Abstract
Background:
Recently developed multivariate sex-specific statistical models can predict anterior cruciate ligament (ACL) injury risk using various knee anatomical factors. However, screening tools able to identify individuals at an increased injury risk are unlikely to be developed based on these models given that sophisticated and time-consuming methods were used to measure those factors on research-grade resolution magnetic resonance images (MRIs).
Purpose:
To determine whether simpler methods, amenable to using clinical-grade resolution MRIs, can identify the same knee anatomical factors previously found to contribute to ACL injury risk using sophisticated methods and research-grade resolution images.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
High-resolution three-dimensional MRIs previously acquired from 87 primary, noncontact, grade III ACL-injured subjects and 87 uninjured matched control subjects for a series of published studies were downgraded to clinical-grade resolution images. The four knee anatomical factors found to contribute to ACL injury risk in females and in males in these published studies—femoral intercondylar notch width at the anterior outlet of the ACL (NW_O), posterior-inferior directed slope of the middle region articular cartilage surface of the tibial plateau’s lateral compartment (LatTibMCS), ACL volume, and tibial plateau’s lateral compartment meniscus-to-subchondral bone wedge angle (LatTibMBA)—were measured using clinical-grade resolution MRI-based methods. Stepwise multivariate conditional logistic regressions were used to identify the combinations of factors most highly associated with ACL injury risk in females and males separately.
Results:
The multivariate model that best predicted ACL injury risk in the female subjects included the LatTibMCS and the NW_O. For the male subjects, this model included the ACL volume and the LatTibMBA. These results corroborate the previously published results that reported models with the same knee anatomical factors to best predict injury risk in this group of young females and males.
Conclusion:
Simpler methods using MRIs downgraded to a clinical-grade resolution can identify the same knee anatomical factors previously found to significantly contribute to ACL injury risk using sophisticated methods and research-grade resolution MRIs.
Keywords: ACL injury, risk factors, knee anatomy
INTRODUCTION
In an effort to develop anterior cruciate ligament (ACL) injury prevention strategies and to identify those at an increased risk of injury and target them for intervention, numerous studies have focused on identifying the various risk factors associated with ACL injuries,18,19 including anatomical factors.1 Beynnon and colleagues,2,3,5,22–24,27 for instance, developed a multivariate evaluation of the knee joint morphology and its implication in ACL injury risk. They recruited primary noncontact ACL-injured subjects shortly after injury and 1:1 sex- and age-matched control subjects from the same high school or college sports team as the injured subject. In one of these studies by Sturnick et al.,23 four measures were associated with ACL injury risk—two for the male group and two different measures for the female group—from 32 individual knee geometry measures and by means of sex-specific multivariate analyses. The width of the femoral intercondylar notch at the anterior outlet of the ACL and the posterior-inferior directed slope of the middle region articular cartilage surface of the tibial plateau’s lateral compartment were identified as the best independent predictors of ACL injury in the female athletes; meanwhile ACL volume and the tibial plateau’s lateral compartment posterior meniscus-to-subchondral bone wedge angle were identified as such in the male athletes.23
Although knee geometry is largely characterized as a group of non-modifiable injury risk factors, sex-specific screening tools could be developed to identify individuals at an increased risk of sustaining an ACL injury. Thereafter, prevention strategies such as injury prevention training programs could target these individuals. Such screening tools need to be efficient both in terms of time and effort to be effective and worthwhile. Ideally, lower resolution magnetic resonance images (MRIs) would be used without sophisticated, time-consuming protocols to measure knee geometry. This raises the question of whether it is critical to use sophisticated, research-grade (high) resolution MRI-based methods, able to correct for internal tibial rotation, for instance, to determine ACL injury risk based on knee anatomy. In essence, can the four knee anatomical factors identified by Sturnick et al.23 be measured accurately and reliably and be identified as predictors of ACL injury using a clinical-grade resolution MRI-based method that does not standardize the internal-external rotational position of the tibia?
The purpose of this study was to determine whether simpler methods, using clinical-grade resolution MR images, can identify the knee anatomical factors previously found to be associated with noncontact ACL injury risk using sophisticated methods with research-grade resolution images.23 The MRIs from the male and female subjects from Sturnick et al.’s study23 were downgraded to a clinical-grade resolution and used for the present study. We hypothesized (1) that the width of the femoral intercondylar notch at the anterior outlet of the ACL and the posterior-inferior directed slope of the middle region articular cartilage surface of the tibial plateau’s lateral compartment would be identified as the best independent predictors of ACL injury in the female athletes and (2) that ACL volume and the tibial plateau’s lateral compartment posterior meniscus-to-subchondral bone wedge angle would be identified as the best independent predictors in the male athletes.
