Abstract
A new inpatient secondary preventive program for patients with musculoskeletal health problems was introduced throughout Austria. The aim of the current work was to evaluate this “Health Prevention Active” program and its possible influences on the quality of medical results upon hospital discharge.
This observational study presents monocentric data for 7448 patients (48.99 ± 6.15 years; 53.7% women) with chronic musculoskeletal disorders who completed a 3-week health program. The focus was placed on measuring medical quality outcomes such as BMI, blood pressure, heart rate, pain, subjective ratings, and achieved power output in cycle ergometer exercise testing. We describe pre-post changes before and after the inpatient program and the results of a follow-up survey conducted after 1 year to identify moderating factors related to health outcomes.
The medical baseline showed obvious deficits regarding obesity, hypertension, and subjective symptoms. Of all patients, 36.5% were completely inactive. The patient's gender and physical activity had a high impact on the medical baseline status. In total, the majority of patients (86.2%; SMD = –0.78 ± 0.59) responded well to the health prevention program, independent of their ages and lifestyles.
Requirements for secondary prevention programs are high. The results of the study reflect the general problems presented by inactivity, obesity, and subjective symptoms like pain. Physical activity was specifically identified as a major factor for the observed medical baseline status.
Keywords: chronic disease, health care, health promotion, musculoskeletal health, physical activity, program evaluation
1. Introduction
1.1. Background
Degenerative diseases of the musculoskeletal system are highly prevalent.[1] The most common symptom is back pain.[2–4] On the basis of a representative national health survey, musculoskeletal health problems were the most frequent reason (36%) for an inpatient rehabilitation; osteoarthritis of the knees/hips (17%) and back pain (13%) are the leading pathologies in musculoskeletal rehabilitation in Austria.[5,6] The number of rehabilitation stays has increased 4-fold, and the most common age group (48%) includes individuals between 45 and 65 years of age.
Special attention in health care is given to ailments that are common in modern society.[7–9] Due to lifestyle profiles and life-threatening conditions, physical activity has become increasingly important as a therapeutic approach to treat chronic diseases.[10,11] The risk of developing chronic diseases can be minimized by up to 50% by practicing an active lifestyle.[12,13] Prevention, professional health care, and multimodal programs are necessarily a part of the treatment of inflammatory or degenerative diseases.[14–21] In Austria, an insured person is entitled to receive medical rehabilitation care over a period of 3 weeks in specialized health (rehabilitation) centers.[22,23]
Outcome measurements are widely used in routine clinical rehabilitation and health care, but current and published results of multiple medical outcomes with individual patient data for inpatient health prevention programs are rare.[24–27]
1.2. Objectives
As part of a common data collection for the routine assessment of medical outcome quality, a prospective cohort study was conducted to evaluate the effectiveness and sustainability of a newly established inpatient health program. In this study, we tested the hypothesis that physical inactivity is one of the most important risk factors for the progression of musculoskeletal diseases.
2. Methods
A pre-post design was used in this study to perform monocentric routine outcome measurements in inpatient health care. The medical quality outcome measurements, which were previously established in the performance profile of the Austrian social security institutions, served as the basis for this work.[23] Descriptive, standardized, numeric medical indicators were provided for a 3-week inpatient health prevention program. Physicians and healthcare professionals performed the data collection during routine medical treatments.
2.1. Study design
To examine the effectiveness and sustainability of the inpatient health program, the health status and outcomes were recorded in a longitudinal cohort study and stratified to detect risk factors. After 1 year (2019), a follow-up survey was conducted with a random subsample of former inpatients. The standardized clinical characteristics of patients (Table 1) were recorded systematically upon the points of admission (t1), discharge (t2), and follow-up (t3) to test the hypothesis that physical activity is one of the most important risk factors for the progression of musculoskeletal disease.
Table 1.
Indicators of medical quality outcomes (outcome measures).
| Indicators for Medical Quality Outcome (MQOidx) | |||||
| General health indicators | Indication specific indicators | ||||
| MED1 | BMI | [kg/m2] | MED4 | Ergometer | [W] |
| Waist circumference | [cm] | ||||
| Shape | [z] | Performance | [z] | ||
| MED2 | Systolic blood pressure | [mm Hg] | MED5 | EQ5D-3L | [%] |
| Diastolic blood pressure | |||||
| Resting heart rate | [bpm] | ||||
| Cardiovascular | [z] | ADL (activities of daily living) | [z] | ||
| MED3 | VAS (pain) | [cm; 0–10] | ISI | (Indication) | |
| EQ VAS (self-rated health) | [%; 0–100] | Specific index | [z] | ||
| Subjective | [z] | MED4 and MED5 | |||
| GHI | (Nonspecific) General Health Index MED1, MED2, and MED3 | [z] | MQOidx | (Overall) Medical Quality Outcome GHI and ISI | [z] |
2.2. Setting and intervention
In 2018, after being tested for a 3-year pilot period, a new inpatient health prevention program “Gesundheitsvorsorge Aktiv” (GVA, “Health Prevention Active”) with a medical-secondary preventive focus replaced the classic, 3-week medical spa therapy in Austria. This program was offered as a voluntary service provided by the social insurance institutions.[22] Compared with an orthopedic rehabilitation, the inpatient health prevention program “GVA” plays a preventive role; the patients taking part in the program are generally younger and do not yet display disorders of the musculoskeletal system, which would require special rehabilitation treatments.
