Abstract
Background & objectives:
During any public health emergency, a need-based national non-communicable diseases (NCD) preparedness plan is essential. People living with NCDs could face challenges owing to restricted mobility, low access to medical care and suboptimal logistics during the pandemic. The present study explored the effect of the COVID-19 pandemic on NCD care in a district of Odisha State of India.
Methods:
This study was carried out during May-June 2020 in the Khurda district of Odisha. A community-based explanatory mixed-method study was followed. Data collection comprised 12 in-depth interviews and 491 structured interviews using Likert-questionnaire with individuals having at least one NCD. Mantel-Haenszel's Chi-square test was used to assess the difference in the effect of COVID-19 on the routine NCD care. Qualitative data were analyzed by content analysis.
Results:
Findings revealed that nearly two-thirds of participants encountered challenges in their routine investigation (69%), day-care procedures (67%) and reaching hospital (61%). Around half of them reported having trouble in doctor appointments (59%), emergency treatment (56%), access to the pharmacy (47%) and delay in healthcare (46%). Thirty seven per cent perceived that they could not access care because of social restriction/lockdown, 29 per cent attributed arranging finance as a constraint to visiting hospitals and 16 per cent avoided going to the hospital, fearing COVID-19 infection.
Interpretation & conclusions:
Our findings showed that people with chronic NCDs faced multiple challenges in accessing health care during the pandemic. A cohesive doctor-pharmacy-patient engagement is vital for managing NCD care during a pandemic. During emergencies, changes in dispensing practices and service provision closer to the patients are crucial. Additionally, health literacy and home-based NCD management should be encouraged.
Keywords: COVID-19, healthcare, long-standing-chronic-condition, multiple chronic diseases, non-communicable diseases, SARS-CoV-2
Non-communicable diseases (NCDs) are usually chronic diseases with long duration1. According to the World Health Organization (WHO), four main types of NCDs are cardiovascular disease (CVD), cancer, chronic respiratory disease (CRD) and diabetes1. Each year, NCD accounts for more than two-thirds of all deaths worldwide, known as a silent global epidemic1,2,3,4. Long-term complications of NCDs often require continuous treatment, which poses new challenges to the healthcare system and creates complications in the prevention and treatment of NCDs4,5.
With the escalating burden of NCDs in India, the presence of multiple NCDs is exacerbating the risk6,7,8. India's Global Burden of Diseases (GBD) study reveals that CVD, CRD and diabetes are the three leading causes of death9. These accounted for a substantial proportion of India's total deaths in 2016 and CVD made an immense contribution to the overall burden (28%). CRD made the second-largest contribution to the overall mortality burden (11%), and diabetes contributed three per cent of the total burden9.
The global spread of COVID-19 has resulted in more than 10 million confirmed cases and about 500 thousand deaths worldwide since the first outbreak till June 202010,11. As a result, the focus of the health system has shifted to the management and control of COVID-19. A rapid survey conducted by the WHO to evaluate NCD care during COVID-19 has found that NCD treatment has been severely impaired in most countries, particularly in countries with severe community transmission12. It has been shown that more than half of the people living with NCD (PLWNCD) in lower-middle-income countries are affected –the increasing trend of COVID-19 may exacerbate the NCD crisis13,14,15,16, as many NCDs are associated with high mortality due to COVID-1917.
Given the substantial magnitude of NCDs, individuals with such chronic care demands may experience challenges related to limited mobility, access to medical care and availability of logistics, particularly during the COVID-19 pandemic. However, there is limited information on the impact of COVID-19 on NCD care in India. This study was, therefore, undertaken to explore the effect of the COVID-19 pandemic on NCD care in a district of Odisha State, India.
Material & Methods
Study design, settings and participants: This explanatory mixed-method study was conducted in the Khurda district of Odisha, India. First, a total of 600 quantitative interviews were conducted using structured questionnaires; after analyzing quantitative data, 12 in-depth interviews (IDIs) were carried out to explore COVID-19 related NCD care challenges if any.
