Abstract
Objectives
The COVID-19 pandemic has had an effect on the incidence of infectious diseases and medical care. This study aimed to describe the impact of the COVID-19 pandemic on community-level antibiotic use.
Methods
Using national antibiotic dispensing data from IQVIA's CompuScript database, this ecological study investigated antibiotic dispensing through community retail pharmacies in Canada from November 2014 to October 2020. Analyses were stratified by age, sex, prescription origin and approximate indication.
Results
Adjusting for seasonality, the national rate of antibiotic dispensing in Canada decreased by 26.5% (50.4 to 37.0 average prescriptions per 1000 inhabitants) during the first 8 months of the Canadian COVID-19 period (March to October 2020), compared with the pre-COVID-19 period. Prescribing rates in children ≤18 years decreased from 43.7 to 12.2 prescriptions per 1000 inhabitants in males (–72%) and from 46.8 to 14.9 prescriptions per 1000 inhabitants in females (–68%) in April 2020. Rates in adults ≥65 decreased from 74.9 to 48.8 prescriptions per 1000 inhabitants in males (–35%) and from 91.7 to 61.3 prescriptions per 1000 inhabitants in females (–33%) in May 2020. Antibiotic prescriptions from family physicians experienced a greater decrease than from surgeons and infectious disease physicians. Prescribing rates for antibiotics for respiratory indications decreased by 56% in May 2020 (29.2 to 12.8 prescriptions per 1000 inhabitants), compared with prescribing rates for urinary tract infections (9.4 to 7.8 prescriptions per 1000 inhabitants; –17%) and skin and soft tissue infections (6.4 to 5.2 prescriptions per 1000 inhabitants; –19%).
Discussion
The first 8 months of the COVID-19 pandemic reduced community antibiotic dispensing by 26.5% in Canada, compared with the marginal decrease of 3% in antibiotic consumption between 2015 and 2019. Further research is needed to understand the implications and long-term effects of the observed reductions on antibiotic use on antibiotic resistance in Canada.
Keywords: Antibiotic, Antibiotic use, Antimicrobial, Antimicrobial stewardship COVID-19, Epidemiology
Introduction
The COVID-19 pandemic has had an unparalleled impact on the Canadian healthcare system. While much of the focus of clinical care and research of COVID-19 has been in the inpatient setting, the access and delivery of primary care services in Canada has dramatically changed, including a notable shift towards virtual care [1,2]. Additionally, physical distancing policies enacted during the pandemic period may have reduced the transmission of communicable pathogens, such as influenza and respiratory syncytial virus and obviated the need for some assessments and antibiotic prescribing (both appropriate and inappropriate) [3]. Whether directly related to changes to primary care accessibility and delivery or from fewer patients seeking medical care, there has been an overall decrease in the number of physician interactions in Canada [1,2], which can have downstream impacts on prescribing. For these reasons, we examined whether COVID-19 resulted in significant national changes in community antibiotic prescribing patterns in Canada [4,5], as has been reported in other regions [6,7].
In Canada, access to antibiotics for use in humans is restricted to prescription by medical and allied health professionals, including physicians, dentists and pharmacists. Between 2015 and 2019, the national rate of antibiotic dispensing in the community had remained stable in Canada, decreasing by only 3% [8]. In recent years, approximately 90% of all antibiotics consumed by humans in Canada were dispensed through community retail pharmacies, with roughly two-thirds of these prescriptions originating from family doctors or general practitioners [8]. Recent literature has suggested that the COVID-19 pandemic has had a disruptive effect on prescribing practices [6,7]. The inappropriate use of antibiotics can have manifold detrimental effects. Inappropriate prescribing, commonly encountered in primary care [[9], [10], [11]], can support the population level selection of antibiotic resistance [12] and drive toxicity, including Clostridioides difficile infection [13]. Conversely, underprescribing of appropriate antibiotics can lead to adverse and potentially deadly infectious complications [14,15]. It is critical that we understand how antibiotic use has changed during the pandemic, such that we can better understand and anticipate potential downstream outcomes. In this study, we sought to describe the impact of the COVID-19 pandemic on Canadian community-level antibiotic prescribing using national antibiotic dispensing data between 2014 and 2020, stratified by age, sex and prescription origin.
