Abstract
A subset of mothers who carry the FMR1 premutation may express a unique phenotype. The relationship between the FMR1 phenotype and mother-child interaction in families with fragile X associated disorders has not been well characterized, despite the importance of high-quality mother-child interaction for child development. This study examined the association between the FMR1 phenotype and the quality of interactions between mothers and their adolescent/young adult sons with fragile X syndrome. Mother-youth synchrony was coded from a dyadic interaction. Maternal anxiety and depression symptoms, executive function deficits, and pragmatic language difficulties were evaluated. Results indicated that pragmatic language was associated with mother-youth synchrony. These findings highlight the importance of family-centered intervention practices for families with fragile X-associated disorders.
Keywords: mother-child interaction, fragile X carrier, pragmatic language, FXS
The quality of mother-child interaction plays a key role in child development. For instance, the amount and variety of language directed to infants are strong predictors of later language outcomes (Huttenlocher et al., 1991; Landry et al., 2006; Tamis-LeMonda et al., 2001). During middle childhood, positive mother-child interactions are linked to better social skills, including improved social information processing and less antisocial behavior (Criss et al., 2003). In adolescence, the quality of mother-child interactions is associated with emotional adjustment, prosocial behavior, and self-esteem (Barber et al., 2001; Gecas & Schwalbe, 1986; Lindsey et al., 2008). These outcomes are consistent with the theoretical framework of the transactional model of development, which posits that developmental outcomes are a function of reciprocal exchanges of the child and the social context (Sameroff et al., 1975; Sameroff & Fiese, 2000). The present study focused on the synchrony of interactions between mothers and their adolescent/young adult sons with fragile X syndrome (FXS), the most common inherited form of intellectual disability (A. Schneider et al., 2009).
The quality of mother-child interactions may have heightened importance for the developmental outcomes of individuals with intellectual and developmental disabilities (IDDs). A large body of research links maternal interaction style to a range of developmental outcomes in children with IDDs, including behavioral problems and language abilities (Baker, Smith, et al., 2011; Greenberg et al., 2006; Siller & Sigman, 2002). Moreover, the influence of mother-child interactions tends to be prolonged in families of children with IDDs, potentially lasting well into the child’s adult years (Seltzer et al., 2011). Children with IDDs are likely to continue to reside with their parents for considerably longer than their typically developing peers, with about half of adults with IDDs living with their middle-aged parents and relying on them for daily assistance (Seltzer et al., 2011). In sum, high-quality mother-child interactions may be crucial within the context of IDDs because reliance on adult- and family-centered learning contexts is increased and sustained well into adulthood.
The quality of mother-child interactions can be measured in a variety of ways. Maternal responsiveness coding schemes, which focus on the mother’s active accommodations to scaffold and support the child’s participation in the interaction, have been used extensively in studies of young children with IDDs (e.g., Brooks-Gunn & Lewis, 1984; Sterling & Warren, 2014; Warren et al., 2010). However, measurement techniques that capture the interaction style of the dyad as a whole may be better suited to index the interactions of adolescents/young adults and their mothers. As children age and advance in their communication skills, there is a greater expectation for mutual responsiveness, accommodation, and equal participation in the interaction (Harrist & Waugh, 2002). Indices of mother-child synchrony effectively capture this type of dynamic interaction, which is characterized by the responsiveness, reciprocity, engagement, mutual focus, and shared affect of the dyad.
The present study focused on the synchrony of interactions between mothers and their adolescent/young adult sons with FXS. A unique aspect of FXS is its inheritance patterns, affecting multiple family members. In most cases, mothers of children with FXS are carriers of the FMR1 premutation, which occurs when there is an expansion of the CGG trinucleotide sequence on the FMR1 gene of 55–200 repeats (Garber et al., 2008). Those with the FMR1 premutation are referred to as “carriers” because there is a chance of passing FXS onto their children, which occurs when the CGG expansion exceeds 200 repeats.
In the past, carriers of the FMR1 premutation were thought to only be at risk for passing FXS to their children; however, a large body of research has now shown there are health implications associated with the FMR1 premutation itself. For instance, two fragile X-associated disorders are caused by the premutation genotype: fragile X-associated tremor ataxia syndrome (FXTAS) and fragile X-associated primary ovarian insufficiency (FXPOI; Fink et al., 2018; Hagerman, 2013). A growing body of evidence also suggests a subset of individuals with the FMR1 premutation are also at higher risk for mental health disorders, executive function limitations, and subtle social and language difficulties (Hagerman et al., 2018; Klusek et al., 2019, 2018; Losh et al., 2012; Roberts et al., 2009, 2016; Shelton et al., 2014). Thus, genetic liability is experienced by both mothers and children within the context of FXS, highlighting the importance of considering maternal phenotypes when characterizing the interactions of mothers and their children with FXS. In the present study, we examined the relationship between core features of the FMR1 premutation phenotype of the mother and the quality of mother-child synchrony, with a focus on maternal anxiety, depression, executive function limitations, and pragmatic language difficulties.
Mother-child synchrony within the context of FXS has not been previously described in the literature. However, studies focused more narrowly on maternal responsivity suggest that mother-child interaction quality plays a role in cognitive and language development in children with FXS. Warren et al. (2010) found that early maternal responsivity predicted the rate of communication and variety of words used in children with FXS at age three. A follow-up of this sample in middle childhood indicated that maternal responsivity maintained as a predictor of a variety of language abilities, including receptive and expressive vocabulary and the rate of different words produced (Brady et al., 2014). In a sample of children with FXS aged one to six years, Wheeler et al. (2007) detected similar relationships between the quality of maternal behaviors (i.e., maintaining and scaffolding behaviors) and receptive language skills in children with FXS. While few studies have examined maternal responsivity in FXS specifically during the adolescent period, evidence suggests that the importance of maternal communicative behaviors and the quality of the mother-child relationship is sustained through adolescence in IDDs and FXS (Klusek et al., 2016; Orsmond et al., 2006; Smith et al., 2008).
Prior research has documented the importance of high-quality mother-child interactions for the development of children with FXS. We aimed to extend this line of work to determine how the core features of the FMR1 premutation phenotype—specifically, mental health symptoms, executive function limitations, and pragmatic language difficulties—contribute to the quality of mother-child interactions. Furthermore, given that prior research has focused largely on mother-child interactions with younger children with FXS, we sought to extend this work to the study of mothers and their adolescent/young adult sons with FXS. Understanding the factors that influence the outcomes of individuals with FXS across the lifespan is needed in order to maximize the effectiveness of family-centered supports aimed at improving the care and quality of life for individuals with FXS and their families. The present study was designed to understand the relationship between core phenotypic features of the FMR1 premutation and the synchrony of interactions between mothers and their adolescent/young adult sons with FXS. We hypothesized that FMR1 premutation-associated symptoms would negatively influence the synchrony of the dyad. For the purposes of this study, the term “mother-youth” is used to refer to the dyadic relationship between our sample of mothers and their sons with FXS, given that some of the adolescent/young adult participants in the present sample would not be considered “children” according to their age.
Method
Participants
Participants included 29 mothers with the FMR1 premutation and their sons with FXS. Participants with FXS were drawn from a larger longitudinal study focused on language development in adolescents with FXS (Abbeduto et al., 2019), while mothers with the FMR1 premutation were enrolled in a related study investigating social language use in mothers with the FMR1 premutation (Klusek et al., 2018). All participants were native English speakers. The genetic status of the full mutation in the sons (>200 CGG repeats) and the FMR1 premutation in the mothers (55–200 CGG repeats) was confirmed through genetic testing or medical record review as part of the larger studies. All participants with FXS used at least two- to three-word phrases according to maternal report and lived at home with their biological mother at the time of the study. None of the mothers had received a clinical diagnosis of FXTAS, per self-report. Families were recruited through parent listservs, social media, and the University of North Carolina at Chapel Hill’s Research Participant Registry Core of the Carolina Institute of Developmental Disabilities.
Descriptive and demographic information for the mothers with the FMR1 premutation and their adolescent/adult aged sons with FXS are presented in Table 1. Information regarding the family environment was collected to describe the group. Consistent with the inclusionary criteria, all youth with FXS lived at home with their mother, 87% lived with their mother and another adult caregiver, and 13% lived with their mother as the only caregiving adult in the home. Twenty percent of the youth with FXS had no siblings, 37% had siblings without FXS, and 43% one or more siblings with FXS. Eighty-seven percent of the youth with FXS attended school or a day program, whereas the remaining 13% did not participate in regular activities (e.g., school, day program, job) outside of the home during the day.