The Odisha State has 41.9 million population18.Bhubaneswar, the capital city, belongs to the Khurda district with a population of 2.3 million and 800/km2 population density. The district has one municipal corporation (Bhubaneswar), two municipalities, two Notified Area Councils and 10 administrative blocks18. The initial COVID-19 cases of Odisha were identified in the district of Khurda19. Since it was one of the worst affected districts in the State, we selected Khurda for our study. Both urban and rural settings of the district were included in our study. The individuals having NCDs (PLWNCD) were identified with the help of community health workers, primary healthcare providers and by a chart review of health registers.
The study was conducted during May-June, 2020 (two months). The ethical clearance was obtained from the ICMR-Regional Medical Research Centre, Bhubaneswar Institutional Ethical Committee, and the State Ethical Review Committee, Department of Health and Family Welfare, Odisha Government. Informed written consent was obtained from the participants before collecting data.
Sample size and sampling: The sample size was determined using Open Epi software (Open Source Epidemiologic Statistics for Public Health, Version 2.3.1). The assumption for sample size calculation was based on population size (N) of 1000000 (for finite population correction factor), 30±5 per cent hypothesized frequency of outcome factor in the population (p), 95 per cent confidence limits (Z1−α/2 = 1.96), precision (d=0.1) and design effect for cluster surveys (DEFF=1.5). The equation for sample size
The required sample size was 484.
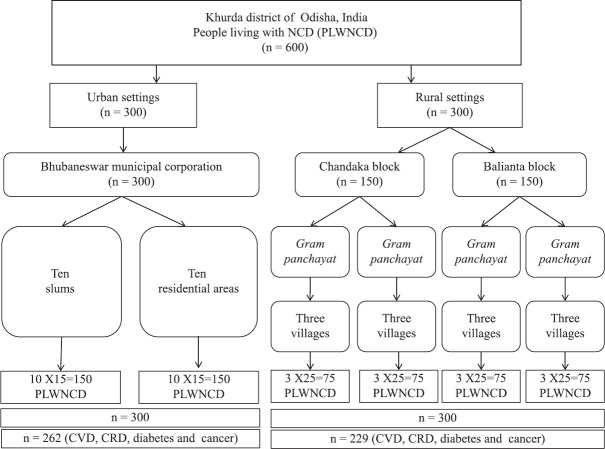
Multi-stage cluster random sampling approaches for data collection were adopted. A total of 600 PLWNCD, 300 each from urban and rural areas, were interviewed. The Bhubaneswar Municipal Corporation was selected for urban settings, and two administrative blocks – Chandaka and Balipatana were chosen for rural interviews. Ten slums and 10 residential areas were randomly selected from this urban setting, and 15 PLWNCD were interviewed from each. Two administrative blocks – Chandaka and Balianta were selected from rural settings, from each block two Gram Panchayat (GP) were further selected and from each GP three villages were randomly selected, and 25 PLWNCD were interviewed from each village. Of the 600 PLWNCD, only those with four NCD conditions – CVD, CRD, diabetes, and cancer (n=491) were included in the study; 229 (47%) were from rural and 262 (53%) urban settings, respectively. The detailed flow chart of the sampling is shown in Fig 1.
Fig. 1.
Flow-chart showing the sampling frame of the study.
Study variables and data collection procedure: The quantitative questionnaire included demographic variables - age, gender, settings, education, occupation and living conditions. The information regarding prevailing NCD conditions was captured. To assess the difficulties experienced in seeking NCD care during pandemic related lockdown (March 24 to May 31, 2020), the Likert scale (not at all, somewhat and very much) was used to collect information. In rural settings and urban slums, face-to-face interviews were conducted while maintaining appropriate COVID-19 norms. However, in urban residential areas, the data were collected by telephone interviews after preparing a line list of households in the sampled zone. Given the strict lockdown in the urban areas, with several containment zones, only telephone interviews were conducted in urban areas. The survey questionnaire was pre-tested before administration, and an agreement of 82 per cent was found between the data collected face-to-face and telephone interviews in the pilot study. Four trained investigators under the direct supervision of the research team were involved in data collection, which spanned from the end of May to the first two weeks of June 2020.
A total of 12 face-to-face IDIs – six in urban and rural settings were conducted to get in-depth information on challenges faced for seeking care during the pandemic and their coping strategies. The participants were selected purposively among the quantitative survey participants.
