Abstract
Objective
The aim of this study was to compare the piezotome versus surgical bur on postoperative edema and pain following open sinus lift surgery.
Materials and methods
This was a double-blinded split mouth randomized clinical trial. The subjects who were candidates for bilateral open sinus lifting in the posterior maxilla were included in this experiment. Each maxillary side was assigned randomly to one group, piezosurgery or surgical diamond bur for sinus lifting. Postoperative pain and edema were evaluated on the second and seventh days after the surgery, using the VAS scale. Data were analyzed by SPSS software.
Results
In this study, 20 subjects including 10 females (50%) and 10 males (50%) with a mean age of 50.87 ± 9.04 years participated. The mean duration of surgery in piezosurgery (240.13 ± 49.5 s) was significantly higher than the surgical bur technique (135.07 ± 43.53 s) (P < 0.001). Pain and edema were significantly decreased on the seventh day postoperatively compared to the second day in both group (P < 0.05). Pain and edema were similar between the two study groups on the second and seventh days after surgery.
Conclusion
The results of this study depicted that the piezosurgery clinical outcomes were similar to surgical bur following open sinus lift surgery.
Keywords: Pain, Edema, Piezosurgery, Open sinus lift
Introduction
Implant therapy has become one of the most common treatments for edentulous patients which can lead to an increase in beauty and functional satisfaction [1, 2]. Bone resorption as well as poor quality and quantity of bone in the posterior region of the maxilla can be a challenge in the success of implant placement [3–5].
The sinus lift is known as a gold-standard procedure for the reconstruction of vertically resorbed ridges in the edentulous posterior maxilla [4, 6].
Several surgical procedures have been used to perform open sinus lifting through the lateral wall, allowing the sinus Schneiderian membrane to be elevated [5, 7]. The conventional approach commonly used in clinics is the use of surgical diamond bur with the rotating handpiece [7, 8].
Piezosurgery is a new osteotomy technique using ultrasonic piezoelectric vibrations [2, 9–11]. Selective cutting is possible with various frequencies that work only on hard tissues [11–13]. This is especially important when working close to essential anatomical structures such as the nerve, vessel, dura matter, or Schneiderian membrane [11, 14].
Regarding the importance and widespread application of diverse devices in the open sinus lifting methods and the fact that few studies evaluate and compare the mentioned techniques [5, 7, 8, 15, 16], the authors conducted this study to compare the effects of piezosurgery and conventional surgical diamond bur on postoperative pain and edema following open sinus lift surgery.
Materials and Methods
Study Design
A protocol of this double-blinded randomized clinical trial was approved by the Ethics and Research Committee of our University. The guidelines of the Helsinki Declaration were followed in this research.
This study had a split-mouth design. It was carried out from October 2018 until December 2019 at our maxillofacial surgery department. All healthy (ASA I, II) non-smoker patients who were eligible for maxillary bilateral sinus augmentation were included in this study after written informed consent. The other conditions for inclusion were the absence of uncontrolled diabetes, systemic disorders, sinusitis as well as immune deficiency disorders and the history of drug abuse. All subjects had 1–4 mm of bone height (from the maxillary sinus floor to alveolar crest) in the treated posterior maxillary region bilaterally, which was confirmed by both pre-operative CBCT and clinical examination. The postoperative infection and wound dehiscence as well as lack of patient’s cooperation for follow-ups were the present research exclusion criteria.
Each patient’s maxillary side was assigned randomly to two groups, piezosurgery and surgical diamond bur groups for sinus lift surgery, using a random number table. Allocation concealment was performed using opaque sealed envelopes with sequential numbering. This was a double-blind study, so neither the statistical analyst nor the patients were aware of the surgical procedure. The codes continued to remain in a secure location until the end of the study.
The Protocol of Surgical Procedure
All the surgical procedures were carried out by a single surgeon using the same protocol in the edentulous posterior maxillary sites. A detailed history and routine laboratory tests as well as radiographic assessments were conducted in all patients preoperatively.
The surgical site was anesthetized using infiltration of lidocaine 2% with epinephrine 1/80,000 and a mucoperiosteal triangular flap was created in the maxillary posterior region and then it was completely elevated. The lateral window approach was used for maxillary sinus augmentation. In this technique, a bone window is generated in the lateral wall of the maxilla, through which the Schneiderian membrane is dissected from the alveolar process of the maxilla and pushed upward.