Table 1.
Maternal and youth demographics and descriptives
| Variable | Descriptive Statistic |
|---|---|
| Maternal Age (years) | |
| M (SD) | 46.52 (5.45) |
| Range | 36–56 |
| Maternal Education % | |
| High school graduate | 20% |
| Some college/Associate’s degree | 36% |
| Bachelor’s college degree | 10% |
| Some graduate work/Master’s degree | 34% |
| Maternal Race % | |
| Black/African American | 3% |
| White | 97% |
| Maternal CGG Repeat Length | |
| M (SD) | 96.43 (15.00) |
| Range | 64–126 |
| Household Income | |
| $0-$50,000 | 18% |
| $50,001-$100,000 | 29% |
| $100,001-$150,000 | 32% |
| >$150,001 | 21% |
| Youth Age | |
| M (SD) | 18.48 |
| Range | 16–27 |
| Youth Nonverbal IQa | |
| M (SD) | 39.79 (6.13) |
| Range | 36–56 |
| Youth Expressive Vocabularyb | |
| M (SD) | 56.83 (17.47) |
| Range | 20–85 |
| Youth Race % | |
| Black/African American | 3% |
| White | 94% |
| Other | 3% |
Measured with the Leiter-R Brief IQ (Roid & Miller, 1997).
Standard scores measured with the Expressive Vocabulary Test, 2nd Edition (Williams, 2007).
Procedures
The protocol of the larger longitudinal study was administered over two consecutive days in a university laboratory setting. Maternal and youth data for the study were collected concurrently for the dyad; however, data were taken from Year 1 (n=1), Year 2 (n=20), Year 3 (n=8), and Year 4 (n=1) of the larger longitudinal study. The time point of administration of the mother-youth interaction task varied according to time constraints and staff availability, given that this was a “convenience” study conducted outside of the scope of the larger parent study. Procedures were approved by the Institutional Review Board of South Carolina. Consent was obtained from the mothers participating, and assent was obtained from the participants with FXS.
Measures
Mother-Youth Synchrony
Mother-youth synchrony was measured by observing and coding two unstructured interactive play tasks. The tasks were based on the mother-child interaction protocol used by Warren et al. (2010) and Brady et al. (2014) but modified for use with adolescents/young adults with FXS. The first task was taken from a protocol developed by Lunkenheimer et al. (2017), which has previously been used to study parent-child interaction in those with Down syndrome (Schworer et al., 2019). The mother-youth dyad was given a wooden puzzle (i.e., Castle Logix™) to put together. Dyads received the following instructions, consistent with the task instructions used by Warren et al. (2010) and Brady et al. (2014): “I want you to build a castle with your mom. Here are the materials for building the castle. In addition, there is a card with tips for building the castle. I will come back to check on you in about 10 minutes.” Immediately after the first task, the castle was replaced with a box of toys, and the dyad was instructed: “Now I have a box of toys and objects for you to look at and play together. I will come back to check on you in about 10 minutes.” Toys included markers, paper, a book of paper airplanes, a foam pocket shot, plastic dragonflies, dinosaur eggs, sticky hands, a finger puppet, a spaghetti ball, medical gloves, a pen, and a pad of sticky notes.
The interactions were video-recorded and coded using an adaptation of the Anchor Points for Observational Ratings of Positive Synchrony (Criss et al., 2003). The coding scheme operationalizes the quality of synchrony between the mother-youth dyad using a 9-point rating scale. The coding scheme reflects the exact rating scale of Criss et al. (2003) with the addition of a code of “0” signifying a refusal to interact with the other partner. A rating of “1” indicates either no engagement or interaction or complete dominance from one partner. A rating of a “4” reflects an interaction in which partners have the same focus, yet one partner may dominate the interaction. A rating of “9” indicates the mother and their adolescent/young adult son are focused on the same activity with equal contribution to the interaction. See Criss et al. (2003) for the full coding scheme. Each one-minute segment of the sample was coded for synchrony quality. Exploratory analyses examining scores across the subtasks revealed no significant differences (t(28)=.216, p=.831). Therefore, to reduce the number of statistical analyses, an average of the total time across both tasks was computed, yielding one overall rating. Prior to coding, two raters practiced coding a series of training files until reliability of >80% agreement on three consecutive practice videos was established. Each videotaped sample was coded by one of the two trained raters. Inter-rater reliability on a random 20% of the coded samples was calculated as an intraclass correlation (ICC) and indicated excellent agreement, ICC (3,2) = .997.
Characteristics of the Mothers with the FMR1 Premutation
Depression Symptoms
Depression symptoms were measured using the Beck Depression Inventory-II (BDI-II; Beck et al., 1996), a self-report questionnaire evaluating symptoms occurring over the past two weeks. The BDI-II is comprised of 21 items rated on a Likert scale from 0–3, with a score of “0” reflecting no evidence of a symptom and a “3,” reflecting a severe rating of a depression symptom. The total score of the BDI-II can range from 0–40, with a higher score reflecting more severe depression symptoms. The BDI-II shows high internal consistency, test-retest reliability, and validity (Dozois et al., 1998; Sprinkle et al., 2002).
Anxiety Symptoms
Anxiety symptoms were measured by the Beck Anxiety Inventory (BAI; Beck & Steer, 1990), a self-report questionnaire evaluating symptoms occurring over the past week. The BAI consists of 21 items rated on a 4-point scale. A score of a “0” signifies symptoms were rated as “not at all” and a “3” signifies symptoms were rated “severely.” The total raw score of the BAI ranges from 0–63, with a higher score reflecting greater severity of anxiety symptoms. The BAI has high internal consistency, acceptable test-retest reliability, and construct validity (Beck & Steer, 1990; Fydrich et al., 1992).
Executive Function
Executive function was indexed using the Hayling Sentence Completion Test (Burgess & Shallice, 1997), a measure of verbal inhibition. Inhibition is well-documented and sensitive to difficulties presented in women with the FMR1 premutation, while difficulties in other executive function domains have not been consistently documented in this population (Klusek et al., 2020). During the Hayling, the examiner reads 15 sentences that are missing the final word. The participant completes the sentence with a word that is unrelated to the sentence, requiring suppression of a prepotent response. The responses are scored for connected and loosely connected errors. The converted error score, which considers both the error severity and frequency of errors, was computed as described in the test manual. Converted error scores range from 0–78, with a higher score indicating worse verbal inhibition performance.
Pragmatic Language
Pragmatic language skills were assessed from a 20-minute conversation sample structured around a standard set of questions concerning neutral, shared experiences, such as “what kinds of activities did you enjoy most as a child?” To maintain a conversational tone, the examiner expanded upon the participants’ turns by commenting, offering information, and asking follow-up questions. Conversational samples were coded for pragmatic language violations using a modified version of the Pragmatic Rating Scale (PRS; Klusek et al., 2016, 2019; Landa et al., 1992). The PRS was developed to capture pragmatic language variation in non-impaired adults and is sensitive to pragmatic differences observed in mothers with the FMR1 premutation (Klusek et al., 2019; Losh et al., 2012). The PRS consists of 26 items, which uses a 3-point scale for each pragmatic violation, rated as either “striking and present,” “mild,” or “absent.” Examples of pragmatic language violations include failure to provide background information, use of pedantic word choice, providing overly-frank or overly-blunt responses, and the inability to clarify to resolve a communication breakdown. The scores for each item are added together for a total pragmatic deficit score. A consensus process between two trained independent coders was used across all participants. Each sample was coded independently by both raters, and discrepancies between the independent codes were resolved by re-watching the videotape and reaching consensus on the appropriate code via discussion. ICCs calculated to determine inter-rater reliability on the scores prior to consensus indicated moderate agreement, ICC (3,2) = .610.
