Abstract
This study examined changes in psychotropic medication use associated with the early months of the coronavirus disease 2019 (COVID-19) pandemic. Using Kaiser Permanente Northern California electronic health records, the authors identified adult patients with fills for psychotropic medications and a non-psychotropic comparator (statins) in the 13 weeks before and after the first-known COVID-19-related death in California (March 4, 2020). Generalized estimating equations were used to derive relative risk ratios (RRR) for medication fills compared with the prior year. Analyses were stratified by new and continued fills and patient characteristics. Among 2,405,824 patients, the mean (SD) age was 49.8 (17.9) years; 52.9% were female; 47.9% identified as White; 8.0% and 7.9% had anxiety and depression disorder diagnoses, respectively. Accounting for secular trends, in the 13 weeks following March 4, 2020, there were increased fills for trazodone (RRR = 1.03, 95% CI = 1.02, 1.04), decreased fills for benzodiazepines (RRR = 0.95, 95% CI = 0.94, 0.96) and hypnotics (RRR = 0.97, 95% CI = 0.96, 0.99), and stable fills for antidepressants (RRR = 1.00, 95% CI = 0.99, 1.00). Relative rates of new fills decreased across most medication classes and continued fills either remained stable or demonstrated non-clinically significant decreases. Patients aged ≥65 years demonstrated decreased fills for most medication classes. In the first 13 weeks of the COVID-19 pandemic, fills for most psychotropic medications remained constant or showed small changes relative to the previous year. Continued (compared with new) fills accounted for observed increases in some medication classes. Older adults demonstrated decreased fills of most medications.
Keywords: anxiety, COVID-19, depression, prescription patterns, psychotropics
1. Introduction
In early 2020, the coronavirus disease 2019 (COVID-19) pandemic led to a series of sudden and profound increases in reported psychiatric symptoms and changes in mental health care delivery methods. Multiple surveys among US adults revealed increased rates of depressive and anxiety-related symptoms; for instance, in a national survey conducted in June 2020, 40% of US adults reported at least 1 adverse mental or behavioral health symptom, including 31% who reported symptoms suggestive of a depressive or anxiety disorder.[1] Recent surveys have also found higher rates of depressive and anxiety symptoms among adults in the initial months of the pandemic compared with previous years,[2] increased rates of serious psychological distress during the pandemic compared with the previous year,[3] and increased rates of depressive and anxiety symptoms during the pandemic.[4] Rates of clinically significant insomnia also increased in the early months of the COVID-19 pandemic, ranging from one-fifth to one-third of adult respondents in studies from China,[5] Greece,[6] and France.[7]
Coincident with the increase in psychiatric symptoms, much outpatient mental health care moved from in-person to telehealth modalities (telephone or video). A survey of US physicians in the summer of 2020 revealed that prior to March 11, 2020, over 92% of behavioral and mental health physicians reported seeing 0 to 5 patients per week via telehealth; at the time of the survey, nearly 60% reported seeing more than 20 patients per week via telehealth.[8] It is not well understood how this profound shift in outpatient mental health care delivery may relate to psychotropic medication prescribing. In the immediate term however, early reports indicated only modest changes in psychotropic medication prescribing.[9–11] National pharmacy claims data suggest increased prescribing of antidepressant and anxiolytic medications in March 2020, with a subsequent decline toward pre-pandemic levels in April 2020.[10] In the first 5 months of 2020, compared with the same period in 2019, an analysis of psychotropic prescription patterns in North York, Ontario demonstrated consistent prescription rates of antidepressants and benzodiazepines across the 2 periods.[12] However, the 2020 period was associated with higher rates of dose and medication changes as well as higher dispensations of benzodiazepines compared with the 2019 period.[12] It is not understood if these trends persisted into the summer of 2020 or if patterns were consistent across medication classes or patient demographic groups.
Telehealth care may deter clinicians from prescribing controlled medication classes such as benzodiazepines and hypnotics due to significant risk for misuse or overdose or may impede starting new medications with patients seen virtually. Prescribing patterns may also differ across patient subgroups; older[13] and non-White[14] patients may have had decreased access to telehealth during the pandemic and consequently to psychotropic medications. Longer-term and more granular data would help characterize changes associated with the COVID-19 crisis, informing proactive planning for future pandemics.
Using electronic health record (EHR) and pharmacy data from Kaiser Permanente Northern California (KPNC), a large, integrated health care system, we examined prescribing trends for commonly used psychotropic medication classes prior to and following the onset of the COVID-19 pandemic compared with the prior year. For a non-psychotropic comparator, we assessed statin prescribing during the same time periods. We additionally stratified trends by patient age, gender, and racial/ethnic groups. We hypothesized that in general, prescriptions for antidepressant, anxiolytic, and insomnia-related medications would increase during the COVID-19 period, corresponding with reports of increased mood and anxiety symptoms. We also hypothesized that pandemic-related increases in psychotropic medications would be lower among patients with new medications, and among older and non-White adults given potential slower uptake of telehealth among older adults[15] and inequalities in mental health access among non-White populations.[16] Last, we hypothesized that continued (in contrast to new) fills would account for any observed increases associated with the pandemic.
