Abstract
Background
High intake of added sugar is linked to weight gain and cardiometabolic risk. In 2018, the US National Salt and Sugar Reduction Initiative (NSSRI) proposed government-supported voluntary national sugar reduction targets. This intervention’s potential health and equity impacts, and cost-effectiveness are unclear.
Methods
A validated microsimulation model, CVD-PREDICT, coded in C++, was used to estimate incremental changes in type 2 diabetes, cardiovascular disease (CVD), quality-adjusted life-years (QALYs), costs and cost-effectiveness of the NSSRI policy. The model was run at the individual-level, incorporating the annual probability of each person’s transition between health status based on their risk factors. The model incorporated national demographic and dietary data from the National Health and Nutrition Examination Survey across 3 cycles (2011-2016), added sugar-related diseases from meta-analyses, and policy costs and health-related costs from established sources. A simulated nationally representative US population was created and followed until age 100 years or death, with 2019 as the year of intervention start. Findings were evaluated over 10 years and a lifetime from healthcare and societal perspectives. Uncertainty was evaluated in a one-way analysis by assuming 50% industry compliance, and probabilistic sensitivity analyses via a second-order Monte Carlo approach. Model outputs included averted diabetes cases, CVD events and CVD deaths, QALYs gained, and formal healthcare cost savings, stratified by age, race, income and education.
Results
Achieving the NSSRI sugar reduction targets could prevent 2.48 million CVD events, 0.49 million CVD deaths, and 0.75 million diabetes cases; gain 6.67 million QALYs; and save $160.88 billion net costs from a societal perspective over a lifetime. The policy became cost-effective (<150K/QALYs) at 6 years, highly cost-effective (< 50K/QALYs) at 7 years, and cost-saving at 9 years. Results were robust from a healthcare perspective, with lower (50%) industry compliance, and in probabilistic sensitivity analyses. The policy could also reduce disparities, with greatest estimated health gains per million adults among Black and Hispanic, lower income, and less educated Americans.
Conclusions
Implementing and achieving the NSSRI sugar reformation targets could generate substantial health gains, equity gains and cost-savings.
Keywords: sugar reformulation, food policy, obesity, cardiovascular disease, cost-effectiveness, health equity
INTRODUCTION
Higher consumption of added sugar, especially from sugar-sweetened beverages (SSBs), is strongly linked to obesity and other cardiometabolic diseases such as type 2 diabetes and cardiovascular disease (CVD).1, 2 These diet-related conditions pose substantial health and economic burdens in the US. More than 2 in 5 American adults have obesity (42.4% prevalence),3 1 in 2 have diabetes or prediabetes,4 and nearly 1 in 2 have CVD, with those from lower-income groups being disproportionately burdened.5, 6 Together, obesity-related conditions are estimated to cost the nation up to $1.42 trillion/year,7 of which $318 billion is attributed to CVD, the leading cause of mortality.6 Americans overconsume added sugar, roughly half of which comes from SSBs.8 Driven by inequitable systemic processes, such as inequitable access to healthy food, and targeted marketing, and nutrition education,9 added sugar consumption is highest among Black Americans and Americans with lower-income and education, worsening health disparities.10-12 Given that nearly all added sugar comes from packaged and commercially produced foods,13 industry reformulation is one potential priority to decrease added sugar intake in the US and reduce the corresponding health and economic burdens.
Product reformulation efforts to reduce contents of less healthful nutrients, such as trans-fat and sodium, have been effective in lowering their intakes in the US and elsewhere.14, 15 In the UK, product reformulation efforts by Public Health England to reduce added sugar content have also been effective, reducing total sugar in products by 2.9% over 2 years.16, 17 Based on these experiences, the US National Salt and Sugar Reduction Initiative (NSSRI), a partnership of more than 100 local, state and national health organizations convened by the New York City Department of Health and Mental Hygiene (NYC DOH), developed and released in 2018 draft category-specific sugar reduction targets for packaged foods (collectively referring to foods and beverages) across 15 food categories.18, 19 Finalized sugar reduction targets after incorporating the industry’s feedback were released in February 2021 with the aims to help achieve a voluntary, gradual, achievable and meaningful industry reformulation nationwide.20
As one potential obstacle to implementation, the health, equity, and economic impacts of the NSSRI’s sugar reformulation targets have not been evaluated. Understanding these potential effects, including the uncertainty and bounds of likely effects, is crucial to further build consensus toward its national, government-supported implementation. To elucidate the effects of implementing the NSSRI sugar reformulation policy in the US, a validated microsimulation model was used to estimate the effects on cardiometabolic health, health equity, costs, and cost-effectiveness, compared to the status quo. This study was performed as a part of the Food Policy Review and Intervention Cost-Effectiveness (Food-PRICE) Project (http://www.food-price.org) in collaboration with the NYC DOH.
METHODS
The study population demographics and dietary intake data are publicly available.21 The source code of the analyses will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Study Overview and Population
A validated micro-simulation model, CVD-PREDICT,22-25 was used to estimate the health, health equity, and economic impacts of the NSSRI sugar reduction targets. The study population was based on US adults aged 35-80 years at baseline with two 24-hour dietary recalls (n=9,718) across three cycles of National Health and Nutrition Examination Survey (NHANES 2011-2016).21 Utilizing the original NHANES dietary survey weights to account for the complex survey design and sampling,26 the study population was sampled with replacement to create a simulated nationally representative US population of 1,000,000 individuals, who were followed until age 100 years or death, whichever came first. Policy effects were assessed over 10 years (2019-2028) and over the cohort lifetime.
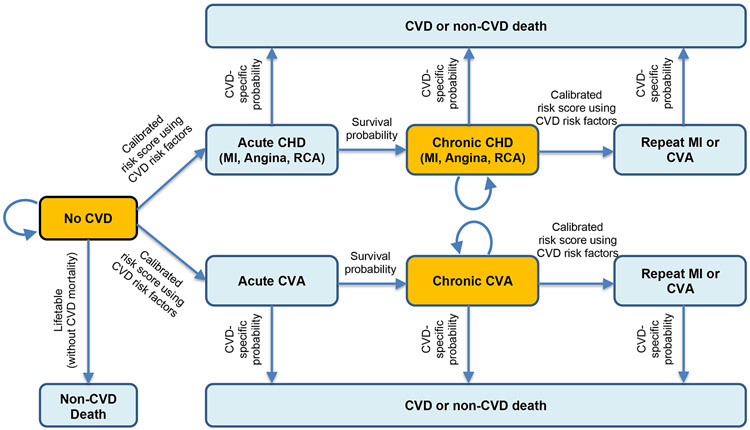
The model incorporated national data on baseline characteristics, cardiometabolic risk factors, dietary intakes, and disease incidence to assess cumulative cardiometabolic health outcomes and costs based on current trends (Figure 1; Text I in the Supplement). At each stage of its logic pathway (Figure I in the Supplement), the best available model inputs, assumptions and associated uncertainties (Table 1; Text II in the Supplement), were used to estimate the health and economic consequences of achieving the nationwide NSSRI added sugar reduction targets. As recommended for economic evaluations of health interventions, the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist was followed in reporting our results (Text III in the Supplement). This study was based on publicly available and de-identified human data, the NHANES 2011-2016, which was approved by the National Center for Health Statistics Research Ethics Review Board Approval under Protocol number 2011-17 with informed consents obtained from all participants.27
Figure 1. The CVD-PREDICT microsimulation model.
Transitions were based on a calibrated risk score including age, sex, systolic blood pressure, total cholesterol, HDL cholesterol, current smoking, and diabetes status. Baseline risk factors were derived from NHANES 2011-16, with further annual changes in all risk factors (including incidence of diabetes) incorporating both age and secular trends. Decreased intake of added sugar could decrease the probability of transitioning of no CVD to acute CVD, and chronic CVD to recurring CVD or CVD death. The model did not estimate direct effects of diabetes mellitus on non-CVD deaths. CVD, Cardiovascular Disease; CHD, Coronary Heart Disease; MI, Myocardial Infarction; RCA, Resuscitated Cardiac Arrest; CVA, Cerebrovascular Accident. HDL, high density lipoprotein.
Table 1.