Characteristics of the Youth with FXS
Autism Symptom Severity
Autism symptom severity was measured using the calibrated severity score of the Autism Diagnostic Observation Schedule-Second Edition (ADOS-2; Lord et al., 2012). The ADOS-2 is a semi-structured, standardized assessment, measuring communication, social interaction, play, and restricted and repetitive behaviors. The ADOS-2 was administered only at the initial time point of the larger study, given evidence that autism symptoms show relative stability over time in adolescents and adults with FXS (Sabaratnam et al., 2003). Therefore, the ADOS-2 was collected in Year 1 of the larger longitudinal study, whereas the mother-youth task and other measures were collected concurrently. Seventy-two percent of the youth with FXS scored above the cutoff for autism spectrum disorder. Our study indexed autism symptom severity using a Calibrated Severity Score (CSS) ranging from 1 to 10, with a score of 10 indicating increased symptom severity. All ADOS-2 administrations were conducted by research reliable examiners. Inter-rater reliability conducted on 15% of the administrations yielded 81% agreement for the algorithm items.
Problem Behavior
Problem behaviors displayed by the youth with FXS were measured using the Child Behavior Checklist (CBCL, Achenbach & Rescorla, 2001), a caregiver report questionnaire rating their child’s emotional and behavioral functioning over the past six months. Each item ranges from a score of “0” to “3”, with a score of “0” indicating “not true” and a score of “3,” indicating “very true or often true.” The CBCL total raw score, assessing overall problem behavior (e.g., aggression, attention difficulties, externalizing, and internalizing behaviors), was used in the analyses. Although some of the youth with FXS were older than 18 years, the 6–18 year form was administered to all participants because the items were deemed to be more appropriate for the developmental level of the sample; this approach is consistent with prior work (Roberts et al., 2018).
Nonverbal IQ
Nonverbal intelligence was assessed using the Leiter-R Brief IQ (Roid & Miller, 1997). The Leiter-R Brief IQ consists of four subscales: figure ground, form completion, sequential order, and repeated patterns. The Leiter-R Brief IQ provides a measure of nonverbal cognitive ability and has been widely used as an index of cognitive ability in populations with intellectual disability (Hooper et al., 2000; Skinner et al., 2005). Growth scale values were used in the analysis, as they yield an equal-interval scale of performance and are less vulnerable to floor effects than standard scores.
Expressive Vocabulary
Expressive vocabulary was indexed using the Expressive Vocabulary Test, 2nd Edition (EVT-2; Williams, 2007). During the administration of the EVT-2, participants are asked to either label or provide a synonym for a set of images. Growth scale value scores were used in the analysis.
Data Analysis
Analyses were conducted using R software (R Core Team, 2019). Data were examined for normality, and skewness was detected for the Hayling, BAI, and BDI-II. All other variables used in the analyses were normally distributed. Tukey’s ladder of powers transformation was applied to determine the optimal normalizing transformation for depression symptoms on the BDI-II (λ=0.75), anxiety symptoms on the BAI (λ=0.75), and executive function abilities on the Hayling (λ=0.5).
Descriptive statistics were then computed, a Pearson correlation matrix was created to examine associations between maternal and youth variables of interest (see Table 2), and scatterplots were examined to visually confirm linear relationships among the variables. Based on theory and precedence in previous literature, the following characteristics of the youth with FXS were selected as potential covariates: autism severity, behavior problems, nonverbal IQ, and expressive vocabulary skills. Intercorrelations among the covariates relating to youth characteristics indicated significant correlations between expressive vocabulary and both autism severity and nonverbal IQ. Among these covariates, nonverbal IQ was only significantly correlated with the expressive vocabulary variable. Therefore, to avoid issues related to multicollinearity, nonverbal IQ was retained as a covariate, and the expressive vocabulary variable was not included in the model.
Table 2.
Correlations among study variables
| Synchrony | PRS | BDI-II | BAI | Hayling | ADOS-2 | CBCL | Leiter-R | EVT-2 | |
|---|---|---|---|---|---|---|---|---|---|
| Synchrony | 1.00 | ||||||||
| PRS | −0.35** | 1.00 | |||||||
| BDI-II | −0.06 | −0.06 | 1.00 | ||||||
| BAI | 0.12 | −0.16 | 0.79*** | 1.00 | |||||
| Hayling | −0.08 | 0.23 | 0.04 | −0.17 | 1.00 | ||||
| ADOS-2 | −0.26 | 0.14 | 0.13 | −0.01 | 0.53** | 1.00 | |||
| CBCL | 0.35 | −0.17 | 0.45* | 0.51** | −0.09 | 0.13 | 1.00 | ||
| Leiter-R | 0.55* | −0.50** | −0.10 | 0.15 | −0.17 | −0.26 | 0.05 | 1.00 | |
| EVT-2 | 0.48 | −0.49* | 0.024 | 0.21 | −0.25 | −0.44* | 0.16 | .74*** | 1.00 |
Note. BDI-II, Beck Depression Inventory-II; BAI, Beck Anxiety Index; Hayling, Hayling Sentence Completion Test; PRS, Pragmatic Rating Scale; ADOS-2, Autism Diagnostic Observation Schedule-Second Edition; CBCL, Child Behavior Checklist; EVT-2, Expressive Vocabulary Test, 2nd Edition.
p<.05,
p<.01,
p<.001
A series of regressions were performed to separately examine maternal depression symptoms, anxiety symptoms, executive function, and pragmatic skills as predictors of mother-youth synchrony, covarying for characteristics of the youth with FXS, including nonverbal IQ, autism severity, and severity of problem behavior in each model. A quadratic term was also probed in the model examining maternal pragmatic skills as the predictor of interest, given that the plotted raw data suggested a nonlinear association. The quadratic term was retained if it accounted for significant variation in the model, and examination of the fit plots indicated improved model fit. Partial eta squared (ηp2) was computed for each model, where “.01” is generally considered a small effect size, “.06” a medium effect size, and “.14” a large effect size (Cohen, 1988). Means, standard deviations, and ranges for the study variables are presented in Table 3.
Table 3.
Maternal and youth characteristics
| Raw | Transformed | |||||
|---|---|---|---|---|---|---|
| M | SD | Range | M | SD | Range | |
| Maternal Characteristics | ||||||
| BDI-II | 9.21 | 7.09 | 0–26 | 4.94 | 3.13 | 0.00–11.51 |
| BAI | 6.32 | 5.10 | 0–16 | 3.68 | 2.54 | 0.00–8.00 |
| Hayling | 8.34 | 9.89 | 0–43 | 2.43 | 1.59 | 0.00–6.56 |
| PRS | 9.41 | 3.63 | 2–17 | N/A | N/A | N/A |
| Youth Characteristics | ||||||
| ADOS-2 | 5.66 | 2.39 | 1–10 | N/A | N/A | N/A |
| CBCL | 30.66 | 12.58 | 6–51 | N/A | N/A | N/A |
| Leiter-R | 39.79 | 6.13 | 36–56 | N/A | N/A | N/A |
| Mother-Youth Interaction | ||||||
| Synchrony | 3.58 | 1.08 | 0–5.5 | N/A | N/A | N/A |
Note. BDI-II, Beck Depression Inventory-II; BAI, Beck Anxiety Index; Hayling, Hayling Sentence Completion Test; PRS, Pragmatic Rating Scale; ADOS-2, Autism Diagnostic Observation Schedule-Second Edition; CBCL, Child Behavior Checklist.
Results
FMR1 Premutation Symptoms as Predictors of Mother-Youth Synchrony
Maternal Depression Symptoms
The overall model testing the influence of maternal depression symptoms and characteristics of the youth with FXS on synchrony did not show a significant effect (F[4,24]=1.61, p=.204, R2=.21; Table 4).
Table 4.
Regression coefficients depicting maternal depression symptoms as a predictor of mother-youth synchrony
| Effect | ß | SE | t | p | ηp² |
|---|---|---|---|---|---|
| Intercept | −8.77 | 6.89 | −1.27 | .215 | |
| BDI-II | −0.05 | 0.07 | −0.75 | .463 | .02 |
| ADOS-2 | −0.06 | 0.09 | −0.70 | .489 | .05 |
| CBCL | 0.02 | 0.02 | 0.86 | .398 | .05 |
| Leiter-R | 0.03 | 0.01 | 1.85 | .078 | .12 |
Note. BDI-II, Beck Depression Inventory-II; ADOS-2, Autism Diagnostic Observation Schedule-Second Edition; CBCL, Child Behavior Checklist.
Maternal Anxiety Symptoms
The overall model testing the influence of maternal anxiety and characteristics of the youth with FXS on synchrony was significant (F[4,23]=4.91, p=.005, R2=.46; Table 5). However, significant variance in the model was not accounted for by maternal anxiety symptoms (p=.327, ηp2=.03).