METHODS
Participants
The present investigation is a secondary analysis of MRI data collected between 2009 and 2012 from high school and college-level athletes for a series of previously published studies performed at the University of Vermont.2,3,5,22–24,27 The MRIs were deidentified before being shared with the investigators at the University of Michigan. This 1:1 matched case-control analysis included 87 subjects with a grade III, noncontact ACL injury and 87 uninjured control subjects selected from the same sport teams as their matched case subject (i.e., exposed to the same type of activity), also matched for age and sex (54 males and 120 females).23 All case subjects had suffered their first noncontact ACL injury at the time of study recruitment, and therefore had no history of prior ACL tears. Subjects with a prior or current ACL tear were not eligible to be included in the control group. To their knowledge, all subjects were free of any other knee pathologies (e.g., meniscus injury, chondral injury, etc.). Additional demographic information, such as age, height, weight, days between injury and MRI, can be found in a previous publication.2
Magnetic Resonance Imaging
Subjects underwent bilateral knee MRIs with the same Philips Achieva 3.0-T scanner (Philips Medical Systems) using an 8-channel dedicated knee coil (SENSE). Each knee, resting in full extension inside the coil, was scanned using two sequences with the following parameters: (1) sagittal-plane three-dimensional (3D) T1-weighted fast-field echo (FFE) scan (repetition time, 18 milliseconds; echo time, 8.1 milliseconds; slice thickness, 1.2 mm; pixel spacing, 0.31 × 0.31 mm); (2) sagittal-plane 3D proton density-weighted (PDW) scan (repetition time, 1000 milliseconds; echo time, 15 milliseconds; slice thickness, 0.7 mm; pixel spacing, 0.28 × 0.28 mm).23 For the ACL-injured subjects, MR images were acquired after injury but before surgery.23
The knee anatomical factors found by Sturnick and colleagues23 to be associated with ACL injury risk in males and females were measured using methods presented by this group23,24,27 but adapted to clinical-grade resolution MRIs based on previously published methods similar in nature.7,13 These anatomical factors were the following: (1) width of the femoral intercondylar notch at the anterior outlet of the ACL (also referred to as ‘femoral intercondylar notch width at the anterior outlet’ [NW_O]); (2) posterior-inferior directed slope of the middle region articular cartilage surface of the tibial plateau’s lateral compartment (also referred to as ‘lateral tibial compartment middle cartilage slope’ [LatTibMCS]); (3) tibial plateau’s lateral compartment posterior meniscus-to-subchondral bone wedge angle (also referred to as ‘lateral tibial compartment meniscus-bone angle’ [LatTibMBA]); and (4) ACL volume.
To obtain clinical-grade resolution MR images in the planes needed to measure the four knee morphological characteristics, the three-dimensional high-resolution images were imported in OsiriX software (www.osirix-viewer.com). For measurement of the femoral intercondylar notch width at the anterior outlet, the sagittal-plane 3D PDW scans were reconstructed to create oblique-coronal plane scans, which ran parallel to the longitudinal axis of the ACL as defined by the long axis parallel to the anterior border of the ACL.27 The scans were also resampled to a slice thickness of 2.2 mm, mimicking a slice thickness of 2.0 mm and a spacing between slices of 0.2 mm routinely used, or that can be easily acquired in sports medicine clinics. To measure the lateral tibial compartment middle cartilage slope and the lateral tibial compartment meniscus-bone angle, the sagittal-plane 3D T1-weighted FFE scans were resampled to a slice thickness of 2.2 mm. To measure the ACL volume, the sagittal-plane 3D T1-weighted FFE scans were reconstructed to create oblique-sagittal plane scans, which ran parallel to the longitudinal axis of the ACL. The scans were also resampled to a slice thickness of 2.2 mm. The in-plane resolution (i.e., pixel spacing) was not altered because it closely matched that of clinical-grade scans with a pixel size of 0.3 mm.
To measure the femoral intercondylar notch width at the anterior outlet, first, a reference line was defined on the oblique-coronal slice that ran along the anterior border of the ACL. This reference line was tangent to the posterior subchondral bone aspect of both femoral condyles.21,27 The femoral intercondylar north width was measured at the notch outlet anteriorly, parallel to the reference line, between the most distal and medial point of the lateral femoral condyle and the edge of the medial femoral condyle (Figure 1a).21,27 To measure the lateral tibial compartment middle cartilage slope, the sagittal-plane slice with the greatest concavity depth of the articular surface of the lateral tibial compartment was used. The middle cartilage slope was defined as the angle between a line connecting the superior-anterior and superior-posterior prominences of the middle articular cartilage surface region of the lateral tibial plateau and the longitudinal axis of the tibia, subtracted from 90° (Figure 1b).24 This longitudinal axis was defined as a straight line connecting the centers of two circles drawn within the proximal tibial on the central sagittal-plane image, as described by Hudek et al.13 For the lateral tibial compartment meniscus-bone angle, the angle between a line connecting the anterior and posterior most peaks of the subchondral bone of the lateral tibial plateau and a line connecting the anterior and superior-posterior most points of the posterior meniscus wedge were defined.24 This angle was measured on the same sagittal-plane image used to measure the lateral tibial compartment middle cartilage slope (Figure 1c). And finally, for the ACL volume, the perimeter of the ACL was traced in all slices in which the ACL was present (Figure 1d). The volume was calculated as the sum of each ACL surface area (as calculated by OsiriX) multiplied by the slice thickness (i.e., 2.2 mm).7,27
Figure 1.