Data analysis: The quantitative data were entered in EpiInfo (Version 7.2, Centers for Disease Control and Prevention, Atlanta, Georgia, USA), and transferred to Stata 16.0 (Stata Corp. College Station, TX, USA) for statistical analysis. Frequency (n) and percentage (%) were used for categorical variables, mean, and the range was used for numerical variables. The Mantel–Haenszel Chi-square test was used to assess the substantial difference in the impact of COVID-19 on the routine NCD care among the people living with single and more than one NCD conditions after adjusting the residential areas (urban and rural) of the participants. For qualitative data, the digitally recorded interviews were transcribed, translated and coded using MAXQDA software (MAXQDA Analytics Pro 2020, VERBI GmbH Berlin, Germany). The content analysis approach was used for data analysis.
Results
A total of 491 individuals having at least one NCD participated in this study. Among the participants, 51 per cent (n=252) were males. The mean age of participants was 56±14.3 yrs, ranging from 18 to 77 yrs; with 75 per cent belonging to 46-70 yrs age bracket. The demographic characteristics of the participants are given in Table I.
Table I.
Demographic characteristics of study participants (n=491)
| Demographic characteristics | Urban (n=262), n (%) | Rural (n=229), n (%) | Total (n=491), n (%) |
|---|---|---|---|
| Sex | |||
| Female | 128 (49) | 111 (49) | 239 (49) |
| Male | 134 (51) | 118 (51) | 252 (51) |
| Age group (yr) | |||
| 18-35 | 25 (9) | 3 | 43 (9) |
| 36-45 | 23 (9) | 14 (6) | 37 (7) |
| 46-70 | 196 (75) | 180 (79) | 376 (77) |
| >70 | 18 (7) | 17 (7) | 35 (7) |
| Education | |||
| No formal schooling | 27 (10) | 63 (28) | 90 (18) |
| Primary (1st-7th) | 31 (12) | 76 (33) | 107 (22) |
| High school (8th-12th) | 74 (28) | 62 (27) | 136 (28) |
| Graduation and above | 130 (50) | 28 (12) | 158 (32) |
| Occupation | |||
| Unskilled workers | 10 (4) | 25 (11) | 35 (7) |
| Skilled workers | 4 (1) | 8 (3) | 12 (2) |
| Business | 30 (12) | 13 (6) | 43 (9) |
| Profession (government/private employee) | 78 (30) | 18 (8) | 96 (20) |
| Homemaker | 76 (29) | 101 (44) | 177 (36) |
| Student | 11 (4) | 8 (3) | 19 (4) |
| Farmers | 0 | 43 (19) | 43 (9) |
| Retired employee | 53 (20) | 13 (6) | 66 (13) |
| Family environment | |||
| Living alone | 9 (4) | 3 (1) | 12 (2) |
| Married and living with spouse | 58 (22) | 7 (3) | 65 (13) |
| Living with children/other family members | 195 (74) | 219 (96) | 414 (84) |
The major NCD conditions observed were CVD 58 per cent (n=285), diabetes 51 per cent (n=255), CRD and cancer 10 per cent (n=49) each (Fig. 2). A total of 27 per cent (n=135) had two NCD conditions, and one per cent (n=4) had three NCD conditions.
Fig. 2.
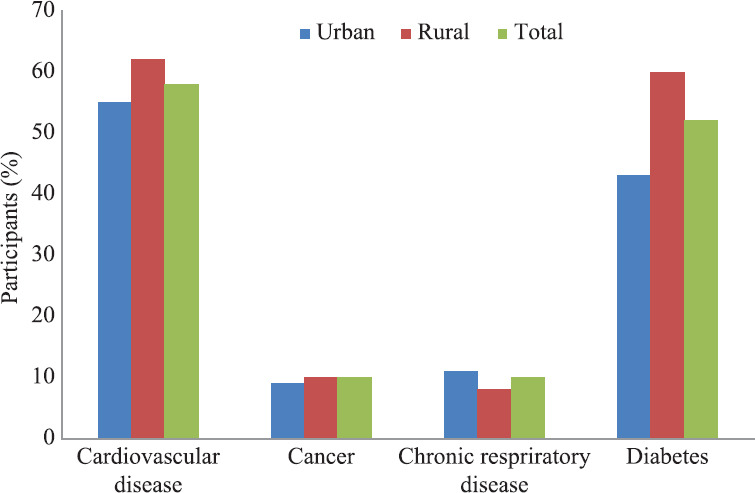
Percentage of participants with four major non-communicable diseases in urban and rural setting.