Table 5.
Regression coefficients depicting maternal anxiety symptoms as a predictor of mother-youth synchrony
| Effect | ß | SE | t | p | ηp² |
|---|---|---|---|---|---|
| Intercept | −10.44 | 4.47 | −2.33 | .029 | |
| BAI | −0.06 | 0.06 | −1.00 | .327 | .03 |
| ADOS-2 | −0.07 | 0.06 | −1.21 | .239 | .11 |
| CBCL | 0.03 | 0.01 | 2.42 | .024 | .21 |
| Leiter-R | 0.03 | 0.01 | 3.15 | .005 | .30 |
Note. BAI, Beck Anxiety Index; ADOS-2, Autism Diagnostic Observation Schedule-Second Edition; CBCL, Child Behavior Checklist.
Maternal Executive Function
The model testing the influence of maternal executive function and characteristics of the youth with FXS on synchrony did not show a significant effect (F[4,24]=1.50, p=.235, R2=.20; Table 6).
Table 6.
Regression coefficients depicting maternal executive function as a predictor of mother-youth synchrony
| Effect | ß | SE | t | p | ηp² |
|---|---|---|---|---|---|
| Intercept | −9.54 | 6.90 | −1.38 | .179 | |
| Hayling | 0.06 | 0.15 | 0.43 | .674 | .01 |
| ADOS-2 | −0.09 | 0.10 | −0.85 | .404 | .05 |
| CBCL | 0.01 | 0.02 | 0.64 | .525 | .03 |
| Leiter-R | 0.02 | 0.01 | 1.94 | .064 | .14 |
Note. Hayling, Hayling Sentence Completion Test; ADOS-2, Autism Diagnostic Observation Schedule-Second Edition; CBCL, Child Behavior Checklist.
Maternal Pragmatic Language
The overall model testing the combined influence of maternal pragmatic language and characteristics of the youth with FXS, including nonverbal IQ, autism severity, and severity of problem behavior on synchrony was significant (F[5,23]=6.31, p<.001, R2=.58). The full model results are presented in Table 7. Nonverbal IQ, autism severity, and severity of problem behavior were not significant predictors of synchrony (p’s>.151). Significant effects were observed for the linear (p=.006, ηp2=.38) and quadratic terms (p=.001, ηp2=.39) for maternal pragmatic language difficulties, with large effect sizes (Figure 1).
Table 7.
Regression coefficients depicting maternal pragmatic skills as a predictor of mother-youth synchrony
| Effect | ß | SE | t | p | ηp² |
|---|---|---|---|---|---|
| Intercept | −6.69 | 5.95 | −1.12 | .273 | |
| PRS | 0.55 | 0.18 | 3.00 | .006 | .38 |
| PRS2 | −0.04 | 0.01 | −3.77 | .001 | .39 |
| ADOS-2 | 0.01 | 0.07 | 0.16 | .872 | .00 |
| CBCL | 0.01 | 0.01 | 0.90 | .377 | .04 |
| Leiter-R | 0.02 | 0.01 | 1.49 | .151 | .09 |
Note. PRS, Pragmatic Rating Scale; ADOS-2, Autism Diagnostic Observation Schedule-Second Edition; CBCL, Child Behavior Checklist.
Figure 1. Curvilinear association between maternal pragmatic language difficulties and mother-youth synchrony.
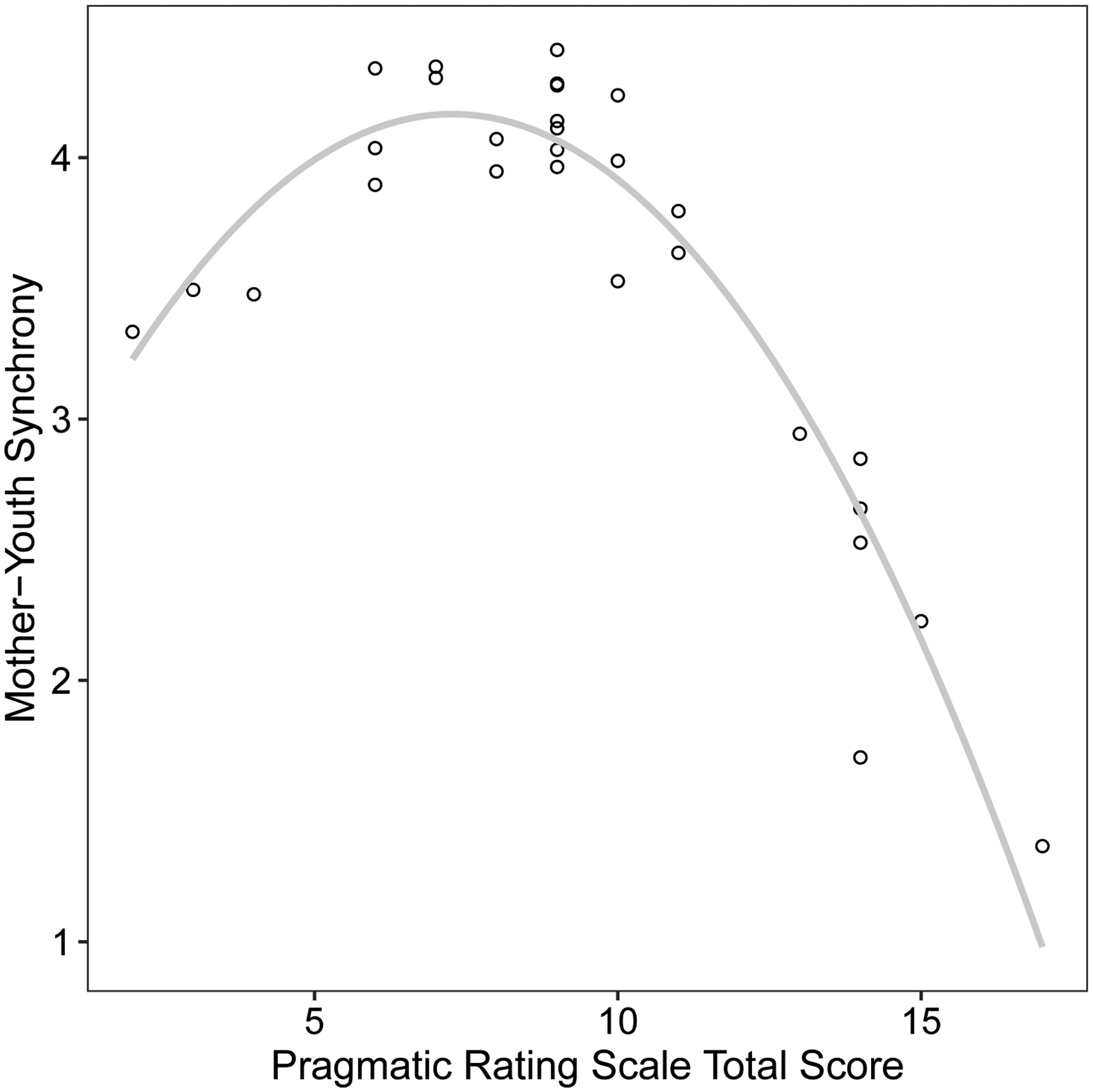
Note. Model-adjusted values are shown, controlling for youth nonverbal IQ, autism severity, and problem behavior. Higher scores for the Pragmatic Rating Scale reflect a greater number of violations and higher scores for mother-youth synchrony reflects a more synchronous relationship.
Discussion
High-quality synchronous social exchanges between mothers and their children are a robust predictor of child social, behavioral, and language outcomes, particularly for those with IDDs. The importance of synchronous interactions between mothers and their children extend to the adolescent period as well and are associated with various positive outcomes, such as self-esteem, prosocial behavior, and psychosocial adjustment (Barber et al., 2001; Chu & Powers, 1995; Gross & McCallum, 2000; Lindsey et al., 2008). For adolescents with IDDs, the quality of the mother-adolescent relationship in adolescence may have increased salience because the reliance on parents as a learning context is intensified relative to typically-developing peers and sustained into adulthood. FXS stands apart from most other IDDs because it is characterized by familial genetic vulnerability, where mothers can experience symptoms related to their status as genetic carriers. The goal of the present study was to determine the potential impact of maternal mental health, executive function, and pragmatic language symptoms on the synchrony of interactions between mothers with the FMR1 premutation and their sons with FXS. We focused on mother-youth dyads consisting of adolescent/young-adult sons, given that FXS familial support continues across the lifespan, and research focused on adolescents and young adults with FXS is scarce. Results indicated that maternal pragmatic language difficulties were strongly linked with low-quality asynchronous interactions, particularly for those mothers who showed high levels of pragmatic difficulty. In contrast, mental health symptoms and executive function abilities in mothers with the FMR1 premutation were not related to the quality of mother-youth synchrony. Findings inform aspects of the FMR1 premutation phenotype that may be relevant to the development of family-centered supports that meet the unique needs of all family members.