Materials and methods
Data sources
The dataset for this ecological study comprised 72 months of antibiotic dispensing data from IQVIA's Canadian CompuScript (CS) database, covering all ten Canadian provinces from November 2014 to October 2020. Information on prescription drug strengths and dosages was obtained from Health Canada's Drug Product Database (DPD) using drug identification numbers (DIN). Population estimates were obtained from mid-year census population estimates from Statistics Canada.
IQVIA's Canadian CS dataset contains information on the estimated quantity of antibiotic prescriptions dispensed through community retail pharmacies using a proprietary geospatial projection method (incorporating pharmacy size and number of pharmacies in the area) based on a sample of more than 6500 of approximately 11 000 pharmacies in Canada. This information is used to assess dispensing patterns for specific drugs of interest. IQVIA databases using projection methods have been previously used in similar studies [[16], [17], [18], [19]]. The data were stratified by patient age, sex, prescription origin and approximate indication. Age groupings were defined as follows: children aged 0–18 years, adults aged 19–64 years and adults aged 65 years and older. Prescription origins (predominantly corresponding to the prescribing physician's specialty) were defined as follows: family physicians (FPs) had specialties of family physician or general practitioner; non-family physicians (non-FPs) were all other physician specialties; and non-physician prescribers were all other licensed prescribers (e.g. allied professionals, dentists, and nurse practitioners). Some physician specialties of interest were identified, specifically paediatricians, infectious disease physicians and surgeons (i.e. general surgeons, orthopaedic surgeons, plastic surgeons and cardiothoracic surgeons). Physician specialty was used as a possible surrogate to explore whether the indication for necessary prescribing changed (e.g. infectious diseases physician antibiotic prescribing) and to examine how volume of prescriptions was reduced due to effects of decreased healthcare access (e.g. prescribing by surgeons). Approximate antibiotic indications were defined based on typical clinical use, and were categorized as infections related to respiratory, urinary tract, skin and soft tissue, or other infections [20] (Table S1).
Antibiotics
This study included antibiotics intended for systemic use (i.e. J01 products, as defined by the 2020 WHO Collaborating Centre for Drug Statistics Methodology Anatomical Therapeutic Chemical (ATC) Classification Index [21], which does not include topical antibiotics, antifungal or antiviral medications), as well as oral vancomycin, oral fidaxomicin and oral colistin. Antibiotics not listed in the WHO ATC index were excluded.
Outcome
Rates of antibiotic dispensing were calculated as the number of prescriptions dispensed per 1000 inhabitants per month. The number of defined daily doses (DDDs) per 1000 inhabitants was also investigated and showed similar trends to prescription counts (Fig. S1). Due to an interest in analysing antibiotic consumption in children, we pursued all primary analyses using prescription counts to allow for comparability, as DDDs cannot be reliably used for paediatric populations [22].
Analysis
Descriptive statistics were used to compare the rates of antibiotic prescription counts each month between January and October 2020 to the corresponding month in 2019. An interrupted time series analysis was used to determine whether the overall monthly trend in antibiotic dispensing was significantly different during the Canadian COVID-19 period compared with the previous year. Although there was no harmonized start date to the implementation of public health measures in Canada, March 2020 was chosen as the first month of the COVID-19 pandemic period to correspond with many initial provincial public health interventions and the closure of the Canadian and United States land boarder to non-essential travel. Monthly antibiotic dispensing rates were stratified by age, sex, prescription origin and approximate indication. For each stratum, seasonality adjustment was performed using a twelfth order autoregressive model with backwards stepwise selection for autoregressive terms. As data were at the monthly level, a twelfth order model was chosen to account for annual (12 time points) correlation between the data, while allowing for the flexibility to explore finer correlation patterns (1–11 time points). A backwards stepwise process was used to determine which autoregressive parameters should be in the model for each strata. Each model incorporated terms for a step and slope change; due to the noticeable abrupt change in the data, we interpreted a significant step change beginning in March 2020 as the effect of the pandemic on antibiotic dispensing and the significance (p value) of this coefficient is reported. This interrupted time series with a seasonality adjustment was used to confirm that any variation observed in percent change was due to the COVID-19 pandemic and not natural seasonal change, especially due to the fact that the COVID-19 period overlapped with months of historically lower antibiotic use. All analyses were conducted in SAS version 9.4.
Ethics statement
This study was conducted using aggregated administrative health data. No data on individuals were available, therefore informed patient consent was not required.