The effect of the COVID-19 pandemic on routine care activities among individuals with NCDs is presented in Table II. The findings indicated that 36 per cent of interviewees had some to a substantial effect on their routine treatment. Around one-third reported their daily diet, physical activity and routine health check-up to be affected. About one-fourth had changed their prescheduled appointment with physicians and discontinued treatment. Those living in urban areas with more than one NCD condition reported a significantly higher challenge in having doctor's consultation compared to those living in rural areas with a single NCD condition (P=0.014). Similarly, urban-dwelling individuals with multiple NCD conditions had substantially discontinued care (P=0.006) compared to their counterparts with a single NCD residing in rural settings. Overall, 35 per cent (n=171) felt the need for emergency hospitalization, which was significantly higher for participants with more than one NCD (multimorbidity) vis-à-vis those with single NCD.
Table II.
Impact of COVID-19 pandemic on daily routine activities among people living with non-communicable diseases (NCDs)
| Routine care of NCDs | Single NCD (n=352) | >1 NCD (n=139) | Mantel-Haenszel Chi-square, P | ||
|---|---|---|---|---|---|
|
|
|
||||
| Urban (n=177), n (%) | Rural (n=175), n (%) | Urban (n=85), n (%) | Rural (n=54), n (%) | ||
| Daily routine has been affected | |||||
| Not at all | 103 (58) | 126 (72) | 49 (57) | 34 (63) | 0.397 |
| Somewhat | 49 (28) | 45 (26) | 27 (32) | 16 (30) | |
| Very much | 25 (14) | 4 (2) | 9 (11) | 4 (7) | |
| Change in physical activity | |||||
| Not at all | 101 (57) | 133 (76) | 53 (62) | 31 (57) | 0.327 |
| Somewhat | 58 (33) | 39 (22) | 27 (32) | 21 (39) | |
| Very much | 18 (10) | 3 (2) | 5 (6) | 2 (4) | |
| Change in diet | |||||
| Not at all | 123 (69) | 128 (73) | 53 (62) | 37 (68) | 0.191 |
| Somewhat | 40 (23) | 45 (26) | 23 (27) | 16 (30) | |
| Very much | 14 (8) | 2 (1) | 9 (11) | 1 (2) | |
| Any discontinuation in treatment | |||||
| Not at all | 125 (71) | 132 (76) | 48 (57) | 35 (65) | 0.006 |
| Somewhat | 37 (21) | 34 (19) | 18 (21) | 13 (24) | |
| Very much | 15 (8) | 9 (5) | 19 (22) | 6 (11) | |
| Change in doctor consultation | |||||
| Not at all | 129 (73) | 143 (82) | 53 (62) | 38 (70) | 0.014 |
| Somewhat | 35 (20) | 19 (11) | 14 (17) | 10 (19) | |
| Very much | 13 (7) | 13 (7) | 18 (21) | 6 (11) | |
| Change in routine check-up | |||||
| Not at all | 107 (61) | 131 (75) | 54 (64) | 32 (59) | 0.321 |
| Somewhat | 45 (25) | 24 (14) | 17 (20) | 13 (24) | |
| Very much | 25 (14) | 20 (11) | 14 (16) | 9 (17) | |
| Coping through difficulty times | |||||
| Managed easily | 96 (54) | 108 (62) | 42 (49) | 27 (50) | 0.124 |
| Managed with difficulty | 81 (46) | 67 (38) | 43 (51) | 27 (50) | |
| Felt urgent need for hospital visit | |||||
| No | 126 (71) | 114 (65) | 46 (54) | 34 (63) | 0.024 |
| Yes | 51 (29) | 61 (35) | 39 (46) | 20 (37) | |
Table III presents the effect of the COVID-19 pandemic on NCDs treatment among participants who felt an urgent need for a hospital visit during the lockdown period. Findings revealed that nearly two-thirds of participants encountered difficulties in their routine investigation (69%, n=118), day-care procedures like dialysis (67%, n=115), and reaching hospital (61%, n=105). Around half of them reported having constraints in doctor appointments (59%, n=104), emergency treatment (56%, n=96), access to the pharmacy (47%, n=80) and reported a delay in health care (46%, n=79). Respondents with multimorbidity (the presence of more than one chronic condition) residing in urban areas expressed substantially higher problems than individuals having a single condition and residing in rural areas (P=0.026).