Key model inputs and sources for cost-effectiveness analysis of the NSSRI voluntary sugar reformulation targets in US adults using the CVD-PREDICT model*
| Model inputs | Value (95% confidence interval) |
Source |
|---|---|---|
| Baseline characteristics | ||
| Demographics | Table VI in the Supplement | NHANES 2011-201621 |
| Cardiovascular disease risk factors | ||
| Prevalent cardiometabolic diseases | ||
| Added sugar intake from SSBs | ||
| Added sugar intake from foods | ||
| Policy effects, 100% industry compliance | Table II in the Supplement | NYC Health20 |
| Sugar from SSBs | 0.60 | |
| Sugar from foods | 0.80 | |
| Policy effects, 50% industry compliance | Table II in the Supplement | NYC Health20 |
| Sugar from SSBs | 0.8000 | |
| Sugar from foods | 0.9000 | |
| Added sugar-cardiometabolic disease etiologic effects † | Table IV in the Supplement | Micha 20172, Lu 201477 |
| BMI (baseline BMI <25kg/m2), per gram of sugar | 0.005 (0.002, 0.007) | |
| BMI (baseline BMI ≥25kg/m2), per gram of sugar | 0.011 (0.007, 0.016) | |
| BMI mediated coronary heart disease, per 5 kg/m2 increase in BMI | 1.28 (1.23, 1.33) | |
| BMI mediated stroke, per 5 kg/m2 increase in BMI | 1.16 (1.10, 1.21) | |
| BMI mediated diabetes mellitus, per 5 kg/m2 increase in BMI | 2.32 (2.04, 2.63) | |
| Coronary heart disease, BMI independent, per gram of sugar from SSBs | 1.009 (1.006, 1.013) | |
| Diabetes mellitus, BMI independent, per gram of sugar from SSBs | 1.010 (1.004, 1.015) | |
| Policy Costs, 8 years ‡ | NYC Health, RTI31 | |
| Government implementation costs | $1,520,855 | |
| Government monitoring and evaluation costs | $2,883,422 | |
| Industry reformulation costs, 100% compliance | $22,935,879,787 | |
| Industry reformulation costs, 50% compliance | $11,467,939,893 | |
| Health-related costs § | ||
| Formal health care costs | ||
| Cardiovascular disease costs | ||
| Chronic disease states, per year | $2,303-$3,485 | Lee 201078, Pignone 200679 |
| Acute disease states, per year | $20,826-$60,383 | O’Sullivan 201180 |
| Procedures and repeat events | $20,826-$60,383 | O’Sullivan 201180 |
| Screening | $38-$82 | Pletcher 200981, Lazar 201182 |
| Medications, per year | $8-$290 | Redbook 200983, Nuckols 201184, Pignone 200679, Shah 201185, |
| Statin-associated adverse events | $192-$7,546 | Lee 201078 |
| Diabetes mellitus costs | ADA 201386, Zhuo 201387 | |
| Institutional care, per year | $1-2,586 | |
| Outpatient care, per year | $7-$519 | |
| Medications and supplies, per year | $36-1,081 | |
| Informal care costs | ||
| Time per outpatient visit, minute | Russell 200888 | |
| Travel | 35 | |
| Waiting | 42 | |
| Wage for adults aged >45 years, per hour | $15.75 | Bureau of Labor Statistics 201332 |
| Productivity costs, dollars | Kim 201689 | |
| Labor force participation rates as full-time workers | 0.076-0.845 | |
| Average annual earnings, per year | $40,138-$57,386 |
All costs are inflated to constant Jan 2019 dollars using the Bureau of Labor Statistics’ Consumer Price Index. 35
Details are presented in Table IV in the Supplement. The association of change in BMI with change in added sugar consumption was assessed using multivariate linear regression. Separate linear relationships were estimated for BMI <25kg/m2 and BMI ≥25kg/m2 since the rate of increase in BMI due to added sugar intake varies based on an individual’s baseline BMI. Values represent cardiometabolic disease relative risks for increased consumption of added sugar at age 50 (45-54) years. RRs for other age groups are presented in Table IV in the Supplement.
Details are presented in Text IV in the Supplement. For data without measurement of variance reported, standard deviation was assumed as 20% of the mean value.
Details are presented in Table V in the Supplement.
BMI, body mass index; CVD-PREDICT, Cardiovascular Disease Policy Model for Risk, Events, Detection, Interventions, Costs, and Trends; and SSB, sugar-sweetened beverage.
NSSRI Policy Scenarios and Effects on Added Sugar Intake
We assessed the NSSRI policy to implement government-supported, voluntary added sugar reduction targets, including short-term targets by the end of year 2023 and long-term targets by the end of year 2026, for 15 categories of packaged foods based on mean sugar content (Table I in the Supplement). The original NSSRI reduction targets for total sugar (set before the Nutrition Facts panel began requiring listing of added sugar) were used as added sugar reduction goals, the underlying aim of the NSSRI policy (Text II in the Supplement). Baseline mean added sugar content in each category was weighted by sales so that products with higher sales volumes factored more heavily into category means. As outlined by the NSSRI and following the UK example, the policy would include (1) federal government implementation to engage industry in setting voluntary reduction targets; (2) federal government monitoring and evaluation during years in which companies are working towards the targets, including rebuilding the NSSRI database to assess progress against the targets, public reporting of findings on the change in sugary density by food category and highlighting companies that choose to commit or meet the targets; and (3) industry reformulations to achieve the targets. We modeled January 1, 2019 as the intervention start. For each food category, the targeted reduction in mean sugar content was 20% by the end of year 2026, except for SSBs which was 40%. We assumed that product reformulations would incrementally, each year, occur over the 8 years of the policy, with each individual product reformulation being sustained, and no further reformulations thereafter (see Table II in the supplement for annualized reductions). We evaluated industry fully meeting the targets, which were developed to be pragmatic and achievable, compared with a base-case of no sugar reformulation. The 15 food categories were mapped to the 24-hour diet recall information from three cycles of NHANES 2011-2016 (Table III in the supplement).21 To determine individual level intakes, added sugar intake from SSBs and food sources were estimated for each individual from up to two 24-hour recalls per person, energy-adjusted using the residual method. 28 We assumed one year lag time between policy implementation and change in sugar intake, followed by immediate health benefits, i.e. BMI change and CVD risk reduction.
Estimated Effects of Added Sugar Intake Changes on Cardiometabolic Risk
Our methods for reviewing and synthesizing the etiologic effect sizes (relative risks) for dietary risk factors and cardiometabolic endpoints (diabetes mellitus, coronary heart disease (CHD), and stroke) have been reported.2, 29 Estimated etiologic effects of added sugar intake were separately derived for SSBs versus foods (including sweetened milk, milk substitutes, and drinks containing milk or milk substitute as a first or second ingredient), as assessed from meta-analyses of prospective cohorts or randomized controlled trials, given larger harms associated with SSB (liquid sugar) consumption. The final model estimates etiologic effects by incorporating these well-established associations: (1) associations of added sugar (from any source) with body mass index (BMI), and subsequent BMI-mediated effects with diabetes, CHD and stroke; and (2) additional BMI-independent associations of added sugar from SSBs (but not other sources) with CHD and diabetes (Table IV in the Supplement). We did not formally model specific dietary complements or substitutes to added sugar, because the estimated etiologic effects on how changes in added sugar influence BMI (and subsequent disease risk) also inherently account for the average dietary substitutes and complements in the population, and are more conservative than simply translating a predicted caloric decrease in added sugar to a reduction in BMI.