Results
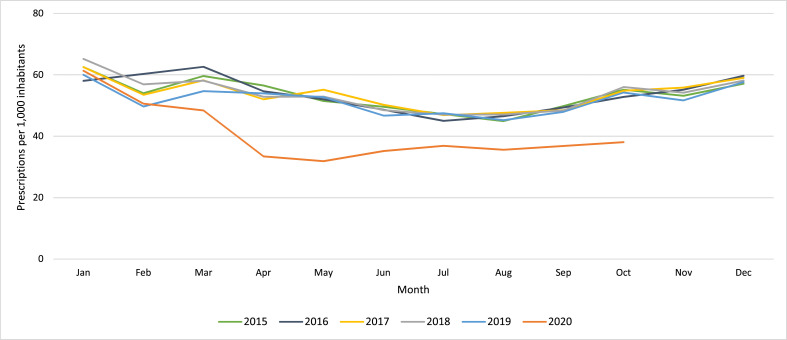
The national rate of antibiotic dispensing in Canada decreased by an average of 26.5% in the first 8 months of the COVID-19 pandemic. National dispensing decreased by up to 40% in May 2020 when compared with the corresponding month in 2019 (52.7 to 31.9 prescriptions per 1000 inhabitants) (Table 1 ). The disparity narrowed to a decrease of 21% in August 2020 (45.2 to 35.6 prescriptions per 1000 inhabitants), then broadened to a decrease of 30% in October 2020 (54.2 to 38.1 prescriptions per 1000 inhabitants) (Fig. 1 ). Adjusting for seasonality, the national rate of antibiotic dispensing during the COVID-19 period (March to October 2020) was significantly different compared with the pre-COVID-19 period (November 2014 to February 2020) (50.4 to 37.0 average prescriptions per 1000 inhabitants, p = 0.002). The observed trends and percent changes were similar when performing the analysis on DDD values (Fig. S1).
Table 1.
Rate of community-dispensed antibiotic prescriptions, 2019–2020, Canada
| Antibiotic prescriptions dispensed per 1000 inhabitants |
|||
|---|---|---|---|
| Month | 2019 | 2020 | Percent change (2019–2020) |
| January | 60.03 | 61.33 | 2.17 |
| February | 49.68 | 50.62 | 1.89 |
| March | 54.71 | 48.38 | –11.57 |
| April | 53.96 | 33.42 | –38.07 |
| May | 52.73 | 31.87 | –39.56 |
| June | 46.72 | 35.18 | –24.70 |
| July | 47.49 | 36.88 | –22.34 |
| August | 45.23 | 35.58 | –21.34 |
| September | 47.94 | 36.83 | –23.18 |
| October | 54.21 | 38.06 | –29.79 |
| Average (March to October) | 50.37 | 37.03 | –26.50 |
Fig. 1.
Rate of community-dispensed antibiotic prescriptions, 2015 to 2020, Canada.
Compared with the corresponding month in 2019, the rate of antibiotic dispensing was lower for all age and sex strata in the first 8 months of the COVID-19 pandemic. The largest decreases were observed during April and May 2020 and the smallest full-month decreases were observed during the summer months of 2020 (Fig. 2 ). In children aged 0–18 years, dispensing decreased by a maximum of 72% in males (43.7 to 12.2 prescriptions per 1000 inhabitants) and by 68% in females (46.8 to 14.9 prescriptions per 1000 inhabitants) in April 2020. In adults aged 19–64 years, dispensing decreased by a maximum of 35% in both males (36.1 to 23.4 prescriptions per 1000 inhabitants) and females (60.0 to 39.0 prescriptions per 1000 inhabitants) in May 2020. In seniors aged 65 years or more, dispensing decreased by 35% in males (74.9 to 48.8 prescriptions per 1000 inhabitants) and by 33% in females (91.7 to 61.3 prescriptions per 1000 inhabitants) in May 2020. Adjusting for seasonality, the national rate of antibiotic dispensing during the COVID-19 period was significantly different (p < 0.01) from the pre-COVID-19 period for each age and sex strata.
Fig. 2.
Percent change in community-dispensed antibiotic prescriptions by age and sex, 2019 and 2020, Canada.