Example measurements of the four anatomical factors examined herein. (a) femoral intercondylar notch width at the anterior outlet of the ACL (NW_O): measured at the notch outlet anteriorly, parallel to the reference line, between the most distal and medial point of the lateral femoral condyle (white circle) and the edge of the medial femoral condyle; (b) lateral tibial compartment middle cartilage slope (LatTibMCS): 90° minus the angle between a line connecting the superior-anterior and superior-posterior prominences of the middle articular cartilage surface region of the lateral tibial plateau (white circles) and the longitudinal axis of the tibia; (c) lateral tibial compartment meniscus-bone angle (LatTibMBA): angle between a line connecting the anterior and posterior most peaks of the subchondral bone of the lateral tibial plateau and a line connecting the anterior and superior-posterior most points of the posterior meniscus wedge (white circles); (d) ACL volume: ACL perimeter was traced in all slices in which the ACL was present.
All measurements were performed on deidentified MR images of the uninjured knees of the ACL-injured subjects and on the corresponding left/right knee of their matched control subjects.23 All measurements were performed by a single investigator (E.K.N.), who remained blinded to the ACL injury status of each participant. Intra-observer reliability of the measurements was assessed by measuring the outcome variables three times, on nonconsecutive days, in a subset of 10 participants and by calculating the intraclass correlation coefficient (ICC). All measurements showed excellent intraobserver reliability,14 with ICCs of 0.97 for the femoral notch width at the anterior outlet of the ACL, 0.94 for the lateral tibial compartment middle cartilage slope, 0.97 for the lateral tibial compartment meniscus-bone angle, and 0.93 for the ACL volume. Interobserver reliability of the measurements was also assessed in the same subset of participants by having two additional examiners (for a total of three examiners) measure each of the outcome variables. Interclass correlation coefficients (ICCs) revealed good interobserver reliability for the femoral notch and lateral tibial compartment measurements (ICCs: NW_O=0.85; LatTibMCS=0.84; LatTibMBA=0.80) and moderate reliability for the ACL volume (ICCs: 0.61).14
Statistical Analysis
Univariate conditional logistic regressions were performed to calculate the sex-specific odds ratios associated with ACL injury risk and to determine whether our clinical-grade resolution MRI-based method could identify the four knee morphologic characteristics as strongly related to risk, as found by Sturnick et al.23 The four morphologic variables were also analyzed together with two stepwise multivariate conditional logistic regressions to identify the combinations of independent knee geometric factors most highly associated with ACL injury risk for the female athletes and male athletes separately. Only variables with p < 0.05 were included in the final ‘male’ and ‘female’ models.23
RESULTS
For the female group of subjects, the series of univariate conditional logistic regressions revealed that each of the four knee morphological measures had a significant relationship with risk of suffering a noncontact ACL injury (Table 1). The multivariate model that best predicted ACL injury risk in the female subjects included the lateral tibial compartment middle cartilage slope and the femoral intercondylar notch width at the anterior outlet (Table 2). For a 1-degree increase from the mean lateral tibial compartment middle cartilage slope, there was a 31.8% increase in ACL injury risk. And for a 1-millimeter decrease from the mean femoral intercondylar notch width at the anterior outlet, there was a 33.5% increase in ACL injury risk. The results of our multivariate regression model corroborate those of Sturnick et al.23 who reported a multivariate model highly predictive of ACL injury risk in females that included the same variables, with a 32.4% and 49.9% increase in risk for a 1-degree increase in the lateral tibial compartment middle cartilage slope and a 1-millimeter decrease in the femoral intercondylar notch width at the anterior outlet, respectively (Table 2).
Table 1.
Univariate conditional logistic regression models for femalesa with comparison to data published in Sturnick et al.23
| Variable (unit change) | Odds Ratio (95% CI) | p value | % Increase in ACL Injury Riskb |
|---|---|---|---|
|
| |||
| NW_O (1 mm) | |||
| Present study | 0.780 (0.655–0.928) | 0.005 | 28.2% |
| Sturnick et al.23 | 0.692 (0.557–0.859) | <0.01 | 44.5% |
| LatTibMCS (1 deg) | |||
| Present study | 1.306 (1.136–1.501) | <0.001 | 30.6% |
| Sturnick et al.23 | 1.303 (1.142–1.486) | <0.001 | 30.3% |
| LatTibMBA (1 deg) | |||
| Present study | 0.829 (0.738–0.933) | 0.002 | 20.6% |
| Sturnick et al.23 | 0.863 (0.781–0.953) | 0.004 | 15.9% |
| ACL volume (100 mm3) | |||
| Present study | 0.829 (0.707–0.970) | 0.020 | 20.6% |
| Sturnick et al.23 | 0.850 (0.719–1.005) | >0.05 | 17.6% |
ACL: anterior cruciate ligament; LatTibMBA: lateral tibial compartment meniscus-bone angle; LatTibMCS: lateral tibial compartment middle cartilage slope; NW_O: femoral intercondylar notch width at the anterior outlet of the ACL.
Regression models were performed using the uninjured leg of ACL-injured subjects and the corresponding knee of control subjects. Odds ratios and associated 95% confidence intervals (CIs) describe the effects of a unit increase from the mean for each variable on risk of suffering a noncontact ACL injury.