Table III.
Impact of COVID-19 pandemic on non-communicable diseases (NCDs) care among the participants those who felt urgent need of hospital visit during lockdown period (n=171)
| Challenge during COVID-19 for NCD care | Single NCD (n=112) | >1 NCD (n=59) | Mantel-Haenszel, Chi-square, P | ||
|---|---|---|---|---|---|
|
|
|
||||
| Urban (n=51), n (%) | Rural (n=61), n (%) | Urban (n=39), n (%) | Rural (n=20), n (%) | ||
| Face difficulty in doctor appointment | |||||
| Not at all | 14 (27) | 30 (49) | 19 (49) | 7 (35) | 0.392 |
| Somewhat | 21 (41) | 22 (36) | 13 (33) | 8 (40) | |
| Very much | 16 (32) | 9 (15) | 7 (18) | 5 (25) | |
| Face difficulty in getting medicine | |||||
| Not at all | 22 (43) | 33 (54) | 27 (69) | 8 (40) | 0.234 |
| Somewhat | 22 (43) | 20 (33) | 10 (26) | 11 (55) | |
| Very much | 7 (14) | 8 (13) | 2 (5) | 1 (5) | |
| Face difficulty in getting investigations | |||||
| Not at all | 15 (29) | 24 (39) | 5 (13) | 9 (45) | 0.305 |
| Somewhat | 20 (39) | 22 (36) | 7 (18) | 8 (40) | |
| Very much | 16 (31) | 15 (25) | 27 (69) | 3 (15) | |
| Feel difficulty in getting any day-care | |||||
| Not at all | 13 (25) | 32 (53) | 4 (10) | 7 (35) | 0.026 |
| Somewhat | 30 (59) | 13 (21) | 26 (67) | 7 (35) | |
| Very much | 8 (16) | 16 (26) | 9 (23) | 6 (30) | |
| Feel difficulty in emergency care | |||||
| Not at all | 20 (39) | 26 (42) | 22 (56) | 8 (40) | 0.264 |
| Somewhat | 19 (37) | 23 (38) | 12 (31) | 11 (55) | |
| Very much | 12 (24) | 12 (20) | 5 (13) | 1 (5) | |
| Feel difficulty in reaching the hospital | |||||
| Not at all | 22 (43) | 24 (39) | 20 (51) | 1 (5) | 0.256 |
| Somewhat | 18 (35) | 26 (43) | 16 (41) | 16 (80) | |
| Very much | 11 (22) | 11 (18) | 3 (8) | 3 (15) | |
| Experience delay in seeking care | |||||
| Not at all | 27 (53) | 36 (59) | 21 (54) | 8 (40) | 0.383 |
| Somewhat | 17 (33) | 17 (28) | 16 (41) | 8 (40) | |
| Very much | 7 (14) | 8 (13) | 2 (5) | 4 (20) | |
The most frequently encountered and major care challenges reported by the participants are depicted. According to participants, during the COVID-19 pandemic, diagnostic services (n=187, 38%) were among the most significant barriers towards seeking treatment; doctor consultation (n=93, 19%) was the second most experienced challenge. Around 15 per cent (n=74) faced problems accessing emergency care; while 14 per cent (n=69) had some difficulties either in visiting hospitals, and/or purchasing medicines. Approximately 37 per cent (n=182) perceived that they were not able to take care of their chronic illnesses because of the prevailing social restriction/lockdown, 29 per cent (n=142) reported financial arrangement as a constraint towards visiting hospitals and 16 per cent (n=79) feared going to hospital apprehending of getting COVID-19 infection. It was found that family network was the primary source of support among the respondents (96%); and about three per cent relied on their friends and neighbours.
Qualitative findings revealed that before the onset of the pandemic, participants managed their NCD conditions by routinely visiting hospitals or physicians. Almost all considered their routine treatment as a lesser priority during the pandemic compared to the threat of COVID-19. Besides, the fear of being infected with COVID-19 modulated their healthcare decision-making. Further, they were cognizant of their increased vulnerability through mass media and public messages and thus were discouraged for social contact by their family members; the hospital was regarded by most as ‘a hotspot for infection’. Patients with some form of respiratory infection or fever were treated with high suspicion, and they underwent COVID-19 screening. Diagnostic facilities were generally avoided.