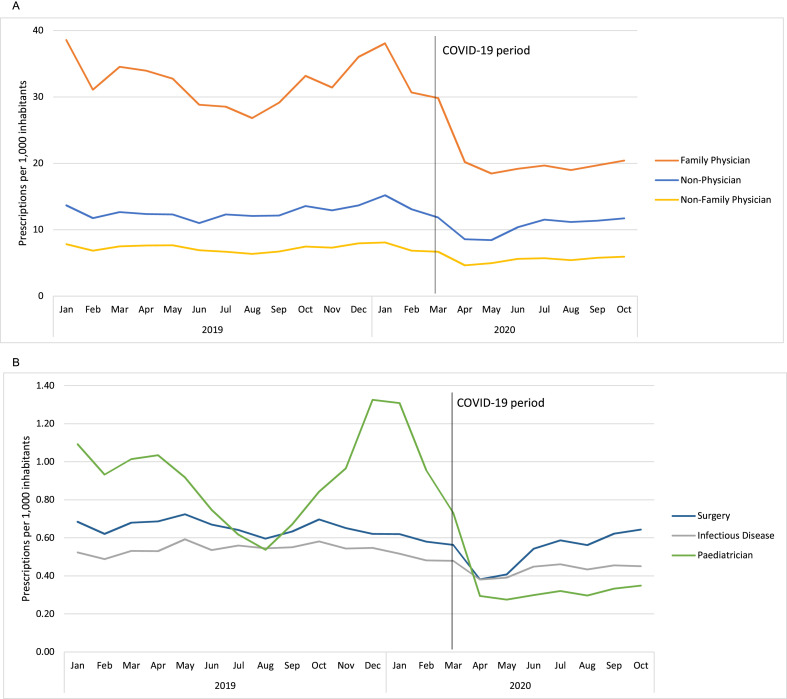
The rates of antibiotic prescriptions originating from all prescriber groups (i.e. FPs, non-FPs and non-physicians) during the COVID-19 period were significantly different from the rates pre-pandemic after adjusting for seasonality (FP 31.0 to 20.8 average prescriptions per 1000 inhabitants, p 0.020; non-FP 7.1 to 5.6 average prescriptions per 1000 inhabitants, p < 0.001; non-physicians 12.3 to 10.6 average prescriptions per 1000 inhabitants, p < 0.001) (Fig. 3 ). While the greatest number of prescriptions originated from FPs before and during the pandemic (accounting for approximately 62% of prescriptions in 2019 and 56% of prescriptions during the first 8 months of the pandemic), the rate of prescriptions originating from FPs decreased by a maximum of 44% in May 2020 (32.8 to 18.5 prescriptions per 1000 inhabitants), compared with a maximum decrease of 39% for non-FPs in April 2020 (7.6 to 4.6 prescriptions per 1000 inhabitants) and by 32% for non-physicians in May 2020 (12.3 to 8.4 prescriptions per 1000 inhabitants) (Fig. 3A). While the rate of antibiotic dispensing nearly returned to pre-COVID-19 rates for non-FPs and non-physicians during the summer of 2020, rates remained well below baseline for FPs until the end of the study.
Fig. 3.
Rates of monthly community-dispensed antibiotic prescriptions by prescription origin (A) family physicians vs. other; (B) infectious disease, paediatrician, and surgical specialists, 2019 and 2020, Canada.
A significant decrease was also observed across select physician specialties, including surgeons (p < 0.001), infectious disease physicians (p < 0.001) and paediatricians (p = 0.013) (Fig. 3B). The rate of prescriptions originating from surgeons decreased by a maximum of 44% in April 2020, the rate of prescriptions originating from infectious disease physicians decreased by a maximum of 34% in May 2020, and the rate of prescriptions originating from paediatricians decreased by a maximum of 72% in April 2020.