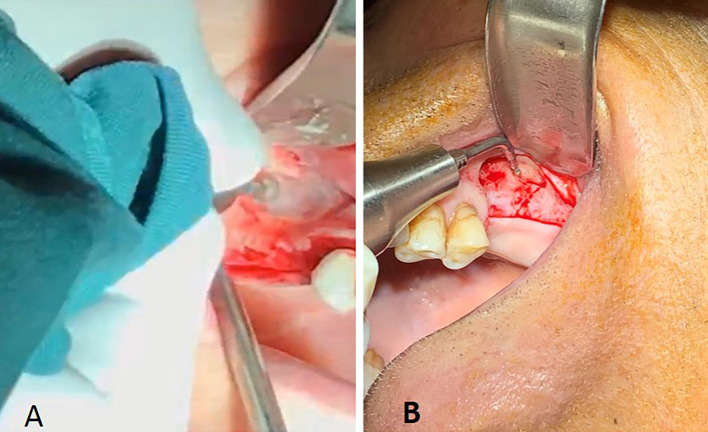
In this research, the osteotomy for maxillary sinus wall to create lateral window was performed by using the Piezosurgery system (Acteon, France) on one side and conventional rotary diamond round burs (NSK, Japan) for another side in a random fashion (Fig. 1). It should be noted that each side sinus lift surgery was performed separately and each patient had two separate surgical appointments with a 2-week time interval.
Fig. 1.
The lateral window osteotomy preparation using the conventional rotary diamond round bur on the right side (a), and the piezosurgery system on the left side of the maxilla (b)
The duration of lateral bone window preparation on each side with each technique was measured by the examiner with the aid of a chronometer.
Then, the sinus mucosa was dissected carefully and elevated conservatively using manual sinus lift curettes. The mineralized allograft bone substitute (Regen, Tehran, Iran) was subsequently inserted into the sinus cavity to maintain space for the formation of the new bone.
Finally, the mucoperiosteal flap was sutured with a 4-0 VICRYL (Soha, Iran) in a tension-free manner.
Throughout the postoperative healing phase, the occurrence of probable clinical complications such as acute or chronic sinus infection or bleeding was observed. To prevent any possible infection, patients received co-amoxiclav (Iranpakhsh, Tehran, Iran) antibiotic therapy (every 6 h postoperatively for 1 week). Additionally, 400 mg of ibuprofen (Iranpakhsh, Tehran, Iran) was administered to reduce edema, inflammation, and pain in all patients (every 8 postoperatively for 5 days). Moreover, Chlorhexidine mouthwash (Iranpakhsh, Tehran, Iran) was recommended twice a day for the next 2 weeks.
It should be noted that the dental implants were not placed simultaneously with the sinus lifting procedures, since the bone height was insufficient in our cases (1–4 mm). In other words, the sinus lift augmentation was accomplished alone and the dental implant placement was planned in the augmented bone ridge during the next surgical stage.
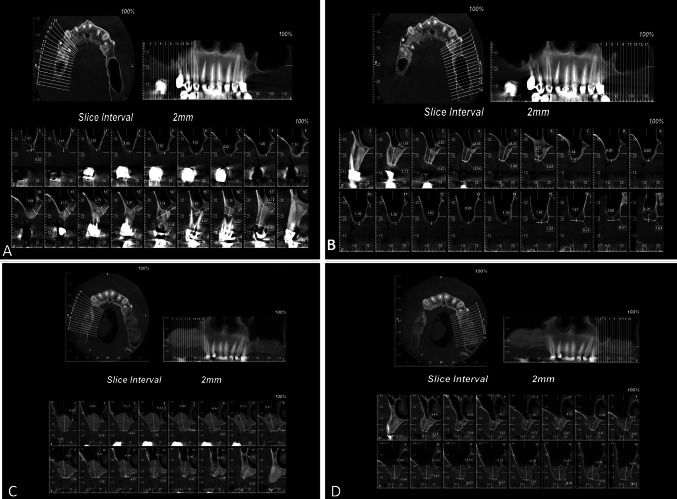
The cone beam computed tomography (CBCT) depicted the success of both techniques after 6 months (Fig. 2).
Fig. 2.
