Introduction
The first case of maxillary sinus opacification and atelectasis was reported by Montgomery in 1964 [1]. It was only after 30 years that the term silent sinus syndrome was coined by Soparkar [2]. Silent sinus syndrome is also called as imploding antrum, chronic maxillary atelectasis. Silent sinus syndrome is a condition characterized by asymptomatic, spontaneous enophthalmos and hypoglobus with characteristic clinical and radiographic features, including ipsilateral maxillary sinus atelectasis or hypoplasia [2].
Case Report
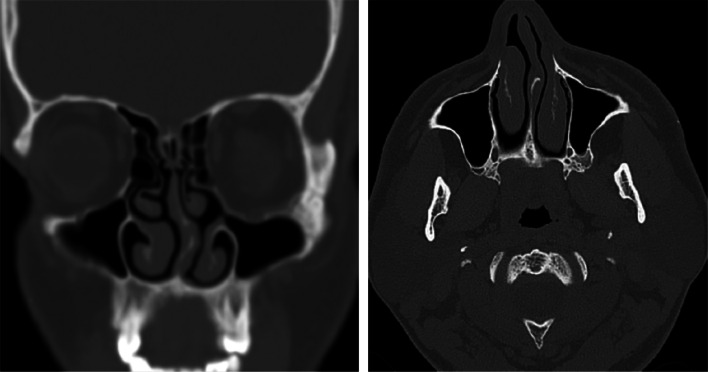
A 28-year-old patient reported to our craniofacial surgery outpatient department, Narayana Health with a complaint of “sinking left eyeball.” The patient reported that he was observing progressive, painless descent in his left eyeball since 8 months. He had no history of facial trauma and ophthalmic surgeries. Clinical examination revealed enophthalmos and vertical dystopia (Fig. 1a). Computed tomography of face showed complete opacification of the left maxillary sinus with occlusion of maxillary ostium, downward displacement of orbital floor with resorption, inward bowing of medial and lateral walls of the maxillary sinus (Fig. 2a, b). All of these had decreased the left maxillary sinus volume and increased left orbital volume. A diagnosis of silent sinus syndrome was made based on the clinical and imaging findings. The patient underwent functional endoscopic sinus surgery in which uncinectomy and opening of the maxillary sinus ostium were done. The patient was followed up periodically for 3 months and was found to have normal sinus drainage. The patient was then operated for correction of enophthalmos and dystopia. A subciliary approach was done to expose the orbital floor. Autogenous iliac bone graft was harvested and contoured to left orbital floor defect and was placed subperiosteally. Twelve months postoperative computed tomography of the face showed complete resolution in the opacification of the maxillary sinus and restoration of left orbital volume to its respective contralateral (Fig. 3). The patient was found to be complaint free at 12-month follow-up.
Fig. 1.

a Preoperative—left enophthalmos (horizontal lines passing through the corneal apices). b Postoperative—corrected left enophthalmos following reconstruction of the orbital floor 12 months after surgery (horizontal lines passing through the corneal apices)
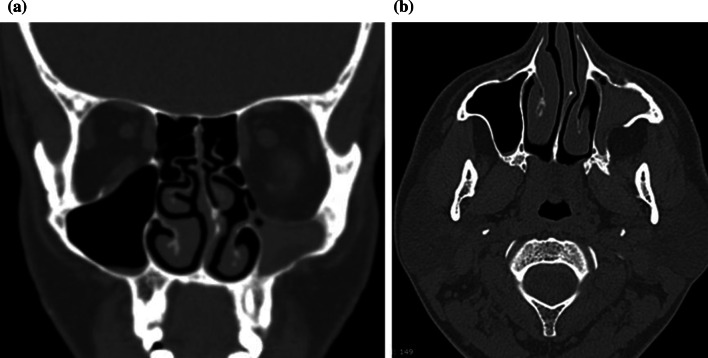
Fig. 2.
a Complete opacification of left maxillary sinus, downward displacement of left orbital floor with resorption. Reduced left maxillary sinus volume and enlargement of left orbit. b Inward bowing of medial and lateral walls of the maxillary sinus
Fig. 3.
Postoperative scan shows resolution of opacification of left maxillary sinus and restoration of left orbital volume
Discussion
Clinical features of silent sinus syndrome are typically patient reporting with spontaneous, painless, progressive enophthalmos and hypoglobus. The diagnosis of silent sinus syndrome can be made clinically, but it should be differentiated from other causes of spontaneous enophthalmos such as Parry–Romberg syndrome and linear scleroderma [3].