Most respondents declined or postponed regular appointments wherever possible. Regarding the management of their illnesses during the pandemic-related lockdown period, many confided that they either continued the same medicine or adjusted the doses according to their symptoms. Some avoided large hospitals for consultation, preferring a small private clinic or pharmacist shop or village doctors (informal healthcare providers). However, some urban participants tried to substitute their routine check-ups by self-care measures like monitoring their blood glucose using test strips and blood pressure with the help of family members or neighbours.
Some participants tried to avail teleconsultation or consulted their physicians through telephone or internet-based platforms. However, non-availability of their health records and background information on treatment was the major challenge while approaching a new physician on a telemedicine platform.
Discussion
Almost half of the participants had difficulties in managing their NCD-related care. Diagnostic services, physician consultation, transport arrangements, financial constraints, mandatory self-isolation, the need for social distancing and fear of visiting hospitals for risk of COVID-19 infections were the major perceived challenges. Telemedicine-enabled healthcare and home-based self-care emerged as alternate strategies for managing chronic illnesses during the pandemic.
In general, the COVID-19 pandemic has significantly affected continuing care for individuals with chronic health conditions. Physical and social distancing also led to inferior management of NCD risk factors14,17,21,22,23. Evidence from previous public health catastrophes and COVID-19 suggests that chronic illnesses may worsen by prevailing economic circumstances and changes in everyday health behaviour23,24. PLWNCDs are at risk for adverse health consequences in emergency situations17,21. Thus, addressing NCDs is an integral component of the planning for COVID-19 and future public health emergencies17,21,22,23,24. In addition, the views of caregivers and healthcare professionals are essential in the Pandemic Response Plans to ensure that the needs of patients are addressed3,25,26. According to the WHO survey also, the COVID-19 pandemic showed severe impact on the NCD services27.
Previous studies in Odisha found that one-third of patients attending primary care settings had multiple chronic conditions (two or more)28,29,30,31. Similar findings have been observed in a chart review of the morbidity profile of urban primary care patients29. Studies have documented the challenges in care-seeking for chronic illnesses like cancer and rheumatoid arthritis32,33,34,35. During pandemic situations, these challenges become accentuated due to the prevailing conditions and patient safety concerns.
People living in urban areas had different challenges compared to rural areas. In particular, three factors intensify the complexities of NCD care. The first was that initially, COVID-19 cases were found in urban areas, and after that, strict implementation of the lockdown followed23,24. Second, many rural patients depend on the public health care system, while most urban patients generally prefer private practitioners/clinics. Third, rural areas have a stronger social network and support system, acting as facilitators for NCD self-management during pandemic26,27,28,29,30,31,32,33.
As chronic NCDs involve continuous engagement with healthcare providers; there is also a need to explore different ways by which physicians may manage their chronic disease patients during the pandemic. During any public health catastrophe, the elderly and the patients with mental illness are affected the most36. Hence, in-depth exploration of these particular subgroups of patients mandates special attention.
The National Health Policy-2017 in India stressed digitalization in the healthcare sector37. In August 2020, the National Digital Health Mission (NDHM) was launched in India to achieve universal health coverage38 and which aims to build a holistic and inclusive digital health environment to streamline healthcare delivery. Therefore, telemedicine-enabled healthcare with disease-specific virtual clinic is a pre-requisite for contactless physician-patients interaction. Digital/electronic records are critical for future pandemic preparedness plans. However, digitization is not the only solution, but only one of the components of the overall pandemic response strategy. Therefore, a decentralized network of doctor-pharmacy-patients is necessary to tackle the NCD treatment needs during public health emergencies.
Prioritizing and improving home-based or self-care for NCDs along with health literacy and community- health-entrepreneurship model could be another strategy. Community-based NCD care through patient activation needs to be promoted.
The study had some limitations. Due to pandemic situation an explanatory design was adopted. We had smaller sample size for quantitative data. It was difficult to measure the true impact of COVID-19 on NCD care as the information on the actual deterioration of conditions was lacking. A control group of people not having NCD would have made the study more meaningful.
