Summary
Background
COVID19 vaccination coverage in Israel varies among population groups. Comparing crude coverage between groups is misleading because of different age structures and socio-economic differences. To describe inequalities in COVID19 vaccine initiation in Israel we analysed the interaction of age and population groups in terms of dose 1 vaccine coverage
Methods
We calculated cumulative age-specific first COVID19 vaccine coverage by population group (Ultra-Orthodox Jewish, Arab, General Jewish). We calculated the relative differences in vaccine coverage between population groups within each age group, and between age groups within each population, using ANOVA and binomial regression after adjusting for socio-economic status
Findings
8,507,723 individuals in 268 cities were included. Compared with the general Jewish population, coverage was lowest in the Ultra-Orthodox population in all age groups (range -12% among 60+ to -52.8% among 10-19 years olds, p<0.001). In all groups, the proportion of vaccinated individuals in younger age groups relative to those aged 60+ decreased with decreasing age and were smallest in the Ultra-Orthodox groups. For example, within the general Jewish population, people aged 20-29 were 14% less likely to be vaccinated than those aged 60+ while within the Ultra-Orthodox population it was 34.5%
Interpretation
In all age groups, the Ultra-Orthodox population had the lowest vaccine coverage. Differences persisted after adjusting for socio-economic status. The younger the age group, the more Ultra-Orthodox Jews were diverging from age peers in terms of initiating COVID19 vaccination, suggesting a generational effect. Tailored approaches are urgently required to encourage vaccination among under-immunized groups in Israel
Funding
No specific funding was received
Research in context.
Evidence before this study
High national-level coverage of COVID-19 vaccine in Israel masks inequalities between population and age groups. Comparison of crude vaccine coverage between groups, notably Ultra-Orthodox, Arab and the general population, may be misleading because of differing age structure, socio economic status and background incidence.
Added value of this study
This study not only shows differences in age-specific COVID19 vaccine coverage between groups comprising Israeli society, but demonstrates a generational effect by which differences in COVID19 vaccine initiation between population groups increase as age decreases. We identify young, ultraorthodox citizens as the most undervaccinated group in Israel. This is a particular concern as this group includes parents of most of the children in Israel, who are currently or slated to become eligible for COVID19 vaccination.
Implications of all the available evidence
There is an urgent need for tailored COVID19 vaccination campaigns targeting Ultra-Orthodox residents under the age of 40 as well for qualitative studies to understand barriers to COVID19 vaccination in the segment of the population.
Alt-text: Unlabelled box
Introduction
By July 2021, The COVID-19 pandemic, which was detected in China in December 2019 and rapidly spread globally, had infected over 187 million and killed at least 4 million individuals,1 disrupting trade, travel, education, and the economy on an unprecedented scale. Despite a range of measures such as social distancing, masks, mass testing, surveillance and repeated lockdowns, implemented to varying degrees of stringency by almost every country in the world, the pandemic continued to spread. The emergence of safe and effective vaccines in December 2020,2, 3, 4 with more at various stages of development5 offer new hope for controlling the pandemic.
Israel has not been spared by the pandemic and as of July 11 2021 reported 846,327 cases and 6,438 deaths.6 By this date Israel had vaccinated 61·6% of the population with one dose of the BNT16b2 mRNA vaccine and 55·8% with the second dose, including over 92% of individuals over the age of 60,6 the highest proportion in the world.6 The benefits of such high vaccine coverage were seen, with a sharp decrease in transmission and incidence since March 20206 despite a gradual easing of control measures. Reasons for this success include Israel's small size, a centralized national system of government, experience in managing large-scale national emergencies, the organizational, IT and logistical capacities of Israel's community-based health care providers, and the mobilization of special government funding for vaccine purchase and distribution.7 In early June 2020, the importation in Israel of the delta variant, against which the effectiveness of the BNT16b2 mRNA vaccine is lower,8 led to an increase in incidence, although effectiveness against severe illness and death remains high and the incidence of severe cases and case fatality rates remains low.9
Vaccinations against COVID in Israel has taken place in community health centres (HMOs), hospitals, ad-hoc vaccination centres in repurposed facilities such as stadiums and sport centres, and mobile units reaching remote and small communities. Community health clinics are located in almost every municipality in Israel and all citizens and residents, by law, have to be registered with one. Those over the age of 60 first became eligible on 20/12/20,10 followed by those over 55 on 12/01/21,11 those over 35 on 28/01/2112 over 16 on 03/02/202113 and finally teenagers over 12 on 06/06/21.14 Until early March 2020, individuals who had evidence of COVID-19 infection and had recovered were not eligible for vaccination. In early March 2020, they became eligible for a single dose. In addition to age eligibility, emergency, healthcare, defense forces and education workers and in late January also high school pupils have been prioritized for vaccination.10,15 Finally, resourceful individuals have at times succeeded in getting vaccinated outside of eligibility criteria, for example by waiting for leftover doses outside of clinics. By 04/01/21, for example, more than 30% of vaccinated individuals were under the age of 6016 despite only a minority (such as healthcare workers and other emergency response personnel) being eligible.