The modular structure of the GVA places a demand-oriented focus on exercise (motivation and optimization) and is characterized by an increased proportion of therapies that encourage physical activity which last on average 2 to 3 hours per day. Active treatments consist of physical activities such as gymnastic and individual physiotherapy sessions, and the training therapy emphasizes underwater, ergometer, Nordic walking, strength, balance, relaxation and motion forms of training. Passive treatments include massage, thermotherapy, electrotherapy, ultrasound and educational lessons, as well as psychological coaching. Each patient can take part in a program that includes a minimum of 1400 minutes of therapy over 3 weeks.
2.3. Study size and sample size estimation
A person is eligible to take part in the GVA inpatient program if they have a chronic disease of the musculoskeletal system without having undergone an acute event or recent surgical intervention on the musculoskeletal system. The GVA is a standardized health program and is publicly available to all socially insured patients with health limitations when medical treatment is deemed necessary to maintain their ability to work or to avoid the need for long-term care.
No patients had to be excluded from study participation. Their participation in the randomized follow-up subsample was on a voluntary basis. The number of cases was derived from the number of all patients treated at the study center (clinical trial center: Humanomed Center Althofen, Austria). Therefore, we did not estimate the sample size before carrying out this prospective cohort study. With a mean effect size and a power of 0.8, a total of 220 subjects would be needed to obtain a significant result for 4 subgroups with 3 measurements each (interaction effect: time × group, 4 × 3; α = 0.05), or 176 subjects to obtain a significant between-subjects factor (group), and a total of 156 subjects would be needed to obtain a significant within-subjects factor (time) effect.
2.4. Medical outcome quality measurements
The focus was placed on assessing general (nonspecific, body constitution based, and subjective discomfort[25,27]) and indication-specific measurements (activities of daily living [ADL] and physical capacity [performance]; Table 1). The summarized standardized mean differences correspond to the overall “Medical Quality Outcome” (MQOidx), the mean value of a general health index (GHI), and an indication specific index (ISI).
2.4.1. Primary and secondary outcome variables
Due to the inclusion of several outcome variables, the summary MQOidx served as the primary endpoint for assessing changes over time and identifying differences between stratified determinants of health status, such as gender, age, International statistical Classification of Diseases and related health problems-diagnosis, and BMI. The level of physical activity (PA) served as a predictor. General health variables and more disease-specific endpoints were presented as secondary outcome variables to allow a more detailed interpretation of changes or health status.
We followed the cohort over time to examine relationships between the predictor (stratified PA level before admission) with respect to the primary outcome variable and changes over time (health status, MQOidx).
2.4.2. Bias
Due to feasibility and ethical considerations, subjects were not selected randomly or by concealed assignment, and there was no control group. Correlations were expected between the outcome and PA in both directions, and these were confounded by lifestyle and environmental conditions. Statistical modeling, therefore, considered subgroups based on age and gender to examine the reliability and external validity of outcomes within each subgroup and to assess the influence of PA in a stratified manner.
2.5. Ethics approval
This study (Routine Outcome Parameters of an Inpatient Rehabilitation in Austria) was reviewed and approved by an ethics committee (IRB vote by the Ethics Committee of the Medical University of Graz, dated 02.05.2019, Protocol Number: 31-321 ex 18/19). Personal and health data were collected as part of routine medical care and quality management in accordance with the Declaration of Helsinki in the currently valid version. The patients were fully informed about the extent and purpose of the study and gave their written consent.
2.6. Statistical methods
Based on data distributions, the individual outcome indicators were transformed into z-values. A value of 50% (median) or a z-value of zero corresponded to the representative mean of the admission and discharge data for all patients at the clinical trial center. Changes between admission to discharge were revealed by examining the effect sizes and standardized mean differences (SMD). A larger positive absolute z-value corresponds to a below-average (worse) value in the sample. Negative z-differences (SMD) generally correspond to an improvement.
Statistical data processing was performed using IBM SPSS Statistics (version 27 IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). Individual missing values were not replaced for statistical analysis (not used for calculations). Unless otherwise stated, the sample size for calculations of statistical models was always as shown in Table 2 (N = 7448). The specification of P-values is only specified in borderline cases (if not explicitly stated: P < .001), and effect sizes were used instead (partial Eta2 [ηp2] and SMD).
Table 2.
Stratified sample—number of patients by main diagnoses, age, and sex.
| Classification according to ICD-10 | Number of patients | Age | Women | ||
| Localization/Main diagnosis | Abs. | % | Mean SD | Abs. | % |
| Back (spine) | 6448 | 86.6% | 48.84 ± 6.15 | 3491 | 54.1% |
| M54, M53 (M51, M50) | |||||
| Knee | 228 | 3.1% | 50.38 ± 5.98 | 102 | 44.7% |
| M17 (M22, M23) | |||||
| Hip | 98 | 1.3% | 50.65 ± 5.24 | 46 | 46.9% |
| M16 | |||||
| Shoulder | 155 | 2.1% | 49.88 ± 5.49 | 85 | 54.8% |
| M75 | |||||
| Other osteoarthritis | 303 | 4.1% | 50.29 ± 5.93 | 155 | 51.2% |
| M25, M15, M19 (M18) | |||||
| Other | 79 | 1.1% | 48.96 ± 6.48 | 51 | 64.6% |
| M77, M06, M35 (M76, M79) | |||||
| Other diseases (musculoskeletal system) | 137 | 1.8% | 48.81 ± 6.84 | 73 | 53.3% |
| ICD-10 Kat. (<n = 3) | |||||
| Total | 7448 | 100.0% | 48.99 ± 6.15 | 4003 | 53.7% |
3. Results
3.1. Participants
During the study period of 2016 to 2018, patients (N = 7448) with different medical diagnoses (48.99 ± 6.15 years, 53.7% women, Table 2) were enrolled in a specialized interdisciplinary medical institution to receive health care.
