Abstract
Background:
Worldwide despite the availability of antiretroviral therapy, human immunodeficiency virus/acquired immunodeficiency syndrome still causes morbidity and mortality among patients. In Sub-Saharan Africa, human immunodeficiency virus/acquired immunodeficiency syndrome remains a major public health concern. The aim of this study was to identify the causes of morbidity and mortality in the modern antiretroviral therapy era in Sub-Saharan Africa.
Methods:
We conducted a systematic review according to the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines. We searched relevant studies from 3 databases which are Google Scholar, PubMed, and CINAHL. Two review authors independently screened titles, abstracts, and full-text articles in duplicate, extracted data, and assessed bias. Discrepancies were resolved by discussion or arbitration of a third review author. R software version 3.6.2 was used to analyze the data. Maximum values were used in order to show which disease was mostly spread out by looking at the highest prevalence reported. This systematic review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO).
Results:
A total of 409 articles were obtained from the database search, finally 12 articles met the inclusion criteria and were eligible for data extraction. Among them, 3 were conducted in Nigeria, 2 were conducted in Uganda, 3 were conducted in South Africa, 1 in Gabon, 1 in Ethiopia, 1 in Ghana, and 1 in Burkina Faso. In most of the included studies, tuberculosis was the leading cause of hospitalization which accounted for between 18% and 40.7% and it was also the leading cause of death and accounted for between 16% and 44.3%, except in 1 which reported anemia as the leading cause of hospitalization and in 2 which reported wasting syndrome and meningitis respectively as the leading causes of death. Opportunistic malignancies accounted between for 1.8% to 5% of hospitalization and 1.2% to 9.8% of deaths.
Conclusions:
Tuberculosis is the commonest cause of hospitalization and death in Sub-Saharan Africa, but it is always followed by other infectious disease and other non-AIDS related causes.
Keywords: antiretroviral treatment, morbidity, mortality, Sub-Saharan Africa
1. Introduction
Worldwide, despite the availability of antiretroviral therapy (ART), human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) still causes morbidity and mortality among patients. Since the first outbreak of HIV in 1981, 39 million people have died due to HIV and related diseases.[1] In Sub-Saharan Africa, HIV/AIDS is a major public health concern. In 2009, 70% of the estimated 33 million people living with HIV (PLHIV), are in Sub-Saharan Africa.[2] This region is the most affected by HIV/AIDS with 68% of the world's patients living with HIV.[3] According to WHO (2013), 74% of HIV related deaths were in Sub-Saharan Africa.[4] In 2014 studies reported that 25.8 million people were estimated to be living with HIV.[5] According to UNAIDS (2018), Sub-Saharan Africa, particularly Eastern and Southern Africa remains the region most affected by the HIV epidemic accounting for 45% of the world's HIV infections and 53% of people living with HIV globally.[6] In this region in 2017, 19.6 million of adults and children were living with HIV, 800,000 of adults and children were newly infected with HIV and 380,000 of adults and children died due to AIDS.[6] In the same year, in Western and Central Africa, 6.1 million of adults and children were living with HIV, with 370,000 adults and children newly infected with HIV, and 280,000 adults and children dying due to AIDS.[6] Tuberculosis remains the leading cause of death among people living with HIV, causing 1 in 3 AIDS-related deaths.[7] All included studies were aimed at assessing either cause of death or of hospitalization among PHLIV during the antiretroviral therapy era. In ART services in Sub-Saharan Africa the proportion of patients with tuberculosis is extremely variable, ranging between 5% and 40%.[8] Some studies from Africa reported that 10% to 20% of deaths among PLHIV are attributable to cryptococcal meningitis.[9,10] Recently, the global burden of cryptococcal meningitis has been re-estimated at 223,100 cases (162,500 cases in Sub-Saharan Africa) leading to 181,100 annual deaths (135,900 deaths in Sub-Saharan Africa). The highest annual incidence of cryptococcal meningitis has been found in Nigeria (27,100 cases), South Africa (21,400 cases), Mozambique (18,600 cases), India (18,300 cases), Uganda (12,200 cases), Ethiopia (9600 cases), Kenya (9000 cases), and Zambia (5000 cases).[5] Anemia is the most common hematological manifestation of HIV disease and is frequent among patients living with HIV on ART in Sub-Saharan Africa, with a prevalence ranging from 45% to 87%.[11] Among PLHIV, chronic kidney disease (CKD) has been observed as one of the main complications, with a prevalence ranging from 3.5% to 48.5% in Sub-Saharan Africa.[12] Antiretroviral therapy has improved the life expectancy of patients living with HIV/AIDS.[13] Maximal and durable suppression of viral replication, restoration of immunologic function, reduction of HIV-related morbidity and mortality, improvement of quality of life, and prolonging survival are the major goals of ART.[14] The fast growth in ART coverage represents one of the great public health success stories in the recent history of HIV care that led to reduction of mortality and improvement of quality of life of people living with HIV/AIDS.[14] However, despite the availability of ART, a substantial proportion of PLHIV have continued to be hospitalized and die from both AIDS-related and non-AIDS-related causes.[15] This study is therefore aimed at identifying the determinants of morbidity and specific causes of mortality in the modern ART era in Sub-Saharan Africa.
2. Methods
We followed the Preferred Reporting Items for the Systematic Reviews and Meta-analysis Protocols (PRISMA-P) 2015 guideline.[16] The protocol of this study is registered in PROSPERO with registration number: CRD42019141933. We searched Observational studies reporting on morbidity and mortality in the ART era in Sub-Saharan Africa.
2.1. Eligibility criteria
2.1.1. Inclusion criteria
Studies reporting on causes of hospitalization and causes of death in the antiretroviral era in Sub-Saharan Africa.
Studies published in the period of 2008 to 2018.