The three largest population groups in Israel are the non-ultra-orthodox Jewish population (thereafter called “general Jewish”), and the Ultra-Orthodox Jewish and Arab (mainly Muslim, including Bedouin, and Christian) populations. These groups comprise the Israeli population alongside smaller groups such as the Druze and Circassians. Each community tends to live in separate localities. In Israel, the Central Bureau of Statistics (CBS) assigns each municipality to one of 10 socio economic clusters from 1 (most deprived) to 10 (least deprived). The allocation of each municipality and methodology is available on their website.17 Compared with the general Jewish population, Ultra-Orthodox and Arab municipalities are socio-economically deprived.18 The Arab population lives mostly in towns and villages, most of them located in the northern Galilee area, while the Jewish population is more urban, and the Ultra-Orthodox population lives almost entirely in urban municipalities in the Center area. In addition these two populations are much younger than the general Jewish population: in 2015 29% of the general Jewish population was under 18, compared with 56% of Ultra-Orthodox Jews and 43% of Arabs19 (Table 1).
Table 1.
Age distribution by population group, Israel, 2015.
| Proportion of total population (%) | Proportion of the group aged under 18 (%) | Proportion of the group aged over 65 (%) | |
|---|---|---|---|
| General Jewish | 67 | 29 | 16 |
| Ultra-Orthodox Jewish | 12 | 56 | 3 |
| Arab* | 21 | 43 | 4 |
includes the Druze population
Source: Israel Central Bureau of Statistics
Despite overall high vaccine coverage in Israel, there are wide variations by geography, and therefore population group. By July 11 2021, vaccination coverage by municipality for the first dose ranged 2·5-99%.6 These disparities exist despite local availability of the vaccine in the entire country and free vaccination for all. Comparing crude coverage between localities and population groups may however be misleading because of the very different age structure underlying each group, because COVID19 incidence varied by locality and because of socio economic variation between these groups, a factor often associated with differences in vaccine coverage.20,21 In order to describe inequalities in COVID19 vaccine initiation we determined differences in age-specific dose 1 vaccine coverage between the main population groups in Israel after taking socio economic differences into consideration, and characterised the influence of age on vaccine coverage within each of these groups.
Methods
We generated a dataset of dose-1 vaccine coverage by age group and by municipality, by linking two publicly available datasets: first, population size by municipality in 5 year age-bands;22 and second, the daily cumulative number of first doses of COVID19 given in each municipality, by 10 year age-bands.23 The datasets were linked using municipality codes unique to each locality. We thus categorized the population in 6 age groups: 10-19, 20-29, 30-39, 40-49, 50-59 and 60 and over. Although 10-12 year olds are not yet eligible for vaccination, we included them in the denominator since denominator data is available only for five years age bands. This leads to underestimating vaccine coverage but does not affect between and within group comparisons. The most recent available population census with age distribution was from 2018,24 so in order to adjust for population growth, we extrapolated the population in each age group by population growth factor for each municipality 2018-2021
For data privacy reasons, vaccination data available from the ministry of Health does not include municipalities under 2000 residents, resulting in a total of 775,231 not included in our analysis. None of these municipalities were Ultra-Orthodox; 101,875 (13.1%) people were living in Arab municipalities, and the rest (86.9%) in Jewish, non Ultra-Orthodox municipalities. The remaining 268 municipalities all had complete data for all age groups.
In the vaccination data, if a cell (date, age group and municipality) contained less than 15 vaccinations it was written “<15” for privacy reasons. In order to aggregate the data in these cells we replaced these values with 10.