The average length of an inpatient stay was 21.73 ± 1.85 days. Of all patients, 1.9% prematurely discontinued their inpatient treatment due to a loss of health capacity (e.g., acute illness) or for private reasons. A categorization of the reasons for hospital treatments was based on the referral diagnosis. Almost every patient suffered from several chronic diseases, such as obesity, hypertension, or another musculoskeletal or metabolic disease (Table 2). The most frequent, main diagnosis at the study center was dorsalgia (M54).
3.1.1. Descriptive data
An examination of the medical initial values (IV, baseline, pre) clearly revealed the deficits of the affected patients (see Table, Supplemental Digital Content 1 that illustrates all available secondary outcome variables for male and female patients to allow a more detailed interpretation of health status). The average BMI was 27.97 ± 5.11 kg/m2 (30.3% of patients had a BMI > 30), and 23.7% of patients had “high-normal” or “hypertensive” (48.4%) blood pressure values (mean RR sys/dia.: 128.64/77.27 ± 12.18/7.7 mmHg). The perceived pain (VAS; 0–10) of patients was 4.79 ± 1.85. Comparing the initial values for the averaged medical factors (MQO) with those of healthy people, a huge difference could be detected between overall MQOidx for patients (0.39 ± 0.94; Table 3) and that of healthy people (–1.15[27]) with a z-difference of –1.54.
Table 3.
Summarized medical quality outcome and physical activity before admission.
| MQO: Medical Quality Outcome—inpatient health care program (GVA) | ||||||
| [z, z-difference (SMD)] | Physical activity∗ (PA) | Baseline, Pre† (mean ± SD) | Mean diff.‡ (SMD ± SD) | 95% CI | Within factor time (ηp2) | Between factor§ PA (ηp2) |
| Nonspecific mean (MED1, MED2, MED3) | 0 min | 0.63 ± 0.96 | −0.82 ± 0.69 | [−0.85 −0.79] | 0.586 | |
| <150 | 0.27 ± 0.92 | −0.75 ± 0.68 | [−0.78 −0.71] | 0.550 | ||
| 150–300 | 0.16 ± 0.9 | −0.73 ± 0.65 | [−0.76 −0.70] | 0.554 | ||
| >300 min | 0.15 ± 0.95 | −0.73 ± 0.67 | [−0.77 −0.69] | 0.540 | ||
| General Health Index (GHI) | 0.35 ± 0.96 | −0.76 ± 0.67 | [−0.77 −0.74] | 0.560 | 0.054 | |
| Overall MQOidx mean (GHI, ISI) | 0 min | 0.61 ± 0.86 | −0.81 ± 0.54 | [−0.83 −0.79] | 0.692 | |
| <150 | 0.32 ± 0.85 | −0.76 ± 0.52 | [−0.79 −0.74] | 0.687 | ||
| 150–300 | 0.15 ± 0.82 | −0.75 ± 0.53 | [−0.77 −0.73] | 0.667 | ||
| >300 min | 0.08 ± 0.93 | −0.75 ± 0.53 | [−0.78 −0.72] | 0.662 | ||
| Medical Quality Outcome (MQOidx) | 0.39 ± 0.94 | −0.78 ± 0.59 | [−0.79 −0.76] | 0.637 | 0.066 | |
| Disease-specific mean (MED4, MED5) | 0 min | 0.34 ± 0.96 | −0.43 ± 0.40 | [−0.45 −0.42] | 0.542 | |
| <150 | 0.25 ± 0.94 | −0.43 ± 0.38 | [−0.45 −0.41] | 0.559 | ||
| 150–300 | 0.10 ± 0.90 | −0.43 ± 0.42 | [−0.45 −0.41] | 0.506 | ||
| >300 min | −0.01 ± 1.01 | −0.43 ± 0.42 | [−0.45 −0.40] | 0.507 | ||
| Indication specific index (ISI) | 0.20 ± 0.95 | −0.43 ± 0.41 | [−0.44 −0.42] | 0.523 | 0.019 | |
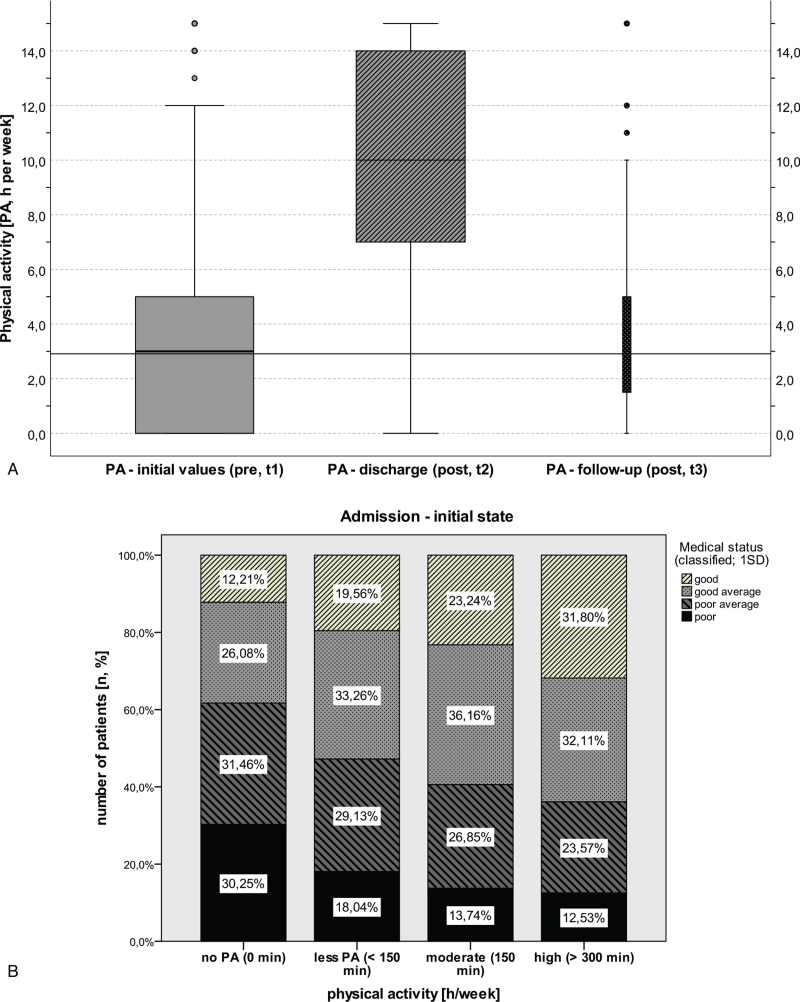
Of all patients, 36.5% were not physical active at all, and 20.1% exercised <150 minutes a week (Fig. 1A). Less daily physical activity (PA) was associated with a poor medical status upon admission (MQO: ηp2 = 0.065; Fig. 1B). The correlation between the factor PA with medical indicators at admission was observed for all medical indicators (see Table 3 and Table, Supplemental Digital Content 3 that illustrates statistical modeling [GLM] results to allow comparison of effects on outcome variables among predictors).