2. Methods
2.1. Setting
KPNC provides integrated health care to approximately 4.3 million members, constituting about one-third of Northern California's insured population. Members are insured through employer-based plans, Medicare, Medicaid, and health insurance exchanges and are generally representative of the insured US population by both sex and race/ethnicity.[17] The KPNC Institutional Review Board reviewed the study and granted a waiver of informed consent to examine EHR data.
2.2. Study sample
The analytic sample comprised 2,405,824 KPNC members, aged ≥18 years, with continuous KPNC membership and prescription medication coverage between December 1, 2017 and June 30, 2020. This date range extended 12 months prior to the comparison (i.e., non-pandemic) period to allow for distinguishing new from continued prescriptions. The fixed study sample allowed for direct comparisons of rates of prescribed medications in the defined period within the 2-year observation window.
2.3. Prescribed medications
Outpatient psychotropic medication fills were extracted from KPNC pharmacy data and classified into broad drug classes: antidepressants, benzodiazepines, non-benzodiazepine hypnotics, trazodone, mood stabilizers and antipsychotics, and stimulants. Additionally, statins were included as a non-psychotropic comparator (see Supplemental Table 1, which lists the generic names of medications included in this study). More than 90% of members obtain prescription medications through KPNC pharmacies; dose, directions for use, supply, and refills for all dispensed prescriptions are stored in electronic databases validated for as-needed and scheduled medications.[18–20] A medication was classified as filled within each observation period if the patient had ≥1 documented fill. For each medication class and within an observation period (December 3, 2019 to June 2, 2020 or December 4, 2018 to June 2, 2019), patients with new prescriptions (no fills of a medication from the same class in the prior 12 months) were identified and distinguished from continued fills (≥1 fill of a medication from the same class in the prior 12 months).
2.4. Patient characteristics
From the EHR, we extracted patients’ sex, age, race/ethnicity, and whether patients’ primary medical insurance was covered by the state Medicaid program or another payer source. To measure socioeconomic status, which has been shown to be associated with psychotropic medication use,[21] we used median household income by geocoding patients’ residential addresses to 2010 US Census blocks. We created a dichotomous variable based on the median estimated household income in the sample (≤$92,295.40 vs >$92,295.40).
2.5. Statistical analysis
A quasi-experimental difference-in-difference design[22] was used to account for secular trends in prescribing fills, comparing the period of interest (March 4, 2020 to June 2, 2020) following the first reported statewide COVID-19 death to the 13 weeks prior (December 3, 2019 to March 3, 2020) with corresponding 13-weeks comparison periods in the year prior (March 4, 2019 to June 2, 2019 and December 4, 2018 to March 3, 2019). McNemar's test was used to examine differences in proportion of patients prescribed study drugs in the 13 weeks prior to and after March 4 for each year. Generalized estimating equations (GEE) were used to derive relative risk ratios (RRR) for each medication within 13 weeks with year (2018–2019 or 2019–2020), period (before or after March 4), and their interaction as covariates. These models were repeated among the subgroup of patients with new prescriptions for each medication class. To test for effect modification by demographic subgroups, we performed stratified McNemar's tests and GEE analyses. Subgroups of interest included age (18–44, 45–64, and ≥65 years), sex, race/ethnicity (non-Hispanic White and Other), and estimated household income. We tested for significant interactions by adding a covariate for subgroup, all 2-way interaction terms, and the 3-way interaction between subgroup, 13-week time frame, and period to the GEE models. Participants missing subgroup data were dropped from these analyses (sex: missing n = 131; income: missing n = 27,292). Significance was defined as 2-tailed P < .05. All analyses were performed using SAS version 9.4 (SAS Institute; Cary, NC).
3. Results
Among the 2,405,824 adults who met study inclusion criteria, the mean (SD) age was 49.8 (17.9) years, 23.2% were age ≥65 years, 52.9% were female, 47.9% were non-Hispanic White, 4.2% had Medicaid insurance, and approximately 8% had an anxiety or depressive disorder diagnosis (Table 1).
Table 1.