Sectors were categorized using the municipality form code in the population size dataset to determine settlements with an Arab (including Druze) majority. There is no official category identifying Ultra-orthodox municipalities, so we classified as Ultra-Orthodox municipalities where Ultra-orthodox residents comprised 60% or more of the population. Municipalities with an Ultra-Orthodox population between 40 and 59% were considered mixed Jewish, and those with 40% or less as General Jewish.1
We calculated overall unadjusted and age-adjusted vaccine coverage for each group, using direct standardization and the Israeli population as a standard. We performed 2 Kruskal Wallis tests: one for sector with four levels (Arab, General Jewish, Ultra-Orthodox Jewish and Mixed Jewish) and one for age with six levels (10-19, 20-29, 30-39, 40-49, 50-59, 60+). The analysis was weighted so that each age group in each municipality was adjusted to represent its relative proportion within each population group or age group.
In order to quantify the relative differences in vaccine coverage between population groups within each age group, and between age groups within each population, we conducted a series of binomial regressions with a log link. In our models the municipality was the unit of analysis, the number of first doses administered, the outcome, the size of the population as the offset and population groups as a categorical explanatory variable We used the CBS Socio economic clusters as a variable in our model to adjust for Socio-economic status.
Analyses were conducted using R and Stata16 (Stata corp, Texas). The analysis made exclusive use of publicly available data and no ethical approval was required.
Role of the funding source: No specific funding was sought or obtained for this study
Results
A total of 8,507,723 individuals (after extrapolation by 2018-2021 growth factor) in 268 cities, towns and villages with valid information were included. Of these 97 municipalities were Arab (including Druze) representing 16.6% of the sample population, 11 were Ultra-Orthodox (7·1% of the sample population), 154 General Jewish (63·2%) and 6 mixed (13·1%), including Jerusalem, Israel's largest city. Overall coverage in General Jewish, Ultra-Orthodox, Mixed and Arab municipalities was 80.1%, 46.7%, 62.7% and 64.4% respectively. Age-adjusted coverage in these same groups was 78.4%, 56%, 65.9% and 68.5% respectively.
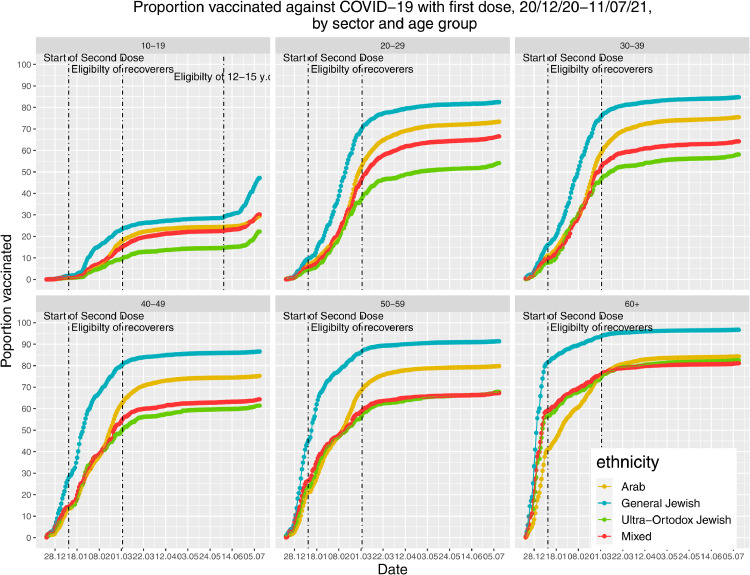
Vaccine coverage decreased with age (Table 2, Figure 1) and the difference between age groups was significant ((H (5) = 699.69, p <0·001, η2p = 0.23). Across all age groups, coverage was lower in other population groups compared with the general Jewish population (Figure 1, Table 2) and the differences between sectors was statistically significant((H(3) = 222.54, p< 0·001, η2 = 0·45)).
Table 2.