Figure 1.
A, B: PA and medical status at admission. Patients reported physical activity (PA) of about 2.91 ± 3.85 hours per week before starting their inpatient stay, and 36.5% of all patients were not physically active at all. PA in leisure time increased by 6.59 ± 4.87 hours per week (ηp2 = 0.653), but returned to the extent at the beginning of the GVA, around 3.50 ± 2.70 hours in follow-up (Fig. 1A). The baseline medical condition depended strongly on physical activity (ηp2 = 0.065; Fig. 1B), indicating that patients with no or less physical activity had a poor health status (initial value MQO classified: <–1SD, –1SD–0, 0–1SD, <1SD). GVA = “Gesundheitsvorsorge Aktiv” [“Health Prevention Active” program].
3.2. Main results
3.2.1. Outcome of the inpatient health prevention program
The overall improvement in MQOidx was around 22.84 ± 17.67 percentile points or a SMD of –0.78 ± 0.59 (radmission-discharge = 0.78; d = 1.31, 95% CI [–1.35, –1.28]). 86.2% of the patients showed improvements immediately after the end of the health program (cut-off: SMD < –0.20). The status of 10.6% of the patients remained unchanged (0.00 ± 0.20), and 3.2% worsened (>0.20) between the beginning and the end of the program (MQOidx). The detailed analysis of average improvement with respect to different health features is shown in Table 3 (and in Tables, Supplemental Digital Content 1–3 that illustrate all available outcome variables to allow a more detailed interpretation of health status, changes and effect sizes). The most pronounced effects could be seen upon analyzing the subjective symptoms of complaints, whereby almost every patient (92.3%) reported a significant improvement (SMDMED3 = –1.06 ± 0.69).
The correlations between the absolute values and changes in general health index with specific index were low (r < 0.100). The extent of improvement in medical outcome and the effect size were strong in all areas (MQOidx: ηp2 = 0.637 see Table 3 and Tables, Supplemental Digital Content 1–3 that illustrate all available outcome variables to allow a more detailed interpretation of changes and effect sizes).
3.2.2. Influencing factors for initial medical values and outcome
If one compares admission and discharge values as a result of the inpatient health care stay, we need to evaluate possible moderating factors like lifestyle (PA), gender, age, and referral diagnosis. In general, between-factors had only a minor influence on the outcome of the health prevention program (interaction) as compared with their influence on initial values (see Table, Supplemental Digital Content 3 that illustrates statistical modeling [GLM] results to allow comparison of effects on outcome variables among predictors).
As shown (Fig. 1B, Table 3), a lower daily PA was associated with a poor medical status at the time of admission. From the beginning of the health prevention program up until the end, PA in leisure time increased by 6.59 ± 4.87 hours per week (ηp2 = 0.653). The correlation between PA before and at the end of the program was low (r = 0.242).
The number of obese men (BMI > 25 kg/m2; 80.4%) exceeded that of women (62%; GenderMED1: ηp2 = 0.042), and male patients were more often hypertensive (60.3% vs female patients: 38.3%; GenderMED2: ηp2 = 0.053; see Tables, Supplemental Digital Content 1–3 that illustrate all available outcome variables to allow a more detailed interpretation of health status, changes, and effect sizes). On the other hand, women reported subjectively more complaints (like painVAS: 4.97 vs 4.59; GenderMED3: ηp2 = 0.026) and expected poorer performance on the cycle ergometer (GenderMED4: ηp2 = 0.410). Men displayed better results for objectively measurable parameters, such as shape and cardiovascular indicators and in physical performance.
After adjusting the data to account for different initial states (IVMQO), the men were shown to be more responsive to the GVA program than women (time × gender with covariate IVMQO: ηp2multivariate = 0.070, ηp2MED1 = 0.019, ηp2MED2 = 0.030, ηp2MED4 = 0.029; see Table, Supplemental Digital Content 3 that illustrates statistical modeling [GLM] results to allow comparison of effects on outcome variables among predictors). Older patients had poorer medical initial statuses (MQO: ηp2 = 0.020) and especially had worse physical performance (MED4: ηp2 = 0.021). In general, improvements were similar in each age group (MQOidx: ηp2 = 0.001; P = .251); the diagnosis was a weak influencing factor for medical status (e.g., MED1: ηp2 = 0.010; knee patients were in noticeably worse “shape”) and changes in medical indicators due the health prevention program between diagnoses were comparable in magnitude (MQO: ηp2 = 0.001, P = .169). The medical initial values (IVMQO) had the strongest moderating effects on the outcome predictions, as poor initial values positively correlated with better medical outcome (e.g., GHI: ηp2 = .118).