Pre-operative CBCT images (a diamond round bur, b piezotome), and postoperative radiographic images of both methods (c diamond round bur, d piezotome)
Variables and Data Collection
The patients’ age, sex, duration of lateral bone window preparation (in seconds), post-operative pain and swelling were recorded in specific checklists by the study examiner.
The predictor variable in this study was the technique used for lateral bone window preparation in sinus lift surgery and the outcomes were surgical duration as well as postoperative pain and edema severity on the second and seventh days following surgery, according to the VAS scale.
The visual analog scale (VAS) was used to assess postoperative pain severity. The VAS tool was a 10- cm ruler displaying 0 (no pain) on one end and 10 (intense pain) on the other. A VAS score lower than 3 indicated mild pain, a score of 3–7 indicated moderate pain, and a score higher than 7 indicated severe pain, regarding the literature (10).
Also, patient edema was measured subjectively on the second and seventh days after surgery using the Visual Analog Scale for edema (VAS edema criteria) introduced by Pasqualini et al. [17].
The above-mentioned VAS edema scale ranges from 0 to 5 [17]. There are no symptoms of swelling in the patient with grade 0, grade 1 has mild swelling, grade 2 has moderate swelling, and grade 3 has severe swelling. Grade 4 has extreme swelling with difficulty in chewing. However, VAS grade 5 has significant swelling with difficulty in opening the mouth.
The data results have been reviewed and the checklist and measurements have eventually been forwarded to the statistical expert.
Data Analyses
The statistical analysis was provided using version 20 of Statistical Product and Service Solutions (SPSS Inc., Chicago, IL). Qualitative variables were expressed as a percentage and quantitative variables as mean ± SD (standard deviation). We employed an independent t test and Mann–Whitney test. P value < 0.05 was considered statistically significant.
Results
In this study, 20 patients including 10 females (50%) and 10 males (50%) with a mean age of 50.87 ± 9.04 years with a range of 37–65 years who need a bilateral maxillary sinus lifting were included.
The mean duration of lateral bone window preparation for sinus lifting in was 240.13 ± 49.5 s the piezosurgery group and 135.17 ± 43.53 s in the conventional surgical diamond round bur group. The independent t-test manifested a significant difference between the two groups (P < 0.001).
Table 1 depicted that the mean pain scores of the postoperative second day observed by the patients in the piezosurgery group was less than conventional bur group (4.20 ± 1.37 vs 4.33 ± 1.23). However, there was no significant difference between the two groups, according to the Mann–Whitney test. Moreover, the mean postoperative pain scores in the 7th day were 3.47 ± 0.99 in the piezosurgery group and 3.47 ± 0.92 in conventional bur group without any significant difference (Table 1).
Table 1.
Comparison of postoperative pain between two study groups in different time intervals
| Group | Number | Mean ± SD | Range (min–max) | P value | |
|---|---|---|---|---|---|
| Postoperative pain on 2nd day | Piezotome | 20 | 4.20 ± 1.37 | 2–7 |
z = 0.58 P =0.564 |
| Conventional diamond round bur | 20 | 4.33 ± 1.23 | 3–7 | ||
| Postoperative pain on 7th day | Piezotome | 20 | 3.47 ± 0.99 | 2–5 | T = 0.00 |
| Conventional diamond round bur | 20 | 3.47 ± 0.92 | 2–5 | P = 1.00 |
T independent T test, Z Mann–Whitney test
According to the Table 2, the mean postoperative edema scores of the 2nd and 7th days observed by the patients in the piezosurgery and conventional bur groups had no significant differences.
Table 2.
Comparison of postoperative swelling and edema between two study groups in different time intervals
| Group | Number | Mean ± SD | Range (min–max) | P value | |
|---|---|---|---|---|---|
| Postoperative edema on 2nd day | Piezotome | 20 | 3.00 ± 0.65 | 2–4 |
z = 0.45 P = 0.655 |
| Conventional diamond round bur | 20 | 3.07 ± 0.70 | 2–4 | ||
| Postoperative edema on 7th day | Piezotome | 20 | 1.67 ± 0.82 | 1–4 |
z = 0.63 P = 0.527 |
| Conventional diamond round bur | 20 | 1.53 ± 0.64 | 1–3 |
Z Mann–Whitney test
Table 3 shows that in the piezosurgery group, the mean postoperative pain VAS score on the second day was 4.20 ± 1.37 which decreased to 3.47 ± 0.99 on the seventh day. It was statistically significant, according to the independent T test (P = 0.016). Furthermore, the mean postoperative edema VAS score on the second day was 3.00 ± 0.65 which decreased to 1.67 ± 0.82on the seventh day. It was statistically significant, regarding the Mann–Whitney test (P = 0.002).