Differences in COVID 19 vaccination by population group among each age group, Israel, April 2021.
| Age group | Population group | Number eligible (n) | Vaccine coverage (%) | Unadjusted RR* (within age groups) | 95%CI | RR adjusted for socio economic status* | 95%CI |
|---|---|---|---|---|---|---|---|
| 60+ | General Jewish | 1113200 | 93·9 | baseline | |||
| Ultra-Orthodox Jewish | 32451 | 82·7 | 0·880 | 0·876-0·885 | 0·917 | 0·912-0·922 | |
| Mixed | 130244 | 86.9 | 0·926 | 0·924-0·927 | 0·955 | 0·953-0·958 | |
| Arab | 107170 | 86·3 | 0·920 | 0·917-0·922 | 0·950 | 0·948-0·953 | |
| 50-59 | General Jewish | 561376 | 89·9 | baseline | |||
| Ultra-Orthodox Jewish | 23831 | 68·5 | 0·762 | 0·755-0·768 | 0·872 | 0·864-0·88 | |
| Mixed | 76360 | 76.8 | 0·854 | 0·851-0·857 | 0·947 | 0·943-0·951 | |
| Arab | 114842 | 80·9 | 0·900 | 0·897-0·903 | 1·002† | 0·998-1·006 | |
| 40-49 | General Jewish | 709265 | 85·0 | baseline | |||
| Ultra-Orthodox Jewish | 42039 | 60·1 | 0·707 | 0·702-0·713 | 0·740 | 0·734-0·746 | |
| Mixed | 94610 | 73.2 | 0·862 | 0·858-0·865 | 0·892 | 0·888-0·896 | |
| Arab | 153143 | 75·6 | 0·890 | 0·887-0·893 | 0·924 | 0·921-0·928 | |
| 30-39 | General Jewish | 756933 | 80·6 | baseline | |||
| Ultra-Orthodox Jewish | 65256 | 53·5 | 0·665 | 0·660-0·669 | 0·696 | 0·69-0·701 | |
| Mixed | 125303 | 68.9 | 0·855 | 0·852-0·858 | 0·885 | 0·881-0·889 | |
| Arab | 165208 | 75·3 | 0 ·934 | 0·932-0·937 | 0·972 | 0·968-0·976 | |
| 20-29 | General Jewish | 707576 | 80·8 | baseline | |||
| Ultra-Orthodox Jewish | 82097 | 54·2 | 0·670 | 0·666-0·675 | 0·83 | 0·824-0·836 | |
| Mixed | 173336 | 66.5 | 0·824 | 0·821-0·827 | 0·967 | 0·963-0·972 | |
| Arab | 237135 | 72·9 | 0·903 | 0 ·901-0·905 | 1·081 | 1·077-1·085 | |
| 10-19 | General Jewish | 767477 | 47·5 | baseline | baseline | ||
| Ultra-Orthodox Jewish | 133654 | 22·2 | 0·467 | 0·462-0·472 | 0·764 | 0·754-0·774 | |
| Mixed | 203627 | 30 | 0·635 | 0·631-0·635 | 0·920 | 0·912-0·928 | |
| Arab | 276088 | 28·9 | 0·607 | 0·604-0·611 | 0·917 | 0·909-0·925 |
All risk ratios are statistically significant, p<0.001 except when marked † where it is not significant
Figure 1.
Proportion vaccinated against COVID−19 with first dose, 20/12/20−11/07/21, by sector and age group.
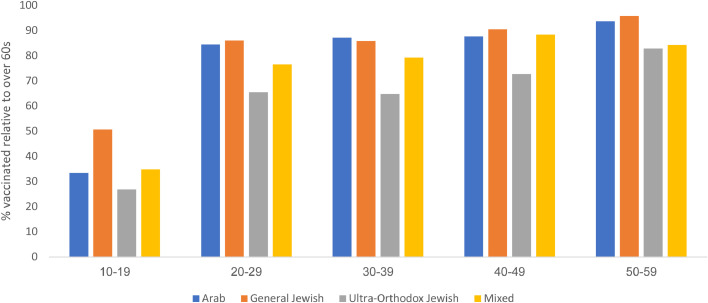
Compared with coverage in general Jewish municipalities, coverage was lower in all other municipalities for all age groups, but was lower in Ultra-Orthodox municipalities for all age groups (range -12%, 95%CI -12·4%;- 11·5% among 60+ to -53·3% 95%CI -53·8%; -52·8% among 10-19 years old, p<0·001, Table 2). After adjusting for socio economic status, differences in coverage reduced, and in some cases disappeared for all groups and especially for the Arab population compared with general Jewish municipalities (Table 2). However differences remained important for the Ultra-Orthodox, in particular among younger age groups. After adjusting for SES, groups under the age of 50 in Ultra-Orthodox municipalities are the only ones vaccinated at less than 85% of the proportion of the same age groups in General Jewish municipalities (Table 2).Within each population group, the proportions of individuals in younger age groups vaccinated relative to older age groups differed. They decreased with decreasing age in all groups and were smaller in the Ultra-Orthodox groups compared with the General Jewish, Mixed and Arab municipalities (Figure 2, Table 3). For example, within the general Jewish population, people aged 20-29 were 14% less likely to be vaccinated than those over the age of 60, increasing to 34·5% in the Ultra-Orthodox population (Figure 2, Table 3). The Ultra-orthodox population was the least vaccinated in all age groups relatively to those aged 60 and over (Figure 2)
Figure 2.