Overall, short-term improvements were clearly visible in all factors and for all subgroups. PA, gender, and especially initial values had moderate influences on the outcome, the health prevention program was effective for the affected patient group, depending on the overall medical outcome.
3.3. Further analyses—sustainability
In a random subsample (n = 532), who had visited a GVA in the last 12 to 16 months, a follow-up survey was done in autumn 2019 (response rate: 31.6%). Responders were representative according to gender, diagnosis, age, and short-term success rates (changes) due to the inpatient health program (Pmultivariate = .804). In addition to patient-reported outcomes (PA, BMI, VAS, VAS valuations of EQ-5D [self-rated health in %; 0–100], and ADL; see Table 1) sick leaves and work activity had been subjectively assessed.
The physical activity returned to the extent at the beginning of the GVA, around 3.50 ± 2.70 h in the follow-up, whereas patients with absolutely no PA in the subsample proportionally decreased from 16% to 6% (P < .01). Sustainable effects compared to admission of GVA and around 1 year later were visible (Pmultivariate = .001, ηp2 = 0.113): pain (VAS: Punivariate < .001, ηp2 = 0.086) and shape indicators (BMI: Punivariate < .001, ηp2 = 0.094) were still better than before the program; significant, long-lasting, positive changes in ADL were not observed (MED5: Punivariate = .280, ηp2 = 0.011).
PA before admission was a main (between) factor that could be used between subjects to estimate medical indicators over the time-course (Pmultivariate = .019; ηp2 = 0.047) and, besides the initial state (Pmultivariate = .000; ηp2 = 0.186), it was identified as the best predictor for prognosis.
Of the post survey sample, 89.5% were gainfully employed 1 year after the health program, and only 4.6% were unemployed. Sick leave taken over the last 12 months was about 2 weeks, which roughly corresponds to the average in the population.[28] On a VAS [0–10], the GVA was regarded as a necessary support (9.24 ± 1.48) that could sustainably improve the ability to work (6.69 ± 2.91) and lifestyle (6.25 ± 2.80). Of those who took part in the program, 77.6% were “very satisfied” and 18.4% “satisfied” with the inpatient program [Likert Scale: 0–4].
4. Discussion
Observational studies provide important data on changes that occur during the recovery process. To examine the effectiveness and sustainability of the inpatient health program, health status, and outcomes were considered in a longitudinal cohort study, stratified by levels of physical activity and gender. The secondary preventive program “GVA,” which has been designed for patients with musculoskeletal health problems, prioritizes active treatments like physical exercise and training therapy. Based on a common and mandatory routine data collection process, general health- and disease-specific medical measurements were extracted from the electronic patient records and summarized to obtain an overall medical outcome (MQOidx) as the primary endpoint. We evaluated the expected changes related to an inpatient prevention program as well as the influences on pre-health care medical conditions and gender differences, testing the hypothesis that physical inactivity is one of the most important risk factors for the progression of musculoskeletal diseases.
4.1. Main findings of the present study
An examination of the medical initial values (IV, baseline, pre) clearly revealed the deficits of the affected patients in general and disease-specific health measures, such as BMI, blood pressure, pain, and mobility status. Most of the patients performed <150 minutes of physical activity per week. Physical activity was identified as major factor that influenced the observed medical health status.
Our results show that most patients with chronic musculoskeletal problems clearly benefited from taking part in a 3-week inpatient health prevention program, independent of their ages and physical activity levels before the health program. When we compared the values upon discharge with the initial medical evaluation data, we noted that 86.2% of patients benefited from the inpatient health care stay. However, 13.8% did not show significant changes from beginning to the end of the program, and the sustainability after 1 year was low.
4.2. Comparison with other studies
The study findings confirm the results of previous studies. The effect sizes of the secondary prevention program “GVA” are comparable to those of inpatient orthopedic rehabilitation.[27] The role of physical activity and multimodal inpatient treatments on health parameters is well-known[29–31] in that it restores physiological functions and helps individuals pursue secondary preventive goals, enabling their quality of life and the functionality of health care to be improved without increasing costs.[18,32]
Since the 1970s, the topic of gender and its impact on health has increased in relevance, both in research and in medical practice. It is known that women report more severe postoperative pain and reduced overall functional ability as compared with men.[33] These results indicate that gender-specific considerations need to be made in health prevention programs and treatments. Cardiac rehabilitation studies have shown that women have significantly lower baseline measures, and there is evidence that they do not improve their cardiorespiratory fitness as much as men, respectively, a differing response is evident.[34,35] This can also be confirmed by our data, we observed that gender affected the medical outcome (success) differently. Men were more frequently affected and showed better results in terms of obesity and hypertension, while women showed slightly better improvements in their reported major complaints. Taking into account the different initial values used for women and men as covariates, gender still influenced the results or even emerged as a primary determinant. The demand-oriented focus on exercise with an increased proportion of physically active therapies in the GVA program may have led to the observed better responsiveness in men.