Percentage (%) increase in ACL injury risk for a unit increase from the mean for the LatTibMCS and for a unit decrease from the mean for the NW_O, the LatTibMBA, and the ACL volume.
Bolded values represent statistical significance.
Table 2.
Best-fit multivariate risk model for femalesa with comparison to data published in the study Sturnick et al.23
| Variable (unit change) | Odds Ratio (95% CI) | p value | % Increase in ACL Injury Riskb |
|---|---|---|---|
|
| |||
| LatTibMCS (1 deg) | |||
| Present study | 1.318 (1.137–1.529) | 0.0003 | 31.8% |
| Sturnick et al.23 | 1.324 (1.135–1.546) | 0.0004 | 32.4% |
| NW_O (1 mm) | |||
| Present study | 0.749 (0.605–0.925) | 0.007 | 33.5% |
| Sturnick et al.23 | 0.667 (0.505–0.881) | 0.004 | 49.9% |
Includes measures of lateral compartment middle cartilage slope (LatTibMCS) and femoral intercondylar notch width at the anterior outlet of the ACL (NW_O). A multivariate conditional logistic regression was performed using the uninjured leg of ACL-injured subjects and the corresponding knee of control subjects. Odds ratios and associated 95% confidence intervals (CIs) describe the effects of a unit increase from the mean for each variable on risk of suffering a noncontact ACL injury.
Percentage (%) increase in ACL injury risk for a unit increase from the mean for the LatTibMCS and for a unit decrease from the mean for the NW_O.
For the male group of subjects, the series of univariate conditional logistic regressions revealed that three of the four knee morphological measures had a significant association with ACL injury risk—femoral notch width at the anterior outlet of the ACL, ACL volume, and the lateral tibial compartment meniscus-bone angle (Table 3). The multivariate model that best predicted ACL injury risk in the male subjects included the ACL volume and the lateral tibial compartment meniscus-bone angle (Table 4). For a 100-mm3 decrease from the mean ACL volume, there was a 42.5% increase in ACL injury risk. And a 1-degree decrease from the mean lateral tibial compartment meniscus-bone angle, there was a 54.3% increase in ACL injury risk. The results of this multivariate regression model also corroborate those of Sturnick et al.23 who reported a multivariate model highly predictive of ACL injury risk in males that included the same variables, with a 43.5% and 23.3% increase in risk for a 100-mm3 decrease in ACL volume and a 1-degree decrease in the lateral compartment meniscus-bone angle, respectively (Table 4).
Table 3.
Univariate conditional logistic regression models for malesa with comparison to data published in the study of Sturnick et al.23
| Variable (unit change) | Odds Ratio (95% CI) | p value | % Increase in ACL Injury Riskb |
|---|---|---|---|
|
| |||
| NW_O (1 mm) | |||
| Present study | 0.741 (0.550–0.998) | 0.048 | 35.0% |
| Sturnick et al.23 | 0.722 (0.528–0.986) | <0.05 | 38.5% |
| LatTibMCS (1 deg) | |||
| Present study | 1.214 (0.989–1.490) | 0.063 | 21.4% |
| Sturnick et al.23 | 1.054 (0.895–1.241) | 0.53 | 5.4% |
| LatTibMBA (1 deg) | |||
| Present study | 0.718 (0.529–0.974) | 0.033 | 39.3% |
| Sturnick et al.23 | 0.900 (0.782–1.036) | 0.14 | 11.1% |
| ACL volume (100 mm3) | |||
| Present study | 0.749 (0.587–0.955) | 0.020 | 33.5% |
| Sturnick et al.23 | 0.767 (0.610–0.964) | <0.05 | 30.4% |
ACL: anterior cruciate ligament; LatTibMBA: lateral tibial compartment meniscus-bone angle; LatTibMCS: lateral tibial compartment middle cartilage slope; NW_O: femoral intercondylar notch width at the anterior outlet of the ACL.
Regression models were performed using the uninjured leg of ACL-injured subjects and the corresponding knee of control subjects. Odds ratios and associated 95% confidence intervals (CIs) describe the effects of a unit increase from the mean for each variable on risk of suffering a noncontact ACL injury.
Percentage (%) increase in ACL injury risk for a unit increase from the mean for the LatTibMCS and for a unit decrease from the mean for the NW_O, the LatTibMBA, and the ACL volume.
Bolded values represent statistical significance.
Table 4.
| Variable (unit change) | Odds Ratio (95% CI) | p value | % Increase in ACL Injury Riskb |
|---|---|---|---|
|
| |||
| ACL volume (100 mm3) | |||
| Present study | 0.702 (0.522–0.945) | 0.019 | 42.5% |
| Sturnick et al.23 | 0.697 (0.523–0.928) | 0.013 | 43.5% |
| LatTibMBA (1 deg) | |||
| Present study | 0.648 (0.438–0.959) | 0.030 | 54.3% |
| Sturnick et al.23 | 0.811 (0.666–0.988) | 0.038 | 23.3% |
Includes measures of the ACL volume and the lateral tibial compartment meniscus-bone angle (LatTibMBA). A multivariate conditional logistic regression was performed using the uninjured leg of ACL-injured subjects and the corresponding knee of control subjects. Odds ratios and associated 95% confidence intervals (CIs) describe the effects of a unit increase from the mean for each variable on risk of suffering a noncontact ACL injury.
