Why should all clinicians address physical activity participation after stroke?
Physical activity is essential for all stroke survivors, it reduces blood pressure and cholesterol, supports weight management and contributes to better brain health and recovery after stroke.1 Physical activity also supports secondary prevention in stroke and cardiovascular disease. One in three stroke survivors experience another stroke within five years and half of those who survive 5–10 years will die of recurrent stroke or other cardiovascular pathology.2 Effective multi-modal approaches to secondary prevention are vital. In a study of stroke survivors medically managed for their risk factors, physical inactivity was the strongest independent predictor of recurrent stroke.3 These data indicate physical inactivity is a critical risk factor to address, and importantly it is modifiable. Physical activity must be addressed and integrated as part of effective stroke rehabilitation and secondary stroke prevention.
The 2020 World Health Organisation guidelines for healthy adults and adults living with a disability recommend undertaking 150–300 minutes of moderate intensity physical activity each week and minimising sedentary behaviour. These exercise targets are promoted for people with stroke by the American Stroke Association, Australian Clinical Guidelines for Stroke Management and Canadian Stroke Best Practices. The American Stroke Association recommendations for stroke survivors suggest 20–60 minutes of aerobic exercise three to five days per week.4 After a stroke achieving the World Health Organisation physical activity targets can be difficult. Lower exercise volumes and intensities may be more sustainable and achievable, while still conferring health benefits. However, as a global stroke community we must aspire to achieving recommended physical activity targets as more physical activity is better for health.
Stroke survivors do not undertake sufficient physical activity to meet recommendations. A meta-analysis demonstrated that on average stroke survivors achieve only 63% of the recommended steps/day for people with a disability (4078 vs 6,500–8,500).5 Activity levels remain low long-term after stroke and adherence to cardiovascular recommendations decreases over time.6 Proposed reasons for low physical activity levels post-stroke vary. Physical impairments experienced by stroke survivors such as weakness, poor fitness and balance impact mobility and physical activity. However, physical ability alone does not explain physical inactivity; stroke survivors who have few physical difficulties do not undertake recommended levels of physical activity.5 Other factors that impact physical activity participation include mood, motivation, finances and caregiver support. Given the various factors that influence physical activity after stroke, all clinicians involved in stroke recovery and rehabilitation have a role to play in increasing physical activity participation.
Future research in physical activity after stroke–Tips for early career researchers
With greater attention to defining “knowledge units” as part of stroke recovery trial development recommended,7 considering the “who, what, how much and when” of decisions for physical activity interventions could serve to support new trials, and subsequently practice guidelines. Stroke survivors are not homogenous; thus accurately identifying the “who” or “responders” to specific interventions is important. Identification of the “active ingredients” or the “what” of a physical activity intervention is also key. While meta-analyses of stroke exercise trials show positive effects of interventions during the active, supported phase, rarely are exercise effects sustained post-intervention, and none translate to sustained increases in physical activity levels. To enhance engagement and sustainability, physical activity programs should be designed and personalised to the person’s ability, goals and preferences. The addition of self-management and behavior change strategies to encourage a life-long habits will be key for success. Involving stroke survivors, carers and clinicians in designing physical activity interventions will optimise engagement and sustainable uptake.
Many questions remain about physical activity prescription, particularly “how much” for secondary stroke prevention. Is 150 minutes/week required to reduce risk? Is it important for stroke survivors to achieve moderate intensity when they exercise? Perhaps light physical activity is sufficient and more feasible? The first step is to define the “dose” of physical activity, specifically intensity and duration, required for cardiovascular benefit. Understanding “when” is the best time to intervene is also vital. Most physical activity studies occur in chronic stroke, long after habits and behaviors are well established. Earlier intervention targeting physical activity behaviour change may be key.4 Stroke clinicians should work collaboratively with stroke survivors to determine an appropriate and achievable physical activity dosage while keeping recommendations in mind.
Breakthroughs in this field will come with strong interdisciplinary and patient partnerships– building the tools to collaborate, effectively engage and co-design with a range of stakeholders will help to produce research that is clinically meaningful and relevant. Mentors are important during all phases of a research career, but it can be challenging to identify the right mentor during the the early career phase.. Many national stroke organisations offer support for early career researchers. Internationally, the European Stroke Organisation has a young stroke physicians and researchers group and for those focused on rehabilitation there is the newly created International Stroke Recovery and Rehabilitation Alliance. The alliance includes people interested in stroke recovery research and clincial practice from all continents and career levels, including world leaders in the field and is a potential forum to find both mentors and collaborators. Getting involved in national or global stroke recovery collaborations provides dual benefits of advancing the field and building your career.