4.3. Implication and explanation of findings
There is a clear need for standardized methods that can be used to collect, analyze, and report gender-specific information to improve outcomes.[36] Normative values for an evaluation like the secondary prevention program “GVA” are not available. Therefore, the present work provide a valid basis for the routine assessment of the quality of medical outcomes based on a common data collection strategy.
We observed that the GVA program had a strong health care effect on all subgroups. This success is likely to be transferable to all inpatient health or rehabilitation stays, as is the preventive effect of physical activity in this environment. The findings of our study underline the fact that the lack of PA or exercise is one of the biggest problems facing members of our society.[37,38] Beside PA, BMI, and gender, the medical initial status was the most important main factor identified between subjects, allowing an estimation of medical indicators over the time-course. Despite the existence of large international differences in healthcare teams and treatment measures in health prevention programs and rehabilitation centers, the presented effect sizes can support individual evaluation.
4.4. Strengths and limitations
Published results of multiple medical outcomes of secondary prevention programs are rare. Stratified outcome scores for evidence-based determinants of health status are essential for health care delivery, because the baseline medical condition has the strongest moderating effect on outcome. Our results allow an evaluation within individuals and provide a normative basis to compare different treatment pathways.
The summarized overall “Medical Quality Outcome” clearly revealed the reduced health statuses of the affected patients, which clearly differ from those of healthy people. A broad definition is used for this primary endpoint, including basic health characteristics and the functional and mobility status. In addition to the summary and importance of the different outcome variables, the primary variable is often systematically related to other influences apart from treatment. Health and physical activity can be both causes and responses, which elicit different responses in different individuals. On the one hand, physical inactivity itself may be causal as a risk factor (PA as a stratified risk factor or covariate), and, on the other hand, it may represent the effect of a chronic disease (PA as outcome measure). The complexity is highlighted by the heterogeneity of factors confounding the measures, or even the use of different definitions and operationalization methods. Therefore, several factors may influence the course of convalescence in rehabilitation and lead to discrepancies in outcomes, especially if differences in baseline values are not separated by genuine confounders such as PA. In addition, our findings suggest the need for gender considerations in health assessment and treatment.
For ethical, practical, and economic reasons, it was not possible to include a randomized control group in this study. Due to the study design, causal conclusions must be drawn with caution. The beneficial effects resulting from participation in an inpatient health prevention program for well-being may not be sustainable, once the patients return to their usual everyday lives[39] and physical activity returns to the level before the health program. However, even minor changes in lifestyle can lead to functional adaptations and normalization of physiological functions and help the patient to recover from chronic inflammatory or degenerative diseases.[40,41]
Due to the use of standardized performance profiles, external reviews and the fact that insurers centrally control the assignment of modalities, we assume that the initial values and outcomes are representative for the inpatient health prevention program (GVA) in Austria.
5. Conclusion
Physical activity has become increasingly important and is one of the most important risk factors for the progression of musculoskeletal diseases. Professional health care and multimodal programs are necessary as part of the treatment of inflammatory or degenerative diseases to maintain the ability to work or to avoid the need for long-term care. The standardization and provision of stratified normative values can make an important contribution to a more personalized medicine. Future research will be carried out to clarify the length of the impact of an inpatient health program and determine what further support is needed to optimize treatment pathways and sustainability.
Acknowledgments
The authors thank the Humanomed Group and their colleagues and the Medical University of Graz as well as the Ludwig Boltzmann Institute for their support in the development and execution of this study.
Author contributions
Each author of this work was significantly involved in the conception, design, data acquisition, data analysis and interpretation. All authors helped write the manuscript and have approved this final version for publication. All authors take responsibility for the accuracy and integrity of all aspects of research. The individual authors had the following respective main tasks:
Conceptualization: Vincent Grote, Elke Böttcher.
Data curation: Vincent Grote, Alexandra Unger, Elke Böttcher.
Formal analysis: Vincent Grote, Maximilian Moser, Elke Böttcher.
Investigation: Vincent Grote, Elke Böttcher, Alexandra Unger.
Methodology: Vincent Grote, Michael Fischer.
Project administration: Elke Böttcher, Vincent Grote.
Resources: Elke Böttcher, Michael Fischer.
Supervision: Peter Hofmann, Maximilian Moser, Michael Fischer.
Validation: Elke Böttcher, Peter Hofmann, Maximilian Moser, Michael Fischer.
Visualization: Vincent Grote.
Writing – original draft: Vincent Grote, Elke Böttcher, Alexandra Unger.
Writing – review & editing: Vincent Grote, Elke Böttcher, Peter Hofmann, Maximilian Moser, Michael Fischer.
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: ηp2 = effect size (partial Eta2), ADL = activities of daily living, BMI = body mass index, EC = Ethics Committee, GHI = general health index (mean value of MED1, MED2, MED3; z), GVA = “Gesundheitsvorsorge Aktiv” [“Health Prevention Active” program], h = hours, ICD = International statistical classification of diseases and related health problems, idx = index for outcome (z), ISI = indication specific index (mean value of MED4, MED5; z), IV = initial value (baseline, pre), MED1 = shape indicator of MQO (BMI and waist circumference; z), MED2 = cardiovascular indicator of MQO (RR and RHR; z), MED3 = subjective indicator of MQO (VAS and EQ-VAS; z), MED4 = performance indicator of MQO (ergometer power in watts; z), MED5 = ADL indicator of MQO (EQ-5D; z), MQO = medical quality outcome (mean value of GHI and ISI; z), N (n) = sample size, P = significance level (risk of error), PA = physical activity, r = correlation coefficient (Pearson), RHR = resting heart rate, RR = Riva-Rocci (abbreviation for blood pressure measurements), SD = standard deviation, SMD = standardized mean difference, VAS = visual analogue scale (perceived pain; 0–10), z = z-value, standard score (scale: 0 ± 1; mean ± SD).