Proportion vaccinated against COVID19 relative to those over the age of 60, by age group, Israel, July 2021 all differences between groups are statistically significant, p<0.001.
Table 3.
Differences in COVID 19 vaccination by age group among each population group, Israel, April 2021. All risk ratios are statistically significant, p<0.001.
| Age group | Population group | Number eligible (n) | Vaccine coverage (%) | RR (within ethnic groups) | 95%CI |
|---|---|---|---|---|---|
| General Jewish | 60+ | 1113200 | 93·9 | baseline | |
| 50-59 | 561376 | 89·9 | 0·958 | 0·957-0·959 | |
| 40-49 | 709265 | 85·0 | 0·905 | 0·904-0·906 | |
| 30-39 | 756933 | 80·6 | 0·858 | 0·857-0·859 | |
| 20-29 | 707576 | 80·8 | 0·860 | 0·859-0·862 | |
| 10-19 | 767477 | 47·5 | 0·506 | 0·505-0·508 | |
| Ultra-Orthodox Jewish | 60+ | 32451 | 82·7 | Baseline | |
| 50-59 | 23831 | 68·5 | 0·828 | 0·82-0·837 | |
| 40-49 | 42039 | 60·1 | 0·727 | 0·72-0·734 | |
| 30-39 | 65256 | 53·5 | 0·648 | 0·642-0·653 | |
| 20-29 | 82097 | 54·2 | 0·655 | 0·65-0·66 | |
| 10-19 | 133654 | 22·2 | 0·269 | 0·266-0·272 | |
| Mixed | 60+ | 130244 | 86.9 | baseline | |
| 50-59 | 76360 | 76·8 | 0·884 | 0·88-0·888 | |
| 40-49 | 94610 | 73·2 | 0·843 | 0·839-0·847 | |
| 30-39 | 125303 | 68·9 | 0·793 | 0·79-0·796 | |
| 20-29 | 173336 | 66·5 | 0·766 | 0·763-0·769 | |
| 10-19 | 203627 | 30 | 0·348 | 0·345-0·35 | |
| Arab | 60+ | 107170 | 86·3 | Baseline | |
| 50-59 | 114842 | 80·9 | 0·937 | 0·934-0·941 | |
| 40-49 | 153143 | 75·6 | 0·876 | 0·873-0·879 | |
| 30-39 | 165208 | 75·3 | 0·872 | 0·869-0·875 | |
| 20-29 | 237135 | 72·9 | 0·845 | 0·842-0·848 | |
| 10-19 | 276088 | 28·9 | 0·334 | 0·332-0·337 |
Discussion
Coverage for the COVID19 vaccine in Israel, varies widely in different groups comprising Israeli society. While adjusting for socio-economic differences accounted for most, and in some cases all of the difference in coverage between the Arab and general Jewish population, differences between the Ultra-Orthodox and General Jewish municipalities persisted after adjustment, suggesting different drivers for underimmunization in these population groups. In all age groups, the Ultra-Orthodox population had the lowest vaccine coverage. Despite government recommendation to vaccinate teenagers vaccine coverage was low among individuals aged 10-19, and younger individuals in the Ultra-Orthodox population were the least likely to be vaccinated, with the size of the relative differences between this group and others increasing with decreasing age, and the relative difference in vaccine coverage between younger and older age groups being larger in the Ultra -Orthodox population than in the general Jewish or Arab population. Expressed differently, the younger the age group, the more Ultra-Orthodox Jews are diverging from their age peers in terms of initiating COVID19 vaccination. These inequalities were exacerbated after vaccination was opened to teenagers from the age of 12 in June 2021. These findings suggest generational differences in terms of vaccination behaviour in this group. This study does not provide an explanation for this observation, but identifying age and population group specific barriers to vaccination, and providing tailored strategies to increase vaccination in this group is an urgent priority considering the uncertainty over the pandemic. Low vaccination in this group could initially be explained by high incidence of COVID19 among young Ultra-Orthodox Jews because infected individuals were not eligible. However they became eligible in March 2021. Incidence was also high among young individuals in the Arab population, yet coverage in this group increased and became much closer to similar age groups in the general Jewish population compared with the Ultra-Orthodox groups. Overall, delaying eligibility for those previously infected means that a high proportion of those unvaccinated were previously infected and have some degree of protection conferred by natural infection. Therefore, in the Israeli context, vaccine coverage underestimates true population immunity.