Maternal Pragmatic Language Skills Predict Mother-Youth Synchrony
Maternal pragmatic language difficulty emerged as a robust predictor of mother-youth synchrony, with a large effect size. This is a novel finding. While theoretically related, pragmatic language and synchrony are independent constructs, and there has been little prior research into their interface. Synchrony focuses on the mutual responsiveness and coordination of behaviors between communication partners (e.g., shared focus on play materials, shared affect). In contrast, pragmatic language difficulty is defined by the flouting of pragmatic language conventions, reflecting the inappropriate or ineffective use of language to convey meaning within social contexts (Landa et al., 1992). Thus, pragmatic language difficulty reflects the frequency and severity of specific pragmatic language violations committed by an individual, whereas synchrony focuses on the degree of coordination and mutual responsiveness between two communication partners. Although pragmatic language skills of mothers with the FMR1 premutation have been documented in prior studies within the context of a conversation with an unfamiliar examiner (Klusek et al., 2017, 2019; Losh et al., 2012), it has been unclear whether pragmatic difficulties exhibited within this adult context would influence interaction behaviors in other contexts, such as interactions with their children. Findings from this study demonstrate a relationship between maternal pragmatic language difficulties and reduced synchrony of mother-youth interactions.
A curvilinear association was detected, indicating that the relationship between maternal pragmatic language features and synchrony was the strongest among the subset of mothers who exhibited the most severe pragmatic difficulties. These findings align with the current understanding of the clinical presentation of the FMR1 premutation, which is characterized by both incomplete penetrance and variable expressivity that is thought to reflect individual differences in FMR1-associated molecular-genetic features, such as levels of messenger RNA and activation ratio (Tassone et al., 2014). Prior studies using the PRS in control mothers have reported average scores ranging from 3 to 6 (Klusek et al., 2017, 2019; Losh et al., 2012). Therefore, the average PRS score of 9.4 found for the present sample of mothers is suggestive of pragmatic difficulty at the group level. However, the relationship between maternal pragmatic difficulties and mother-youth synchrony appeared to be primarily driven by the subset of mothers who scored substantially above the group mean. A sharp decline in synchrony was observed with pragmatic scores about one standard deviation above the group mean, while this relationship was weaker as scores approached the group mean. Thus, among the subset of mothers who show increased symptom expression, the pragmatic language phenotype of the FMR1 premutation may have enhanced clinical significance in terms of outcomes.
Elevated pragmatic language violations are a well-documented aspect of the FMR1 premutation phenotype in mothers (Klusek et al., 2019; Losh et al., 2012). Although this aspect of the phenotype has been historically conceptualized as a “subtle” or clinically insignificant trait, the results of this study suggest the pragmatic language phenotype of the FMR1 premutation in mothers has clinical relevance for the developmental outcomes of their children with FXS. Our study is not the first report to document maternal pragmatic language competence as a factor that may impact child/family outcomes in IDDs. Pragmatic language difficulties among mothers with the FMR1 premutation have also been linked with lower receptive vocabulary, poorer expressive syntax skills, and increased autism symptom severity among children with FXS (Klusek et al., 2016; Losh et al., 2012). Similar patterns have been reported in studies of families of children with autism spectrum disorder, with maternal pragmatic language violations being linked to child expressive language impairment (Stern et al., 2017) and communication deficits (Klusek et al., 2014). Evidence from the study of a construct related to pragmatic competence— maternal responsivity— also indicates that early and sustained responsivity from mothers of children with FXS is an important predictor of the language and communication outcomes of their children throughout early and middle childhood (Brady et al., 2014; Warren et al., 2010). Altogether, this body of research suggests that subtle differences in maternal communication and interaction styles in the FMR1 premutation can be meaningful for the developmental outcomes of their children with FXS.
Longitudinal research is needed to better understand the unfolding of the relationship between maternal pragmatic language difficulties and synchronous dyadic interactions across development of the individual with FXS. We assume that the observed relationship between maternal pragmatic difficulties and asynchronous interactions in the present sample of adolescent/young adult sons with FXS reflects the accumulation of effects across time, where these mother-youth dyadic interaction patterns have persisted from earlier developmental periods and have been characteristic of the family dynamic for quite some time. Longitudinal work is needed to test this assumption, as well as to determine the stability of the pragmatic difficulties experienced by mothers with the FMR1 premutation across adulthood. Considering growing evidence of age-related decline in executive and psychiatric functioning in women with the FMR1 premutation (Klusek et al., 2020; Roberts et al., 2016), it is possible that pragmatic difficulties in mothers with the FMR1 premutation become more prominent in late-middle age, and therefore may not be a salient feature in young mothers. On the other hand, pragmatic language difficulties in the FMR1 premutation are thought to reflect elevated risk for autism and the broad autism phenotype, which are neurodevelopmental features that emerge in childhood (Farzin et al., 2006; Losh et al., 2012; A. Schneider et al., 2016). Future longitudinal work is needed to determine the stability and temporal emergence of pragmatic language deficits in mothers with the FMR1 premutation and to elucidate effects on child outcomes and mother-child interaction patterns across developmental periods.
Gaining an understanding of how the central features of the FMR1 phenotype in mothers relate to mother-child interactions has direct implications for the development of effective interventions for children with FXS. Bidirectional interactions between a child and their social context are believed to accumulate over time to facilitate development (Sameroff et al., 1975; Sameroff & Fiese, 2000). Indexing the mechanisms that drive the quality of the bidirectional interaction is imperative in improving the quality of the interaction. Within the context of families of children with IDDs, parents often play an expanded role in their children’s social learning context and continue to play a role across a longer than typical developmental period (Seltzer et al., 2011). Therefore, it is critical to understand maternal characteristics that may make it difficult for some parents to implement parent-mediated interventions proposed for FXS (McDuffie et al., 2016). For instance, features of pragmatic language, such as difficulty adjusting background information to meet the communication partner’s level, may lead to reduced synchrony related to communication breakdowns. Intervention research has documented intervention challenges related to pragmatic language traits in parents of children with autism spectrum disorder (e.g., Parr et al., 2015). Specifically, features of the broad autism phenotype in parents of children with autism spectrum disorder have been shown to negatively affect the rate of change in parent interaction style during parent-mediated intervention, suggesting that parents’ pragmatic abilities may moderate the effectiveness of parent-mediated intervention (Parr et al., 2015). Our findings, which identify maternal pragmatic language challenges as the strongest predictor of a synchronous mother-youth interaction, support the idea of individualized treatment models for parent-mediated intervention that focus on the social-communicative strengths and weaknesses of mothers. For example, individualized strategies for mothers who tend to dominate conversations may focus on parental responsiveness, whereas strategies for mothers with withdrawn pragmatic language features (e.g., lack of initiation, failure to elaborate on other’s turns) may emphasize parental engagement and increased use of language-modeling strategies. Future intervention research should consider the FMR1 premutation phenotype as a factor that may facilitate the effectiveness of parent-implemented intervention of individuals with FXS.
Maternal Anxiety, Depression, and Executive Function Symptoms are not Associated with Mother-Youth Synchrony
Anxiety and depression were not predictive of mother-youth synchrony, despite several mothers in the sample reporting clinically significant symptoms of depression (23%) or anxiety (30%). Some prior work suggests a relationship between maternal anxiety and mother-child interaction style (Rodgers, 1993; S. Schneider et al., 2009), though this relationship has not been studied in families of children with IDD. Maternal depression has also been found to impact mother-child interactions in studies focused on non-IDD groups (Cox et al., 1987; Harnish et al., 1995; Leckman-Westin et al., 2009). However, findings are variable, with several studies reporting a relationship (Greenberg et al., 2004; Orsmond et al., 2007) and others finding none (Baker, Seltzer, et al., 2011; Wheeler et al., 2007). One study that focused on children with FXS found that maternal depression did show a small association with maternal responsivity during a mother-child interaction, although other variables were stronger predictors (Sterling et al., 2013). Further investigation of the link between maternal mental health and the quality of mother-child interactions is warranted, as documentation of this relationship is not as established for mothers of children with IDDs, including FXS.