Studies reporting on PLHIV and those on ART.
Studies reporting on adult men or women aged 18 years or older.
Peer-reviewed English language publications.
Observational studies published in Sub-Saharan Africa.
2.1.2. Exclusion criteria
Studies reporting on morbidity or mortality on non HIV patients.
Studies reporting on adult men or women under the age of 18 years.
2.2. Search strategy for identifying relevant studies
To identify relevant studies, we searched in the following database: Google Scholar, Pub Med, and CINAHL. Studies published in English from January 2008 to December 2018, conducted in Sub-Saharan Africa. The main search strategy conducted in PubMed/Medline was as follows: “(((Morbidity OR Opportunistic infection related HIV) [MeSH Terms]) AND ((Mortality OR Death) [MeSH Terms]) AND ((ART OR Antiretroviral therapy) [MeSH Terms]) AND ((Sub-Saharan Africa) [MeSH Terms])). We adapted this search strategy for a possible extension to other databases and we also contacted experts in the field to identify additional eligible studies and we manually searched reference lists from relevant studies.
2.3. Data collection, analysis, and synthesis
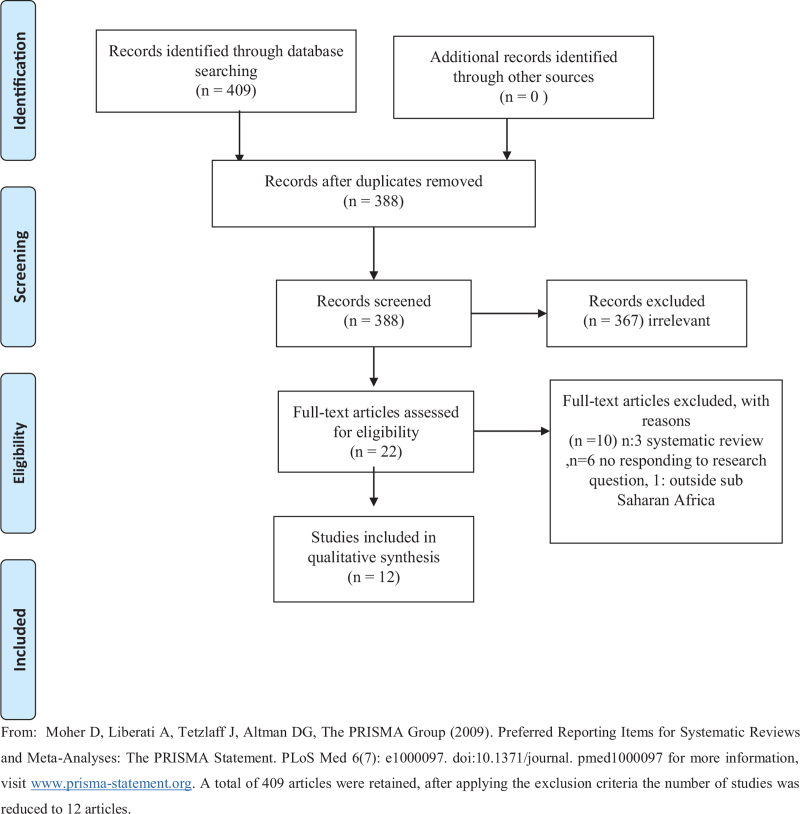
Two reviewers followed independently inclusion criteria for selecting studies, articles were identified and screened by their titles and abstracts for eligibility. The full texts of articles were retrieved. The process of literature selection and reasons for exclusion and inclusion were documented by a Preferred Reporting Items for Systematic Review and Meta-Analysis flow diagram (Fig. 1).[17] The information about the most causes of hospitalization and death related to HIV in the antiretroviral treatment was captured into a spreadsheet, and analyzed using R statistical computing software of the R Core Team, 2020, version 3.6.2. The count and percentages were summarized in the form of quartiles (Q1, Q2, and Q3). The proportions were further graphically visualized in the form of a multiple bar chart for ease of comparison. Maximum values were used in order to show which disease was mostly spread out by looking at the highest prevalence reported. This review was based on publish data, it did not involve contact with participants, therefore no ethical approval was required for it to be conducted. However, the present review was part of a large study approved by the University of KwaZulu-Natal/Biomedical Research Ethics Committee (UKZN/BREC) under reference number BE 345/19.
Figure 1.
PRISMA flow diagram. From: Moher et al.[17] A total of 409 articles were retained, after applying the exclusion criteria the number of studies was reduced to 12 articles.
3. Results
For the initial search, a total of 409 articles were retained, the number of studies was reduced to 12 after applying the exclusion criteria (Fig. 1).
3.1. Characteristics of included studies
Out of 22 reviewed articles, 12 articles were eligible for data extraction (Table 1). All 12 studies included were published between 2008 and 2018 in English and they were conducted in Sub-Saharan Africa. Of these, 3[18–20] were conducted in Nigeria, 2[21,22] were conducted in Uganda, 3 were conducted in South Africa,[23–25] 1 in Gabon,[26] 1 in Ethiopia,[27] 1 in Ghana,[28] and 1 in Burkina Faso.[29] The total sample size of 12 studies was 14,619 participants, predominantly women. According to the study designs of the included studies, we noticed 7 retrospective chart/cohort studies,[18–20,23,26,28,29] 3 prospective studies,[21,22,25] 2 cross-sectional study.[24,27] All included studies were aimed at assessing either cause of death or the most frequent diagnoses among PLHIV during the antiretroviral therapy era. In all included studies the commonest cause of hospitalization was tuberculosis[18–24,26,27,29] except in 1[28] and the most common cause of death was tuberculosis in all the included studies[18–24,26–29] except in 2.[29,30] We summarized the characteristics of all included studies in Table 1, and from this list, we extracted data related to the causes of hospitalization and death in the modern ART era in Sub-Saharan Africa. Most of the articles reported on death than hospitalization, and tuberculosis was the most disease reported (Table 1).