Tailored approaches to vaccination are widely recognized as an effective approach to successful vaccination programmes in minority groups.
Our study demonstrates how coverage figures can be misinterpreted if interpreted at face value because of the very different age structures and background incidence in the different populations included in this study. Socio economic differences also partly account for observed differences. While an adjusted, age-stratified analysis shows that among different ethno-religious groups differences in those over the age of 50 are relatively small, other groups, especially younger Ultra-Orthodox groups, remain under-vaccinated. This is a threat to achieving optimal protection against COVID19 through vaccination, which will require equitable coverage in all population groups, in particular in a small, densely populated country such as Israel. If the Ultra-Orthodox population under 40 remains under vaccinated, the risk of recurrent clusters of COVID19 in this population is high, in particular as international travel reopens and high volume of travel between Ultra-Orthodox communities in Israel and abroad resumes. This epidemiological picture has been described in the Ultra-Orthodox communities for other infectious diseases such as measles.25 As vaccine eligibility extends further to younger children, as is planned in Israel, the impact of an under vaccinated Ultra-Orthodox population may be compounded by the fact that the proportion of children under the age of 18 is higher in this group than any other population group in Israel, and most parents will be under the age of 40, the least vaccinated group. Although our study does not measure parent's intention to vaccinate their children, evidence suggests that parent's intention to vaccinate their children against COVID is lower than their intention to vaccinate themselves.26 While it is important to identify and address immunity gaps in the most underserved groups, continued efforts to improve coverage is essential, in particular in younger individuals where coverage remains low in all population groups.
This study is to our knowledge the first to describe how age and belonging to a particular group interact to influence COVID19 vaccine coverage in Israel. Our study has used comprehensive datasets taken from official governmental databases, covering the majority of the population is Israel. Bias and representativeness are therefore unlikely to be issues.
Differences in COVID19 vaccination according to ethnicity has also been observed in other countries such as the UK27 and the USA.28 However, it is important to note that unlike most ethnic minorities in other countries, Arabs in Israel achieve higher vaccine coverage for routine vaccination than the Jewish majority.29
There are several limitations to this study. First, the most recent demographic data was from 2018, which leads to a slight underestimation of the denominator and over estimation of vaccine coverage. However the timeframe between 2017 and 2021 is too short to significantly impact on the relative distribution of the population by age or population group, and relative measures are therefore unlikely to be significantly affected. We applied a correction factor based on national growth to try and minimize the effect of an underestimated denominator. We also assumed that the population groups considered in the study (General Jewish, Ultra-Orthodox and Arab) are homogenous in their vaccination behaviour, which is unlikely to be true. More localized analyses, combined with qualitative research understanding barriers and enablers in specific communities, will enable to understand drivers of vaccination with more granularity.
Data were available at the municipality, rather than individual level. As with all ecological studies, there is a risk of ecological fallacy since it is not known within municipalities that are not entirely populated by one group or another whether vaccine coverage differs among groups. Since the vaccination roll out is national and everyone has the same level of access to resources, the risk for ecological fallacy is however low. The fact that cities classed as mixed fall somehow in between, suggesting a gradient in coverage according to the proportion of the population being Ultra-Orthodox, also provide reassurance
Another limitation was that the exact numbers of daily vaccination administered was suppressed from the dataset when it was less than 15 for fear of deductive disclosure. As a pragmatic measure, we assigned ten vaccines when less than 15 was indicated. Although not exact, the small numbers compared with the overall large sample size are unlikely to bias the findings.