Maternal executive function, indexed by verbal response inhibition, was not a predictor of mother-youth synchrony, despite below-average executive function scores observed in 30% of the sample. Response inhibition is consistently documented as an area of executive function difficulty in women with the FMR1 premutation (Klusek et al., 2020; Kraan et al., 2014; Shelton et al., 2014). However, response inhibition is just one aspect of executive function, and future studies examining other components of executive function in relation to mother-child synchrony may reveal a different pattern. To our knowledge, ours is the first study to examine the interface between maternal executive function skills and familial interactions within the context of FXS, although maternal executive function deficits have been linked to negative caregiving behaviors in families of neurotypical children (Cuevas et al., 2014). Therefore, future studies aimed at the examination of other components of executive function (e.g., attention or working memory) in mothers with the FMR1 premutation are needed in order to understand the impact of executive function on mother-child interaction.
Strengths, Limitations, and Directions
This study contributes to scant knowledge on the relationship between maternal FMR1 premutation phenotypes and family interactions. Unlike most prior work in FXS that has focused primarily on maternal contributions to interaction quality, this study applied a synchrony coding scheme that captured the communicative contributions of both partners, which is critical in the study of adolescents/young adults where there is a greater expectation for a bidirectional interaction between communication partners. Although the importance of maternal responsivity in the early development of children with FXS has been previously documented, this study expanded the investigation of maternal factors that influence the quality of mother-child interactions to adolescents and young adults with FXS.
Because this was a convenience sample drawn from a larger study that was designed to test different research questions, some aspects of the design were not planned with the present study in mind. For example, the relatively small sample size of 29 dyads limited our ability to employ more complex statistical models to answer our research questions (i.e., maternal predictors were tested separately rather than examining the relative contributions of each maternal predictor within the same regression model). Another limitation is that the 20-minute mother-youth task provides a relatively short sampling period that was carried out in an unfamiliar laboratory setting and, therefore, limits on generalizability must be acknowledged. It will be critical for future studies to investigate these mother-youth interactions over longer periods of time and in alternative contexts, such as the participants’ own homes. Finally, while none of the mothers participating in this study had received clinical diagnoses of FXTAS, we lacked information on FXPOI—another FMR1 premutation-associated condition that may be relevant to the study of mother-child interaction quality due to the relationship between hormonal changes related to menopause and several maternal features of interest in the current study, including depression and executive function (Bromberger et al., 2011; Greendale et al., 2009).
Future directions include the examination of mother-youth synchrony as a factor that may predict independence and adult outcomes more generally in adolescents/young adults with FXS. While the present study focused on the contributions of the maternal phenotype while accounting for youth characteristics, understanding the specific contribution of youth skills, such as youth pragmatic language, as predictors of synchrony may lend insight into individualized therapy to support optimal outcomes of youth with FXS. Understanding the relationship between the FMR1 phenotype and mother-child interaction in females with FXS is needed as well, as the expression of FXS can present differently for males and females. The inclusion of another IDD comparison group in future work could also provide useful information, as adolescents with IDDs rely on a family-centered context much more than their neurotypical counterparts, and cross-syndrome comparisons could yield information on syndrome-specific patterns that may have implications for clinical practice. For example, similar patterns may be observed in families of children with autism spectrum disorder, as elevated pragmatic language difficulties have also been documented among mothers of children with autism spectrum disorder.
Conclusions
The present study suggests that maternal pragmatic language skills contribute to the quality of interactions between mothers with the FMR1 premutation and their adolescent/young adult sons with FXS. Given that FXS is characterized by familial genetic vulnerability, understanding the clinical features associated with the FMR1 premutation is important when developing family-centered interventions. This study establishes a framework for further investigation of the influence of maternal pragmatic language on the effectiveness of interventions within the FXS population.
Acknowledgments
We are grateful to the families who participated in this research. We also appreciate the contribution of Sydney Burrell with her assistance in coding the mother-child interactions and Caitlin Miller who assisted with the initial review of possible mother-child interaction coding schemes and modification of the coding scheme.
This work was supported by the National Institute of Child Health and Human Development (R01HD024356, PI: Leonard Abbeduto; U54HD079125, PI: Leonard Abbeduto; R03HD098291, PI: Jessica Klusek), the National Institute on Deafness and Other Communication Disorders (F32DC013934, PI: Jessica Klusek; R21DC017804, PI: Jessica Klusek), and the National Institute of Mental Health (L40MH108014, PI: Laura J. Mattie).
References
- Abbeduto L, Thurman AJ, McDuffie A, Klusek J, Feigles RT, Ted Brown W, Harvey DJ, Adayev T, LaFauci G, Dobkins C, & Roberts JE (2019). ASD Comorbidity in Fragile X Syndrome: Symptom Profile and Predictors of Symptom Severity in Adolescent and Young Adult Males. Journal of Autism and Developmental Disorders, 49(3), 960–977. 10.1007/s10803-018-3796-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla L (2001). Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. Aseba Burlington, VT. [Google Scholar]
- Baker JK, Seltzer MM, & Greenberg JS (2011). Longitudinal effects of adaptability on behavior problems and maternal depression in families of adolescents with autism. Journal of Family Psychology, 25(4), 601. 10.1037/a0024409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Smith LE, Greenberg JS, Seltzer MM, & Taylor JL (2011). Change in Maternal Criticism and Behavior Problems in Adolescents and Adults With Autism Across a 7-Year Period. Journal of Abnormal Psychology, 120(2), 465–475. 10.1037/a0021900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber JG, Bolitho F, & Bertrand L (2001). Parent-child synchrony and adolescent adjustment. Child and Adolescent Social Work Journal, 18(1), 51–64. 10.1023/A:1026673203176 [DOI] [Google Scholar]
- Beck A, Steer R, & Brown G (1996). Beck Depression Inventory-II. San Antonio. [Google Scholar]
- Beck AT, & Steer RA (1990). Manual for the Beck anxiety inventory. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Brady N, Warren SF, Fleming K, Keller J, & Sterling A (2014). Effect of sustained maternal responsivity on later vocabulary development in children with fragile X syndrome. Journal of Speech, Language, and Hearing Research, 57(1), 212–226. 10.1044/1092-4388(2013/12-0341) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromberger JT, Kravitz HM, Chang Y-F, Cyranowski JM, Brown C, & Matthews KA (2011). Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychological Medicine, 41(9), 1879–1888. 10.1017/S003329171100016X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks-Gunn J, & Lewis M (1984). Maternal Responsivity in Interactions with Handicapped Infants. Child Development, 55(3), 782–793. JSTOR. 10.2307/1130129 [DOI] [PubMed] [Google Scholar]
- Burgess P, & Shallice T (1997). Hayling Sentence Completion Test. Suffolk: Thames Valley Test Company. [Google Scholar]
- Chu L, & Powers PA (1995). Synchrony in adolescence. Adolescence, 30(118), 453. [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic. [Google Scholar]