Table 1.
Characteristics of the included studies.
| Authors and date of publication, geographic location, conducted date | Sample size | % female | AverageAge, yr | Intervention | Aim of the study | Study design | OutcomesCauses of hospitalization(N, %) | OutcomesCauses of death(N, %) |
| Agaba et al, 2011, NigeriaConducted date: January–December 2007 | 354 | 69.2 | 35 ± 9 | Use of ART | Determine clinical characteristic and predictor of mortality in hospitalized HIV infected Nigerians | Retrospective chart review | TB (119, 33.6%), CCM (31, 8.8%), septicemia (13, 16.4%), AT (41, 11.6%), CD (23, 6.5%), OM (17, 4.8%), other infections (15, 4.2%), ADC (4, 1.1%), NHRI (32, 9%), NSD (14, 4%) | TB (37, 30.1%), CCM (16, 13.0%), Septicemia (21, 17.1%), AT (4, 3.3%), CD (10, 8.1%), OM (12, 9.8%), other infection (8, 6.5%), ADC (3, 2.4%), NHRI (7, 5.7%), NSD (5, 4%) |
| Namutebi et al, 2013, UgandaConducted date: January–March 2011 | 201 | 50 | 34 | On ART | Determine causes and outcomes of hospitalization in adults on ART. | Prospective cohort study | TB (37, 18%), CCM (22, 11%), Zidovudine—with anemia (19, 10%), sepsis (10, 5%) and Kaposi's sarcoma (10, 5%). | 42 patients (21%) died: TB (10, 24%), CCM (8, 19%), Sepsis (5, 12%), UNS (9, 21%), other illnesses (10, 24%). |
| Saavedra et al, 2017, GhanaConducted date: January 2012–October 2013 | 547 | 53.8 | 41.5 | Most of the patients were not on ART. | Investigate most frequent admitting diagnosis and causes of death | Retrospective study (medical records) | Anemia (76, 34.2%), Toxoplasmosis: (65, 29.3%), pneumonia: (57, 25.7%), TB (45, 20.3%), HIV wasting syndrome: (44, 19.8%), GE (28, 12.6%) | TB (77, 34.7%), Anemia (67, 30.2%), cerebral toxoplasmosis (61, 27.5%), pneumonia (51, 23.0%), GE (23, 10.4%) |
| Solomon et al, 2018, EthiopiaConducted date: May 1–August 30 2017 | 744 | 40.5 | 24 | Receiving ART | Elucidate the spectrum, magnitude and determining factors of the major opportunistic infections | A cross-sectional study | Pulmonary tuberculosis (118, 18%), SCAP (107, 16.3%), and oral candidiasis (103, 15.6%). | Bacterial meningitis (16, 28.6%), PTB (13, 23.8%), SCAP (13, 23.8%). |
| Okome et al, 2014, GabonConducted date: January 1, 2002–September 30, 2010 | 687 | 57 | 34 | Administration of ART | Establish an epidemiologic profile of opportunistic diseases | A retrospective study | TB (114, 24.89%), herpes zoster (HZ) (73, 15.94%), CT (65, 14.19%), OC (65, 14.19%), and severe pneumonia (SP) (43, 9.39%), CM (2, 0.44%) and pneumocystosis (1, 0.21%), KS (9, 1.96%) | |
| Ogoina et al, 2012, NigeriaConducted date: January 2006–December 2009 | 207 | 47.3 | 36 | Administrating ART | Examine morbidity and mortality patterns of hospitalized patients | A retrospective cohort analysis of routinely collected medical records | TB (16, 29.1%), sepsis (6, 7.3%), chronic diarrhea (6, 7.3%), KS (1, 1.8%), CT (1, 1.8%), viral meningoencephalitis (1, 1.8%), CCM (1, 1.8%), herpes zoster (1, 1.8%), AT (10, 18.1%), renal failure (2, 3.6%), hypertensive heart failure (2, 3.6%) | TB (7, 36.9%), sepsis (4, 21.1%), KS (1, 5.3%), VME (1, 5.3%) CCM (1, 5.3%), RF (1, 5.3%) SP (1, 5.3%), acute bacterial meningitis (1, 5.3%). |
| Gyuse et al, 2010, NigeriaConducted date: January 2005–December 2007 | 350 | 61 | 35.4 | Introduction of ART | Determine the causes of death among to plan strategies in improving mortality | Retrospective study | TB (24.0%), followed by sepsis and septicemia (13.0%), meningitis, encephalitis and anemia (11.0%), respiratory diseases (5%), hepatitis (2%), gastrointestinal disease (3%), and RF (3%). | |