Another limitation is that the proportion of Ultra-Orthodox population (7·1%) and Arab population (16·6%) is smaller in the study sample than in the population (12% and 21% respectively). This is mostly because significant proportions of these populations live in municipalities counted as General Jewish or mixed (30% of the ultra-Orthodox and 10% of the Arab population); Jerusalem, classed as mixed in our study, is home to over 24% of the Ultra-Orthodox population 19% of the Arab population.
Our analysis offers an in-depth characterization of how age, population groups and their interplay impact on vaccine coverage. As of July 11th, 2021 Israel is among the countries most vaccinated against COVID-19. Nevertheless the rate of coverage increase is slowing down as those eager to be vaccinated have now received the vaccine. The vaccination progamme now requires tailored approaches in order to convince those who are more indifferent or perhaps even skeptical about vaccination,26 to get vaccinated. Our study identifies a number of groups, in particular younger individuals in general but also specifically in the Ultra-orthodox population, as falling behind others in terms of vaccine coverage. Qualitative studies understanding the causes behind this divergence are urgently needed to inform tailored vaccination strategies.
Contributors
YG led the the data management and analysis and contributed to writing the original draft. ME designed the study and methodology, contributed to the data analysis and contributed to writing the original draft. EA advised on integrating socio-economic data to the analysis, contributed to the re-analysis of the data, and subsequent revision of the manuscript. All authors verified the data and approved the final manuscript
Data availability statement
All data used in this study are publicly available. Vaccination data by municipality and age are available from the Israel Ministry of Health COVID19 data repository: https://data.gov.il/dataset/covid-19
Data about population size in each municipality and socio economic status of each municipality can be found in the Israel Central Bureau for Statistics website: https://www.cbs.gov.il/EN/Pages/default.aspx
Declaration of Interests
None of the authors declare any conflict of interest.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) dashboard. Accessed July 11, 2021. https://covid19.who.int/
- 2.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baden L, El Sahly H, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramasamy MN, Minassian AM, Ewer KJ, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396(10267):1979–1993. doi: 10.1016/S0140-6736(20)32466-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Draft landscape and tracker of COVID-19 candidate vaccines. Accessed July 11, 2021. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 6.Israel Ministry of Health. COVID-19 dashboard. Accessed July 11, 2021. https://datadashboard.health.gov.il/COVID-19/general
- 7.Rosen B, Waitzberg R, Israeli A. Israel's rapid rollout of vaccinations for COVID-19. Isr J Health Policy Res. 2021;10(1) doi: 10.1186/s13584-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Israel Ministry of Health. Decline in vaccine effectiveness against infection and symptomatic illness. July 5 2021. https://www.gov.il/en/departments/news/05072021-03
- 9.Stowe J, Andres N, Gower C et al. Effectiveness of COVID-19 vaccines against hospital admission with the Delta (B.1.617.2) variant. Public Health England (Pre-print). Accessed July 11 2021.https://khub.net/web/phe-national/public-library/-/document_library/v2WsRK3ZlEig/view_file/479607329?_com_liferay_document_library_web_portlet_DLPortlet_INSTANCE_v2WsRK3ZlEig_redirect=https%3A%2F%2Fkhub.net%3A443%2Fweb%2Fphe-national%2Fpubli
- 10.Israel Ministry of Health. The First Ones to Have the COVID-19 Vaccine within the “Ten Katef” Vaccine Campaign. Accessed July 11, 2021. https://www.gov.il/en/departments/news/16122020-01
- 11.Israel Ministry of Health. Starting Tuesday (12.1.21), insured HMO members 55 years old or older will be vaccinated. Accessed July 11, 2021. https://www.gov.il/en/departments/news/11012021-01
- 12.Israel Ministry of Health. Back to life – The vaccination campaign expands. Accessed July 11, 2021. https://www.gov.il/en/departments/news/27012021-04