Percentage (%) increase in ACL injury risk for a unit decrease from the mean for each variable.
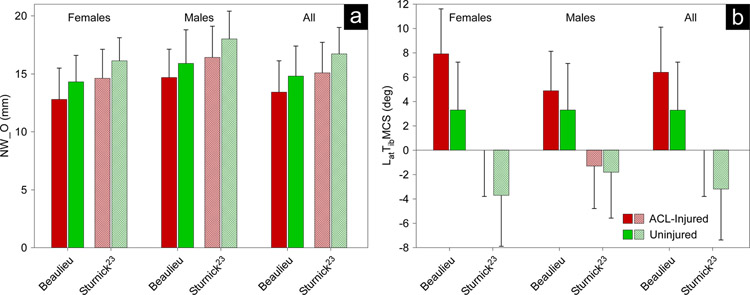
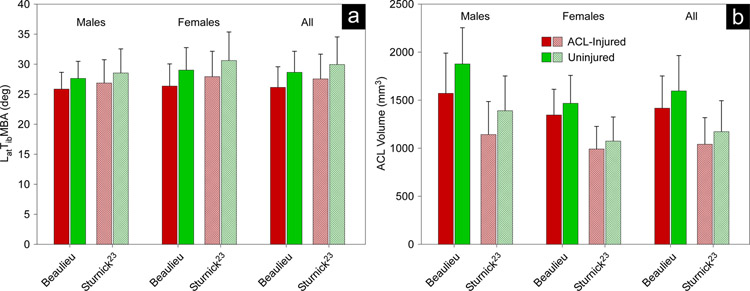
In terms of the measurement data, various similarities and differences were found between those presented herein and those of Sturnick et al.23 (Figures 2–3). The femoral intercondylar notch width data of the present study were less than 2 mm lower (approximately a 11% difference), on average, (Figure 2a) and the lateral tibial compartment meniscus-bone angle about one degree lower (approximately a 5% difference), on average (Figure 3a), than those reported by Sturnick et al.23 Our data of the lateral tibial compartment middle cartilage slope and the ACL volume, however, appeared to be systematically greater. The lateral tibial compartment middle cartilage slope of the present study was, on average, 6.5 degrees greater than those of Sturnick et al.23 (Figure 2b); meanwhile we measured the ACL volume as 401 mm3 greater (approximately 36% greater), on average (Figure 3b).
Figure 2.
Bar graphs of the mean (and one standard deviation by error bars) values of the knee morphological measures found to best predict ACL injury risk in the female subjects as determined by a multivariate conditional logistic regression model: (a) NW_O; (b) LatTibMCS. Comparisons of data of ACL-injured and uninjured female, male, and all athletes from the present study and those published in the study of Sturnick et al.23 ACL: anterior cruciate ligament; LatTibMCS: lateral tibial compartment middle cartilage slope; NW_O: femoral intercondylar notch width at the anterior outlet of the ACL.
Figure 3.
Bar graphs of the mean (and one standard deviation by error bars) values of the knee morphological measures found to best predict ACL injury risk in the male subjects as determined by a multivariate conditional logistic regression model: (a) LatTibMBA; (b) ACL volume. Comparisons of data of ACL-injured and uninjured male, female, and all athletes from the present study and those published in the study of Sturnick et al.23 ACL: anterior cruciate ligament; LatTibMBA: lateral tibial compartment meniscus-bone angle.
DISCUSSION
The goal of the present study was to determine whether knee anatomical factors previously found to be associated with increased risk of suffering ACL injury using sophisticated methods with research-grade resolution MR images23 can also be identified with simpler methods—methods capable of being used with clinical-grade resolution images. Our results reveal that, indeed, simpler clinic-friendly methods can identify such knee anatomical factors associated with the risk of suffering a noncontact ACL injury for both males and females. Supporting our hypothesis and consistent with Sturnick et al.,23 the width of the femoral intercondylar notch at the anterior outlet of the ACL and the posterior-inferior directed slope of the middle region articular cartilage surface of the tibial plateau’s lateral compartment best predicted injury risk in the female athletes, and ACL volume and the tibial plateau’s lateral compartment posterior meniscus-to-subchondral bone wedge angle best predicted risk in the male athletes.