How to cite this article: Grote V, Böttcher E, Unger A, Hofmann P, Moser M, Fischer MJ. Observational study of an inpatient program for musculoskeletal disorders: The effects of gender and physical activity. Medicine. 2021;100:43(e27594).
This study was supported by the Ludwig Boltzmann Society, Vienna. The researchers did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. VG was and EB is employed at the clinical trial center (Humanomed Center Althofen, Austria). All other authors had no relationship to the study center.
Data availability: The datasets analyzed in this manuscript are not publicly available, because ethical and legal restrictions (data contain potentially identifying and sensitive patient information). If not already reported within this work, the authors may provide descriptive data on individual medical indicators for admission and discharge or the expected change due to inpatient health care for various groups and diagnoses. Requests for access to anonymized datasets should be directed to vincent.grote@rehabilitation.lbg.ac.at.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
Quality-of-outcome measures were documented in the discharge report at the beginning and at the end of the inpatient health prevention program. The overall MQOidx (primary outcome) and GHI, ISI (secondary outcome) were calculated for each patient for the initial and discharge statuses, and the difference between those factors (difference: post-pre) was used as an individual success factor for the health prevention program.
The total sample included 7765 patients, the analysis sample consisted of 7448 patients (95.9%) who had accrued more than 17 days of a health care stay and valid measurements for admission and discharge. From a total sample, 167 patients (2.1%) had missing values, and 150 patients (1.9%) prematurely discontinued their inpatient treatment (dropouts).
Primary endpoint, aggregated medical outcome factors (GHI and ISI) showed that the program was clearly successful during the health care stay for 86.2% of patients (MQOidx; threshold SMD < –0.2). The medical initial states clearly differed according to different amounts of physical activity (stratified predictor) in all medical indicators, but not for changes due to the inpatient health prevention program (see Table, Supplemental Digital Content 3 that illustrates statistical modeling [GLM] results to allow comparison of effects on outcome variables among predictors).
N = 7,448 (48.99 ± 6.15 years, 53.7% female, 46.3% male patients).
MED1 = –6.25 + BMI∗0.10 + WC∗0.04; MED2 = –11.73 + RRdia∗0.07 + RRsys∗0.04 + RHR∗0.02; MED3 = 1.72 + VAS∗0.26 + EQVAS∗–0.04 (WC, waist circumference; RR, blood pressure sys./dia.; RHR, resting heart rate; VAS, Visuelle Analog Scale; EQ-VAS, self-rated health).
PA before admission to GVA (h per week; 0 min: 36.5%, <150 min: 20.1%, 150–300 min: 27.5%, >300 min: 15.9%).
A positive z-value corresponds to a below-average value (0 = no significant changes between pre vs post).
Average improvement from admission (pre, t1) to discharge (post, t2): standardized mean difference (SMD) = zpost − zpre.
GLM for repeated measurements (2 × 4 design): within factor time (2) and between factor PA (4): all P < .001.
References
- [1].Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain-where to from here? Am J Public Health 2019;109:35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Edwards J, Hayden J, Asbridge M, Gregoire B, Magee K. Prevalence of low back pain in emergency settings: a systematic review and meta-analysis. BMC Musculoskelet Disord 2017;18:143.doi: 10.1186/s12891-017-1511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012;64:2028–37. [DOI] [PubMed] [Google Scholar]
- [4].Alzahrani H, Cheng SWM, Shirley D, Mackey M, Stamatakis E. Physical activity and health-related quality of life in people with back pain: a population-based pooled study of 27,273 adults. J Phys Activ Health 2020;17:177–88. [DOI] [PubMed] [Google Scholar]
- [5].Hospital discharge statistics 2018 [press release]. Press release: 12.130-196/19, 18.11.2019 2019. [Google Scholar]
- [6].Klimont J, Baldaszti E, Ihle P, Unger W, Arrouas M. Österreichische Gesundheitsbefragung 2014 [Austrian Health Survey 2014]. Wien; 2015. [Google Scholar]
- [7].Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lewis R, Gomez Alvarez CB, Rayman M, Lanham-New S, Woolf A, Mobasheri A. Strategies for optimising musculoskeletal health in the 21(st) century. BMC Musculoskelet Disord 2019;20:164.doi: 10.1186/s12891-019-2510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Collaborators GBDD. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;393:1958–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 2015;25: (suppl): 01–72. [DOI] [PubMed] [Google Scholar]
- [11].Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [DOI] [PubMed] [Google Scholar]
- [12].Thornton JS, Fremont P, Khan K, et al. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the canadian academy of sport and exercise medicine. Clin J Sport Med 2016;26:259–65. [DOI] [PubMed] [Google Scholar]
- [13].Nunan D, Mahtani KR, Roberts N, Heneghan C. Physical activity for the prevention and treatment of major chronic disease: an overview of systematic reviews. Syst Rev 2013;2:56.doi: 10.1186/2046-4053-2-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Marin TJ, Van Eerd D, Irvin E, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Syst Rev 2017;6:CD002193.doi: 10.1002/14651858.CD002193.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Meyer C, Denis CM, Berquin AD. Secondary prevention of chronic musculoskeletal pain: a systematic review of clinical trials. Ann Phys Rehabil Med 2018;61:323–38. [DOI] [PubMed] [Google Scholar]