Table 3.
Comparison of edema and pain between postoperative second and seventh days after sinus lift surgery in piezosurgery group
| Interval | Number | Mean ± SD | Range (min–max) | P value |
|---|---|---|---|---|
| Postoperative pain on 2nd day | 20 | 4.20 ± 1.37 | 2–7 |
T = 2.75 P = 0.016 |
| Postoperative pain on 7th day | 20 | 3.47 ± 0.99 | 2–5 | |
| Postoperative edema on 2nd day | 20 | 3.00 ± 0.65 | 2–4 |
z = 3.17 P = 0.002 |
| Postoperative edema on 7th day | 20 | 1.67 ± 0.82 | 1–4 |
T independent T test, Z Mann–Whitney test
Regarding Table 4, the mean pain and swelling scores in the conventional surgical group on the seventh postoperative day was significantly lower than compared to the second postoperative day (P = 0.006 and P < 0.001, respectively).
Table 4.
Comparison of edema and pain between postoperative second and seventh days after sinus lift surgery in conventional diamond round bur group
| Interval | Number | Mean ± SD | Range (min–max) | P value |
|---|---|---|---|---|
| Postoperative pain on 2nd day | 20 | 4.33 ± 1.23 | 3–7 |
z = 2.75 P = 0.006 |
| Postoperative pain on 7th day | 20 | 3.47 ± 0.92 | 2–5 | |
| Postoperative edema on 2nd day | 20 | 3.07 ± 0.70 | 2–4 |
z = 3.49 P < 0.001 |
| Postoperative edema on 7th day | 20 | 1.53 ± 0.64 | 1–3 |
Z Mann–Whitney test
It should be noted that all of our patients had full recovery and healing, with no signs or symptoms of maxillary sinus disease or perforation after the sinus augmentation procedures.
Discussion
The purpose of this clinical trial was to compare the piezotome versus surgical bur on postoperative edema and pain following open sinus lift surgery.
Sinus elevation is a popular surgical procedure that is performed to increase the bone volume in the maxillary sinus floor to enable the installation of implant fixtures, especially when the initial height of the alveolar bone cannot ensure the primary stability of the implants that are placed simultaneously [1, 2, 5]. The elevation and lifting of the maxillary sinus membrane and its grafting with bone substitutes have become a routine practice over the past 40 years [4, 18]. There are various methods of carrying out this operation [4, 5, 18, 19].
Regarding the increasing use of piezosurgery in many areas of oral and maxillofacial surgery and it is widely reported protective effects, the careful evaluation of this technique in the implant and sinus lift surgery is warranted [1, 14, 20].
Piezosurgery utilizes ultrasonic vibration which allows clean cutting with precise incisions, is a relatively new technique for osteotomy and osteoplasty [1, 14, 20].
Advantages of piezoelectric ultrasonic surgical instruments are the precise and accurate micrometric bone cuts as well as clear surgical fields without soft tissue damage [1, 20].
Regarding the literature, the use of piezosurgery decreases the chance of perforation of the sinus membrane [5, 8, 15, 16]. The outcomes of this study revealed that no perforation of the schneiderian membrane occurred in both methods, which may be attributed to the small sample size or surgeon’s experience. These results were in line with the Rador et al. study [8].
Moreover, the systematic review by Jordi et al. confirmed that the piezosurgery method takes longer time to perform compared with those with rotating instruments, but correlates with fewer postoperative complications [2], which was consistent with our study results. More recently, some other scholars supported the use of piezosurgery in cranial osteoplasty, also in high-risk cases, without any chance of dura mater perforation [12, 14, 21].
Based on our result, piezosurgery greatest weakness appears to be the time factor. The mean surgical duration in the piezo group (240.23 ± 49.5 s) was significantly longer than that of the conventional group (135.17 ± 43.53 s) (P < 0.001). This time difference between the two procedures is clinically small; however, the additional time may be needed for osteotomy by piezoelectric surgery can be up to five times greater in the site of larger bone density or thickness [5].