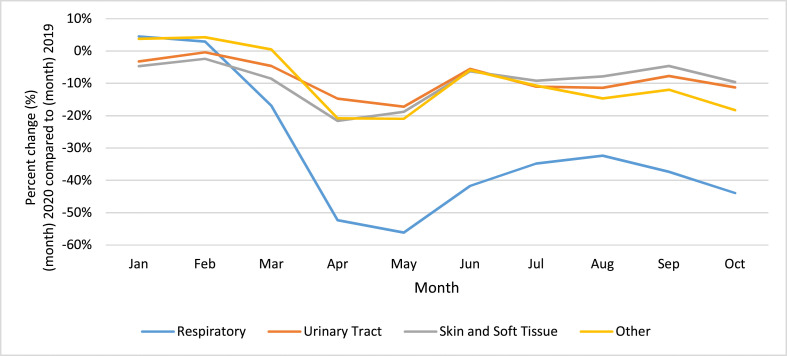
When grouping antibiotics by approximate indication, antibiotics typically used for respiratory infections showed the greatest decrease in prescribing in the early months of the COVID-19 period (a decrease of 56% in May 2020; 29.2 to 12.8 prescriptions per 1000 inhabitants), compared with the same months in 2019 (Fig. 4 ). Prescriptions for antibiotics associated with urinary tract, skin and soft tissue and other infections experienced more modest decreases of 17% (9.4 to 7.8 prescriptions per 1000), 19% (6.4 to 5.2 prescriptions per 1000) and 21% (7.1 to 5.6 prescriptions per 1000), respectively in May 2020. By October 2020, prescribing rates for antibiotics typically used for respiratory infections did not recover (a decrease of 44% compared with October 2019); however, prescribing rates for antibiotics typically used for urinary tract infections and skin and soft tissue infections decreased by only 11% and 10%, respectively.
Fig. 4.
Percent change in community-dispensed antibiotic prescriptions by approximate indication, 2019 and 2020, Canada.
Discussion
Between March and October 2020, the COVID-19 pandemic resulted in an average 26.5% national reduction in the total number of antibiotic prescriptions filled by community retail pharmacies compared with 2019. By age, the largest decrease in antibiotic dispensing was observed in children (up to a maximum of 70% in April 2020) and the smallest decrease was observed in seniors (up to a maximum of 34% in May 2020). By approximate indication, the largest decrease was observed in antibiotics typically used for respiratory infections.
Similar findings have been reported in the United States [6] and the UK [7]. This trend aligns with the national decrease in the number of physician visits throughout Canada [1,2], suggesting that reduced access to prescribers may have played a role in reducing community antibiotic dispensing. Other factors may include the collateral benefit of implementing public health measures that reduced the rates of all communicable diseases [23], and the potential reluctance for individuals to seek medical attention without severe symptoms, regardless of the availability of care. During the COVID-19 pandemic, influenza indicators have been exceptionally low and there has been no evidence of community transmission of influenza in Canada [24]. This remarkable reduction in seasonal influenza, despite increased testing [24], supports the lower rates of non-COVID-19 viral respiratory infections. The reduction in antibiotic prescribing may be the consequence of the reduction in the overall syndromic presentations of respiratory infections where antibiotics may be prescribed, including those inappropriate prescriptions for viral infections. This is supported by this study, as antibiotics approximately indicated for respiratory illnesses experienced the greatest prescribing decrease. While COVID-19 has had a disproportionate impact on seniors (notably, those in congregate living [25]), the rate of antibiotic dispensing in those aged 65 years and older appears to have been the least affected by the pandemic. It is possible that a greater proportion of non-communicable infections (e.g. urinary tract infections, cellulitis) attenuated the decrease in seniors during the pandemic, given that non-communicable infections would be expected to continue unabated. When stratifying by sex, the rate of antibiotic prescriptions was highest in females before and during the pandemic.
The significant decrease in antibiotic dispensing during the Canadian COVID-19 period may have long-term impacts on the development of antibiotic resistance. While overall reduced dispensing may slow the progression of antibiotic resistance the intensity of dispensing may have increased in specific populations. Additionally, the shift to virtual care may have resulted in increased diagnostic uncertainty, compared with diagnoses made during physical examination. These scenarios may increase progression to antibiotic resistance [26].
We were unable to examine the reasons for the reduction in dispensing. Although the CS database is nationally representative, it does not include information from the three Canadian territories, nor from inpatient populations. The database is administrative in nature and therefore is not maintained for research purposes. The CS database does not link antibiotic prescriptions to diagnoses, limiting assessment or interpretation of prescription appropriateness. Indications were approximated based on typical clinical usage. Information on morbidity and mortality was not available, limiting analysis or interpretation pertaining to the potential underuse of antibiotics. We were unable to assess if the observed reduction in antibiotic dispensing during the COVID-19 pandemic in Canada led to increased infectious complications. We were also unable to account for antibiotic recommendations that were not received by retail pharmacies. While effort has been made to adjust for seasonality, the COVID-19 pandemic has introduced novel simultaneous factors that are difficult to identify, define and fully account for.