In conclusion, our study showed that people with two or more chronic NCDs (multimorbidity) encountered more challenges, thus future studies should focus on individuals’ challenges with managing multimorbidity during COVID-19. A cohesive doctor-pharmacy-patient engagement is vital for managing NCD care during a pandemic. During emergencies, changes in dispensing practices such as duration and person, and service provision closer to the patient are crucial. Additionally, community NCD care-related health literacy and community health entrepreneurship model, including home-based NCD treatment, should be encouraged.
Acknowledgment:
The authors thank to all the study participants for sharing their valuable experiences. and acknowledge the support of the field team in the data collection process and the State Health and Family Welfare department, Odisha, for facilitating the study.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.World Health Organization. Non-communicable diseases country profiles. 2018. [accessed on May 7, 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases .
- 2.Kathirvel S. Sustainable development goals and non-communicable diseases: Roadmap till 2030 –A plenary session of world non-communicable diseases congress 2017. Int J Noncommun Dis. 2018;3:3. [Google Scholar]
- 3.Nugent R, Bertram MY, Jan S, Niessen LW, Sassi F, Jamison DT, et al. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet. 2018;391:2029–35. doi: 10.1016/S0140-6736(18)30667-6. [DOI] [PubMed] [Google Scholar]
- 4.Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob Health. 2017;5:e277–89. doi: 10.1016/S2214-109X(17)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lopez AD, Williams TN, Levin A, Tonelli M, Singh JA, Burney PG, et al. Remembering the forgotten non-communicable diseases. BMC Med. 2014;12:200. doi: 10.1186/s12916-014-0200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arokiasamy P. India's escalating burden of non-communicable diseases. Lancet Glob Health. 2018;6:e1262–3. doi: 10.1016/S2214-109X(18)30448-0. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee A. Noncommunicable diseases in India: Challenges and the way forward. J Postgrad Med. 2019;65:5–6. doi: 10.4103/jpgm.JPGM_157_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kundu MK, Hazra S, Pal D, Bhattacharya M. A review on non-communicable diseases (NCDs) burden, its socio-economic impact and the strategies for prevention and control of NCDs in India. Indian J Public Health. 2018;62302 doi: 10.4103/ijph.IJPH_324_16. [DOI] [PubMed] [Google Scholar]
- 9.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: A systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8:e35. [PMC free article] [PubMed] [Google Scholar]
- 11.Hu Y, Sun J, Dai Z, Deng H, Li X, Huang Q, et al. Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. [accessed on July 7, 2020]. Available from: https://www.who.int/publications/i/item/9789240010291 .
- 13.Kretchy IA, Asiedu-Danso M, Kretchy JP. Medication management and adherence during the COVID-19 pandemic: perspectives and experiences from low-and middle-income countries. Res Social Adm Pharm. 2021;17:2023–6. doi: 10.1016/j.sapharm.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yadav UN, Rayamajhee B, Mistry SK, Parsekar SS, Mishra SK. A syndemic perspective on the management of non-communicable diseases amid the COVID-19 pandemic in low- and middle-income countries. Front Public Health. 2020;8:508. doi: 10.3389/fpubh.2020.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kluge HH, Wickramasinghe K, Rippin HL, Mendes R, Peters DH, Kontsevaya A, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395:1678–80. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okereke M, Ukor NA, Adebisi YA, Ogunkola IO, Favour Iyagbaye E, Adiela Owhor G, et al. Impact of COVID-19 on access to healthcare in low- and middle-income countries: Current evidence and future recommendations. Int J Health Plann Manage. 2021;36:13–7. doi: 10.1002/hpm.3067. [DOI] [PubMed] [Google Scholar]
- 17.Thakur JS. Novel coronavirus pandemic may worsen existing global noncommunicable disease crisis. Int J Noncommun Dis. 2020;5:1. [Google Scholar]
- 18.Government of India. Census 2011. [accessed on May 7, 2020]. Available from: https://www.census2011.co.in/census/city/270-bhubaneswar.html .
- 19.COVID Dashboard. State dashboard for Odisha. Government of Odisha. [accessed on May 7, 2020]. Avaialble from: https://www.mygov.in/covid-19 .
- 20.Dean AG, Sullivan KM, Soe MM. OpenEpi: open source epidemiologic statistics for public health, version 2.3. 1. [accessed on April 28, 2020]. Available from: http://www. openepi.com .