Microsimulation Model Structure and Outputs
The CVD-PREDICT model, a validated microsimulation model coded in C++, simulates and quantifies effects of policies on CHD, stroke, and diabetes (Text I in the Supplement). The model is run at the individual-level, incorporating the annual probability of each person’s continuous-time transition between health states based on their risk factors including age, sex, systolic blood pressure, total cholesterol, HDL-cholesterol, smoking, and diabetes. Once an individual is in a chronic disease state, he/she remains in that state as prior history of CVD poses elevated risk of repeated events and mortality. Diabetes is treated both as one of the risk factors for CVD in the model, and as one health outcome in response to the sugar reformulation. The probability of CHD and stroke were derived from validated CHD and stroke risk equations and case fatality risks based on a calibrated Framingham-based risk function as well as validated empiric historical disease trends.30 Underlying age and time trends in CVD risk factors, diabetes incidence, and subsequent estimated CVD incidence and mortality were derived from NHANES. At any given time point, a simulated individual was in one health state, with the probability of experiencing subsequent events based on individual cardiometabolic risk factors and changes in risks from added sugar intake (Figure 1). Model outputs included total diabetes cases, total CVD events (fatal and non-fatal), and CVD deaths, based on more detailed model outcomes including deaths from CHD or stroke; non-fatal events including myocardial infarction, stroke, angina, resuscitated cardiac arrest, and diabetes incidence; and associated quality-adjusted life years (QALYs) and event-associated health-related costs for each. Children and young adults below age 35 years were not included in the model, due to relatively low absolute rates of diabetes and CVD, as well as insufficient established risk equations at these ages. Outputs were estimated for the overall adult population and also stratified by age (35-54 years, 55-74 years, ≥75 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), income (poverty-income ratio (PIR) ≤1.85, PIR >1.85) and education (<high school, high school or some college, college graduate or above) to investigate potential impacts on health equity. The policy’s potential impact on health disparities across different races/ethnicities, income levels, and education levels was assessed via the percentage change in the disparity ratio (the ratio of disease cases per million adults in the two comparison subgroups), comparing the disparity ratio with the policy to the disparity ratio in the base case:
Policy and Health-Related Costs
Policy costs included: (1) government implementation costs, (2) government monitoring and evaluation costs, and (3) industry compliance and reformulation costs (see detailed policy costs in Text IV in the Supplement). Government costs to administer and evaluate the policy were estimated from NYC DOH. Industry costs to reformulate products in response to the sugar targets were estimated using the 2015 FDA Reformulation Cost Model as prepared by the Research Triangle Institute (RTI) International (Text IV in the Supplement).31 Health-related costs included formal healthcare (medical), informal care, and productivity costs, as previously described (Table V in the supplement).23 Formal healthcare costs included those for CVD (CHD and stroke), including acute and chronic disease states, surgical procedures, screening, medications, other treatments, and statin-associated side effects; and for diabetes, including costs for institutional care, outpatient care, outpatient medications, and supplies. Based on previous analyses of a national SSB tax policy, 34.6% of the total national formal healthcare savings would occur for the government, including Medicare, Medicaid, dual-eligible and other government insurance beneficiaries.24 We assumed that a similar proportion of healthcare savings would be observed for the government among any total national healthcare savings in the present policy scenario. Informal care costs included costs for patient’s travel and waiting time as derived from the Bureau of Labor Statistics.32 Productivity costs were calculated using age-specific average annual earnings derived from the Current Population Survey.33
Statistical Analyses
Cost-effectiveness was evaluated following the recommendations from the Second Panel on Cost-Effectiveness in Health and Medicine.34 Analyses were conducted from a (1) healthcare perspective, including policy implementation and monitoring costs and industry reformulation costs as the full “intervention” cost, and formal healthcare costs, and a (2) societal perspective, further incorporating informal care and productivity costs. All costs were inflated to constant 2019 US dollars using the Consumer Price Index calculator,35 and all costs and QALYs were discounted at 3% annually. Net costs were calculated as policy costs minus health-related costs. Incremental cost-effectiveness ratios (ICERs) were calculated as the net change in costs divided by the net change in QALYs. ICERs were assessed annually by running the CVD-PREDICT model at every year to explore the years when the policy became cost-effective and cost-saving. For positive net costs, the ICERs were compared with a willingness-to-pay threshold at $150,000 (cost-effective) and $50,000 (highly cost-effective) per QALY, consistent with American College of Cardiology and American Heart Association recommendations.36
Probabilistic sensitivity analyses via a second-order Monte Carlo approach were conducted to jointly incorporate the uncertainty distributions of key model inputs, including policy effect sizes on added sugar intake, etiologic effects of added sugar reduction, policy costs, health-related costs, and utility weights (Table 1). 1,000 simulations were run jointly drawing from the uncertainty distributions of each of these inputs over a lifetime. Results were presented as 95% uncertainty intervals around the medians for clinical and economic outcomes, based on the 2.5th and 97.5th percentiles of the 1,000 simulations. We also conducted a one-way sensitivity analysis to assess the potential impact of a lower industry compliance rate (50%), with half of the products meeting the targets.
RESULTS
Population Characteristics and Policy Impacts on Added Sugar Intake
Among the estimated national population of US adults aged 35-80 years at baseline, mean (SD) age was 55.6 (12.8) years, about half (52.3%) were female, 69.8% were white, 14.5% did not complete high school, and 28.4% were low-income (Table VI in the Supplement). Mean (SD) BMI was 29.5 (6.8) kg/m2, 15.6% were current smokers, and 36.5% were on hypertension treatment. The baseline mean (SD) added sugar intake from NSSRI-targeted categories was 17.3 (31.7) g/day from SSBs and 18.9 (18.1) g/day from foods. After 10 years of the policy, daily added sugar intake from SSBs and foods were estimated to have decreased by a mean 4.1 g/day and 2.5 g/day, respectively; corresponding decreases over a lifetime were 6.3 g/day and 3.7 g/day (Table 2).
Table 2.
Health gains, costs, and cost-effectiveness of the NSSRI voluntary sugar reformulation policy among US adults at 10 years and lifetime from societal and healthcare perspectives*
| 10 years | Lifetime | |
|---|---|---|
| Population, million | 163.18 | 163.18 |
| Average simulated follow-up years per person | 9.40 | 28.33 |
| Reduction in added sugar intake per person (g/day) | ||
| From SSBs | 4.1 (22.9%)† | 6.3 (34.0%)† |
| From foods | 2.5 (11.0%)† | 3.7 (17.0%)† |
| Cases averted, thousand | ||
| CVD events‡ | 515 (2.5%)† | 2,483 (2.7%)† |
| CVD deaths§ | 68 (1.5%)† | 490 (1.7%)† |
| Diabetes mellitus cases | 209 (0.8%)† | 750 (2.0%)† |
| QALYs gained∥, million | 0.33 (0.02%)† | 6.67 (0.2%)† |
| Change in policy costs, $ billion | ||
| Government implementation costs | 0.002 | 0.002 |
| Government monitoring and evaluation costs | 0.003 | 0.003 |
| Industry reformulation costs¶ | 23.01 | 23.01 |
| Change in health-related costs, $ billion | ||
| Formal healthcare costs# | −27.29 | −141.05 |
| Informal care costs** | −0.03 | −0.08 |
| Productivity costs†† | −4.73 | −42.75 |
| Net costs, $ billion | ||
| Healthcare perspective‡‡ | −4.28 | −118.04 |
| Societal perspective§§ | −9.04 | −160.88 |
| ICER, $/QALY | ||
| Healthcare perspective | Cost-saving | Cost-saving |
| Societal perspective | Cost-saving | Cost-saving |
Health outcomes were evaluated among US adults aged 35-80 years at baseline (n=163.175 million). Simulated population was followed until death or for 100 years, whichever came first. All costs were inflated to 2019 dollars. Health and economic outcomes were compared with a base-case scenario of no added sugar reformulation.
%change from base case.
CVD events include MI, CVA, ANG and RCA.
CVD deaths include IHD deaths and CVA deaths.
QALYs were discounted at 3% annually.
Industry reformulation costs were estimated using the Research Triangle Institute (RTI) reformulation model, accounting for percentage of products reformulated, reformulation type, test types, and compliance period.31 Total reformulation costs are the same at 10 years and lifetime because all models assumed no further reformulation after 8 years’ intervention period.
Formal healthcare costs were calculated from the change in total healthcare costs associated with CVD events including chronic/acute disease states, surgical procedures, screening costs, and drug costs; with diabetes mellitus cases including institutional care, outpatient care, outpatient medications and supplies, discounted at 3% annually. A negative value indicates healthcare savings.
Informal care costs were calculated from the change in costs associated with patient’s travel and waiting time as derived from the Bureau of Labor Statistics, discounted at 3% annually. A negative value indicates informal care savings.
Productivity costs were calculated from the change in costs associated with productivity costs, derived from age-specific average annual earnings from the Current Population Survey,33 discounted at 3% annually.
Net costs from a healthcare perspective equaled government’s policy administration, monitoring and evaluation costs plus industry reformulation costs plus formal healthcare costs, discounted at 3% annually. A negative sign indicates positive monetary savings.
Net costs from a societal perspective equaled government’s policy administration, monitoring and evaluation costs plus industry reformulation costs plus total health-related costs (including formal/informal care costs and indirect costs), discounted at 3% annually. A negative value indicates positive monetary savings.