Baseline characteristics of 2,405,824 Kaiser Permanente Northern California adult members.
| Characteristic | Overall |
| Age, n (%), years | |
| 18–45 | 1,021,735 (42.5) |
| 46–64 | 824,822 (34.3) |
| ≥65 | 559,267 (23.2) |
| Sex, n (%) | |
| Female | 1,273,133 (52.9) |
| Male | 1,132,560 (47.1) |
| Other/missing | 131 (0.0) |
| Race/ethnicity, n (%) | |
| Black | 171,048 (7.1) |
| Asian/Pacific Islander | 515,289 (21.4) |
| Hispanic/Latinx | 450,497 (18.7) |
| Other/unknown | 115,833 (4.8) |
| White | 1,153,157 (47.9) |
| Median neighborhood household income, mean ± SD, US$∗ | 92,295 ± 40,707 |
| Any medication treatment (time period), n (%) | |
| Antidepressants (2018–2019) | 258,721 (10.8) |
| Antidepressants (2019–2020) | 266,325 (11.1) |
| Benzodiazepines (2018–2019) | 92,457 (3.8) |
| Benzodiazepines (2019–2020) | 83,323 (3.5) |
| Hypnotics (2018–2019) | 18,188 (0.8) |
| Hypnotics (2019–2020) | 15,869 (0.7) |
| Trazodone (2018–2019) | 58,845 (2.4) |
| Trazodone (2019–2020) | 62,517 (2.6) |
| Mood stabilizers/antipsychotics (2018–2019) | 55,325 (2.3) |
| Mood stabilizers/antipsychotics (2019–2020) | 58,100 (2.4) |
| Stimulants (2018–2019) | 3,120 (0.1) |
| Stimulants (2019–2020) | 3,382 (0.1) |
| Statins (2018–2019) | 455,402 (18.9) |
| Statins (2019–2020) | 476,401 (19.8) |
3.1. Antidepressants, benzodiazepines, hypnotics, and trazodone
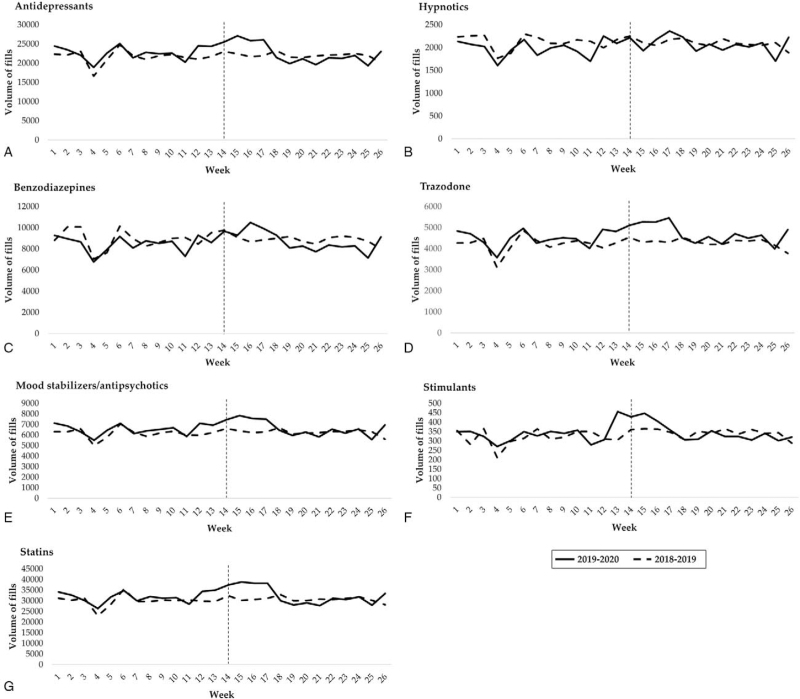
In the first 13 weeks of the COVID-19 period (March 4, 2020 to June 2, 2020), 8.9% of patients filled ≥1 prescription for antidepressants, 0.5% for hypnotics, 2.5% for benzodiazepines, and 2.0% for trazodone. Before accounting for prior-year patterns, these rates were significantly increased compared with the previous 13 weeks (December 3, 2019 to March 3, 2020) for antidepressants (+1.5%), and trazodone (+5.8%) (Table 2; Fig. 1). Over the same period, fills decreased for benzodiazepines (−3.6%) and hypnotics (−3.5%). Fills of antidepressants and trazodone as well as mood stabilizers and antipsychotics, stimulants, and statins increased compared with the prior year between mid-February and late March 2020 (Fig. 1). To account for secular trends, we contrasted these changes before and after March 4, 2020 with fills in the same periods 1 year prior. These difference-in-differences models indicated increased fills for trazodone (RRR = 1.03, 95% CI = 1.02, 1.04), decreased fills for benzodiazepines (RRR = 0.95, 95% CI = 0.94, 0.96) and hypnotics (RRR = 0.97, 95% CI = 0.96, 0.99), and stable fills for antidepressants (RRR = 1.00, 95% CI = 0.99, 1.00) after accounting for prior-year patterns.
Table 2.