| Macpherson et al, 2009, South AfricaConducted date: October 2005–September 2007 | 1131 | 67 | 37 | Initiated on ART | Determine relative contribution of death to cohort exit and causes and predictors of mortality | Retrospective cohort study | TB (47, 44.3%) and diarrhoeal diseases (26, 24.5%), meningitis (5, 4.7%), hepatic failure (3, 2.83%), opportunistic malignancies (KS, prostate, cervix, bladder, endometrium) (7, 6.59%), pneumonia (2, 1.89%), septicemia (4, 3.77%), HIV encephalopathy (1, 0.94%), diabetic ketoacidosis (1, 0.94%), renal failure (1, 0.94%) | |
| Kouanda et al, 2012, Burkina fasoConducted date: January 2003–December 2008 | 5608 | 70 | 35 | Receiving ART | Investigate causes of death and the factors associated with mortality in a cohort of patients on ART | Retrospective cohort study | AIDS (64%) and non-AIDS related (36%). | Wasting (113, 26.9%), TB (67, 16%), esophageal /pulmonary candidiasis (22, 5.2%), chronic diarrhea (17, 4.1%), Toxoplasmosis (16, 3.8%), Cryptococcosis (7, 1.7%), encephalopathy /dementia (7, 1.7%), pneumocystosis (PC) (6, 1.4%), OM (5, 1.2%), Leishmaniasis (5, 1.2%), BP (4, 1.0%), cytomegalovirus disease (1, 0.2%), anemia (22, 5.2%), septicemia (13, 3.1%), respiratory disease (16, 3.8%), AT (16, 3.8%), metabolic disease (13, 3.1%), myocardiopathy (14, 3.3%), BM (4, 1.0%), high blood pressure (4, 1.0%), depression (3, 0.7%), septic abortion (2, 0.5%). |
| Meintjes et al, 2015, South AfricaConducted date: June 2012–October 2013 | 585 | 57.8 | 35.3 | ART | Describe hospital level disease burden and factors contributing to morbidity and mortality | Cross-sectional study with prospective follow-up | TB (238, 40.7%), Bacterial infection (100, 17.1%), AIDS other than TB (64, 10.9%). Major organ dysfunction (59, 10.1%), other diagnosis (35, 6.0%), Venous thromboembolis (1, 5.3%), Drug related (24, 4.1%), non-communicable diseases (22, 3.8%), psychiatric (9, 1.5%), none diagnosed (3, 0.5%). | TB (37.2%) and other AIDS- (24.4%) |
| Moore et al, 2011, UgandaConducted date: May 2003–December 2006 | 1132 | 73 | 38 | ART | Describe mortality over time and to determine clinical conditions associated with death | Prospective study | Most common condition TB (21% of deaths), Candida disease (15%). cryptococcal disease (12%), Pneumocystis jiroveci pneumonia (8%) and KS (6%) | |
| Mzileni et al, 2008, South AfricaConducted date: July 2004–December 2006 | 3073 | 67.4 | ART | Describe mortality trends and causes of deaths | Prospective observational study | TB (42, 20.5%), CD (25, 12.2%), CCM (18, 8.8%), bacterial pneumonia/pneumocystis pneumonia (12, 5.8%), KS and lymphoma (17, 8.3%), hepatitis (6, 2.9%). |
A total of 398 studies were excluded as they did not meet the inclusion criteria, of those 10 underwent a full manuscript review and were found to have no valuable data for the following reasons: 3 systematic reviews,[31–33] 1 article outside of Sub-Saharan Africa,[34] 6 articles not responding to the research question.[35–40]
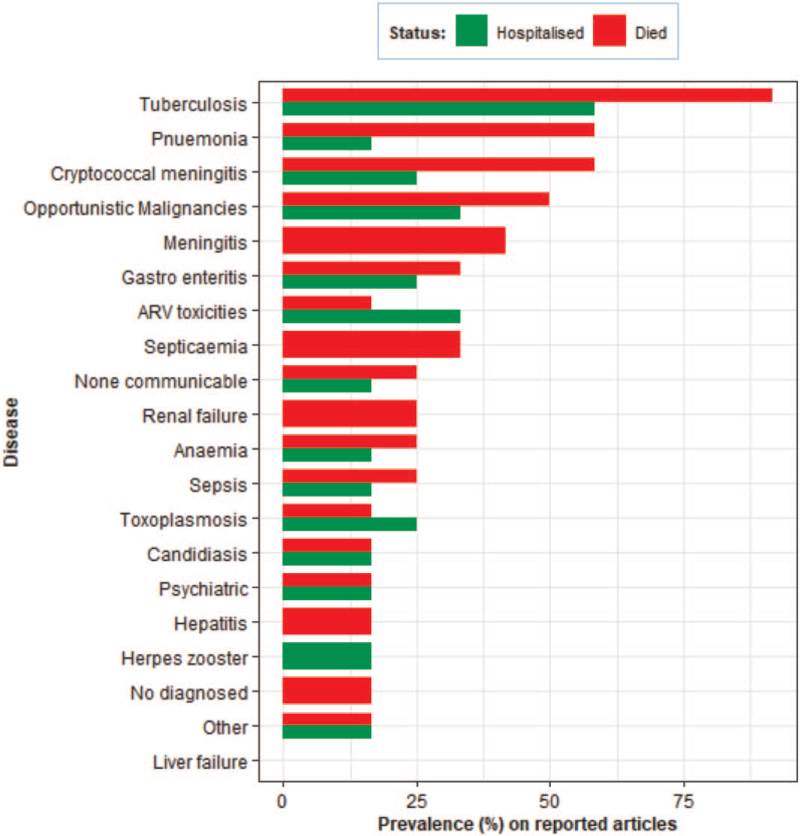
Figure 2 reports the prevalence (%) of articles that described the causes of death and of hospitalization. Six articles reported both causes of death and hospitalization, 5 articles reported causes of death and 1 reported causes of hospitalization. Tuberculosis was the most reported disease by many of the articles. Fifty-eight percent and 92% of analyzed studies investigated TB to be most reported disease that conduct to hospitalization and death respectively, followed by cryptococcal meningitis. The least reported disease was Candidiasis with 17% of hospitalizations and 17% of deaths.
Figure 2.
Prevalence of articles. The prevalence (%) of articles that described the causes of death in red and of hospitalization in green. Six articles reported both causes of death and hospitalization, 5 articles reported causes of death and one reported causes of hospitalization.
Table 2 reports tuberculosis, anemia, and toxoplasmosis were the leading reason of hospitalization 40.7%, 34.2%, and 29.3%, respectively. Pneumocystosis is the least cause of hospitalizations accounting for 0.2%.
Table 2.