CVD, Cardiovascular Disease; MI, myocardial infarction; CVA, cerebral vascular accident; ANG, angina; RCA, resuscitated cardiac arrest; IHD, ischemic heart disease; QALY, quality-adjusted life-year; ICER, incremental cost-effectiveness ratio.
Cardiometabolic Health Outcomes
Over a lifetime (mean simulated follow-up, 28.3 years), the sugar reformulation policy could prevent 2.48 million CVD events, 0.49 million CVD deaths, and 0.75 million diabetes cases, with a net gain of 6.67 million QALYs. At 10 years (2019-2028), corresponding gains were 0.51 million CVD events, 0.07 million CVD deaths, 0.21 million diabetes cases, and 0.33 million QALYs (Table 2, Figure 2).
Figure 2. Estimated reductions in total CVD events (Panel A) and diabetes cases (Panel B), gains in QALYs (Panel C), formal healthcare savings (Panel D), net savings from a healthcare perspective (Panel E) and from a societal perspective (Panel F) of the NSSRI voluntary sugar reformulation policy in US adults over 10 years and lifetime.
Blue bars are for the main policy scenario with 100% industry compliance; orange bars are for the sensitivity analysis with 50% industry compliance. CVD, cardiovascular disease; QALY, quality adjusted life year.
Costs and Cost-Effectiveness
The NSSRI sugar reformulation policy was estimated to incur $0.002 billion in government implementation costs, $0.003 billion in monitoring and evaluation costs, and $23.01 billion in industry reformulation costs (Text IV in the Supplement). From a healthcare perspective, considering policy costs and formal healthcare costs, the NSSRI policy was estimated to save $4.28 billion in total net costs by year 10, and $118.04 billion over a lifetime. Based on previously estimated proportional healthcare savings for Medicare, Medicaid, dual-eligible and other government insurance beneficiaries,24 the NSSRI could save the government $9.44 billion by year 10, and $48.80 billion over a lifetime. Net cost-savings were larger from a societal perspective, incorporating additional informal care and productivity costs, with total net savings of $9.04 billion by year 10, and $160.88 billion over a lifetime (Table 2). Evaluated by year, the policy was estimated to meet a cost-effectiveness threshold of 150K/QALY by the end of year 6, and estimated to be cost-saving by the end of year 9 from both healthcare and societal perspectives. The policy was estimated to become highly cost-effective at a threshold of 50K/QALY by the end of year 7 from a societal perspective, and year 8 from a healthcare perspective (Figure II in the Supplement).
Demographic Subgroups
Health benefits were apparent in all population subgroups by age, race, income and education (Figure 3; Table VII in the Supplement). Health gains and healthcare cost-savings per million adults were most prominent among younger adults, Black and Hispanic Americans, and Americans with lower income and less education (Table VIII in the Supplement). The policy was estimated to consistently decrease health disparities among different races/ethnicities, income and education levels (Table 3).
Figure 3. Population size (Panel A), estimated reductions in total CVD events (Panel B), CVD deaths (Panel C) and diabetes cases (Panel D), gains in QALYs (Panel E), and formal healthcare savings (Panel F) of the NSSRI voluntary sugar reformulation policy over a lifetime in US adults by age, race/ethnicity, income and education.
The distribution of the population in each subgroup was derived from the survey weighted percentages among adults aged 35-80 years in NHANES 2011-2016. Other race includes Asian (61.8%) and multiracial population. Formal healthcare savings included cost savings for all chronic and acute disease states, surgical procedures, screening, treatments, and statin associated adverse effects; diabetes, institutional care, outpatient care, medications and supplies, discounted at 3% annually. CVD, cardiovascular disease; QALY, quality adjusted life year.
Table 3.
Impact of the NSSRI voluntary sugar reformulation policy on health disparities
| CVD events per million adults | CVD deaths per million adults | Diabetes cases per million adults | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Base Case | NSSRI policy |
Disparity impact* |
Base Case | NSSRI policy |
Disparity impact* |
Base Case | NSSRI policy |
Disparity impact* |
|
| Race/ ethnicity | |||||||||
| Non-Hispanic white† | 541,726 | 527,802 | 178,481 | 175,745 | 211,266 | 206,925 | |||
| Non-Hispanic black | 611,883 | 591,109 | 189,620 | 185,829 | 281,590 | 275,041 | |||
| Disparity ratio‡ | 1.1295 | 1.1199 | −7.4% | 1.0624 | 1.0574 | −8.1% | 1.3329 | 1.3292 | −1.1% |
| Hispanic | 611,157 | 592,155 | 189,833 | 186,255 | 280,143 | 274,242 | |||
| Disparity ratio‡ | 1.1282 | 1.1219 | −4.9% | 1.0636 | 1.0598 | −6.0% | 1.3260 | 1.3253 | −0.2% |
| Income§ | |||||||||
| High† | 532,815 | 521,393 | 173,938 | 171,635 | 210,821 | 207,118 | |||
| Low | 625,163 | 601,258 | 199,961 | 195,638 | 273,616 | 266,862 | |||
| Disparity ratio‡ | 1.1733 | 1.1532 | −11.6% | 1.1496 | 1.1398 | −6.5% | 1.2979 | 1.2885 | −3.2% |
| Education∥ | |||||||||
| High† | 493,295 | 486,396 | 160,829 | 159,459 | 190,468 | 187,874 | |||
| Low | 618,151 | 595,539 | 201,818 | 197,775 | 286,597 | 280,222 | |||
| Disparity ratio‡ | 1.2531 | 1.2244 | −11.3% | 1.2549 | 1.2403 | −5.7% | 1.5047 | 1.4915 | −2.6% |
Calculated as the percent change in the disparity ratio (the ratio of disease cases per million adults in the two comparison subgroups), comparing the disparity ratio with the policy to the disparity ratio in the base case.
Reference group.
The ratio of disease cases per million adults in this subgroup compared to the reference subgroup with the lowest disease cases per million adults.
Based on the ratio of family income to poverty (low: PIR≤1.85; high: PIR>1.85).
Based on highest educational attainment (low: <high school; high: college graduate or above).
Uncertainty and Sensitivity Analyses
In probabilistic sensitivity analyses, from a societal perspective, the NSSRI sugar reformulation policy had a 90.4% probability (904 out of 1,000 simulations) of being cost-saving, an additional 9.2% probability of being highly cost-effective (<$50k/QALY), and a further 0.4% probability of being cost-effective (<$150k/QALY) at 10 years, as well as a 100% probability of being cost-saving over the cohort lifetime (Figure 4; Table IX in the Supplement). Results were consistent if industry only achieved 50% compliance with the targets, with approximately half of the health benefits and net cost-savings (Figure 4; Table X, Table XI, Figure III in the Supplement).
Figure 4. Cost-effectiveness plane for the NSSRI voluntary sugar reformulation policy among US adults over lifetime.
Values are presented from a societal perspective in incremental costs ($billions) versus incremental quality-adjusted life years (million QALYs), compared to a base scenario of no added sugar reformulation. Each colored dot is the result of each of 1,000 Monte Carlo iterations, and the ellipse depicts the 95% UIs. Interventions that fall into the lower right quadrant of the cost-effectiveness plane indicate that the interventions would be cost saving and improve health outcomes. Blue dots are for the main policy scenario with 100% industry compliance; orange dots are for the sensitivity analysis with 50% industry compliance.
DISCUSSION
Using nationally representative data and a validated microsimulation model, the NSSRI government-supported, voluntary sugar reformulation policy was estimated to generate significant health gains and cost-savings. Over a lifetime, the policy could prevent 2.48 million total CVD events and 0.75 million diabetes cases, gain 6.67 million QALYs and generate $160.88 billion in societal savings. The policy became cost-effective at 6 years, and cost-saving at 9 years from both healthcare and societal perspectives. Even with lower industry compliance (50%) it yielded significant health and cost savings. These novel findings support a critical role for the government and industry to level the playing field and reduce added sugars from SSBs and foods in the U.S.
When population subgroups were assessed, health gains per million adults were greater among younger adults, Black and Hispanic adults, and Americans with lower income and less education. The policy was estimated to consistently reduce health disparities, a particularly timely and relevant issue. These findings inform ongoing policy discussions and highlight the substantial health, equity and economic opportunities – and corresponding costs of inaction or inadequately sustained efforts – to reduce added sugar consumption in the US.