Medication fill changes by class.
| 2018–2019 | 2019–2020 | Difference in differences | ||||||||
| Medication, n (%) | Dec 4–Mar 4 | Mar 4–Jun 2 | % Change | P value | Dec 3–Mar 4 | Mar 4–Jun 2 | % Change | P value | RRR (95% CI) | P value |
| Antidepressants | 202,414 (8.4) | 205,689 (8.5) | +1.6 | <.001 | 212,098 (8.8) | 215,307 (8.9) | +1.5 | <.001 | 1.00 (0.99–1.00) | .642 |
| Hypnotics | 14,462 (0.6) | 14,343 (0.6) | −0.8 | .171 | 13,177 (0.5) | 12,711 (0.5) | −3.5 | <.001 | 0.97 (0.96–0.99) | <.01 |
| Benzodiazepines | 65,835 (2.7) | 66,687 (2.8) | +1.3 | <.001 | 62,216 (2.6) | 59,998 (2.5) | −3.6 | <.001 | 0.95 (0.94–0.96) | <.001 |
| Trazodone | 43,205 (1.8) | 44,327 (1.8) | +2.6 | <.001 | 45,879 (1.9) | 48,545 (2.0) | +5.8 | <.001 | 1.03 (1.02–1.04) | <.001 |
| Mood stabilizers/ antipsychotics | 44,485 (1.8) | 45,442 (1.9) | +2.2 | <.001 | 47,017 (1.9) | 48,654 (2.0) | +3.5 | <.001 | 1.01 (1.00–1.02) | <.01 |
| Stimulants | 2,394 (0.1) | 2,578 (0.1) | +7.7 | <.001 | 2,505 (0.1) | 2,750 (0.1) | +9.8 | <.001 | 1.02 (0.98–1.06) | .351 |
| Statins | 364,936 (15.2) | 375,345 (15.6) | +2.9 | <.001 | 387,316 (16.1) | 401,627 (16.7) | +4.0 | <.001 | 1.01 (1.00–1.01) | <.001 |
Figure 1.
Weekly volume of fills for selected psychotropic medication classes and statins. Numbers on the x-axis represent the 26 wk between December 4, 2018 to June 2, 2019 or between December 3, 2019 to June 2, 2020. The vertical dotted line represents March 4, the first documented death attributed to COVID-19 in California in 2020.
3.2. Other psychotropic medications
In the first 13 weeks of the COVID-19 period, 2.0% of patients filled ≥1 prescription for mood stabilizers and antipsychotics and 0.1% for stimulants. Before accounting for prior-year patterns, these rates were significantly increased compared with the previous 13 weeks for mood stabilizers and antipsychotics (+3.5%) and stimulants (+9.8%) (Table 2; Fig. 1). Accounting for fill patterns in the prior year, difference-in-difference models indicated slightly increased fills for mood stabilizers and antipsychotics (RRR = 1.01, 95% CI = 1.00, 1.02) and stable fills for stimulants (RRR = 1.02, 95% CI = 0.98, 1.06).
3.3. Statins
In the first 13 weeks of the COVID-19 period, 16.7% of patients filled ≥1 prescription for statins. Before accounting for prior-year patterns, these rates were significantly increased compared with the previous 13 weeks (+4.0%) (Table 2; Supplemental Tables 2–3, which contain the RRR values for new and continued fills for each medication class, including statins). Accounting for fill patterns in the prior year, difference-in-difference models indicated slightly increased fills for statins (RRR = 1.01, 95% CI = 1.00, 1.01).
3.4. Patients with new prescriptions
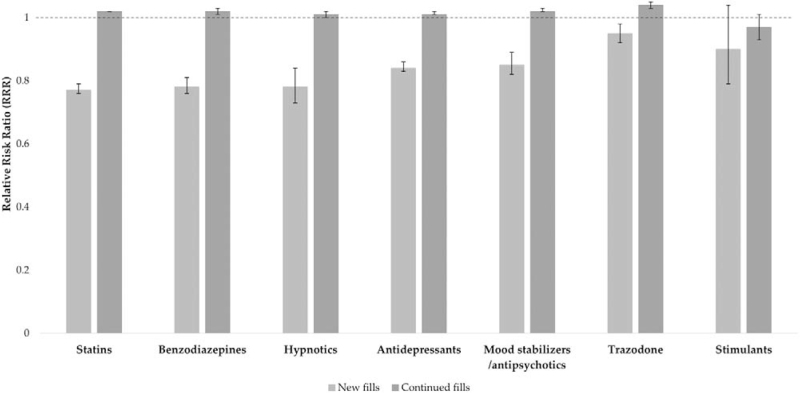
In the first 13 weeks of the COVID-19 period, 1.6% of patients filled ≥1 new prescription for antidepressants, 0.1% for hypnotics, 0.7% for benzodiazepines, 0.6% for trazodone, 0.4% for mood stabilizers and antipsychotics, 0.0% for stimulants, and 1.4% for statins. Before accounting for prior-year patterns, these rates were significantly increased compared with the previous 13 weeks for antidepressants (+18.6%, P < .001), trazodone (+22.9%, P < .001), mood stabilizers and antipsychotics (+25.6%, P < .001), stimulants (+66.4%, P < .001), and statins (+14.8%, P < .001) (Supplemental Tables 2–3, which contain the RRR values for new and continued fills for each medication class). Over the same period, fills decreased for benzodiazepines (−6.2%, P < .001) and hypnotics (−2.5%, P < .001). However, after accounting for secular trends, difference-in-difference models indicated that for nearly all medication classes, new fills were substantially lower than expected, specifically for antidepressants (RRR = 0.84, 95% CI = 0.83, 0.86), benzodiazepines (RRR = 0.78, 95% CI = 0.76, 0.81), hypnotics (RRR = 0.78, 95% CI = 0.73, 0.84), mood stabilizers and antipsychotics (RRR = 0.85, 95% CI = 0.82, 0.88), and statins (RRR = 0.77, 95% CI = 0.76, 0.79). Only new fills for stimulants remained stable relative to prior-year patterns. In contrast to the relative decreases in new fills, there were either no changes or clinically insignificant relative decreases in continued fills for all medication classes (Fig. 2, Supplemental Tables 2–3, which contain the RRR values for new and continued fills for each medication class).