- Cox A, Puckering C, Pound A, & Mills M (1987). The impact of maternal depression in young children. Journal of Child Psychology and Psychiatry, 28(6), 917–928. 10.1111/j.1469-7610.1987.tb00679.x [DOI] [PubMed] [Google Scholar]
- Criss MM, Shaw DS, & Ingoldsby EM (2003). Mother-son positive synchrony in middle childhood: Relation to antisocial behavior. Social Development, 12(3), 379–400. 10.1111/1467-9507.00239 [DOI] [Google Scholar]
- Cuevas K, Deater-Deckard K, Kim-Spoon J, Watson AJ, Morasch KC, & Bell MA (2014). What’s mom got to do with it? Contributions of maternal executive function and caregiving to the development of executive function across early childhood. Developmental Science, 17(2), 224–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozois DJA, Dobson KS, & Ahnberg JL (1998). A psychometric evaluation of the Beck Depression Inventory–II. Psychological Assessment, 10(2), 83–89. 10.1037/1040-3590.10.2.83 [DOI] [Google Scholar]
- Farzin F, Perry H, Hessl D, Loesch D, Cohen J, Bacalman S, Gane L, Tassone F, Hagerman P, & Hagerman R (2006). Autism Spectrum Disorders and Attention-Deficit/Hyperactivity Disorder in Boys with the Fragile X Premutation. Journal of Developmental & Behavioral Pediatrics, 27(2), S137. [DOI] [PubMed] [Google Scholar]
- Fink DA, Nelson LM, Pyeritz R, Johnson J, Sherman SL, Cohen Y, & Elizur SE (2018). Fragile X Associated Primary Ovarian Insufficiency (FXPOI): Case Report and Literature Review. Frontiers in Genetics, 9. 10.3389/fgene.2018.00529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fydrich T, Dowdall D, & Chambless DL (1992). Reliability and validity of the beck anxiety inventory. Journal of Anxiety Disorders, 6(1), 55–61. 10.1016/0887-6185(92)90026-4 [DOI] [Google Scholar]
- Garber KB, Visootsak J, & Warren ST (2008). Fragile X syndrome. European Journal of Human Genetics, 16(6), 666–672. 10.1038/ejhg.2008.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gecas V, & Schwalbe ML (1986). Parental Behavior and Adolescent Self-Esteem. Journal of Marriage and Family, 48(1), 37–46. JSTOR. 10.2307/352226 [DOI] [Google Scholar]
- Greenberg J, Seltzer MM, Hong J, & Orsmond GI (2006). Bidirectional Effects of Expressed Emotion and Behavior Problems and Symptoms in Adolescents and Adults With Autism. American Journal on Mental Retardation, 111(4), 229. 10.1352/0895-8017(2006)111[229:BEOEEA]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Greenberg J, Seltzer MM, Krauss MW, Chou RJ-A, & Hong J (2004). The effect of quality of the relationship between mothers and adult children with schizophrenia, autism, or Down syndrome on maternal well-being: The mediating role of optimism. American Journal of Orthopsychiatry, 74(1), 14–25. 10.1037/0002-9432.74.1.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greendale GA, Huang M-H, Wight RG, Seeman T, Luetters C, Avis NE, Johnston J, & Karlamangla AS (2009). Effects of the menopause transition and hormone use on cognitive performance in midlife women. Neurology, 72(21), 1850–1857. 10.1212/WNL.0b013e3181a71193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross PH, & McCallum RS (2000). Operationalization and predictive utility of mother–daughter synchrony. School Psychology Quarterly, 15(3), 279–294. 10.1037/h0088788 [DOI] [Google Scholar]
- Hagerman P (2013). Fragile X-associated tremor/ataxia syndrome (FXTAS): Pathology and mechanisms. Acta Neuropathologica, 126(1), 1–19. 10.1007/s00401-013-1138-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman RJ, Protic D, Rajaratnam A, Salcedo-Arellano MJ, Aydin EY, & Schneider A (2018). Fragile X-Associated Neuropsychiatric Disorders (FXAND). Frontiers in Psychiatry, 9. 10.3389/fpsyt.2018.00564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnish JD, Dodge KA, Valente E, & Group CPPR (1995). Mother-child interaction quality as a partial mediator of the roles of maternal depressive symptomatology and socioeconomic status in the development of child behavior problems. Conduct problems prevention research group. Child Development, 66(3), 739–753. 10.1111/j.1467-8624.1995.tb00902.x [DOI] [PubMed] [Google Scholar]
- Harrist AW, & Waugh RM (2002). Dyadic synchrony: Its structure and function in children’s development. Developmental Review, 22, 555–592. 10.1016/S0273-2297(02)00500-2 [DOI] [Google Scholar]
- Hooper S, Hatton D, Baranek GT, Roberts JP, & Bailey DB (2000). Nonverbal assessment of IQ, attention, and memory abilities in children with fragile-X syndrome using the Leiter-R. Journal of Psychoeducational Assessment, 18(3), 255–267. 10.1177/073428290001800305 [DOI] [Google Scholar]
- Huttenlocher J, Haight W, Bryk A, Seltzer M, & Lyons T (1991). Early Vocabulary Growth: Relation to Language Input and Gender. Developmental Psychology, 27(2), 236–248. 10.1037/0012-1649.27.2.236 [DOI] [Google Scholar]
- Klusek J, Fairchild AJ, & Roberts JE (2019). Vagal Tone as a Putative Mechanism for Pragmatic Competence: An Investigation of Carriers of the FMR1 Premutation. Journal of Autism and Developmental Disorders, 49(1), 197–208. 10.1007/s10803-018-3714-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Hong J, Sterling A, Berry-Kravis E, & Mailick MR (2020). Inhibition deficits are modulated by age and CGG repeat length in carriers of the FMR1 premutation allele who are mothers of children with fragile X syndrome. Brain and Cognition, 139. 10.1016/j.bandc.2019.105511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Losh M, & Martin GE (2014). Sex differences and within-family associations in the broad autism phenotype. Autism, 18(2), 106–116. 10.1177/1362361312464529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, McGrath SE, Abbeduto L, & Roberts JE (2016). Pragmatic Language Features of Mothers With the FMR1 Premutation Are Associated With the Language Outcomes of Adolescents and Young Adults With Fragile X Syndrome. Journal of Speech, Language, and Hearing Research, 59(1), 49–61. 10.1044/2015_JSLHR-L-15-0102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Porter A, Abbeduto L, Adayev T, Tassone F, Mailick MR, Glicksman A, Tonnsen BL, & Roberts JE (2018). Curvilinear Association Between Language Disfluency and FMR1 CGG Repeat Size Across the Normal, Intermediate, and Premutation Range. Frontiers in Genetics, 9. 10.3389/fgene.2018.00344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J, Schmidt J, Fairchild AJ, Porter A, & Roberts JE (2017). Altered sensitivity to social gaze in the FMR1 premutation and pragmatic language competence. Journal of Neurodevelopmental Disorders, 9(1), 31. 10.1186/s11689-017-9211-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraan CM, Hocking DR, Georgiou-Karistianis N, Metcalfe SA, Archibald AD, Fielding J, Trollor J, Bradshaw JL, Cohen J, & Cornish KM (2014). Impaired response inhibition is associated with self-reported symptoms of depression, anxiety, and ADHD in female FMR1 premutation carriers. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 165(1), 41–51. 10.1002/ajmg.b.32203 [DOI] [PubMed] [Google Scholar]
- Landa R, Piven J, Wzorek MM, Gayle JO, Chase GA, & Folstein SE (1992). Social language use in parents of autistic individuals. Psychological Medicine, 22(1), 245–254. 10.1017/S0033291700032918 [DOI] [PubMed] [Google Scholar]
- Landry SH, Smith KE, & Swank PR (2006). Responsive parenting: Establishing early foundations for social, communication, and independent problem-solving skills. Developmental Psychology, 42(4), 627–642. 10.1037/0012-1649.42.4.627 [DOI] [PubMed] [Google Scholar]
- Leckman-Westin E, Cohen PR, & Stueve A (2009). Maternal depression and mother–child interaction patterns: Association with toddler problems and continuity of effects to late childhood. Journal of Child Psychology and Psychiatry, 50(9), 1176–1184. 10.1111/j.1469-7610.2009.02083.x [DOI] [PubMed] [Google Scholar]
- Lindsey EW, Colwell MJ, Frabutt JM, Chambers JC, & MacKinnon-Lewis C (2008). Mother-Child Dyadic Synchrony in European American and African American Families during Early Adolescence. Merrill-Palmer Quarterly, 54(3), 289–315. [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, & Bishop S (2012). Autism diagnostic observation schedule–2nd edition (ADOS-2). Los Angeles, CA: Western Psychological Corporation. [Google Scholar]