- [16].Singh R, Kucukdeveci AA, Grabljevec K, Gray A. The role of interdisciplinary teams in physical and rehabilitation medicine. J Rehabil Med 2018;50:673–8. [DOI] [PubMed] [Google Scholar]
- [17].Furlan AD, Irvin E, Munhall C, et al. Rehabilitation service models for people with physical and/or mental disability living in low- and middle-income countries: a systematic review. J Rehabil Med 2018;50:487–98. [DOI] [PubMed] [Google Scholar]
- [18].Howard-Wilsher S, Irvine L, Fan H, et al. Systematic overview of economic evaluations of health-related rehabilitation. Disabil Health J 2016;9:11–25. [DOI] [PubMed] [Google Scholar]
- [19].Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ 2015;350:h444.doi: 10.1136/bmj.h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Stucki G, Bickenbach J, Gutenbrunner C, Melvin J. Rehabilitation: the health strategy of the 21st century. J Rehabil Med 2018;50:309–16. [DOI] [PubMed] [Google Scholar]
- [21].Schwarz B, Neuderth S, Gutenbrunner C, Bethge M. Multiprofessional teamwork in work-related medical rehabilitation for patients with chronic musculoskeletal disorders. J Rehabil Med 2015;47:58–65. [DOI] [PubMed] [Google Scholar]
- [22].Bachner F, Bobek J, Habimana K, et al. Austria: health system review. Health Syst Transit 2018;20:01–254. [PubMed] [Google Scholar]
- [23].Gyimesi M, Fülöp G, Ivansits S, et al. Rehabilitationsplan 2016 [Rehabilitation plan 2016]. Vienna: Hauptverband der österreichischen Sozialversicherungsträger [Main Association of Austrian Social Security Organizations]; 2016. [Google Scholar]
- [24].Schuler M, Murauer K, Stangl S, et al. Pre-post changes in main outcomes of medical rehabilitation in Germany: protocol of a systematic review and meta-analysis of individual participant and aggregated data. BMJ Open 2019;9:e023826.doi: 10.1136/bmjopen-2018-023826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Grote V, Böttcher E, Mur E, Kullich W, Puff H. Medical Quality Outcomes: Unspecific Outcome Parameters of an Inpatient Musculoskeletal System Rehabilitation in Austria. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin 2019;29:104–17. [Google Scholar]
- [26].Grote V, Unger A, Puff H, Böttcher E. Bernardo-Filho M, Sá-Caputo D, Taiar R. What to expect: medical quality outcomes and achievements of a multidisciplinary inpatient musculoskeletal system rehabilitation. Physical Therapy Effectiveness. London, United Kingdom: IntechOpen; 2020. 65–91. https://www.intechopen.com/contact-us [Google Scholar]
- [27].Grote V, Unger A, Bottcher E, et al. General and disease-specific health indicator changes associated with inpatient rehabilitation. J Am Med Dir Assoc 2020;21:2017.e2010–27. [DOI] [PubMed] [Google Scholar]
- [28].Leoni T. Absenteeism report 2019. Vienna: Austrian Institute of Economic Research; 2019. [Google Scholar]
- [29].Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ 2006;174:801–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].WHO. Global action Plan on Physical Activity 2018-2030: More Active People for a Healthier World. Geneva, Switzerland: World Health Organization; 2018. [Google Scholar]
- [31].Luan X, Tian X, Zhang H, et al. Exercise as a prescription for patients with various diseases. J Sport Health Sci 2019;8:422–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Krischak G, Tepohl L, Dannenmaier J, Hartschuh U, Auer R, Kaluscha R. Health economic effects of rehabilitation for chronic back pain - an observational study with combined secondary data from statutory health Insurance and German Pension Fund. Rehabilitation (Stuttg) 2019;58:392–7. [DOI] [PubMed] [Google Scholar]
- [33].Choong ALC, Shadbolt C, Dowsey MM, Choong PFM. Sex-based differences in the outcomes of total hip and knee arthroplasty: a narrative review. ANZ J Surg. 91, 553–7. [DOI] [PubMed] [Google Scholar]
- [34].Rengo JL, Khadanga S, Savage PD, Ades PA. Response to exercise training during cardiac rehabilitation differs by sex. J Cardiopulmon Rehabil Prev 2020;40:319–24. [DOI] [PubMed] [Google Scholar]
- [35].Parker BA, Kalasky MJ, Proctor DN. Evidence for sex differences in cardiovascular aging and adaptive responses to physical activity. Eur J Appl Physiol 2010;110:235–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Beck JJ, Pandya NK, Carter CW, Mulcahey MK. Current concept review: inclusion and analysis of diverse study populations in orthopaedic research. J Am Acad Orthop Surg: . 2021;29:e479–e87. [DOI] [PubMed] [Google Scholar]
- [37].Trost SG, Blair SN, Khan KM. Physical inactivity remains the greatest public health problem of the 21st century: evidence, improved methods and solutions using the ’7 investments that work’ as a framework. Br J Sports Med 2014;48:169–70. [DOI] [PubMed] [Google Scholar]
- [38].WHO. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- [39].Oliveira CB, Franco MR, Maher CG, et al. Physical activity interventions for increasing objectively measured physical activity levels in patients with chronic musculoskeletal pain: a systematic review. Arthritis Care Res (Hoboken) 2016;68:1832–42. [DOI] [PubMed] [Google Scholar]
- [40].Strauss-Blasche G, Ekmekcioglu C, Klammer N, Marktl W. The change of well-being associated with spa therapy. Forsch Komplementarmed Klass Naturheilkd 2000;7:269–74. [DOI] [PubMed] [Google Scholar]
- [41].Grote V, Levnajic Z, Puff H, et al. Dynamics of vagal activity due to surgery and subsequent rehabilitation. Front Neurosci 2019;13:1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.