Prevalence of the cause of hospitalization.
| Diagnosis | ||||||
| Number of studies | Min | Q1 | Q2 | Q3 | Max | |
| Tuberculosis | 7 | 18 | 19.1 | 24.9 | 31.4 | 40.7 |
| Anemia | 2 | 10 | 16.1 | 22.1 | 28.2 | 34.2 |
| Toxoplasmosis | 3 | 1.8 | 8 | 14.2 | 21.7 | 29.3 |
| Pneumonia | 2 | 16.3 | 18.7 | 21 | 23.3 | 25.7 |
| Cachexia | 1 | 19.8 | 19.8 | 19.8 | 19.8 | 19.8 |
| ARV_toxicities | 4 | 4.1 | 8.5 | 10.8 | 13.2 | 18.1 |
| Septicemia | 1 | 16.4 | 16.4 | 16.4 | 16.4 | 16.4 |
| Herpes | 2 | 1.8 | 5.3 | 8.9 | 12.4 | 15.9 |
| Candidiasis | 2 | 14.2 | 14.5 | 14.9 | 15.2 | 15.6 |
| Gastroenteritis | 3 | 6.5 | 8.7 | 10.9 | 11.8 | 12.6 |
| Cryptoccocal meningitis | 3 | 1.8 | 5.3 | 8.8 | 9.9 | 11 |
| Others | 2 | 4.2 | 5.9 | 7.6 | 9.2 | 10.9 |
| Non communicable disease | 2 | 3.6 | 5 | 6.3 | 7.7 | 9.1 |
| Sepsis | 2 | 5 | 5.6 | 6.2 | 6.7 | 7.3 |
| Malignancies | 4 | 1.8 | 1.9 | 3.4 | 4.8 | 5 |
| No_diagnosed | 1 | 4 | 4 | 4 | 4 | 4 |
| Renal failure | 1 | 3.6 | 3.6 | 3.6 | 3.6 | 3.6 |
| Meningitis | 1 | 1.8 | 1.8 | 1.8 | 1.8 | 1.8 |
| Psychiatric | 2 | 1.1 | 1.2 | 1.3 | 1.4 | 1.5 |
| Pneumocystosis | 1 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 |
In Table 3, tuberculosis, anemia, and meningitis were the leading cause of death at 44.3%, 30.2%, and 28.6%, respectively. The least cause of death was pneumocystosis with 1.4%.
Table 3.
Prevalence of the cause of death.
| Diagnosis | ||||||
| Number of studies | Min | Q1 | Q2 | Q3 | Max | |
| Tuberculosis | 8 | 16 | 22.4 | 24 | 35.8 | 44.3 |
| Anemia | 2 | 5.2 | 8.1 | 11 | 20.6 | 30.2 |
| Meningitis | 4 | 1 | 4.7 | 5.3 | 11 | 28.6 |
| Toxoplasmosis | 2 | 1.7 | 8.2 | 14.6 | 21.1 | 27.5 |
| Gastroenteritis | 4 | 4.1 | 7.1 | 9.2 | 13.9 | 24.5 |
| Others | 1 | 6.5 | 11 | 15.4 | 19.9 | 24.4 |
| no_diagnosed | 2 | 4 | 9 | 14 | 19 | 24 |
| Pneumonia | 6 | 1 | 3.6 | 5.8 | 8.7 | 23 |
| Sepsis | 2 | 13 | 17 | 21 | 21.1 | 21.1 |
| Septicemia | 3 | 3.1 | 3.6 | 8.4 | 14 | 17.1 |
| Candidiasis | 2 | 5.2 | 7.7 | 10.1 | 12.6 | 15 |
| Cryptoccocal meningitis | 6 | 0.4 | 3.5 | 8.8 | 12 | 13 |
| Malignancies | 5 | 1.2 | 5.5 | 6.3 | 7.9 | 9.8 |
| Non communicable disease | 3 | 1.4 | 2.1 | 2.8 | 5.1 | 7.4 |
| Renal failure | 2 | 0.9 | 2 | 3 | 4.2 | 5.3 |
| ARV_toxicities | 2 | 3.3 | 3.4 | 3.5 | 3.7 | 3.8 |
| Hepatitis | 1 | 2 | 2.2 | 2.5 | 2.7 | 2.9 |
| Liver failure | 1 | 2.8 | 2.8 | 2.8 | 2.8 | 2.8 |
| Psychiatric | 2 | 0.7 | 1.1 | 1.5 | 2 | 2.4 |
| Pneumocystosis | 1 | 1.4 | 1.4 | 1.4 | 1.4 | 1.4 |
4. Discussion
The objective of this study was to identify the causes of hospitalization and causes of death among PLHIV in the ART era in Sub-Saharan Africa. The causes reported were opportunistic infections, opportunistic malignancies, and non-AIDS related. Among opportunistic infections, in most of the included studies, tuberculosis was the commonest leading cause of hospitalization and death among people living with HIV. It accounted for between 18% and 40.7% of hospitalization (Table 2) and 16% and 44.3% (Table 3) of death. The prevalence of death reported due to tuberculosis was higher than what had been reported in Thailand.[41] This may be a consequence of many countries in Sub-Saharan Africa not having well developed medical analysis laboratory, therefore late diagnosis of tuberculosis could imply the increased rate of mortality. Non-expanding access and late initiation of antiretroviral therapy and anti-tuberculosis treatment in some countries in Sub-Saharan Africa could also increase the burden of the disease.[42] Studies conducted in Rio de Janeiro, Brazil estimated 80% of reduction of tuberculosis incidence for PLHIV associated with the use of antiretroviral therapy.[43]
Many patients in Sub-Saharan Africa arrived at the hospital at an advanced stage of disease with cluster of differentiation 4 (CD4) ≤200 cells/mm3. Many patients do not have information on disease because of lack of counseling and testing services in the region.[44]
If patients start ART at the higher baseline CD4 count, there is a potential to decrease morbidity and mortality.[45] Among the included studies, one reported from Ghana did not find tuberculosis as the first cause of hospitalization in Sub-Saharan Africa, it reported anemia as the first cause of hospitalization.[28] The included studies reported that anemia accounted for 34.2% of hospitalization (Table 2) and 30.2% of death (Table 3). Similarly, in America, another study among African women living with HIV found almost the same result.[46] Anemia is a known independent risk factor for death among patients living with HIV. It has been reported that 59% of patients who suffer from anemia are likely to die even if other opportunistic infections associated with it are treated appropriately.[47] Anemia is known to be multifactorial, several factors such as poor nutrition, malaria, hookworm infection, and other infections have been reported among its causes.[48] Other studies showed a relation between the prevalence of anemia and HIV.[49,50] This may be a result of late initiation of ART. A study in South Africa showed that early initiation of ART resolved 66% of anemia in HIV positive patients after just 1 year of treatment.[51] Two of the included studies in Burkina Faso,[29] and in Ethiopia,[27] did not find tuberculosis as the most cause of death, they found wasting syndrome and bacterial meningitis, respectively. Similarly, out of the included studies, other studies did not find tuberculosis as the first leading cause of hospitalization and of death, in Europe, precisely in French Guyana, they reported that among AIDS-related deaths the most frequent diseases were histoplasmosis and toxoplasmosis.[52]