In addition to our best fitting statistical models to predict primary noncontact ACL injury matching those of Sturnick at al.,23 various similarities and differences were found in the measurement data between studies. The data of the femoral intercondylar notch width at the anterior outlet of the ACL and the lateral tibial compartment meniscus-bone angle were remarkably similar (Figure 2a and 3a). However, seemingly systematic differences were present in the data of the lateral tibial compartment middle cartilage slope and the ACL volume (Figure 2b and 3b). These systematic differences in the lateral tibial compartment middle cartilage slope data between studies can most likely be attributed to substantial differences in the definition of the longitudinal axis of the tibia given that the slope is calculated in reference to this axis. We approximated the longitudinal axis with a straight line that connected the centers of two circles drawn within the proximal tibial on a sagittal-plane MRI slice at the center of the lateral tibial plateau.13 This method has been used extensively4,12,15,16 and can provide a relatively quick approximation of the longitudinal tibial axis with clinical-grade resolution MR images. On the other hand, Sturnick et al.24 defined a tibial coordinate system based on bony geometry and landmarks, with the longitudinal axis of the tibia defined by a line connecting the centroids of a distal and proximal outline of tibial cortical bone in the transverse plane. This method is more labor-intensive and requires three-dimensional, research-grade resolution MR images, but in return, it yields an accurate longitudinal axis orientation. The differences in ACL volume data may be due, in part to examiner variability in identifying ACL tissue, and in part to differences in the MRI slice thickness. The outline of the ligament can be ambiguous at times, especially near the attachment sites and on the slices displaying the medial and lateral edges of the ligament. Manual segmentation of the ACL, therefore, can include an element of subjectivity, which was evident in the reliability data of the measurement. The ICCs of both this study and that of Sturnick et al.23,27 indicated excellent intra-examiner reliability (< 0.90), but only moderate inter-examiner reliability (0.50–0.75) for ACL volume. Furthermore, our clinical-grade resolution MR images had a thickness of 2.2 mm compared with 1.2 mm for the MR images used by Sturnick et al.23 Given that the ACL volume is calculated as the ligament area outlined in each MRI slice multiplied by the slice thickness, volume data may have been overestimated in the present study. It appears, however, to be a consistent and somewhat systematic overestimation, as with the lateral tibial compartment middle cartilage slope data.
Several other noteworthy differences in the methods used to measure the various knee morphological factors exist between our study and that of Sturnick et al.23 Measurements of the lateral tibial compartment middle cartilage slope and the lateral tibial compartment meniscus-bone angle differed the most. With research-grade (high) resolution three-dimensional MRI scans, Sturnick et al.24 used sophisticated and time-consuming methods that consisted of: (1) manually segmenting the tibial plateau subchondral bone, articular cartilage surface, and posterior aspect of the meniscus; (2) transforming the data points of each segmented structure to a tibial coordinate system to correct for varying tibia orientations in the MRI scanner; (3) interpolating the data points in the sagittal plane of the tibial coordinate system and along its mediolateral direction, thereby increasing the spatial resolution; (4) measuring the concavity depth of the cartilage profile of the lateral tibial compartment in each sagittal-plane slice; and finally (5) on the slice of maximum concavity depth, measuring the middle cartilage slope and the meniscus-bone angle in the lateral tibial compartment.23,24 In contrast, our clinical-grade resolution MRI-based method consisted of finding the sagittal-plane slice with the greatest concavity depth of the articular surface of the lateral tibial compartment, and then measuring the middle cartilage slope and the meniscus-bone angle on that slice, including approximating the longitudinal axis of the tibia as discussed in the previous paragraph. Therefore, the methods used herein do not allow for the correction of variable tibia orientation in the MRI scanner, use a mere approximation of the longitudinal axis of the tibia, and are based on images of lower spatial resolution.
To measure the femoral intercondylar notch width at the anterior outlet of the ACL and the ACL volume, we replicated the exact methodologies used by Sturnick et al.23,27, but with MR images of different parameters. As described in the “Methods” section, we downgraded the images used by Sturnick et al.23,27 from a slice thickness of 1.2 mm to a thickness of 2.2 mm. Also, to quantify the ACL volume, we used oblique-sagittal plane images (running parallel to the longitudinal axis of the ACL); whereas Sturnick et al.23,27 used pure sagittal plane images. Despite these methodological differences, our methods were also able to identify the knee morphological factors associated with increased risk of ACL injury.
The ability to do so with simpler, clinic-friendly methods has tremendous implications for injury risk screening and injury prevention. For an injury risk screening tool to become successful and widely used, it must be effective and efficient in terms of both time and effort. Beynnon and colleagues were able to identify, with a multivariate approach, several knee anatomic factors able to predict ACL injury risk in a series of studies.2,3,5,22–24,27 Although their sophisticated and robust methods appear to be effective, they are time- and labor-intensive, not practical to measure in a clinical setting, and have limited application with clinical-grade resolution MRIs. For instance, it took them approximately 145 minutes to perform all four measurements on a single knee, which amounts to nearly six times longer in comparison to the simpler methods used for this study that took 25 minutes, on average. This is in addition to the extra time to acquire the MRIs, which we estimated to be approximately 33% more time (22.6 min vs. ~17 min per knee). Therefore, they could not realistically be used for injury screening purposes in the clinical setting. The simpler methods presented herein could be used for such purposes. We do recognize that the simpler methods, though used with clinical-grade resolution MRIs, can take some time to perform and may not be able to be applied en masse. Perhaps these methods could be automated with techniques such as deep learning9 to improve their efficiency and reliability, thereby increasing their widespread implementation. Thereafter, injury prevention strategies could target the individuals at an increased risk of sustaining an ACL injury. Prior to developing injury risk screening tools, however, it is important to apply the sex-specific multivariate injury risk models identified by Sturnick et al.23, and identified in the present study, to a different group of primary noncontact ACL-injured subjects and matched uninjured control subjects to validate the models. Specifically, this future work could establish the models’ sensitivity and specificity, as well as their receiver operating characteristic (ROC) curve to illustrate their ability to identify females and males at increased risk of ACL injury. This would also assist in establishing limits of acceptability for the four knee anatomical factors, outside of which one would be at high risk of sustaining a noncontact ACL injury. Currently, no such limits exist, with more research needed to establish them. Although individual efforts have been made toward this goal,8 consolidating data from various studies to establish limits of acceptability is difficult, if not impossible, due to the great methodological variability between studies. For instance, investigators have utilized different variations of some factors (e.g., lateral tibial slope) and different techniques to measure a specific factor and have made the measurements in different populations—all methodological differences that can affect the absolute values measured for each factor, and thereby contribute to different ‘normal’ and ‘at-risk’ ranges of values in terms of ACL injury risk.