- 13.Ministry of Health. Operation Back to Life Expands | Ministry of Health. Accessed July 11, 2021. https://www.gov.il/en/departments/news/03022021-01
- 14.Israel Ministry of Health's Position regarding the expansion of the vaccination operation to ages 12-16 years. Accessed July 11, 2021. https://www.gov.il/en/departments/news/02062021-01
- 15.Israel Ministry of Health. Vaccination for pupils aged 16-18 (Including 12th Grade Pupils over 18). Accessed July 11, 2021. https://www.gov.il/en/departments/news/21012021-04
- 16.Walla news. Distribution of ages in COVID-19 vaccinated. Accessed July 8, 2021. [in Hebrew]. https://news.walla.co.il/item/3409450
- 17.Israel Central Bureau of Statistics. Characterization and Classification of Geographical Units by the Socio-Economic Level of the Population, 2017. Accessed August 18 2021. https://www.cbs.gov.il/en/publications/Pages/2021/socio-2017-e.aspx
- 18.Bleikh H, Claude B, Gilad B. State of the Nation Report 2016-Society, Economy and Policy in Israel. Taub Center for Social Policy Studies in Israel. 2016. Poverty and inequality in Israel: trends and decompositions. [Google Scholar]
- 19.Israel Central Bureau of Statistics. Annual statistics of Israel. 2015. Accessed July 11 2021. https://www.cbs.gov.il/he/publications/Pages/2015/שנתון-סטטיסטי-לישראל-2015-מספר-66.aspx
- 20.Byrne L, Ward C, White JM, Amirthalingam G, Edelstein M. Predictors of coverage of the national maternal pertussis and infant rotavirus vaccination programmes in England. Epidemiol Infect. 2018 Jan;146(2):197–206. doi: 10.1017/S0950268817002497. Epub 2017 Dec 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tessier E, Warburton F, Tsang C, Rafeeq S, Boddington N, Sinnathamby M, et al. Population-level factors predicting variation in influenza vaccine uptake among adults and young children in England, 2015/16 and 2016/17. Vaccine. 2018 May 31;36(23):3231–3238. doi: 10.1016/j.vaccine.2018.04.074. Epub 2018 Apr 30. [DOI] [PubMed] [Google Scholar]
- 22.Israel Central Bureau of Statistics. Population in settlements by age, sex, statistical area and settlement form, 2017-2019. Accessed July 11 2021. https://www.cbs.gov.il/he/subjects/Pages/אוכלוסייה-ביישובים.aspx
- 23.Israel Government Data Base - Vaccinated against COVID-19 by settltement. Accessed July 11 2021. https://data.gov.il/dataset/covid-19/resource/12c9045c-1bf4-478a-a9e1-1e876cc2e18
- 24.Israel Central Bureau of Statistics. Local authorities in Israel, 2018. Accesed July 11 2021. https://www.cbs.gov.il/he/publications/Pages/2020/הרשויות-המקומיות-בישראל-2018.aspx
- 25.Stein-Zamir C, Zentner G, Abramson N, et al. Measles outbreaks affecting children in Jewish ultra-orthodox communities in Jerusalem. Epidemiol Infect. 2008;136(2):207–214. doi: 10.1017/S095026880700845X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The OpenSAFELY Collaborative. Trends and clinical characteristics of COVID-19 vaccine recipients: a federated analysis of 57.9 million patients’ primary care records in situ using OpenSAFELY. Available as a pre-print (medRxiv). Accessed August 18 2021. https://www.medrxiv.org/content/10.1101/2021.01.25.21250356v3
- 28.Pingali C, Meghani M, Razzaghi H, et al. COVID-19 vaccination coverage among insured persons aged ≥16 years, by race/ethnicity and other selected characteristics - Eight Integrated Health Care Organizations, United States, December 14, 2020-May 15, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(28):985–990. doi: 10.15585/mmwr.mm7028a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stein-Zamir C, Israeli A. Timeliness and completeness of routine childhood vaccinations in young children residing in a district with recurrent vaccine-preventable disease outbreaks, Jerusalem, Israel. Euro Surveill. 2019;24(6) doi: 10.2807/1560-7917.ES.2019.24.6.1800004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this study are publicly available. Vaccination data by municipality and age are available from the Israel Ministry of Health COVID19 data repository: https://data.gov.il/dataset/covid-19
Data about population size in each municipality and socio economic status of each municipality can be found in the Israel Central Bureau for Statistics website: https://www.cbs.gov.il/EN/Pages/default.aspx