Figure 2.
Relative rates of new and continued fills for selected psychotropic medications and statins in 2019–2020 compared with 2018–2019. Error bars represent standard errors of relative risk ratios.
3.5. Trends in fills by patient characteristics
Stratified difference-in-differences models suggested that overall fill patterns were consistent for medication classes across patient sex, race/ethnicity, and income (Supplemental Tables 4–10, which contain the RRR values for each medication class by patient characteristics). When fills were examined by age group, fill rates for many medications were reduced for older adults (ages ≥65 years) relative to younger (18–45 years) and middle aged (46–64 years) adults based on difference-in-differences models. Contrary to younger and middle-aged adults who had stable hypnotic fills, older adults had a reduction in hypnotic fills when accounting for prior-year patterns (older adult RRR = 0.93, 95% CI = 0.91, 0.96; 3-way interaction P < 0.01). Whereas younger and middle-aged adults had relative increases in trazodone fills when accounting for prior-year fills, older adult rates were stable (older adult RRR = 1.01, 95% CI = 0.99, 1.02; 3-way interaction P < 0.001). Older adults also saw slightly lower antidepressant and statin fills compared to other groups in difference-in-differences analyses. All age groups had relatively decreased benzodiazepine fills and stable stimulant fills. Older adults had modest increases in mood stabilizers and antipsychotics (RRR = 1.02, 95% CI = 1.00, 1.04) but rates did not significantly differ across age groups (3-way interaction P = 0.47).
4. Discussion
During the COVID-19 study period, medication fills for psychotropic medications and statins were stable or changed only modestly after accounting for prior-year patterns. When compared to prior-year fill rates, there was a slight increase in trazodone, mood stabilizers/antipsychotics, and statins; small decreases in benzodiazepines and hypnotics; and no significant change in antidepressants and stimulants. All medications, except benzodiazepines and hypnotics, showed a brief increase in fills in late February and early March 2020, followed by a decrease and reversion to 2019 levels by April 2020, but these dynamics did not lead to clinically meaningfully different overall prescription rates in 2020 vs 2019.
The stability in prescription fills was specific to patients who continued use of a medication from the same class. This pattern suggests that patients and prescribers may have responded to concerns regarding reduced availability of prescription medications due to the pandemic. These concerns may have led to a brief initial “stockpiling” of medications to avoid disruptions in pharmacotherapy.
Reports of critical medication shortages in the first half of 2020 highlighted supply-chain failures that led to decreased supplies of many medications, some of which had no direct role in the treatment of COVID symptoms.[23,24] Patients may have responded to this information by stockpiling any medication, with the concern that they might not have access to these medications in the near future. For instance, in a US-based survey of adults (N = 361) in April 2020, 53% of respondents reported stockpiling “medicine,” similar to stockpiling rates of bottled water (57%) and bread (53%).[25] In Australia, adults with diabetes demonstrated substantially increased rates of dispensed antidiabetic medications from February through early April 2020 compared with the same period in the 4 previous years.[26] Our observation that statins followed a similar pattern suggests that this phenomenon was not unique to psychotropics and, instead, may have characterized general prescribed medication fill patterns in the early stages of the pandemic.