Consumption of added sugar increases risk for obesity, diabetes, and cardiometabolic diseases.1, 2 Many factors shape individual food consumption patterns and associated health outcomes, including industry marketing, a history of structural racism and discriminatory policies and practices that have resulted in high concentrations of poverty and inequitable access to healthy foods, trends in sociocultural norms, agricultural policies and food prices, and the built food environment. To address these systems challenges, system approaches are most effective.37 Several system strategies having been proposed to reduce SSB intake, including taxation,24, 38 health warning labels,39 removal of SSBs from schools,40 and restriction of SSB purchases using nutrition assistance funding such as in the Supplemental Nutrition Assistance Program (SNAP).41 Several of these approaches are being pursued outside the U.S., including SSB taxes (now covering ~2 billion people worldwide);42 front-of-pack icons for high added sugars in SSBs or foods, such as in the U.K., Australia and New Zealand;43, 44 black box health warning labels for high added sugars in SSBs or foods, such as in Chile and Mexico;45, 46 and (most recently) banning of sales of SSBs and junk food to minors (< 18 year old) in the states of Oaxaca and Tabasco, Mexico.47 Outside of school-based approaches and Nutrition facts labeling, such strategies have not yet been widely implemented in the U.S.,48 with ongoing legal challenges from industry to some policies such as health warning labels or front-of-pack icons;49, 50 and state preemption of other strategies, such as SSB taxation, under industry pressure.51, 52
In this setting, a government-supported program of voluntary industry targets for reformulation can be an important tool. Such an approach has the potential to gradually change public taste preference,53, 54 avoid triggering compensatory consumer behaviors,55, 56 and level the playing field for industry by facilitating comparable standards. In addition, the implementation costs for this policy would not fall regressively on consumers who are more likely to be of lower income and educational status.
Although still in early stages, government-supported sugar reformulation is being increasingly implemented internationally, especially in recent years. 57-59 In 2016, the Norwegian health authorities signed an agreement with the food industry, The Partnership for a Healthier Diet, which contains specific reduction targets for added sugar, saturated fat and salt as well as increase targets for berries, vegetables, whole grains and seafood. The added sugar target is to reduce population intake by at least 12.5% by 2021, and eventually contribute to a maximum of 10% of the total population energy intake.57 The industry has currently suspended its voluntary co-operation as a protest against a 2018 increase in the excise duties on sugary products, and as such planned industry compliance assessments have also been put on hold.60 In 2017, the government of Singapore brought together seven major soft drink manufacturers who voluntarily agreed to reduce the sugar contents in their beverages to a maximum of 12g/100ml by 2020.58 In 2019, the Spanish Minister of Health signed agreements with associations representing 398 food and beverage companies to progressively reduce added sugar, saturated fat, and salt by an average of 10% across 13 product groups and 57 subcategories by 2020, in order to reduce obesity and combat inequalities.59 This plan contains reformulation commitments for manufacturers, retailers, caterers, restaurants and vendors,61 and industry compliance evaluation is ongoing. In contrast to these government-supported efforts with specific added sugar targets and evaluation plans, the food industry in France and Switzerland set self-regulatory sugar reduction commitments over 10 years ago, but with unclear progress as of today.62
The most thoroughly evaluated government-supported sugar reformulation policy is from the UK, who in mid-2016 implemented a policy asking the food industry to reduce mean total sugar content by about 5% per year across 8 food categories through 2020.16 In the first year, an overall average 2% reduction in sugar content was achieved, and a 2.9% reduction by the end of the second year.17 This modest overall reduction concealed better progress in certain food categories, such as yogurt and cereals, and lesser progress in others, such as puddings and sweet confectionary.17 Notably, however, the UK reformulation policy did not target SSBs, the single largest overall source of added sugars, as SSBs were being targeted by another dedicated SSB tax policy announced by the UK government around the same time.63 Thus, our model assessed both the potential full benefits of implementing the NSSRI policy, and the sensitivity analysis demonstrating that even partial compliance with the targets could achieve meaningful health gains and cost savings. The NSSRI encourages food and beverage companies to meet the sales-weighted sugar targets by lowering the sugar content of existing products, introducing new, less sugar dense products, and/or by increasing sales of lower sugar products. Adding further potential strategies, such as incentives for the food industry in the form of subsidies or reimbursements, in combination with taxing, icons, health warnings, and educational campaigns, may increase industry compliance and success of the policy.15, 64
To our knowledge this is the first study to estimate the health and health equity impacts, costs, and cost-effectiveness of implementing the NSSRI sugar reformulation policy. The few modeling studies available have assessed the potential impacts of actual or hypothetical added sugar reformulation policies in other countries, such as in the UK,65, 66 Australia,67 Netherlands68 and Mexico,69 and showed promise. Those studies largely focused on obesity as the outcome with only one 66 also assessing economic outcomes. A modeling study estimated that the UK policy, if achieving 100% compliance rate, could reduce obesity prevalence in adults by 5.5%, avert 154,550 diabetes cases, save 51,729 QALYs, and reduce healthcare costs by £285.8 million over 10 years. 66 Our investigation greatly extends these previous analyses by evaluating the health and economic impacts of a government-supported voluntary added sugar reformulation policy in the US.
Our findings also have salience during the COVID-19 pandemic. Given that obesity, diabetes and cardiovascular diseases are established top risk factors for hospitalization and worse prognosis from COVID-19,70, 71 and further contribute to inequities in COVID-19 outcomes,72 public health measures aimed at improving diet-related cardiometabolic burdens and corresponding population resiliency warrant particular attention for both this and future health crises.
This study has several strengths. We utilized a validated microsimulation model and nationally representative data inputs, which increase the validity and generalizability of our estimates. We used the best available evidence on health effects of added sugar from SSBs and foods, including uncertainty in these estimates, and used the real world data or best available data for cost estimates. The policy’s impacts were assessed over shorter time periods and lifetime, from both healthcare and societal perspectives, providing a more comprehensive assessment of the policy and a range of results for different stakeholders. The impact of uncertainty was assessed in both one-way and probabilistic sensitivity analyses.
Potential limitations should be considered. Our model cannot prove the health and cost effects of the NSSRI policy in US adults. Instead, these estimates provide bounds of likely effects that support timely implementation and close monitoring and evaluation of effects. As with any medical or public health intervention, the findings should be considered as estimates of the average population effects, rather than for any individual person. The model did not assume any potential underlying secular trends in added sugar intake. Although all cost assumptions were adjusted for inflation using the CPI calculator, small, residual discrepancies in cost differences over time cannot be excluded. Our model population did not include children, adolescents or younger adults <35 years of age, effects of diabetes on non-cardiovascular outcomes, or health gains or cost savings from reductions in other diseases (e.g. dental caries, other obesity related conditions such as gallstones, respiratory illness, certain cancers and depression).73-76 We only modeled a static population over time, without adding future waves of current under-35 individuals who would “age into” the interested group. Therefore, our findings could underestimate the full health and cost benefits.
In conclusion, our investigation suggests that full or even partial implementation of the NSSRI sugar reformulation policy could generate substantial health gains, equity gains, and both healthcare and societal cost savings.
Supplementary Material
Clinical Perspective.
What’s New?
In February 2021, the New York City Department of Health released sugar reduction targets for the US National Salt and Sugar Reduction Initiative (NSSRI), aiming to achieve a voluntary gradual industry reformulation nationwide.
This study estimated that the government-supportive NSSRI sugar reduction policy could prevent 2.48 million CVD events, 0.49 million CVD deaths, and 0.75 million diabetes cases; gain 6.67 million QALYs; and save $160.88 billion costs.
The greatest health and economic gains per million adults were estimated to be generated among Americans who are of Black and Hispanic race/ethnicity, have lower incomes, and lower education levels.
What are the clinical implications?
The study findings inform ongoing policy discussions and highlight the substantial health and economic opportunities to reduce added sugar consumption.
The NSSRI sugar reduction policy was estimated to bring additional benefits in reducing health and economic disparities, a particularly timely and relevant issue.
These findings support a critical role for the government and industry to level the playing field of public health measures, reduce added sugars from SSBs and foods, and improve diet-related cardiometabolic burdens and corresponding population resiliency.