- 21.Basu S. Non-communicable disease management in vulnerable patients during COVID-19. Indian J Med Ethics. 2020;5:103–5. doi: 10.20529/IJME.2020.041. [DOI] [PubMed] [Google Scholar]
- 22.Baracchini C, Pieroni A, Viaro F, Cianci V, Tiberio I, et al. Acute stroke management pathway during coronavirus-19 pandemic. Neurol Sci. 2020;41:1003–5. doi: 10.1007/s10072-020-04375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burki TK. Cancer care in the time of COVID-19. Lancet Oncol. 2020;21:628. doi: 10.1016/S1470-2045(20)30201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan BJ, Franklin RC, Burkle FM, Smith EC, Aitken P, Leggat PA. Determining key influences on patient ability to successfully manage noncommunicable disease after natural disaster. Prehosp Disaster Med. 2019;34:241–50. doi: 10.1017/S1049023X1900431X. [DOI] [PubMed] [Google Scholar]
- 25.Ranscombe P. Rural areas at risk during COVID-19 pandemic. Lancet Infect Dis. 2020;20:545. doi: 10.1016/S1473-3099(20)30301-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International journal of surgery. Int J Surg. 2020;78:185–93. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dyer O. COVID-19: Pandemic is having “severe” impact on non-communicable disease care, WHO survey finds. BMJ. 2020;369:m2210. doi: 10.1136/bmj.m2210. [DOI] [PubMed] [Google Scholar]
- 28.Pati S, Swain S, Knottnerus JA, Metsemakers JFM, vanden Akker M. Magnitude and determinants of multimorbidity and health care utilization among patients attending public versus private primary care: A cross-sectional study from Odisha, India. Int J Equity Health. 2020;19:57. doi: 10.1186/s12939-020-01170-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pati S, Swain S, Hussain MA, vanden Akker M, Metsemakers J, Knottnerus JA, et al. Prevalence and outcomes of multimorbidity in South Asia: A systematic review. BMJ Open. 2015;5:e007235. doi: 10.1136/bmjopen-2014-007235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pati S, Pati S, Akker MV, Schellevis FF, Jena S, Burgers JS. Impact of comorbidity on health-related quality of life among type 2 diabetic patients in primary care. Prim Health Care Res Dev. 2020;21:e9. doi: 10.1017/S1463423620000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sinha R, Pati S. Addressing the escalating burden of chronic diseases in India: Need for strengthening primary care. J Family Med Prim Care. 2017;6:701–8. doi: 10.4103/jfmpc.jfmpc_1_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pati S, Hussain MA, Chauhan AS, Mallick D, Nayak S. Patient navigation pathway and barriers to treatment seeking in cancer in India: A qualitative inquiry. Cancer Epidemiol. 2013;37:973–8. doi: 10.1016/j.canep.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 33.Pati S, Sahoo KC, Samal M, Jena S, Mahapatra P, Sutar D, et al. Care-seeking pathways, care challenges, and coping experiences of rural women living with rheumatoid arthritis in Odisha, India. Prim Health Care Res Dev. 2019;20:e83. doi: 10.1017/S146342361900032X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pati S, Agrawal S, Swain S, Lee JT, Vellakkal S, Hussain MA, et al. Non communicable disease multimorbidity and associated health care utilization and expenditures in India: Cross-sectional study. BMC Health Serv Res. 2014;14:451. doi: 10.1186/1472-6963-14-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pati S, Mahapatra P, Kanungo S, Uddin A, Sahoo KC. Managing multimorbidity (multiple chronic diseases) amid COVID-19 pandemic: A community-based study from Odisha, India. Front Public Health. 2020;8:584408. doi: 10.3389/fpubh.2020.584408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steardo L, Verkhratsky A. Psychiatric face of COVID-19. Transl Psychiatry. 2020;10:1–2. doi: 10.1038/s41398-020-00949-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bajpai V. National Health Policy, 2017: Revealing public health chicanery. Econ Polit Wkly. 2018;53:31. [Google Scholar]
- 38.Columbia Universities Libraries. India's National Digital Health Mission. [accessed on May 7, 2020]. Available from: https://academiccommons.columbia.edu/doi/10.7916/d8-wq8f-9094 .