Most prior pharmacoepidemiologic studies that have examined trends in use of psychotropic medications following a disaster have identified a single discrete event, such as an earthquake,[27,28] terrorist attack,[29–32] or another man-made disaster.[33–35] In contrast, the COVID-19 pandemic has been an ongoing, dynamic series of events. In addition, prior studies employed heterogenous methods to examine changes in medication use, thereby making comparisons of our results with previous studies challenging. However, our findings are generally concordant with previous studies that have demonstrated a short-lived and modest increased use of psychotropics immediately following a disaster.[27,31,36]
In contrast to continued prescriptions, new fills for psychotropic medications were substantially lower than what would have been expected based on 2019 rates. Patients were especially less likely to fill new prescriptions for benzodiazepines, hypnotics, and statins. Only for stimulants were new fills not significantly lower. This pattern of results is similar to that found in the 12 weeks following the September 11 terrorist attacks; namely, rates of new fills of psychotropic medications did not substantially change compared to the same period in the previous year.[29] In our study, this finding may be explained by the hesitancy of patients to initiate care during the tumultuous initial weeks of the pandemic; not only are most psychotropics prescribed in primary care,[37] but in KPNC, most referrals to psychiatry originate in primary care.
It is especially reassuring that new fills for benzodiazepines and hypnotics, both of which carry high potential for serious side effects, abuse, and diversion, did not increase immediately following the onset of the pandemic. In contrast, in North York, Ontario, rates of prescriptions for benzodiazepines in the first 5 months of 2020 were higher compared with the same period in 2019.[12] The reasons for this specific discrepancy between the results of the current study and those of the Ontario-based study[12] may be multifactorial, attributable to a combination of increased prescriber awareness of the hazards of benzodiazepines and hypnotics; an emphasis on safer pharmacologic and behavioral interventions; and uncertainty regarding the regulatory issues surrounding prescription of controlled substances via telehealth, especially in the initial months of the pandemic.
Psychotropic fills among older adults generally decreased relative to rates for younger adults. Interestingly, older adults may report less severe mental health effects during the pandemic compared with younger adults,[38] which may partially explain why older adults were less likely to exhibit increased use of psychotropic medications in the early stages of the pandemic. Other explanations may include prescriber behavior (e.g., caution regarding prescribing psychotropics in elderly populations; awareness of hazards of psychotropic use in the context of medical comorbidities) and patient factors (e.g., low technological literacy among older adults in a period in which telemedicine may have been the only mode of outpatient health care delivery). However, older adults did demonstrate modest relative increases in mood stabilizers and antipsychotics, which may have been partially accounted for by low-dose antipsychotics (such as quetiapine) for insomnia.
The results reported here should be interpreted in the context of several limitations. First, we were unable to examine the effects of loss in medical insurance coverage as we selected for patients with continuous coverage through the study period. However, nationally, changes in coverage appeared to be considerably smaller than changes in employment during this period.[39] In addition, this methodologic choice allowed us to examine fill trends among a consistent cohort. Second, our classification of large heterogeneous medication classes may have obscured subtle changes in fill rates of individual medications. Furthermore, we did not examine changes in doses over this period because of the complexity of comparing doses of different agents within the same class and across age and sex groups. We also did not examine frequency of fills. Third, our data are limited to the first 13 weeks of the pandemic in California; subsequent studies may investigate the longer-term effects of the pandemic on psychotropic fill trends. Fourth, this study was conducted in a Northern California-based, large integrated health system with an insured population; our findings may not generalize to different patient populations, practice settings, or geographic regions. Last, the large sample sizes result in even small changes achieving statistical significance. For this reason, it is important to consider the clinical and policy significance of the observed trends alongside their statistical significance.
It is notable that the observed trends during the COVID pandemic occurred within the context of a longer term national increase in psychotropic medication prescribing, most notably for antidepressants[40] and benzodiazepines.[41] Therefore, ideally this study would have examined psychotropic prescription trends over a longer pre-COVID observation period. However, similar to multiple previous reports that have examined the effects of a natural or man-made disaster on psychotropic prescribing patterns,[27–36,42] we chose to focus on patterns during the pandemic and in the same period the year prior. Despite the limited observation period, this approach has the benefit of describing a single cohort across the entire observation period, thereby reducing patient-level variability.
5. Conclusion
In the early stages of the COVID-19 pandemic, psychotropic medication fills among adult members of a large, integrated health care system increased over about 1 month before returning to pre-pandemic rates. Fills of benzodiazepines and hypnotics either decreased or remained constant. These findings run counter to expectations that use of psychotropic medications, especially anxiolytics and sedatives, would increase during the pandemic.[43] These results are reassuring. Simultaneously, our findings should prompt clinicians, health system leaders, and social policy makers to ensure that patients are receiving appropriate non-pharmacologic interventions, including financial and family-based resources, to address the documented worsening of mental health associated with the pandemic.
Author contributions
Conceptualization: Matthew E Hirschtritt, Mark Olfson, Esti Iturralde.
Data curation: Natalie Slama.
Formal analysis: Natalie Slama.
Funding acquisition: Matthew E Hirschtritt, Esti Iturralde.
Investigation: Matthew E Hirschtritt, Esti Iturralde, Stacy A Sterling.
Methodology: Stacy A Sterling, Mark Olfson, Esti Iturralde.
Supervision: Matthew E Hirschtritt, Stacy A Sterling, Esti Iturralde.
Validation: Natalie Slama, Stacy A Sterling.