ACKNOWLEDGEMENTS
We thank all collaborators and advisory groups in the Food Policy Review and Intervention Cost-Effectiveness (Food-PRICE) project (www.food-price.org) and New York City Department of Health and Mental Hygiene (NYC DOH, https://www1.nyc.gov/site/doh/index.page).
SOURCES OF FUNDING
This research was supported by the NIH, NHLBI (R01 HL130735, PI Micha; and R01 HL115189, PI Mozaffarian). In addition, Dr. Liu was supported by a postdoctoral fellowship award (17POST33670808) from the American Heart Association. The funding agencies did not contribute to design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Non-standard Abbreviations and Acronyms
- ACE
Angiotensin-converting enzyme
- ACC
American College of Cardiology
- AHA
American Heart Association
- ADA
American Diabetes Association
- ANG
Angina
- BMI
Body mass index
- CHEERS
Consolidated Health Economic Evaluation Reporting Standards
- CHD
Coronary heart disease
- CPI
Consumer Price Index
- COVID-19
Coronavirus disease of 2019
- CVA
Cerebral vascular accident
- CVD
Cardiovascular disease
- FDA
Food and Drug Administration
- FOOD-PRICE
Food Policy Review and Intervention Cost-Effectiveness
- GP
General practitioner
- HDL
High-density lipoprotein
- ICER
Incremental cost-effectiveness ratio
- IHD
Ischemic heart disease
- MI
Myocardial infarction
- NHANES
National Health and Nutrition Examination Survey
- NSSRI
National Salt and Sugar Reduction Initiative
- NYC DOH
New York City Department of Health and Mental Hygiene
- PIR
Poverty-income ratio
- QALY
Quality-adjusted life year
- RCA
Resuscitated cardiac arrest
- RR
Relative risk
- RTI
Research Triangle Institute
- SD
Standard deviation
- SSB
Sugar sweetened beverage
Footnotes
DISCLOSURES
Dr. Micha reports research funding from Bill and Melinda Gates Foundation, Nestle and Danone, and personal fees from Development Initiatives; Dr. Mozaffarian reports research funding from the Gates Foundation, and the Rockefeller Foundation; personal fees from Acasti Pharma, Barilla, Cleveland Clinic Foundation, Danone, GOED, and Motif FoodWorks; and participating on scientific advisory boards of start-up companies focused on innovations for health including Brightseed, Calibrate, DayTwo, Elysium Health, Filtricine, Foodome, HumanCo, January inc., Perfect Day, Season, and Tiny Organics; Dr. Gaziano reports research funding from United HealthCare, Teva, Novartis, and consulting from Takeda; all outside the submitted work.
REFERENCES
- 1.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R and Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174:516–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Micha R, Penalvo JL, Cudhea F, Imamura F, Rehm CD and Mozaffarian D. Association Between Dietary Factors and Mortality From Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA. 2017;317:912–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CentersForDiseaseControlAndPrevention. Adult Obesity Facts: Obesity is a common, serious, and costly disease. https://www.cdc.gov/obesity/data/adult.html. Published 2021. Accessed 8/11/2021. [Google Scholar]
- 4.CentersForDiseaseControlAndPrevention. Diabetes Basics. https://www.cdc.gov/diabetes/basics/index.html. Published 2019. Accessed 8/11/2021. [Google Scholar]
- 5.Conrad Z, Rehm CD, Wilde P and Mozaffarian D. Cardiometabolic Mortality by Supplemental Nutrition Assistance Program Participation and Eligibility in the United States. Am J Public Health. 2017;107:466–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 7.The Milken Institute. Weighing Down America: The Health and Economic Impact of Obesity. Prepared by: Hugh Waters RD. 2016. [Google Scholar]
- 8.Powell ES, Smith-Taillie LP and Popkin BM. Added Sugars Intake Across the Distribution of US Children and Adult Consumers: 1977-2012. J Acad Nutr Diet. 2016;116:1543–1550 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell LM, Wada R and Kumanyika SK. Racial/ethnic and income disparities in child and adolescent exposure to food and beverage television ads across the U.S. media markets. Health Place. 2014;29:124–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rehm CD, Penalvo JL, Afshin A and Mozaffarian D. Dietary Intake Among US Adults, 1999-2012. JAMA. 2016;315:2542–2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J, Rehm CD, Onopa J and Mozaffarian D. Trends in Diet Quality Among Youth in the United States, 1999-2016. JAMA. 2020;323:1161–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shan Z, Rehm CD, Rogers G, Ruan M, Wang DD, Hu FB, Mozaffarian D, Zhang FF and Bhupathiraju SN. Trends in Dietary Carbohydrate, Protein, and Fat Intake and Diet Quality Among US Adults, 1999-2016. JAMA. 2019;322:1178–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drewnowski A and Rehm CD. Consumption of added sugars among US children and adults by food purchase location and food source. Am J Clin Nutr. 2014;100:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doell D, Folmer D, Lee H, Honigfort M and Carberry S. Updated estimate of trans fat intake by the US population. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2012;29:861–874. [DOI] [PubMed] [Google Scholar]
- 15.Hyseni L, Elliot-Green A, Lloyd-Williams F, Kypridemos C, O'Flaherty M, McGill R, Orton L, Bromley H, Cappuccio FP and Capewell S. Systematic review of dietary salt reduction policies: Evidence for an effectiveness hierarchy? PLoS One. 2017;12:e0177535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tedstone A, Targett V, Owtram G, Pyne V, Allen R, Bathrellou K, MacKinlay B, Clegg E, Morgan K and Swan G. Public Health England. Sugar reduction: Achieving the 20%. A technical report outlining progress to date, industry guidelines, 2015 sugar baseline levels in 9 food categories and the next steps. https://www.gov.uk/government/publications/sugar-reduction-achieving-the-20. Published March/30/2017. Accessed 8/11/2021. [Google Scholar]
- 17.PublicHealthEngland. Sugar reduction: report on progress between 2015 and 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832618/Sugar_reduction_summary__of_progress_2015-2018.pdf. Published September/20/2019. Accessed 7/31/2021. [Google Scholar]
- 18.NYCHealth. National Salt and Sugar Reduction Initiative https://www1.nyc.gov/assets/doh/downloads/pdf/cardio/nsri-partners.pdf. Published July/2021. Accessed 8/11/2021. [Google Scholar]
- 19.NYCHealth. Preliminary Voluntary Sugar Reduction Targets from the National Salt and Sugar Reduction Initiative. https://www1.nyc.gov/assets/doh/downloads/pdf/cardio/nssri-targets.pdf. Published October/29/2018. Accessed 7/31/2021. [Google Scholar]
- 20.NYCHealth. Sugar Reduction Targets from the National Salt and Sugar Reduction Initiative. https://www1.nyc.gov/assets/doh/downloads/pdf/cardio/nssri-revised-sugar-targets.pdf. Published February/24/2021. Accessed 5/5/2021. [Google Scholar]
- 21.NationalCenterforHealthStatistics. Centers for Disease Control and Prevention. NHANES Questionnaires, Datasets, and Related Documentation. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Published 2019. Accessed 03/25/2019. [Google Scholar]
- 22.Pandya A, Sy S, Cho S, Alam S, Weinstein MC and Gaziano TA. Validation of a Cardiovascular Disease Policy Microsimulation Model Using Both Survival and Receiver Operating Characteristic Curves. Med Decis Making. 2017;37:802–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee Y, Mozaffarian D, Sy S, Huang Y, Liu J, Wilde PE, Abrahams-Gessel S, Jardim TSV, Gaziano TA and Micha R. Cost-effectiveness of financial incentives for improving diet and health through Medicare and Medicaid: A microsimulation study. PLoS Med. 2019;16:e1002761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilde P, Huang Y, Sy S, Abrahams-Gessel S, Jardim TV, Paarlberg R, Mozaffarian D, Micha R and Gaziano T. Cost-Effectiveness of a US National Sugar-Sweetened Beverage Tax With a Multistakeholder Approach: Who Pays and Who Benefits. Am J Public Health. 2019;109:276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pandya A, Sy S, Cho S, Weinstein MC and Gaziano TA. Cost-effectiveness of 10-Year Risk Thresholds for Initiation of Statin Therapy for Primary Prevention of Cardiovascular Disease. JAMA. 2015;314:142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NationalCenterforHealthStatistics. Centers for Disease Control and Prevention. NHANES Tutorials - Module 3: Weighting. https://wwwn.cdc.gov/nchs/nhanes/tutorials/module3.aspx. Published 2021. Accessed 7/31/2021. [Google Scholar]