Radiographic signs of silent sinus syndrome are pathognomonic, and there is occlusion of the maxillary infundibulum, caused by lateral retraction of the uncinate process with apposition against the inferomedial aspect of the orbital wall [3]. The orbital floor is inferiorly displaced and increased concavity of the medial and lateral maxillary walls toward the antrum, the ultimate consequence of which is an overall decrease in maxillary sinus volume causing increased orbital volume and enophthalmos.
The following criteria have been defined for the diagnosis of silent sinus syndrome [4]:
Absence of significant sinus complaints, in particular no episodes of acute rhinosinusitis in the previous 6 months and no history of chronic rhinosinusitis,
Remodeling and inferior bowing of the maxillary roof/orbital floor as demonstrated on a coronal sinus CT scan,
No history of orbital trauma or enophthalmos of another etiology,
No documented congenital deformity or significant anatomic abnormality of the sinus and/or nasal cavity.
The exact etiology is unknown, but there are many theories put forth to explain the phenomenon. Initially, a developmental anomaly such as hypoplastic maxillary sinus was implicated. But now, it is attributed to have an acquired cause. The most widely accepted theory is chronic maxillary sinus obstruction with hypoventilation, a state that eventually causes negative pressure to develop within the sinus [1, 2]. After occlusion of the maxillary infundibulum, mucous begins to accumulate and eventually fills the sinus. The stagnant mucous incites a low-grade inflammatory response within the sinus and causes osteolysis of the sinus walls. The sinus walls, thinned by inflammation, are pulled into the sinus by the negative sinus pressure [5]. Typically, the periosteum is not affected.
Treatment of silent sinus syndrome has two distinct goals. The first goal is to regularize aeration of the maxillary sinus through normalization of drainage from the nasal cavity [9]. The second goal is to restore the normal orbital architecture. To reestablish a normal appearance, three deformities must be addressed: the hypoglobus, the enophthalmos, and the upper lid sulcus deformity (occurs in severe cases, absent in our case). The use of floor implants corrects the hypoglobus and greatly enhances the anterior projection of the eye [10]. In cases with significant upper lid sulcus depression, orbital floor implants alone may not be the optimal treatment. A pre-aponeurotic dermis fat graft may refine the esthetic outcome in these cases [11]. Alloplastic materials also have found a similar application for upper lid sulcus deformities [12].
Four different options have been described in the literature [2, 6–8]. They include:
A conservative approach without touching maxillary sinus or orbit, only treating diplopia with prisms
Antrostomy of the maxillary sinus
Antrostomy of the maxillary sinus and orbital floor reconstruction as single-staged procedure
Antrostomy of the maxillary sinus and orbital floor reconstruction as two-staged procedure
The initial management in this syndrome should be conservative. If this is inadequate, then normal sinus drainage is restored by enlarging the maxillary ostium with functional endoscopic sinus surgery. Surgical intervention to improve sinus aeration typically halts the progress of maxillary sinus contraction but does not restore sinus volume.
Historically, surgical treatment was accomplished by performing a Caldwell–Luc procedure. Endoscopic sinus surgery to create a wide maxillary antrostomy is now considered gold standard treatment of choice. But the surgeon should be careful about the abnormally low position of the globe in order to prevent orbital complications. More recently, balloon sinuplasty has been described as an alternative, less invasive procedure for the aeration of the maxillary sinus [13].
In patients with diplopia or severe cosmetic deformity, repair of the orbital floor with placement of a subperiosteal implant can be performed at the same time or after functional endoscopic sinus surgery [3]. No agreement exists on whether the orbital floor repair should occur simultaneously or in a staged procedure. Most reports suggest a 2-month waiting period between sinus surgery and orbital floor repair based on the idea that restoring sinus drainage and aeration may correct, at least in part, enophthalmos, and immediate floor repair could lead to an overcorrection [14].
The determinants of the vertical position of the globe should be evaluated carefully while planning orbital floor grafting. The determinants include integrity of the suspensory ligaments of Lockwood, intact orbital walls, volume of periorbital fat and extraocular muscles. Implants such as polyethylene, titanium mesh, silicone, and Medpore can be used or autologous bone may be contoured into a subperiosteal implant, which is placed on the orbital floor. This aids in the repositioning of the globe, thereby improving enophthalmos and eyelid position.