The strength and limitations of our study should be acknowledged. First, a strength is that all the methods and measurements described in the “Methods” section for this secondary study were performed at a different institution and by a different set of investigators than the original Sturnick et al. study23. The fact that our results corroborate those of the primary study lends confidence in the results. Second, another strength is that the study design of the Sturnick et al. study,23 and therefore of the present study, overcame many of the pitfalls of previous studies. Often, anatomical factors for ACL injury risk have been examined independently with variations in study designs and control group characteristics,8,10,20,26 with poor case-control matching,10,26 in the injured knee of the case subjects8,26 despite known knee geometry changes following ACL injury3 and in a combined group of men and women10,20 despite known disparities in knee joint morphology between sexes.6,11,15,17,25 In contrast, Sturnick et al.23 matched the case subjects with control subjects from the same sports team, thus controlling for exposure to activity types, training, playing conditions, environmental conditions, coaching, and other extrinsic risk factors.3 They also developed a method to overcome the lack of standardized orientation of the knee during MRI scans by modeling the entire cartilage and bony 3D surface of the proximal tibia in an anatomical coordinate system.3 Both knees of the ACL-injured athletes were found to display more internal tibial rotation than the matched control athletes during acquisition of the MRI scans.2 And the geometric measures were acquired from the MRI of the uninjured knee of the ACL-injured subjects. Third, a limitation was that only the four factors identified by Sturnick et al.23 to be significantly associated with ACL injury were included in this study and therefore considered for inclusion in our multivariate regression models, unlike Sturnick et al.23 who considered eight variables for their models (down from 32 variables to avoid including correlated variables). Therefore, our best fitting models to predict ACL injury risk may have been different had we included all eight variables in this study. Considering how closely our data match those of Sturnick et al.,23 we believe this to be unlikely. Fourth, there was a substantial difference in sample size between the female and male groups of athletes (120 females vs. 54 males), which could have influenced the various factors found to significantly predict ACL injury risk for each group. It is possible that a larger sample size in the male group could reveal additional associations between knee morphology and injury risk. However, the fact that two knee anatomic factors predicted ACL injury risk in the smaller size group of male athletes, but not in the female athletes, reinforces the conclusion that these factors can significantly predict ACL injury risk in males. Fifth, actual clinical MRIs were not used. Instead, clinical-grade MRIs were produced digitally by downgrading the research-grade MRIs. However, the digital downgrade procedure yielded MR images with parameters that closely matched those of scans obtained in sports medicine clinics. Also, by measuring the anatomical factors on the same set of MRIs used in the Sturnick et al. study, we eliminated numerous potential confounding factors that could have generated erroneous differences between our results and those of Sturnick et al.23 Such confounding factors include placement of the knee within the scanner, alignment of the scanner’s coordinate system with that of the knee, differences in soft tissue morphology if scans are done on different days, and differences between samples of subjects if MR images are obtained from a different sample population, among others. And finally, the implementation of injury risk screening tools based on knee anatomical risk factors require that MRIs be acquired prospectively. The feasibility of such screening tools may be questioned, therefore, considering the cost associated with MRI acquisition. With technological advancements being made in the field of imaging, however, costs are decreasing.
CONCLUSION
Simpler methods using MRIs downgraded to a clinical-grade resolution can identify the same knee anatomical factors previously found to significantly contribute to ACL injury risk using sophisticated methods and research-grade resolution MRIs.
Clinical Relevance:
Sex-specific screening tools could be developed to identify individuals at an increased risk of sustaining an ACL injury based on the knee geometry previously associated with injury risk but using time- and effort-efficient clinical-grade resolution MRI-based methods. Thereafter, injury prevention could target these individuals.