- 27.NationalCenterforHealthStatistics. Centers for Disease Control and Prevention. NCHS Research Ethics Review Board (ERB) Approval. https://www.cdc.gov/nchs/nhanes/irba98.htm. Published November/29/2017. Accessed 6/4/2021. [Google Scholar]
- 28.Willet W Nutritional Epidemiology Implications of Total Energy Intake for Epidemiologic Analyses. Third ed. NY, USA: Oxford University Press; 2013(40). [Google Scholar]
- 29.Micha R, Shulkin ML, Penalvo JL, Khatibzadeh S, Singh GM, Rao M, Fahimi S, Powles J and Mozaffarian D. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One. 2017;12:e0175149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pandya A, Weinstein MC, Salomon JA, Cutler D and Gaziano TA. Who needs laboratories and who needs statins?: comparative and cost-effectiveness analyses of non-laboratory-based, laboratory-based, and staged primary cardiovascular disease screening guidelines. Circ Cardiovasc Qual Outcomes. 2014;7:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.RTI International. Reformulation Cost Model: Final Report. Prepared by: Mary K Muth SB, Jenna Brophy, Kristen Capogrossi, Michaela Coglaiti, Shawn Karns, Catherine Viator. 2015. T. O. Contract No. HHSF-223-2011-10005B [Google Scholar]
- 32.U.S.BureauOfLaborStatistics. Age of reference person: Annual expenditure means, shares, standard errors, and coefficients of variation, Consumer Expenditure Survey, 2016. https://www.bls.gov/cex/tables.htm. Published 2018. Accessed 7/31/2021. [Google Scholar]
- 33.UnitedStatesCensusBureau. Current Population Survey. https://www.census.gov/programs-surveys/cps.html. Published 2017. Accessed 2020/04/09. [Google Scholar]
- 34.Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, Kuntz KM, Meltzer DO, Owens DK, Prosser LA, et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316:1093–1103. [DOI] [PubMed] [Google Scholar]
- 35.U.S.BureauOfLaborStatistics. Consumer Price Index Inflation Calculator. https://data.bls.gov/cgi-bin/cpicalc.pl. Published 2020. Accessed 2020/02/06. [Google Scholar]
- 36.Anderson JL, Heidenreich PA, Barnett PG, Creager MA, Fonarow GC, Gibbons RJ, Halperin JL, Hlatky MA, Jacobs AK, Mark DB, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2304–2322. [DOI] [PubMed] [Google Scholar]
- 37.Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR Jr., Kraus WE, Kris-Etherton PM, Krummel DA, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee Y, Mozaffarian D, Sy S, Liu J, Wilde PE, Marklund M, Abrahams-Gessel S, Gaziano TA and Micha R. Health Impact and Cost-Effectiveness of Volume, Tiered, and Absolute Sugar Content Sugar-Sweetened Beverage Tax Policies in the United States: A Microsimulation Study. Circulation. 2020;142:523–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee BY, Ferguson MC, Hertenstein DL, Adam A, Zenkov E, Wang PI, Wong MS, Gittelsohn J, Mui Y and Brown ST. Simulating the Impact of Sugar-Sweetened Beverage Warning Labels in Three Cities. Am J Prev Med. 2018;54:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.FoodandNutritionService and USDA. National School Lunch Program and School Breakfast Program: Nutrition Standards for All Foods Sold in School as Required by the Healthy, Hunger-Free Kids Act of 2010. Final rule and interim final rule. Federal Register. 2016;81:50131–50151. [PubMed] [Google Scholar]
- 41.Mozaffarian D, Liu J, Sy S, Huang Y, Rehm C, Lee Y, Wilde P, Abrahams-Gessel S, de Souza Veiga Jardim T, Gaziano T, et al. Cost-effectiveness of financial incentives and disincentives for improving food purchases and health through the US Supplemental Nutrition Assistance Program (SNAP): A microsimulation study. PLoS Med. 2018;15:e1002661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.ObesityEvidenceHub. Countries that have implemented taxes on sugar-sweetened beverages. https://www.obesityevidencehub.org.au/collections/prevention/countries-that-have-implemented-taxes-on-sugar-sweetened-beverages-ssbs. Published May/14/2021. Accessed 8/12/2021. [Google Scholar]
- 43.Storcksdieck genannt Bonsmann GM S, Ciriolo E, van Bavel R, Wollgast J. Publications Office of the European Union. JRC Overview of Front-Of-Pack (FOP) schemes providing nutrition information. https://publications.jrc.ec.europa.eu/repository/handle/JRC113586. Published May/25/2020. Accessed 7/31/2021. [Google Scholar]
- 44.Shangguan S, Afshin A, Shulkin M, Ma W, Marsden D, Smith J, Saheb-Kashaf M, Shi P, Micha R, Imamura F, et al. A Meta-Analysis of Food Labeling Effects on Consumer Diet Behaviors and Industry Practices. Am J Prev Med. 2019;56:300–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.White M and Barquera S. Mexico Adopts Food Warning Labels, Why Now? Health Systems & Reform. 2020;6:e1752063. [DOI] [PubMed] [Google Scholar]
- 46.Taillie LS, Reyes M, Colchero MA, Popkin B and Corvalán C. An evaluation of Chile's Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: A before-and-after study. PLoS Med. 2020;17:e1003015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frederick J National Public Radio. Mexican States Ban Sale Of Junk Food To Minors. https://www.npr.org/2020/09/05/909969074/mexico-bans-sale-of-junk-food-to-minors. Published September/5/2020. Accessed 7/31/2021. [Google Scholar]
- 48.Johnson DB, Podrabsky M, Rocha A and Otten JJ. Effect of the Healthy Hunger-Free Kids Act on the Nutritional Quality of Meals Selected by Students and School Lunch Participation Rates. JAMA Pediatrics. 2016;170:e153918. [DOI] [PubMed] [Google Scholar]
- 49.Pomeranz JL, Mozaffarian D and Micha R. Sugar-Sweetened Beverage Warning Policies in the Broader Legal Context: Health and Safety Warning Laws and the First Amendment. Am J Prev Med. 2020;58:783–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pomeranz JL, Wilde P, Mozaffarian D and Micha R. Mandating Front-of-Package Food Labels in the U.S. - What are the First Amendment Obstacles? Food Policy. 2019;86: 10.1016/j.foodpol.2019.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.O’Connor A and Sanger-Katz M. The New York Times. California, of All Places, Has Banned Soda Taxes. How a New Industry Strategy Is Succeeding. https://www.nytimes.com/2018/06/27/upshot/california-banning-soda-taxes-a-new-industry-strategy-is-stunning-some-lawmakers.html. Published June/27/2018. Accessed 7/31/2021. [Google Scholar]
- 52.Paarlberg R, Mozaffarian D, Micha R and Chelius C. KEEPING SODA IN SNAP: Understanding the Other Iron Triangle. Society. 2018;55:308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wyness LA, Butriss JL and Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutr. 2012;15:254–261. [DOI] [PubMed] [Google Scholar]
- 54.Levings JL, Cogswell ME and Gunn JP. Are reductions in population sodium intake achievable? Nutrients. 2014;6:4354–4361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beauchamp GK, Bertino M and Engelman K. Failure to compensate decreased dietary sodium with increased table salt usage. JAMA. 1987;258:3275–3278. [PubMed] [Google Scholar]
- 56.Janssen AM, Kremer S, van Stipriaan WL, Noort MW, de Vries JH and Temme EH. Reduced-Sodium Lunches Are Well-Accepted by Uninformed Consumers Over a 3-Week Period and Result in Decreased Daily Dietary Sodium Intakes: A Randomized Controlled Trial. J Acad Nutr Diet. 2015;115:1614–1625. [DOI] [PubMed] [Google Scholar]
- 57.NorwegianDirectorateofHealth(Helsedirektoratet). Partnership for a healthier diet. https://www.helsedirektoratet.no/english/partnership-for-a-healthier-diet. Published March/11/2016. Accessed 5/7/2021. [Google Scholar]
- 58.Lai L The Straits Times. Seven drink companies pledge to reduce sugar in beverages to 12% or less by 2020. https://www.straitstimes.com/singapore/seven-drink-companies-pledge-to-reduce-sugar-in-beverages-to-12-or-less-by-2020. Published February/6/2018. Accessed 5/27/2021. [Google Scholar]
