoperative sensory impairment, they found out that one-third molar extraction (0.8%) presented with postoperative permanent sensory impairment. No correlation between nerve injury and direct contact with the IAN or canal decorticalization on CBCT could be established.
Uzun et al. [16] conducted a study to assess the reliability of radiographic signs on panoramic radiographs to determine the relationship between mandibular third molars and the inferior alveolar canal. In total, 198 impacted third molars were included in this study. In 46 cases (23.2%), the inferior alveolar canal was exposed during extraction. Four radiographic signs—darkening of the root, narrowing of the root, narrowing of the inferior alveolar canal and diversion of the inferior alveolar canal—were associated with inferior alveolar canal exposure (p < 0.05). Concurrence of 2 or more of 7 radiographic signs increased the risk of inferior alveolar canal exposure (p < 0.001). The vertical relationship between impacted third molar and the inferior alveolar canal was found to be a risk indicator for inferior alveolar canal exposure (p < 0.001). No significant correlation was found between inferior alveolar canal exposure and inferior alveolar nerve damage (p = 0.148). To conclude, they suggested panoramic radiography is useful for assessing the risk of inferior alveolar canal exposure during impacted third molar extraction.
Conclusion
A true close relationship between the third molars and the mandibular canal increases the risk of inferior alveolar nerve injury, and an accurate evaluation of the relationship is essential to avoid the risk of surgery. The accuracy of the plain radiographs to diagnose an intimate relationship between the neurovascular bundle and the third molar root has its limitations. Surgeons should be aware of the limitations of the radiographic markers of panoramic radiography and should consider more detailed imaging in specific cases in which 1 or more radiographic marker is present.
Funding
None.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Approval
The current research was approved by the ethics committee of Vydehi Institute of Dental Sciences and Research Centre, Bangalore, India.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sukalpa Datta, Email: Dattasukalpa14@gmail.com.
Rayan Malick, Email: drrayan14@gmail.com.
Suresh Menon, Email: psurmenon@gmail.com.
M. E. Sham, Email: ehtaisham@yahoo.com
Veerendra Kumar, Email: drveeru07@gmail.com.
S. Archana, Email: archana.dr.s@gmail.com
References
- 1.Shujaat S, Abouelkheir HM, Al-Khalifa KS, Al-Jandan B, Marei HF. Preoperative assessment of relationship between inferior dental nerve canal and mandibular impacted third molar in Saudi population. Saudi Dental J. 2014;26:103–107. doi: 10.1016/j.sdentj.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rood JP, Shehab N. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28:20–25. doi: 10.1016/0266-4356(90)90005-6. [DOI] [PubMed] [Google Scholar]
- 3.Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;63:3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 4.Bell G, Rodgers J, Grime R, Edwards K, Hahn M, Dorman M, et al. The accuracy of dental panoramic tomographs in determining the root morphology of mandibular third molar teeth before surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:119–125. doi: 10.1067/moe.2003.16. [DOI] [PubMed] [Google Scholar]
- 5.Bell GW. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve radiological and surgical findings, and clinical outcome. Br J Oral Maxillofac Surg. 2004;42:21–27. doi: 10.1016/S0266-4356(03)00186-4. [DOI] [PubMed] [Google Scholar]
- 6.Leung YY, Cheung LK. Correlation of radiographic signs, inferior dental nerve exposure, and deficit in third molar surgery. J Oral Maxillofac Surg. 2011;69:1873–1879. doi: 10.1016/j.joms.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 7.Gomes AA, Vasconcelos BE, Silva ED, Caldas AF, Neto IP. Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J Oral Maxillofac Surg. 2008;66:256–259. doi: 10.1016/j.joms.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Szalma J, Lempel E, Jeges S, Szabo G, Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:294–302. doi: 10.1016/j.tripleo.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 9.Littner MM, Kajie I, Tamse A, Dicapua P, Aviv T. Relationship between the apices of the lower molars and mandibular canal-a radiographic study. Oral Surg Oral Med Oral Pathol. 1986;62:595–602. doi: 10.1016/0030-4220(86)90326-9. [DOI] [PubMed] [Google Scholar]
- 10.Nortje CJ, Farman AG, Grotepass FW (1977–1978) Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg 15:55–63 [DOI] [PubMed]
- 11.Blaeser BF, August MA, Donoff RB, Kaban LB, Dodson TB. Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg. 2003;61:417–421. doi: 10.1053/joms.2003.50088. [DOI] [PubMed] [Google Scholar]
- 12.Bundy MJ, Cavola CF, Dodson TB. Panoramic radiographic findings as predictors of mandibular nerve exposure following third molar extraction: digital versus conventional radiographic techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e36–e40. doi: 10.1016/j.tripleo.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Szalma J, Vajta L, Lempel E, Jeges S, Olasz L. Darkening of third molar roots on panoramic radiographs: is it really predominantly thinning of the lingual cortex? Int J Oral Maxillofac Surg. 2013;42(4):483–488. doi: 10.1016/j.ijom.2012.06.018. [DOI] [PubMed] [Google Scholar]
- 14.de Almeida Barros RQ, de Melo NB, de Macedo Bernardino Í, Arruda MALLA, Bento PM. Association between impacted third molars and position of the mandibular canal: a morphological analysis using cone-beam computed tomography. Br J Oral Maxillofac Surg. 2018;56(10):952–955. doi: 10.1016/j.bjoms.2018.10.280. [DOI] [PubMed] [Google Scholar]
- 15.Bozkurt P, Görürgöz C. Detecting direct inferior alveolar nerve—third molar contact and canal decorticalization by cone-beam computed tomography to predict postoperative sensory impairment. J Stomatol Oral Maxillofac Surg. 2020;121(3):259–263. doi: 10.1016/j.jormas.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 16.Uzun C, Sumer A, Sumer M. Assessment of the reliability of radiographic signs on panoramic radiographs to determine the relationship between mandibular third molars and the inferior alveolar canal. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;129(3):260–271. doi: 10.1016/j.oooo.2019.09.008. [DOI] [PubMed] [Google Scholar]