There has been a significant decrease in the rate of community antibiotic use during the COVID-19 pandemic in Canada. In this natural experiment, the rate of antibiotic dispensing decreased by up to 40% in the first 8 months of the COVID-19 pandemic (March to October 2020) when compared with the same time period in 2019. In contrast, despite national efforts to increase awareness and reduce inappropriate antibiotic prescribing, antibiotic dispensing only decreased by 3% between 2015 and 2019. Further study is needed to fully understand the implications of the observed reduction. The many long-term impacts of COVID-19 on the health of the population remain unknown; however, the possibility of a sustained reduction in unnecessary antibiotic use may be a positive consequence of the COVID-19 pandemic.
Transparency declaration
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Competing interests: B.D.K., J.S., G.S., D.R.M., K.L.S., N.D., D.G.T. and J.B. have no competing interests to declare. B.D.K., J.S., G.S., D.R.M., K.L.S., N.D., D.G.T. and J.B. have no conflicts of interest to declare. All authors have submitted a COI disclosure form. B.D.K. affirms that this work is honest, accurate and transparent. No details have been omitted.
Author contributions
B.D.K., J.S. and G.S. conceived and designed the study. B.D.K. and G.S. performed the data preparation and analysis. B.D.K. wrote the first draft of the manuscript with J.S. and G.S. D.M., K.L.S., N.D., D.G.T. and J.B. assisted with data interpretation and reviewed the manuscript. All authors reviewed and approved the final version of the manuscript. B.D.K. is guarantor of the paper.
Access to data
The statements, findings, conclusions, views and opinions contained and expressed in this report are based in part on data obtained under license from IQVIA Solutions Canada Inc. concerning the following information service(s): CompuScript, data period November 2014 to October 2020. All Rights Reserved.
Acknowledgements
The statements, findings, conclusions, views and opinions expressed herein are not necessarily those of IQVIA Solutions Canada Inc. or any of its affiliated or subsidiary entities.
The views expressed in the submitted article are those of the authors and not an official position of the Public Health Agency of Canada.
Editor: J. Rodriguez-Baño
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cmi.2021.10.013.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Glazier R.H., Green M.E., Wu F.C., Frymire E., Kopp A., Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193:E200–E210. doi: 10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Institute of Health Information . 2020. How COVID-19 affected physician services.https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/how-covid-19-affected-physician-services Available from: [Google Scholar]
- 3.Glass R.J., Glass L.M., Beyeler W.E., Min H.J. Targeted social distancing design for pandemic influenza. Emerg Infect Dis. 2006;12:1671–1681. doi: 10.3201/eid1211.060255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson K.M., Dumkow L.E., Burns K.W., Yee M.A., Egwuatu N.E. Comparison of diagnosis and prescribing practices between virtual visits and office visits for adults diagnosed with sinusitis within a primary care network. Open Forum Infect Dis. 2019;6:ofz393. doi: 10.1093/ofid/ofz393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ray K.N., Shi Z., Gidengil C.A., Poon S.J., Uscher-Pines L., Mehrotra A. Antibiotic prescribing during pediatric direct-to-consumer telemedicine Visits. Pediatrics. 2019;143 doi: 10.1542/peds.2018-2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.King L.M., Lovegrove M.C., Shehab N., Tsay S., Budnitz D.S., Geller A.I., et al. Trends in U.S. outpatient antibiotic prescriptions during the COVID-19 pandemic. Clin Infect Dis. 2021;73:e652–e660. doi: 10.1093/cid/ciaa1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu N., Aylin P., Rawson T., Gilchrist M., Majeed A., Holmes A. Investigating the impact of COVID-19 on primary care antibiotic prescribing in North West London across two epidemic waves. Clin Microbiol Infect. 2021;27:762–768. doi: 10.1016/j.cmi.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Public Health Agency of Canada . 2020. Canadian antimicrobial resistance surveillance system report – update 2020. Available from: https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2020-report.html. [Google Scholar]