Pain and edema were similar between the two study groups on the second and seventh days after surgery, with no significant difference between them. Pain and edema were significantly decreased on the seventh day postoperatively compared to the second day in both piezosurgery and conventional diamond bur methods, respectively. These results were consistent with Rador, Rickert, Kotrikova, Barone, and Landes et al. studies [5, 8, 13, 16, 22].
As a matter of fact, piezosurgery generates less vibration and noise as it uses micro-vibrations, as opposed to macro-vibration and noise created by typical surgical burs and saws [5, 7, 10]. This makes the piezo system more manageable and provides greater control throughout the operation [2]. Heinemann et al. and Torrella et al. claimed that during the operation, piezosurgery provides the patient and the surgeon with greater comfort and causes less morbidity and complications compared to conventional procedures [23, 24].
A meta-analysis of randomized controlled studies (RCT) by Jiang et al. showed that the piezosurgery method, compared to those with rotating instruments, takes longer to conduct but associates with less postoperative complications such as post-operative pain and swelling [20]. According to our study, the pain was lower in the piezo group on the second postoperative day (4.20 + − 1.37) vs bur (4.33 + − 1.23), which was very similar to Jiang et al. result in this time interval.
Limitations and Suggestions
One of the present limitations of the experiment was the sample size, so we recommend selecting a larger sample size with a higher patient population to demonstrate the connection between the variables and the significance. The fact that this evaluation was a single-center research was another weakness. Further studies achieve better results if they gain more attention from the maxillofacial surgeons and compare different treatment centers.
Conclusion
The results of this study depicted that that in, the piezosurgery clinical outcomes were similar to conventional diamond bur following open sinus lift surgery, and could be a proper alternative to conventional diamond bur.
Funding
None. This study was self-funded.
Compliance with Ethical Standards
Conflict of Interest
The authors have no conflict of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shahakbari R, Eshghpour M, Mianbandi V, Pourgonabadi S, Tohidi E, Seyedi S, et al. The comparison of utilizing piezotome and surgical disc in ridge splitting of atrophic edentulous maxillary ridge. J Maxillofac Oral Surg. 2019 doi: 10.1007/s12663-019-01253-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu J, Hua C, Pan J, Han B, Tang X. Piezosurgery vs conventional rotary instrument in the third molar surgery: a systematic review and meta-analysis of randomized controlled trials. J Dent Sci. 2018;13(4):342–349. doi: 10.1016/j.jds.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Velazquez-Cayon R, Romero-Ruiz MM, Torres-Lagares D, Perez-Dorao B, Wainwright M, Abalos-Labruzzi C, et al. Hydrodynamic ultrasonic maxillary sinus lift: review of a new technique and presentation of a clinical case. Med Oral Patol Oral Cir Bucal. 2012;17(2):e271–e275. doi: 10.4317/medoral.17430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stern A, Green J. Sinus lift procedures: an overview of current techniques. Dent Clin N Am. 2012;56(1):219–233. doi: 10.1016/j.cden.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Barone A, Santini S, Marconcini S, Giacomelli L, Gherlone E, Covani U. Osteotomy and membrane elevation during the maxillary sinus augmentation procedure. A comparative study: piezoelectric device vs conventional rotative instruments. Clin Oral Implants Res. 2008;19(5):511–515. doi: 10.1111/j.1600-0501.2007.01498.x. [DOI] [PubMed] [Google Scholar]
- 6.Rahpeyma A, Khajehahmadi S. Open sinus lift surgery and the importance of preoperative cone-beam computed tomography scan: a review. J Int Oral Health JIOH. 2015;7(9):127–133. [PMC free article] [PubMed] [Google Scholar]
- 7.Delilbasi C, Gurler G. Comparison of piezosurgery and conventional rotative instruments in direct sinus lifting. Implant Dent. 2013;22(6):662–665. doi: 10.1097/id.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 8.Radvar MMM, Vaezi S, Shahi A. Clinical comparison of sinus lift via summers osteotomy and piezosurgery. J Mash Dent Sch. 2017;41(4):325–330. doi: 10.22038/jmds.2017.9891. [DOI] [Google Scholar]