In Taiwan, Asia, it was reported that the first HIV-associated opportunistic infections were esophageal candidiasis.[53] Opportunistic malignancies accounted between 1.8% and 5% of hospitalization (Table 2) and 1.2% and 9.8% of death in our included studies (Table 3). It was noticed that kaposi sarcoma was the most reported[18,21,22,25] as cause of hospitalization and death among PLHIV. Lack of detecting early neoplasm through screening may imply the increase of the disease in Sub-Saharan Africa because many medical laboratories in Sub-Saharan Africa do not have devices and laboratories required to support the screening.[54] Many people initiate ART when kaposi sarcoma is already at advanced stages.[55] Similarly, in India, kaposi sarcoma had been reported as the most opportunistic malignancy between 2% and 5%.[30]
Among non-AIDS related, in some of our included studies, ARV toxicities were shown to cause morbidity and mortality.[18,19,21] The prevalence was almost the same in the 3 studies. To reduce morbidity and mortality, counseling about the adverse effects of antiretroviral drugs and aggressive monitoring of patients must be conducted before and after initiation to the antiretroviral therapy.[56] Other non-AIDS related conditions such as non-communicable disease, psychiatric, had been reported on in some of our included studies.[18,22,24,29] A better knowledge of the commonest comorbidities is very important to improve health promotion, prevention, and care among HIV patients. Poverty, limited access to ART, malnutrition, and interruption of supply at the program level had been found to be among the factors which limit the control of HIV and the effectiveness of ART in African countries.[18]
In conclusion, tuberculosis was the most common cause of hospitalization and death in Sub-Saharan Africa according to the included studies, this was followed by other infectious diseases, opportunistic malignancies, and other non-AIDS related causes. To reduce morbidity and mortality in the ART era, all the different causes of hospitalization and causes of death must be attended to.
Acknowledgments
The authors would like to acknowledge and thank the Nelson R Mandela School of the College of Health Sciences, University of KwaZulu-Natal, for the support.
Author contributions
Manimani Riziki Ghislain conceptualized the study and prepared the manuscript under the guidance and supervision of Nombulelo Magula. Manimani Riziki Ghislain and Gloire-Aime Aganze Mushebenge identified, selected, and screened the articles for eligibility, and the discrepancies were resolved by the intervention of Nombulelo Magula. The process of literature selection and reasons for exclusion and inclusion were all authors including contribution to the development and design of the study. Manimani Riziki Ghislain and Nombulelo Magula contributed to the methodology and reviewing of the manuscript. All authors contributed to the final version. All authors read and approved the final manuscript.
Conceptualization: Manimani Riziki Ghislain, Nombulelo Magula.
Data curation: Manimani Riziki Ghislain, Gloire-Aime Aganze Mushebenge.
Methodology: Manimani Riziki Ghislain, Nombulelo Magula.
Supervision: Nombulelo Magula.
Validation: Nombulelo Magula.
Writing – original draft: Manimani Riziki Ghislain.
Writing – review & editing: Nombulelo Magula, Manimani Riziki Ghislain.
Footnotes
Abbreviations: ART = antiretroviral therapy, CD4 = cluster of differentiation 4, HIV/AIDS = human immunodeficiency virus/acquired immunodeficiency syndrome, Q2 = median, PICO = population, intervention, comparator and outcome, PLHIV = patients living with HIV, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, UKZN = University of KwaZulu-Natal.
How to cite this article: Ghislain MR, Mushebenge GA, Magula N. Cause of hospitalization and death in the antiretroviral era in Sub-Saharan Africa published 2008–2018. Medicine. 2021;100:43(e27342).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
% = percentage, ADC = AIDS-demented complex, AT = ARV toxicity, CCM = cryptococcal meningitis, CD = chronic diarrhea, GE = gastroenteritis, KS = kaposi sarcoma, N = number, NHRI = non-HIV related illness, NSD = no specified diagnosis, OM = opportunistic malignancies, RF = renal failure, SCAP = severe community-acquired pneumonia, TB = tuberculosis, UNS = undiagnosed neurological syndromes.
Q2 = median.
Q2 = median.