REFERENCES
- 1.Bayer S, Meredith SJ, Wilson K, et al. Knee morphological risk factors for anterior cruciate ligament injury: a systematic review. J Bone Joint Surg Am. 2020;102(8):703–718. [DOI] [PubMed] [Google Scholar]
- 2.Beynnon BD, Hall JS, Sturnick DR, et al. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42(5):1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beynnon BD, Vacek PM, Sturnick DR, et al. Geometric profile of the tibial plateau cartilage surface is associated with the risk of non-contact anterior cruciate ligament injury. J Orthop Res. 2014;32(1):61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blanke F, Kiapour AM, Haenle M, et al. Risk of noncontact anterior cruciate ligament injuries is not associated with slope and concavity of the tibial plateau in recreational alpine skiers: a magnetic resonance imaging-based case-control study of 121 patients. Am J Sports Med. 2016;44(6):1508–1514. [DOI] [PubMed] [Google Scholar]
- 5.Carter JC, Sturnick DR, Vacek PM, et al. Relationship between geometry of the extensor mechanism of the knee and risk of anterior cruciate ligament injury. J Orthop Res. 2017;35(5):965–973. [DOI] [PubMed] [Google Scholar]
- 6.Chandrashekar N, Slauterbeck J, Hashemi J. Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: a cadaveric study. Am J Sports Med. 2005;33(10):1492–1498. [DOI] [PubMed] [Google Scholar]
- 7.Chaudhari AM, Zelman EA, Flanigan DC, Kaeding CC, Nagaraja HN. Anterior cruciate ligament-injured subjects have smaller anterior cruciate ligaments than matched controls: a magnetic resonance imaging study. Am J Sports Med. 2009;37(7):1282–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dare DM, Fabricant PD, McCarthy MM, et al. Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: an MRI-based case-control study of 152 patients. Am J Sports Med. 2015;43(7):1632–1639. [DOI] [PubMed] [Google Scholar]
- 9.Flannery SW, Kiapour AM, Edgar DJ, Murray MM, Fleming BC. Automated magnetic resonance image segmentation of the anterior cruciate ligament. J Orthop Res. 2020. November 26; [Epub ahead of print] PMID: 33241856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grassi A, Macchiarola L, Urrizola Barrientos F, et al. Steep posterior tibial slope, anterior tibial subluxation, deep posterior lateral femoral condyle, and meniscal deficiency are common findings in multiple anterior cruciate ligament failures: an MRI case-control study. Am J Sports Med. 2019;47(2):285–295. [DOI] [PubMed] [Google Scholar]
- 11.Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62. [DOI] [PubMed] [Google Scholar]
- 12.Hosseinzadeh S, Kiapour AM. Age-related changes in ACL morphology during skeletal growth and maturation are different between females and males. J Orthop Res. 2020. May 19; [Epub ahead of print] PMID: 32427346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo TK, Li MY. A guideline of selecting and reporting intraclass correl444444466666ation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lipps DB, Oh YK, Ashton-Miller JA, Wojtys EM. Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med. 2012;40(1):32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okazaki Y, Furumatsu T, Kodama Y, et al. Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2021;29(1):44–50. [DOI] [PubMed] [Google Scholar]
- 17.Schneider A, Si-Mohamed S, Magnussen RA, Lustig S, Neyret P, Servien E. Tibiofemoral joint congruence is lower in females with ACL injuries than males with ACL injuries. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1375–1383. [DOI] [PubMed] [Google Scholar]
- 18.Shultz SJ, Schmitz RJ, Benjaminse A, Collins M, Ford K, Kulas AS. ACL Research Retreat VII: an update on anterior cruciate ligament injury risk factor identification, screening, and prevention. J Athl Train. 2015;50(10):1076–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shultz SJ, Schmitz RJ, Cameron KL, et al. Anterior Cruciate Ligament Research Retreat VIII summary statement: an update on injury risk identification and prevention across the anterior cruciate ligament injury continuum, March 14–16, 2019, Greensboro, NC. J Athl Train. 2019;54(9):970–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Staeubli HU, Adam O, Becker W, Burgkart R. Anterior cruciate ligament and intercondylar notch in the coronal oblique plane: anatomy complemented by magnetic resonance imaging in cruciate ligament-intact knees. Arthroscopy. 1999;15(4):349–359. [DOI] [PubMed] [Google Scholar]
- 22.Sturnick DR, Argentieri EC, Vacek PM, et al. A decreased volume of the medial tibial spine is associated with an increased risk of suffering an anterior cruciate ligament injury for males but not females. J Orthop Res. 2014;32(11):1451–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sturnick DR, Vacek PM, DeSarno MJ, et al. Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med. 2015;43(4):839–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sturnick DR, Van Gorder R, Vacek PM, et al. Tibial articular cartilage and meniscus geometries combine to influence female risk of anterior cruciate ligament injury. J Orthop Res. 2014;32(11):1487–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vasta S, Andrade R, Pereira R, et al. Bone morphology and morphometry of the lateral femoral condyle is a risk factor for ACL injury. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2817–2825. [DOI] [PubMed] [Google Scholar]
- 26.Vrooijink SH, Wolters F, Van Eck CF, Fu FH. Measurements of knee morphometrics using MRI and arthroscopy: a comparative study between ACL-injured and non-injured subjects. Knee Surg Sports Traumatol Arthrosc. 2011;19 Suppl 1:12–16. [DOI] [PubMed] [Google Scholar]
- 27.Whitney DC, Sturnick DR, Vacek PM, et al. Relationship between the risk of suffering a first-time noncontact ACL injury and geometry of the femoral notch and ACL: a prospective cohort study with a nested case-control analysis. Am J Sports Med. 2014;42(8):1796–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]