To summarise:
Find a mentor in the field.
Be open to collaboration.
Build or become part of a team that includes a range of clinical and research stakeholders, including stroke consumers.
Learn how to effectively communicate and co-design with stroke consumers and clinicians.
Use thoughtful frameworks to help guide your research approach (e.g. Stroke Recovery and Rehabilitation Roundtable Trials Development Framework7)
Tips for incorporating physical activity into your current stroke rehabilitation clinical practice
So, what do we do now while we wait for better guidance about the who, what, how much and when of physical activity prescription after stroke? Stroke survivors interact with a range of health professionals: neurologists, general practitioners, nurses, allied health and exercise professionals. All health professionals working in stroke should have working knowledge of physical activity guidelines and when to refer on to those with expertise. From a health professional perspective, simply advising people with stroke to adhere to physical activity guidelines is inadequate.8 Are there current models of care that can be adapted to help us support and empower patients to make physical activity a part of their lives?
Can we learn from other chronic disease groups? For example, cardiac rehabilitation has been shown to be appropriate for, and effective at, reducing cardiovascular risk, yet few people with stroke participate in these programs. Specifically, tailoring programs for stroke survivors improves attendance at cardiac rehabilitation programs.9 Cardiac rehabilitation models warrant further investigation given their ability to reduce cardiovascular risk. Whether these programs translate into sustained participation in physical activity is yet to be proven.
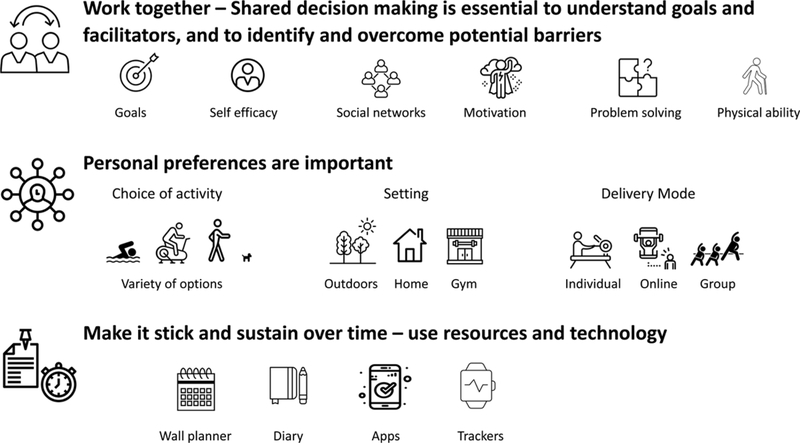
Stroke clinical practice guidelines are increasingly recommending specific attention to cardiorespiratory fitness and physical activity. However, too often physical rehabilitation commonly focuses on impairments and activity limitations and often fails to address participation. Some good examples of physical activity programs for stroke survivors exist,10 but proven approaches to developing sustainable exercise behaviors do not. Once stroke survivors go home, medical general practitioners often have tools to help them subjectively assess and provide basic physical activity counselling to patients, however this is unlikely to be stroke-specific, where a tailored approach is required. In the World Stroke Organisation’s Post Stroke Checklist, leisure, activities, hobbies and work are considered in the ‘life after stroke item’, with referral to a stroke support group or association the action item when a need is identified. Peer support can be game-changing for some survivors, however specific education, practical support and tools are needed in the area of physical activity. We know that stroke survivors have individual preferences, barriers and facilitators to physical activity. These need to be understood and individual solutions worked through in partnership with the clinician and stroke survivor. For an individual who faces many barriers to commencing physical activity, (which is common in stroke), referrals should be made to clinicians who are experts in physical activity and stroke (e.g., neurological physical therapists). These individuals have the knowledge and skills needed to prescribe and monitor a personalised physical activity program. However, even experts struggle to implement physical activity recommendations and thus we need evidence-based implementation strategies. We know that for a physical activity intervention to be sustained the stroke survivor must be central and a key driver of the program. Together clinicians and stroke survivors should explore barriers and facilitators which, if addressed, will likely improve uptake. There are many personalisation factors to be explored that may facilitate physical activity participation: the physical activity messaging provided, type of physical activity, setting and delivery mode, possible use of technology and choice of behavior change and self-management strategies. The clinician’s role is to support and counsel, scaffold with friends and family, and most importantly help to build confidence and self-efficacy. Figure 1 shows examples of topics to explore when addressing physical activity with stroke survivors. As our suite of proven interventions grows, we need to promptly develop user-friendly clinician guides, tools, and funding models to enable rapid translation and uptake.