- 9.Schwartz K.L., Langford B.J., Daneman N., Chen B., Brown K.A., McIsaac W., et al. Unnecessary antibiotic prescribing in a Canadian primary care setting: a descriptive analysis using routinely collected electronic medical record data. CMAJ Open. 2020;8:E360–E369. doi: 10.9778/cmajo.20190175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smieszek T., Pouwels K.B., Dolk F.C.K., Smith D.R.M., Hopkins S., Sharland M., et al. Potential for reducing inappropriate antibiotic prescribing in English primary care. J Antimicrob Chemother. 2018;73 doi: 10.1093/jac/dkx500. ii36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fleming-Dutra K.E., Hersh A.L., Shapiro D.J., Bartoces M., Enns E.A., File T.M., et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315:1864–1873. doi: 10.1001/jama.2016.4151. [DOI] [PubMed] [Google Scholar]
- 12.MacFadden D.R., Fisman D.N., Hanage W.P., Lipsitch M. The relative impact of community and hospital antibiotic use on the selection of extended-spectrum beta-lactamase-producing Escherichia coli. Clin Infect Dis. 2019;69:182–188. doi: 10.1093/cid/ciy978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown K.A., Khanafer N., Daneman N., Fisman D.N. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother. 2013;57:2326–2332. doi: 10.1128/AAC.02176-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wagenlehner F.M.E., Pilatz A., Naber K.G., Weidner W. Therapeutic challenges of urosepsis. Eur J Clin Invest. 2008;38:45–49. doi: 10.1111/j.1365-2362.2008.02008.x. [DOI] [PubMed] [Google Scholar]
- 15.Balinskaite V., Bou-Antoun S., Johnson A.P., Holmes A., Aylin P. An assessment of potential unintended consequences following a national antimicrobial stewardship program in England: an interrupted time series analysis. Clin Infect Dis. 2019;69:233–242. doi: 10.1093/cid/ciy904. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz K.L., Chen C., Langford B.J., Brown K.A., Daneman N., Johnstone J., et al. Validating a popular outpatient antibiotic database to reliably identify high prescribing physicians for patients 65 years of age and older. PLoS One. 2019;14 doi: 10.1371/journal.pone.0223097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King L.M., Bartoces M., Fleming-Dutra K.E., Roberts R.M., Hicks L.A. Changes in US outpatient antibiotic prescriptions from 2011–2016. Clin Infect Dis. 2020;70:370–377. doi: 10.1093/cid/ciz225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Staub M.B., Ouedraogo Y., Evans C.D., Katz S.E., Talley P.P., Kainer M.A., et al. Analysis of a high-prescribing state’s 2016 outpatient antibiotic prescriptions: implications for outpatient antimicrobial stewardship interventions. Infect Control Hosp Epidemiol. 2020;41:135–142. doi: 10.1017/ice.2019.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischer B., Jones W., Vojtila L., Kurdyak P. Patterns, changes, and trends in prescription opioid dispensing in Canada, 2005–2016. Pain Physician. 2018;21:219–228. [PubMed] [Google Scholar]
- 20.Schwartz K.L., Achonu C., Brown K.A., Langford B., Daneman N., Johnstone J., et al. Regional variability in outpatient antibiotic use in Ontario, Canada: a retrospective cross-sectional study. CMAJ Open. 2018;6:E445–E452. doi: 10.9778/cmajo.20180017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO Collaborating Centre for Drug Statistics Methodology . 2020. ATC/DDD index 2020.https://www.whocc.no/atc_ddd_index/ Available from: [Google Scholar]
- 22.World Health Organization More about DDDs. 2021. https://www.who.int/medicines/regulation/medicines-safety/toolkit_ddd_more/en/ Available from:
- 23.Brueggemann A.B., van Rensburg Mjj, Shaw D., McCarthy N.D., Jolley K.A., Maiden M.C., et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3:e360–e370. doi: 10.1016/S2589-7500(21)00077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Public Health Agency of Canada . 2021. FluWatch report: March 7, 2021 to March 20, 2021 (weeks 10–11)https://www.canada.ca/en/public-health/services/publications/diseases-conditions/fluwatch/2020-2021/weeks-10-11-march-7-march-20-2021.html Available from: [Google Scholar]
- 25.Liu M., Maxwell C.J., Armstrong P., Schwandt M., Moser A., McGregor M.J., et al. COVID-19 in long-term care homes in Ontario and British Columbia. CMAJ. 2020;192:E1540–E1546. doi: 10.1503/cmaj.201860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olesen S.W., Barnett M.L., MacFadden D.R., Brownstein J.S., Hernández-Díaz S., Lipsitch M., et al. The distribution of antibiotic use and its association with antibiotic resistance. Elife. 2018;7 doi: 10.7554/eLife.39435. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.