References
- [1].UNAIDS. 2014 Fact Sheet: UNAIDS; 2014 (cited May 11, 2015). [Google Scholar]
- [2].UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2010; 2010. Available at: http://data.unaids.org/pub/Report/2009/JC1700_Epi_Update_2009_en.pdf. Accessed July 8, 2011. [Google Scholar]
- [3].Muhula SO, Peter M, Sibhatu B, et al. Effects of highly active antiretroviral therapy on the survival of HIV-infected adult patients in urban slums of Kenya. Pan Afr Med J 2015;20:20–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].WHO. “Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Summary of Key Features and Recommendations,” Tech. Rep. Geneva, Switzerland: WHO; 2013. [Google Scholar]
- [5].Rajasingham R, Smith RM, Park BJ, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis 2017;17:873–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].UNAIDS data 2018. [Google Scholar]
- [7].da Silva Escada RO, Velasque L, Ribeiro SR, et al. Mortality in patients with HIV-1 and tuberculosis co-infection in Rio de Janeiro, Brazil-associated factors and causes of death. BMC Infect Dis 2017;17:01–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Komati S, Shaw PA, Stubbs N, et al. Tuberculosis risk factors and mortality for HIV infected persons receiving antiretroviral therapy in South Africa. AIDS (London, England) 2010;24:1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Okongo M, Morgan D, Mayanja B, et al. Causes of death in a rural, population-based human immunodeficiency virus type 1 (HIV-1) natural history cohort in Uganda. Int J Epidemiol 1998;27:698–702. [DOI] [PubMed] [Google Scholar]
- [10].French N, Gray K, Watera C, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS 2002;16:1031–8. [DOI] [PubMed] [Google Scholar]
- [11].Daka D, Lelissa D, Amsalu A. Prevalence of anaemia before and after the initiation of antiretroviral therapy at ART centre of Hawassa University Referral Hospital, Hawassa, South Ethiopia. Sch J Med 2013;3:01–6. [Google Scholar]
- [12].Yanagisawa N, Ando M, Ajisawa A, et al. Clinical characteristics of kidney disease in Japanese HIV-infected patients. Nephron Clin Pract 2011;118:c285–91. [DOI] [PubMed] [Google Scholar]
- [13].Wanyeki I, Cole D, Sills G, Bass P. Five year survival probabilities after ART start at 3 hospitals in Guyana. In Proceedings of the Caribbean HIV Conference 2011 Nov. Nassau, The Bahamas. [Google Scholar]
- [14].Assefa Y, Gilks CF, Lynen L, et al. Performance of the antiretroviral treatment program in Ethiopia, 2005-2015: strengths and weaknesses toward ending AIDS. Int J Infect Dis 2017;60:70–6. [DOI] [PubMed] [Google Scholar]
- [15].Data Collection on Adverse Events of Anti-HIV drugs (D: A: D) Study Group. Factors associated with specific causes of death amongst HIV-positive individuals in the D: A: D Study. AIDS 2010;24:1537–48. [DOI] [PubMed] [Google Scholar]
- [16].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647.1–9. [DOI] [PubMed] [Google Scholar]
- [17].Moher D, Liberati A, Tetzlaff J, et al. PRISMA group preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Agaba PA, Digin E, Makai R, et al. Clinical characteristics and predictors of mortality in hospitalized HIV-infected Nigerians. J Infect Develop Count 2011;5:377–82. [DOI] [PubMed] [Google Scholar]
- [19].Ogoina D, Obiako RO, Muktar HM, et al. Morbidity and mortality patterns of hospitalised adult HIV/AIDS patients in the era of highly active antiretroviral therapy: a 4-year retrospective review from Zaria, Northern Nigeria. AIDS Res Treat 2012;2012: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Gyuse AN, Bassey IE, Udonwa NE, et al. HIV/AIDS related mortality among adult medical patients in a tertiary health institution in South–South, Nigeria. Asian Pac J Trop Med 2010;3:141–4. [Google Scholar]
- [21].Namutebi AM, Kamya MR, Byakika-Kibwika P. Causes and outcome of hospitalization among HIV-infected adults receiving antiretroviral therapy in Mulago hospital, Uganda. Afr Health Sci 2013;13:977–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Moore DM, Yiannoutsos CT, Musick BS, et al. Determinants of early and late mortality among HIV-infected individuals receiving home-based antiretroviral therapy in rural Uganda. J Acquir Immune Defic Syndr 2011;58:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].MacPherson P, Moshabela M, Martinson N, et al. Mortality and loss to follow-up among HAART initiators in rural South Africa. Trans R Soc Trop Med Hyg 2009;103:588–93. [DOI] [PubMed] [Google Scholar]
- [24].Meintjes G, Kerkhoff AD, Burton R, et al. HIV-related medical admissions to a South African district hospital remain frequent despite effective antiretroviral therapy scale-up. Medicine (Baltimore) 2015;94: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Mzileni MO, Longo-Mbenza B, Chephe TJ. Mortality and causes of death in HIV-positive patients receiving antiretroviral therapy at Tshepang Clinic in Doctor George Mukhari Hospital. Pol Arch Med Wewn 2008;118:548–54. [PubMed] [Google Scholar]
- [26].Okome-Nkoumou M, Guiyedi V, Ondounda M, et al. Opportunistic diseases in HIV-infected patients in Gabon following the administration of highly active antiretroviral therapy: a retrospective study. Am J Trop Med Hyg 2014;90:211–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Solomon FB, Angore BN, Koyra HC, et al. Spectrum of opportunistic infections and associated factors among people living with HIV/AIDS in the era of highly active anti-retroviral treatment in Dawro Zone hospital: a retrospective study. BMC Res Notes 2018;11:01–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Saavedra A, Campinha-Bacote N, Hajjar M, et al. Causes of death and factors associated with early mortality of HIV-infected adults admitted to Korle-Bu Teaching Hospital. Pan Afr Med J 2017;27: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kouanda S, Meda IB, Nikiema L, et al. Determinants and causes of mortality in HIV-infected patients receiving antiretroviral therapy in Burkina Faso: a five-year retrospective cohort study. AIDS Care 2012;24:478–90. [DOI] [PubMed] [Google Scholar]