- 9.Arakji H, Shokry M, Aboelsaad N. Comparison of piezosurgery and conventional rotary instruments for removal of impacted mandibular third molars: a randomized controlled clinical and radiographic trial. Int J Dent. 2016;2016:8169356. doi: 10.1155/2016/8169356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atieh MA, Alsabeeha NHM, Tawse-Smith A, Duncan WJ. Piezoelectric versus conventional implant site preparation: a systematic review and meta-analysis. Clin Implant Dent Relat Res. 2018;20(2):261–270. doi: 10.1111/cid.12555. [DOI] [PubMed] [Google Scholar]
- 11.Magrin GL, Sigua-Rodriguez EA, Goulart DR, Asprino L. Piezosurgery in bone augmentation procedures previous to dental implant surgery: a review of the literature. Open Dent J. 2015;9:426–430. doi: 10.2174/1874210601509010426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carini F, Saggese V, Porcaro G, Baldoni M. Piezolelectric surgery in dentistry: a review. Minerva Stomatol. 2014;63(1–2):7–34. [PubMed] [Google Scholar]
- 13.Landes CA, Stubinger S, Rieger J, Williger B, Ha TK, Sader R. Critical evaluation of piezoelectric osteotomy in orthognathic surgery: operative technique, blood loss, time requirement, nerve and vessel integrity. J Oral Maxillofac Surg. 2008;66(4):657–674. doi: 10.1016/j.joms.2007.06.633. [DOI] [PubMed] [Google Scholar]
- 14.Pereira CC, Gealh WC, Meorin-Nogueira L, Garcia-Junior IR, Okamoto R. Piezosurgery applied to implant dentistry: clinical and biological aspects. J Oral Implantol. 2014;40(Spec No):401–408. doi: 10.1563/aaid-joi-d-11-00196. [DOI] [PubMed] [Google Scholar]
- 15.Rahimi A. Comparison of piezosurgery and conventional hand-pieces in open sinus lifting surgery. Am J Oral Maxillofac Surg. 2018;5(1):29–41. [Google Scholar]
- 16.Rickert D, Vissink A, Slater JJ, Meijer HJ, Raghoebar GM. Comparison between conventional and piezoelectric surgical tools for maxillary sinus floor elevation. A randomized controlled clinical trial. Clin Implant Dent Relat Res. 2013;15(2):297–302. doi: 10.1111/j.1708-8208.2011.00364.x. [DOI] [PubMed] [Google Scholar]
- 17.Pasqualini D, Cocero N, Castella A, Mela L, Bracco P. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: a comparative study. Int J Oral Maxillofac Surg. 2005;34(1):52–57. doi: 10.1016/j.ijom.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 18.Silva LD, de Lima VN, Faverani LP, de Mendonca MR, Okamoto R, Pellizzer EP. Maxillary sinus lift surgery-with or without graft material? A systematic review. Int J Oral Maxillofac Surg. 2016;45(12):1570–1576. doi: 10.1016/j.ijom.2016.09.023. [DOI] [PubMed] [Google Scholar]
- 19.Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35(8 Suppl):216–240. doi: 10.1111/j.1600-051X.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 20.Jiang Q, Qiu Y, Yang C, Yang J, Chen M, Zhang Z. Piezoelectric versus conventional rotary techniques for impacted third molar extraction: a meta-analysis of randomized controlled trials. Medicine. 2015;94(41):1–7. doi: 10.1097/MD.0000000000001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pavlikova G, Foltan R, Horka M, Hanzelka T, Borunska H, Sedy J. Piezosurgery in oral and maxillofacial surgery. Int J Oral Maxillofac Surg. 2011;40(5):451–457. doi: 10.1016/j.ijom.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Kotrikova B, Wirtz R, Krempien R, Blank J, Eggers G, Samiotis A, et al. Piezosurgery–a new safe technique in cranial osteoplasty? Int J Oral Maxillofac Surg. 2006;35(5):461–465. doi: 10.1016/j.ijom.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 23.Heinemann F, Hasan I, Kunert-Keil C, Gotz W, Gedrange T, Spassov A, et al. Experimental and histological investigations of the bone using two different oscillating osteotomy techniques compared with conventional rotary osteotomy. Ann Anat. 2012;194(2):165–170. doi: 10.1016/j.aanat.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Torrella F, Pitarch J, Cabanes G, Anitua E. Ultrasonic ostectomy for the surgical approach of the maxillary sinus: a technical note. Int J Oral Maxillofac Implants. 1998;13(5):697–700. [PubMed] [Google Scholar]