- 59.Valdivia AG. Forbes. Public-Private Collaboration To Address The Health And Economic Challenge Of Obesity In Spain. https://www.forbes.com/sites/anagarciavaldivia/2019/01/25/public-private-collaboration-to-address-the-health-and-economic-challenge-of-obesity-in-spain/?sh=582cd4f748c8. Published January/25/2019. Accessed 5/7/2021. [Google Scholar]
- 60.Hatløy A, Bråthen K, Stave SE and Hilsen AI. The Fafo Research Foundation. Partnership for a healthier diet: Mid-term report 2019. https://www.fafo.no/images/pub/2020/10336.pdf. Published October/26/2020. Accessed 5/7/2021. [Google Scholar]
- 61.TheSpanishAgencyForFoodSafetyAndNutrition(AESAN). Collaboration PLAN for the improvement of the composition of food and beverages and other measures 2020. https://www.aesan.gob.es/AECOSAN/docs/documentos/nutricion/Plan_Colaboracion_INGLES.pdf. Published 2019. Accessed 5/7/2021. [Google Scholar]
- 62.NOURISHINGandMOVINGpolicydatabases. Voluntary reformulation of food products - Policy Actions. https://policydatabase.wcrf.org/level_one?page=nourishing-level-one#step2=4#step3=353. Published 2021. Accessed 05/07/2021. [Google Scholar]
- 63.HMRevenue&Customs. Policy paper: Soft Drinks Industry Levy. https://www.gov.uk/government/publications/soft-drinks-industry-levy/soft-drinks-industry-levy. Published December/5/2016. Accessed 9/12/2020. [Google Scholar]
- 64.Huang Y, Kypridemos C, Liu J, Lee Y, Pearson-Stuttard J, Collins B, Bandosz P, Capewell S, Whitsel L, Wilde P, et al. Cost-Effectiveness of the US Food and Drug Administration Added Sugar Labeling Policy for Improving Diet and Health. Circulation. 2019;139:2613–2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ma Y, He FJ, Yin Y, Hashem KM and MacGregor GA. Gradual reduction of sugar in soft drinks without substitution as a strategy to reduce overweight, obesity, and type 2 diabetes: a modelling study. Lancet Diabetes Endocrinol. 2016;4:105–114. [DOI] [PubMed] [Google Scholar]
- 66.Amies-Cull B, Briggs ADM and Scarborough P. Estimating the potential impact of the UK government's sugar reduction programme on child and adult health: modelling study. BMJ. 2019;365:l1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yeung CHC, Gohil P, Rangan AM, Flood VM, Arcot J, Gill TP and Louie JCY. Modelling of the impact of universal added sugar reduction through food reformulation. Sci Rep. 2017;7:17392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hendriksen MA, Tijhuis MJ, Fransen HP, Verhagen H and Hoekstra J. Impact of substituting added sugar in carbonated soft drinks by intense sweeteners in young adults in the Netherlands: example of a benefit-risk approach. Eur J Nutr. 2011;50:41–51. [DOI] [PubMed] [Google Scholar]
- 69.Basto-Abreu A, Braverman-Bronstein A, Camacho-Garcia-Formenti D, Zepeda-Tello R, Popkin BM, Rivera-Dommarco J, Hernandez-Avila M and Barrientos-Gutierrez T. Expected changes in obesity after reformulation to reduce added sugars in beverages: A modeling study. PLoS Med. 2018;15:e1002664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.O'Hearn M, Liu J, Cudhea F, Micha R and Mozaffarian D. Coronavirus Disease 2019 Hospitalizations Attributable to Cardiometabolic Conditions in the United States: A Comparative Risk Assessment Analysis. J Am Heart Assoc. 2021;10:e019259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F and Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Price-Haywood EG, Burton J, Fort D and Seoane L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N Engl J Med. 2020;382:2534–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH FG. Overweight, Obesity, and Depression: A Systematic Review and Meta-analysis of Longitudinal Studies. Archives of General Psychiatry. 2010;67:220–229. [DOI] [PubMed] [Google Scholar]
- 74.CentersForDiseaseControlAndPrevention. Cancers Associated with Overweight and Obesity Make up 40 percent of Cancers Diagnosed in the United States. https://www.cdc.gov/media/releases/2017/p1003-vs-cancer-obesity.html. Published October/3/2017. Accessed 8/20/2020. [Google Scholar]
- 75.Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M, et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation . Obesity (Silver Spring). 2020;28:1195–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Newbrun E. Sugar and dental caries: a review of human studies. Science. 1982;217:418–423. [DOI] [PubMed] [Google Scholar]
- 77.Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB and Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383:970–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee KK, Cipriano LE, Owens DK, Go AS and Hlatky MA. Cost-effectiveness of using high-sensitivity C-reactive protein to identify intermediate- and low-cardiovascular-risk individuals for statin therapy. Circulation. 2010;122:1478–1487. [DOI] [PubMed] [Google Scholar]
- 79.Pignone M, Earnshaw S, Tice JA and Pletcher MJ. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med. 2006;144:326–336. [DOI] [PubMed] [Google Scholar]
- 80.O'Sullivan AK, Rubin J, Nyambose J, Kuznik A, Cohen DJ and Thompson D. Cost estimation of cardiovascular disease events in the US. Pharmacoeconomics. 2011;29:693–704. [DOI] [PubMed] [Google Scholar]
- 81.Pletcher MJ, Lazar L, Bibbins-Domingo K, Moran A, Rodondi N, Coxson P, Lightwood J, Williams L and Goldman L. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150:243–254. [DOI] [PubMed] [Google Scholar]
- 82.Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K and Goldman L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124:146–153. [DOI] [PubMed] [Google Scholar]
- 83.ThomsonCorporation. Red book: Pharmacy’s Fundamental Reference. Montvale, NJ: Thomson PDR; 2009. [Google Scholar]
- 84.Nuckols TK, Aledort JE, Adams J, Lai J, Go MH, Keesey J and McGlynn E. Cost implications of improving blood pressure management among U.S. adults. Health Serv Res. 2011;46:1124–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shah ND, Mason J, Kurt M, Denton BT, Schaefer AJ, Montori VM and Smith SA. Comparative effectiveness of guidelines for the management of hyperlipidemia and hypertension for type 2 diabetes patients. PLoS One. 2011;6:e16170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yang WDT, Halder P, Gallo P, Kowal SL, Hogan PF. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhuo X, Zhang P and Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013;45:253–261. [DOI] [PubMed] [Google Scholar]
- 88.Russell LB, Ibuka Y and Carr D. How Much Time Do Patients Spend on Outpatient Visits?: The American Time Use Survey. Patient. 2008;1:211–222. [DOI] [PubMed] [Google Scholar]
- 89.Kim DD BA, Duffy SQ and Zarkin GA. Worked Example 1: Cost-effectiveness of treatments for individuals with alcohol use disorders: A reference case analysis. Oxford: Oxford University Press; 2017. [Google Scholar]
- 90.Sullivan PW and Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Medical Decision Making. 2006;26:410–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.United States Life Table, 2014. Prepared by: National Vital Statistics Reports. 2017. [PubMed] [Google Scholar]
- 92.Tedstone A, Owtram G, Montel S, O’Kennedy E, Coulton V, Targett V, Perkins C, Sweeney K, Dowd L, Clegg E, et al. Public Health England. Sugar reduction: juice and milk based drinks. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/708930/Sugar_reduction_juice_and_milk_based_drinks.pdf. Published May/2018. Accessed 7/31/2021. [Google Scholar]
- 93.Kocer D, Hicsasmaz Z, Bayindirli A and Katnas S. Bubble and pore formation of the high-ratio cake formulation with polydextrose as a sugar- and fat-replacer. Journal of Food Engineering. 2007;78:953–964. [Google Scholar]
- 94.Huang Y, Pomeranz J, Wilde P, Capewell S, Gaziano T, O'Flaherty M, Kersh R, Whitsel L, Mozaffarian D and Micha R. Adoption and Design of Emerging Dietary Policies to Improve Cardiometabolic Health in the US. Curr Atheroscler Rep. 2018;20:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, Kaptoge S, Whitlock G, Qiao Q, Lewington S, et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PloS one. 2013;8:e65174. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.