Writing – original draft: Matthew E Hirschtritt.
Writing – review & editing: Matthew E Hirschtritt, Natalie Slama, Stacy A Sterling, Mark Olfson, Esti Iturralde.
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: COVID-19 = coronavirus disease 2019, EHR = electronic health record, GEE = generalized estimating equation, KPNC = Kaiser Permanente Northern California, RRR = relative risk ratio.
How to cite this article: Hirschtritt ME, Slama N, Sterling SA, Olfson M, Iturralde E. Psychotropic medication prescribing during the COVID-19 pandemic. Medicine. 2021;100:43(e27664).
This research was supported by a research grant from the Division of Research, Kaiser Permanente Northern California, Oakland, CA (Drs Hirschtritt, Sterling, and Iturralde and Ms Slama). Dr Hirschtritt receives salary support from The Permanente Medical Group, Oakland, CA.
The granting agencies had no role in the design, analysis, interpretation, or publication of this study.
The authors report no financial relationships with commercial interests.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
Missing n = 27,292 (1.1%).
References
- [1].Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic – United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020;89:531–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Breslau J, Finucane ML, Locker AR, Baird MD, Roth EA, Collins RL. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev Med 2021;143:106362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic – United States, August 2020-February 2021. MMWR Morb Mortal Wkly Rep 2021;70:490–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Li Y, Qin Q, Sun Q, Sanford LD, Vgontzas AN, Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med 2020;16:1417–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res 2020;289:113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kokou-Kpolou CK, Megalakaki O, Laimou D, Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res 2020;290:113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].The COVID-19 Healthcare Coalition Telehealth Impact Study Work Group. Telecare impact: physician survey analysis. COVID-19 Healthcare Coalition. Published October 2020. Available at: https://c19hcc.org/telehealth/physician-survey-analysis/. Accessed December 21, 2020. [Google Scholar]
- [9].Express Scripts, Express Scripts. America's State of Mind Report. 2020;Available at: https://www.express-scripts.com/corporate/americas-state-of-mind-report. Accessed July 30, 2020. [Google Scholar]
- [10].Aitken M, Kleinrock M. Shifts in Healthcare Demand, Delivery, and Care during the COVID-19 Era; 2020. Available at: https://www.iqvia.com/insights/the-iqvia-institute/covid-19/shifts-in-healthcare-demand-delivery-and-care-during-the-covid-19-era. Accessed July 30, 2020. [Google Scholar]
- [11].Vaduganathan M, van Meijgaard J, Mehra MR, Joseph J, O’Donnell CJ, Warraich HJ. Prescription fill patterns for commonly used drugs during the COVID-19 pandemic in the United States. JAMA 2020;323:2524–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yu C, Boone C, Askarian-Monavvari R, Brown T. The trends in pharmacotherapy for anxiety, depression and insomnia during COVID-19: a North York area pilot study. Univ Toronto Med J 2021;98:41–6. [Google Scholar]
- [13].Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med 2020;180:1389–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc 2020;28:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kalicki AV, Moody KA, Franzosa E, Gliatto PM, Ornstein KA. Barriers to telehealth access among homebound older adults. J Am Geriatr Soc 2021;69:2404–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cook BL, Trinh N-H, Li Z, Hou SS-Y, Progovac AM. Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatr Serv 2017;68:09–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gordon N, Lin T. The Kaiser Permanente Northern California Adult Member Health Survey. Perm J 2016;20:15–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Graham DJ, Campen D, Hui R, et al. Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case-control study. Lancet 2005;365:475–81. [DOI] [PubMed] [Google Scholar]
- [19].Lam JR, Schneider JL, Quesenberry CP, Corley DA. Proton pump inhibitor and histamine-2 receptor antagonist use and iron deficiency. Gastroenterology 2017;152:821–9.e1. [DOI] [PubMed] [Google Scholar]
- [20].Schatz M, Zeiger RS, Vollmer WM, et al. Validation of a beta-agonist long-term asthma control scale derived from computerized pharmacy data. J Allergy Clin Immunol 2006;117:995–1000. [DOI] [PubMed] [Google Scholar]
- [21].Mauramo E, Lallukka T, Laaksonen M, Martikainen P, Rahkonen O, Lahelma E. Past and present socioeconomic circumstances and psychotropic medication: a register-linkage study. J Epidemiol Community Health 2012;66:1143–51. [DOI] [PubMed] [Google Scholar]