- Losh M, Klusek J, Martin GE, Sideris J, Parlier M, & Piven J (2012). Defining genetically meaningful language and personality traits in relatives of individuals with fragile X syndrome and relatives of individuals with autism. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 159B(6), 660–668. 10.1002/ajmg.b.32070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunkenheimer E, Kemp CJ, Lucas‐Thompson RG, Cole PM, & Albrecht EC (2017). Assessing Biobehavioural Self-Regulation and Coregulation in Early Childhood: The Parent-Child Challenge Task. Infant and Child Development, 26(1), e1965. 10.1002/icd.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDuffie A, Machalicek W, Bullard L, Nelson S, Mello M, Tempero-Feigles R, Castignetti N, & Abbeduto L (2016). A Spoken Language Intervention for School-Aged Boys with fragile X Syndrome. American Journal on Intellectual and Developmental Disabilities, 121(3), 236–265. 10.1352/1944-7558-121.3.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsmond GI, Lin L-Y, & Seltzer MM (2007). Mothers of adolescents and adults with autism: Parenting multiple children with disabilities. Intellectual and Developmental Disabilities, 45(4), 257–270. 10.1352/1934-9556(2007)45[257:MOAAAW]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Orsmond GI, Seltzer MM, Greenberg JS, & Krauss MW (2006). Mother–child relationship quality among adolescents and adults with autism. American Journal on Mental Retardation, 111(2), 121–137. 10.1352/0895-8017(2006)111[121:MRQAAA]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Parr JR, Gray L, Wigham S, McConachie H, & Couteur AL (2015). Measuring the relationship between the parental Broader Autism Phenotype, parent–child interaction, and children’s progress following parent mediated intervention. Research in Autism Spectrum Disorders, 20, 24–30. 10.1016/j.rasd.2015.07.006 [DOI] [Google Scholar]
- Roberts JE, Bailey DB, Mankowski J, Ford A, Sideris J, Weisenfeld LA, Heath TM, & Golden RN (2009). Mood and anxiety disorders in females with the FMR1 premutation. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 150B(1), 130–139. 10.1002/ajmg.b.30786 [DOI] [PubMed] [Google Scholar]
- Roberts JE, Ezell JE, Fairchild AJ, Klusek J, Thurman AJ, McDuffie A, & Abbeduto L (2018). Biobehavioral composite of social aspects of anxiety in young adults with fragile X syndrome contrasted to autism spectrum disorder. American Journal of Medical Genetics, Part B: Neuropsychiatric Genetics, 177(7), 665–675. 10.1002/ajmg.b.32674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Tonnsen BL, McCary LM, Ford AL, Golden RN, & Bailey DB Jr (2016). Trajectory and predictors of depression and anxiety disorders in mothers with the FMR1 premutation. Biological Psychiatry, 79(10), 850–857. 10.1016/j.biopsych.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers AY (1993). The assessment of variables related to the parenting behavior of mothers with young children. Children and Youth Services Review, 15(5), 385–402. 10.1016/0190-7409(93)90011-W [DOI] [Google Scholar]
- Roid GH, & Miller LJ (1997). Leiter international performance scale-revised (Leiter-R). Wood Dale, IL: Stoelting. [Google Scholar]
- Sabaratnam M, Murthy NV, Wijeratne A, Buckingham A, & Payne S (2003). Autistic-like behaviour profile and psychiatric morbidity in Fragile X Syndrome. European Child & Adolescent Psychiatry, 12(4), 172–177. 10.1007/s00787-003-0333-3 [DOI] [PubMed] [Google Scholar]
- Sameroff A, Chandler M, & others. (1975). Reproductive risk and the continuum of caretaking casualty. Review of Child Development Research, 4, 187–244. [Google Scholar]
- Sameroff A, & Fiese B (2000). Transactional regulation: The developmental ecology of early intervention. Handbook of Early Childhood Intervention, 2, 135–159. [Google Scholar]
- Schneider A, Hagerman RJ, & Hessl D (2009). Fragile X syndrome—From genes to cognition. Developmental Disabilities Research Reviews, 15(4), 333–342. 10.1002/ddrr.80 [DOI] [PubMed] [Google Scholar]
- Schneider A, Johnston C, Tassone F, Sansone S, Hagerman RJ, Ferrer E, Rivera SM, & Hessl D (2016). Broad autism spectrum and obsessive–compulsive symptoms in adults with the fragile X premutation. The Clinical Neuropsychologist, 30(6), 929–943. 10.1080/13854046.2016.1189536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S, Houweling JEG, Gommlich-Schneider S, Klein C, Nündel B, & Wolke D (2009). Effect of maternal panic disorder on mother–child interaction and relation to child anxiety and child self-efficacy. Archives of Women’s Mental Health, 12(4), 251–259. 10.1007/s00737-009-0072-7 [DOI] [PubMed] [Google Scholar]
- Schworer E, Fidler DJ, Lunkenheimer E, & Daunhauer LA (2019). Parenting behaviour and executive function in children with Down syndrome. Journal of Intellectual Disability Research, 63(4), 298–312. 10.1111/jir.12575 [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Floyd FJ, Song J, Greenberg JS, & Hong J (2011). Midlife and Aging Parents of Adults with Intellectual and Developmental Disabilities: Impacts of Lifelong Parenting. American Journal on Intellectual and Developmental Disabilities, 116(6), 479–499. 10.1352/1944-7558-116.6.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton AL, Cornish K, Kraan C, Georgiou-Karistianis N, Metcalfe SA, Bradshaw JL, Hocking DR, Archibald AD, Cohen J, Trollor JN, & Fielding J (2014). Exploring inhibitory deficits in female premutation carriers of fragile X syndrome: Through eye movements. Brain and Cognition, 85, 201–208. 10.1016/j.bandc.2013.12.006 [DOI] [PubMed] [Google Scholar]
- Siller M, & Sigman M (2002). The behaviors of parents of children with autism predict the subsequent development of their children’s communication. Journal of Autism and Developmental Disorders, 32(2), 77–89. 10.1023/A:1014884404276 [DOI] [PubMed] [Google Scholar]
- Skinner M, Hooper S, Hatton DD, Roberts J, Mirrett P, Schaaf J, Sullivan K, Wheeler A, & Bailey DB (2005). Mapping nonverbal IQ in young boys with fragile X syndrome. American Journal of Medical Genetics Part A, 132A(1), 25–32. 10.1002/ajmg.a.30353 [DOI] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, Seltzer MM, & Hong J (2008). Symptoms and Behavior Problems of Adolescents and Adults With Autism: Effects of Mother–Child Relationship Quality, Warmth, and Praise. American Journal on Mental Retardation, 113(5), 387–402. 10.1352/2008.113:387-402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprinkle SD, Lurie D, Insko SL, Atkinson G, Jones GL, Logan AR, & Bissada NN (2002). Criterion validity, severity cut scores, and test-retest reliability of the Beck Depression Inventory-II in a university counseling center sample. Journal of Counseling Psychology, 49(3), 381–385. 10.1037/0022-0167.49.3.381 [DOI] [Google Scholar]
- Sterling AM, & Warren SF (2014). Maternal Responsivity in Mothers of Young Children with Down Syndrome. Developmental Neurorehabilitation, 17(5), 306–317. 10.3109/17518423.2013.772671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling AM, Warren SF, Brady N, & Fleming K (2013). Influences on Maternal Responsivity in Mothers of Children With Fragile X Syndrome. American Journal on Intellectual and Developmental Disabilities, 118(4), 310–326. 10.1352/1944-7558-188.4.310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern YS, Maltman N, & Roberts MY (2017). The Influence of Maternal Pragmatics on the Language Skills of Children with Autism. Journal of Developmental and Behavioral Pediatrics : JDBP, 38(5), 339–344. 10.1097/DBP.0000000000000445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamis-LeMonda Bornstein, & Baumwell. (2001). Maternal responsiveness and children’s achievement of language milestones. Child Development, 72(3), 748–767. 10.1111/1467-8624.00313 [DOI] [PubMed] [Google Scholar]
- Tassone F, Hagerman PJ, & Hagerman RJ (2014). Fragile X Premutation. Journal of Neurodevelopmental Disorders, 6(1), 22. 10.1186/1866-1955-6-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren, Brady N, Sterling A, Fleming K, & Marquis J (2010). Maternal Responsivity Predicts Language Development in Young Children With Fragile X Syndrome. American Journal on Intellectual and Developmental Disabilities, 115(1), 54–75. 10.1352/1944-7558-115.1.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler A, Hatton D, Reichardt A, & Bailey D (2007). Correlates of maternal behaviours in mothers of children with fragile X syndrome. Journal of Intellectual Disability Research : JIDR, 51(Pt. 6), 447–462. 10.1111/j.1365-2788.2006.00896.x [DOI] [PubMed] [Google Scholar]
- Williams KT (2007). Expressive vocabulary test second edition (EVT™ 2). J. Am. Acad. Child Adolesc. Psychiatry [Google Scholar]