Conclusion
Silent sinus syndrome is a rare acquired condition characterized by painless, spontaneous, progressive enophthalmos and hypoglobus caused due to maxillary sinus hypoventilation due to blockage of the osteomeatal complex. Early diagnosis is paramount. If diagnosed early, surgical intervention such as functional endoscopic sinus surgery to enlarge the maxillary ostium is suffice. Late diagnosis would require correction of secondary orbital deformities.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The procedure performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the participant included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Prashanth Lowell Monis, Email: monislowell@gmail.com.
Malav H. Parikh, Email: dr.malavparikh@gmail.com
Hrishikesh Bhowmick, Email: hrishi007b55@gmail.com.
Kaushik Pai, Email: kaushikspai@gmail.com.
Samarth Shetty, Email: drsamarthshetty@gmail.com.
Paul C. Salins, Email: drpaul.salins@gmail.com
References
- 1.Montgomery WW. Mucocele of the maxillary sinus causing enophthalmos. Eye Ear Nose Throat Mon. 1964;43:41–44. [PubMed] [Google Scholar]
- 2.Soparkar CN, Patrinely JR, Cuaycong MJ, et al. The silent sinus syndrome. A cause of spontaneous enophthalmos. Ophthalmology. 1994;101(4):772–778. doi: 10.1016/s0161-6420(94)31267-x. [DOI] [PubMed] [Google Scholar]
- 3.Hourany R, Aygun N, Della Santina CC, et al. Silent sinus syndrome: an acquired condition. Am J Neuroradiol. 2005;26(9):2390–2392. [PMC free article] [PubMed] [Google Scholar]
- 4.Van der Meer E, Harris JB, Toohill RJ, et al. The silent sinus syndrome: a case series and literature review. Laryngoscope. 2001;111(6):975–978. doi: 10.1097/00005537-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Illner A, Davidson HC, Harnsberger HR, et al. The silent sinus syndrome: clinical and radiographic findings. Am J Roentgenol. 2002;178(2):503–506. doi: 10.2214/ajr.178.2.1780503. [DOI] [PubMed] [Google Scholar]
- 6.Iseli HP, Hafezi F, Mojon DS. Conservative treatment of vertical diplopia in a patient with silent sinus syndrome. Ophthalmologica. 2003;217(4):308–309. doi: 10.1159/000070641. [DOI] [PubMed] [Google Scholar]
- 7.Rose GE, Lund VJ. Clinical features and treatment of late enophthalmos after orbital decompression: a condition suggesting cause for idiopathic “imploding antrum” (silent sinus) syndrome. Ophthalmology. 2003;110(4):819–826. doi: 10.1016/S0161-6420(02)01994-2. [DOI] [PubMed] [Google Scholar]
- 8.Thomas RD, Graham SM, Carter KD. Management of the orbital floor in silent sinus syndrome. Am J Rhinol. 2003;17(2):97–100. doi: 10.1177/194589240301700206. [DOI] [PubMed] [Google Scholar]
- 9.Blackwell KE, Goldberg RA, Calcaterra TC. Atelectasis of the maxillary sinus with enophthalmos and midface depression. Ann Otol Rhinol Laryngol. 1993;102(6):429–432. doi: 10.1177/000348949310200604. [DOI] [PubMed] [Google Scholar]
- 10.Ando A, Cruz AA. Management of enophthalmos and superior sulcus deformity induced by the silent sinus syndrome. Aesthetic Plast Surg. 2005;29(2):74–77. doi: 10.1007/s00266-004-0118-1. [DOI] [PubMed] [Google Scholar]
- 11.Van Gemert JV, Leone CR., Jr Correction of a deep superior sulcus with dermis-fat implantation. Arch Ophthalmol. 1986;104(4):604–607. doi: 10.1001/archopht.1986.01050160160034. [DOI] [PubMed] [Google Scholar]
- 12.Bello VM, Levine MR. Superior sulcus deformity. Arch Ophthalmol. 1980;98(12):2215–2216. doi: 10.1001/archopht.1980.01020041067014. [DOI] [PubMed] [Google Scholar]
- 13.Kilty SJ. Maxillary sinus atelectasis (silent sinus syndrome): treatment with balloon sinuplasty. J Laryngol Otol. 2014;128(2):189–191. doi: 10.1017/S0022215113003538. [DOI] [PubMed] [Google Scholar]
- 14.Katz SE, Costin B, Levine MR. Silent sinus syndrome. In: Black E, Nesi F, Calvano C, Gladstone G, Levine M, editors. Smith and Nesi’s ophthalmic plastic and reconstructive surgery. New York: Springer; 2012. pp. 1047–1048. [Google Scholar]