- [22].National Bureau of Economic Research, Imbens GM, Wooldridge JM. Recent Developments in the Econometrics of Program Evaluation. 2008;Available at: https://www.nber.org/system/files/working_papers/w14251/w14251.pdf. Accessed January 24, 2021. [Google Scholar]
- [23].Choo EK, Rajkumar SV. Medication shortages during the COVID-19 crisis: what we must do. Mayo Clin Proc 2020;95:1112–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Piatek OI, Ning JC-M, Touchette DR. National drug shortages worsen during COVID-19 crisis: proposal for a comprehensive model to monitor and address critical drug shortages. Am J Health Syst Pharm 2020;77:1778–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Micalizzi L, Zambrotta NS, Bernstein MH. Stockpiling in the time of COVID-19. Br J Health Psychol 2021;26:535–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Engstrom T, Baliunas DO, Sly BP, et al. Toilet Paper, minced meat and diabetes medicines: Australian panic buying induced by COVID-19. Int J Environ Res Public Health 2021;18:6954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Trifirò G, Italiano D, Alibrandi A, et al. Effects of L’Aquila earthquake on the prescribing pattern of antidepressant and antipsychotic drugs. Int J Clin Pharm 2013;35:1053–62. [DOI] [PubMed] [Google Scholar]
- [28].Rossi A, Maggio R, Riccardi I, Allegrini F, Stratta P. A quantitative analysis of antidepressant and antipsychotic prescriptions following an earthquake in Italy. J Trauma Stress 2011;24:129–32. [DOI] [PubMed] [Google Scholar]
- [29].Druss BG, Marcus SC. Use of psychotropic medications before and after Sept. 11, 2001. Am J Psychiatry 2004;161:1377–83. [DOI] [PubMed] [Google Scholar]
- [30].DiMaggio C, Galea S, Madrid PA. Population psychiatric medication prescription rates following a terrorist attack. Prehosp Disaster Med 2007;22:479–84. [DOI] [PubMed] [Google Scholar]
- [31].McCarter L, Goldman W. Use of psychotropics in two employee groups directly affected by the events of September 11. Psychiatr Serv 2002;53:1366–8. [DOI] [PubMed] [Google Scholar]
- [32].Austin PC, Mamdani MM, Jaakkimainen L, Hux JE. Trends in drug prescriptions among elderly residents of Ontario in the weeks after September 11, 2001. JAMA 2002;288:575–7. [DOI] [PubMed] [Google Scholar]
- [33].Fassaert T, Dorn T, Spreeuwenberg PMM, van Dongen MCJM, van Gool CJAW, Yzermans CJ. Prescription of benzodiazepines in general practice in the context of a man-made disaster: a longitudinal study. Eur J Public Health 2007;17:612–7. [DOI] [PubMed] [Google Scholar]
- [34].Han K-M, Kim K-H, Lee M, Lee S-M, Ko Y-H, Paik J-W. Increase in the prescription rate of antidepressants after the Sewol Ferry disaster in Ansan, South Korea. J Affect Disord 2017;219:31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Dorn T, Yzermans CJ, van der Zee J. Prospective cohort study into post-disaster benzodiazepine use demonstrated only short-term increase. J Clin Epidemiol 2007;60:795–802. [DOI] [PubMed] [Google Scholar]
- [36].Beaglehole B, Bell C, Frampton C, Hamilton G, McKean A. The impact of the Canterbury earthquakes on prescribing for mental health. Aust N Z J Psychiatry 2015;49:742–50. [DOI] [PubMed] [Google Scholar]
- [37].Mark TL, Levit KR, Buck JA. Datapoints: psychotropic drug prescriptions by medical specialty. Psychiatr Serv 2009;60:1167. [DOI] [PubMed] [Google Scholar]
- [38].Vahia IV, Jeste DV, Reynolds CF. Older adults and the mental health effects of COVID-19. JAMA 2020;324:2253–4. [DOI] [PubMed] [Google Scholar]
- [39].McDermott D, Cox C, Rudowitz R, Garfield R. How has the pandemic affected health coverage in the U.S.? Kaiser Family Foundation. Published December 9, 2020. Available at: https://www.kff.org/policy-watch/how-has-the-pandemic-affected-health-coverage-in-the-u-s/. Accessed May 12, 2021. [Google Scholar]
- [40].National Center for Health Statistics, Brody DJ, Gu Q. Antidepressant Use among Adults: United States, 2015–2018. 2020;Available at: https://www.cdc.gov/nchs/products/databriefs/db377.htm. Accessed May 28, 2021. [Google Scholar]
- [41].Agarwal SD, Landon BE. Patterns in outpatient benzodiazepine prescribing in the United States. JAMA Netw Open 2019;2:e187399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Usher K, Brown LH, Buettner P, et al. Rate of prescription of antidepressant and anxiolytic drugs after Cyclone Yasi in North Queensland. Prehosp Disaster Med 2012;27:519–23. [DOI] [PubMed] [Google Scholar]
- [43].Turban J, Gold J. The Pandemic is Spiking Anxiety. Before You Take Anti-anxiety Medication, Understand the Risks. WBUR. Published May 18, 2020. Available at: https://www.wbur.org/cognoscenti/2020/05/18/coronavirus-anxiety-benzos-jack-turban-jessica-gold. Accessed March 3, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.