Figure 1:
Tips for addressing physical activity participation when working with stroke survivors
Conclusion
Physical activity is fundamentally important for many aspects of health and well-being along with secondary prevention of stroke. Hopefully in the future we will have better guidance on physical activity prescription and interventions for stroke survivors, but for now it is clear that a personalised approach is warranted. All stroke clinicians play an important role in encouraging and empowering stroke survivors to become physically active and make physical activity a part of their everyday lives.
Funding Sources/Disclosures:
Dr Fini: University of Melbourne ECR grant.
Professor Bernhardt: NHMRC Fellowship.
The Florey Institute of Neuroscience and Mental Health acknowledges strong support from the Victorian Government; in particular the Operational Infrastructure Support Grant.
References
- 1.D’Isabella NT, Shkredova DA, Richardson JA, Tang A. Effects of exercise on cardiovascular risk factors following stroke or transient ischemic attack: a systematic review and meta-analysis. ClinRehabil.2017;31:1561–1572. [DOI] [PubMed] [Google Scholar]
- 2.Hardie K, Hankey GJ, Jamrozik K, Broadhurst RJ, Anderson C. Ten-Year Survival After First-Ever Stroke in the Perth Community Stroke Study. Stroke.2003;34:1842–1846. [DOI] [PubMed] [Google Scholar]
- 3.Turan TN, Nizam A, Lynn MJ, Egan BM, Le NA, Lopes-Virella MF, Hermayeret KL, Harrell J, Derdeyn CP, Fiorella D et al. Relationship between risk factor control and vascular events in the SAMMPRIS trial. Neurology.2017;88:379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Billinger SA, Arena R, Bernhardt J, Eng JJ., Franklin BA, Johnson CM, Mackay-Lyons M, Macko RF, Mead GE, Roth E et al. Physical Activity and Exercise Recommendations for Stroke Survivors: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke.2014;45:2532–2553. [DOI] [PubMed] [Google Scholar]
- 5.Fini NA, Holland AE, Keating J, Simek J, Bernhardt J. How Physically Active Are People Following Stroke? Systematic Review and Quantitative Synthesis. PhysTher.2017;97:707–717. [DOI] [PubMed] [Google Scholar]
- 6.Fini NA, Bernhardt J, Churilov L, Clark R, Holland AE. Adherence to physical activity and cardiovascular recommendations during the 2years after stroke rehabilitation discharge. AnnPhysRehabilMed.2021;64:101455. [DOI] [PubMed] [Google Scholar]
- 7.Bernhardt J, Hayward KS, Dancause N, Lannin NA, Ward NS, Nudo RJ, Farrin A, Churilov L, Boyd LA, Jones TA et al. A Stroke Recovery Trial Development Framework: Consensus-Based Core Recommendations from the Second Stroke Recovery and Rehabilitation Roundtable. IntJStroke.2019;14:792–802. [DOI] [PubMed] [Google Scholar]
- 8.Boysen G, Krarup LH, Zeng X, Oskedra A, Korv J, Anderson G, Gluud C, Pederson A, Lindahl M, Hansen L et al. , ExStroke Pilot Trial of the effect of repeated instructions to improve physical activity after ischaemic stroke: a multinational randomised controlled clinical trial. BMJ,2009;339:b2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marzolini S, Fong K, Jagroop D, Neirinckx J, Liu J, Reyes R, Grace SL, Oh P, Colella TJF. Eligibility, Enrollment, and Completion of Exercise-Based Cardiac Rehabilitation Following Stroke Rehabilitation: What Are the Barriers? PhysTher.2020;100:44–56. [DOI] [PubMed] [Google Scholar]
- 10.van Wijck F, Bernhardt J, Billinger SA, Bird ML, Eng J, English C, Teixeira-Salmela LF, Mackay-Lyons M, Melifonwu R, Sunneragen KS et al. Improving life after stroke needs global efforts to implement evidence-based physical activity pathways. IntJStroke.2019;14:457–459. [DOI] [PubMed] [Google Scholar]