- [30].Mamidi A, DeSimone JA, Pomerantz RJ. Central nervous system infections in individuals with HIV-1 infection. J Neurovirol 2002;8:158–67. [DOI] [PubMed] [Google Scholar]
- [31].Biset Ayalew M. Mortality and its predictors among HIV infected patients taking antiretroviral treatment in ethiopia: a systematic review. AIDS Res Treat 2017;2017: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ford N, Shubber Z, Meintjes G, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. Lancet HIV 2015;2:e438–44. [DOI] [PubMed] [Google Scholar]
- [33].Lawn SD, Harries AD, Anglaret X, et al. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS 2008;22:1897–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Post FA, Szubert AJ, Prendergast AJ, et al. Causes and timing of mortality and morbidity among late presenters starting antiretroviral therapy in the REALITY trial. Clin Infect Dis 2018;66: (suppl_2): S132–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Ayele G, Tessema B, Amsalu A, et al. Prevalence and associated factors of treatment failure among HIV/AIDS patients on HAART attending University of Gondar Referral Hospital Northwest Ethiopia. BMC Immunol 2018;19:01–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Herbst AJ, Cooke GS, Bärnighausen T, et al. Adult mortality and antiretroviral treatment roll-out in rural KwaZulu-Natal, South Africa. Bull World Health Organ 2009;87:754–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Fonsah JY, Njamnshi AK, Kouanfack C, et al. Adherence to antiretroviral therapy (ART) in Yaoundé-Cameroon: association with opportunistic infections, depression, ART regimen and side effects. PLoS One 2017;12:e0170893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Rubaihayo J, Tumwesigye NM, Konde-Lule J. Trends in prevalence of selected opportunistic infections associated with HIV/AIDS in Uganda. BMC Infect Dis 2015;15:01–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Setegn T, Takele A, Gizaw T, et al. Predictors of mortality among adult antiretroviral therapy users in south eastern Ethiopia: retrospective cohort study. AIDS Res Treat 2015;2015: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Steele KT, Steenhoff AP, Newcomb CW, et al. Early mortality and AIDS progression despite high initial antiretroviral therapy adherence and virologic suppression in Botswana. PLoS One 2011;6:e20010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Cain KP, Anekthananon T, Burapat C, et al. Causes of death in HIV-infected persons who have tuberculosis, Thailand. Emerg Infect Dis 2009;15:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Lucas SB, De Cock KM, Hounnou A, et al. Contribution of tuberculosis to slim disease in Africa. BMJ 1994;308:1531–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Santoro-Lopes G, de Pinho AM, Harrison LH, et al. Reduced risk of tuberculosis among Brazilian patients with advanced human immunodeficiency virus infection treated with highly active antiretroviral therapy. Clin Infect Dis 2002;34:543–6. [DOI] [PubMed] [Google Scholar]
- [44].Jacobson KB, Moll AP, Friedland GH, Shenoi SV. Successful tuberculosis treatment outcomes among HIV/TB coinfected patients down-referred from a district hospital to primary health clinics in rural South Africa. PLoS One 2015;10:e0127024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Koethe JR, Lukusa A, Giganti MJ, et al. Association between weight gain and clinical outcomes among malnourished adults initiating antiretroviral therapy in Lusaka, Zambia. J Acquir Immune Defic Syndr 2010;53:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Volberding PA, Levine AM, Dieterich D, et al. Anaemia in HIV Working Group. Anaemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis 2004;38:1454–63. [DOI] [PubMed] [Google Scholar]
- [47].Jamieson C. The investigation of the effects of anemia on the outcome of patients with stage 4 AIDS. Fourth South African AIDS Conference in Durban, South Africa, abstract 408; 2009. [Google Scholar]
- [48].Alem M, Enawgaw B, Gelaw A, et al. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo Health Center Gondar town, Northwest Ethiopia. J Interdisc Histopathol 2013;1:137–44. [Google Scholar]
- [49].Redig AJ, Berliner N. Pathogenesis and clinical implications of HIV-related anemia in 2013. Hematol 2013;2013:377–81. [DOI] [PubMed] [Google Scholar]
- [50].Kreuzer K-A, Rockstroh J. Pathogenesis and pathophysiology of anemia in HIV infection. Ann Hematol 1997;75:179–87. [DOI] [PubMed] [Google Scholar]
- [51].Kerkhoff AD, Wood R, Cobelens FG, et al. Resolution of anemia in a cohort of HIV-infected patients with a high prevalence and incidence of tuberculosis receiving antiretroviral therapy in South Africa. BMC Inect Dis 2014;14:01–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Lewden C, Sobesky M, Cabie A, et al. Causes of death among HIV infected adults in French Guyana and the French West Indies in the era of highly active antiretroviral therapy (HAART). Med Mal Infect 2004;34:286–92. [PubMed] [Google Scholar]
- [53].Hung CC, Chen MY, Hsieh SM, et al. Clinical spectrum, morbidity, and mortality of acquired immunodeficiency syndrome in Taiwan: a 5-year prospective study. J Acquir Immune Defic Syndr 2000;24:378–85. [DOI] [PubMed] [Google Scholar]
- [54].Guindo MA, Shott JP, Saye R, et al. Promoting good clinical laboratory practices and laboratory accreditation to support clinical trials in sub-Saharan Africa. Am J Trop Med Hyg 2012;86:573–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Letang E, Lewis JJ, Bower M, et al. Immune reconstitution inflammatory syndrome associated with kaposi sarcoma: higher incidence and mortality in Africa than in the UK. AIDS 2013;27:1603–13. [DOI] [PubMed] [Google Scholar]
- [56].Abdool Karim SS, Naidoo K, Grobler A, et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med 2010;362:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]