Abstract
Schizophrenia is a severe psychiatric disorder with high premature mortality rates. This is a meta-analysis and systematic review of the prevalence of suicidal ideation (SI) and suicide plan (SP) among people with schizophrenia. PubMed, Web of Science, Embase, and PsycINFO were systematically searched from their respective inception to October 10, 2020. Data on prevalence of SI and/or SP were synthesized using the random effects model. Twenty-six studies covering 5079 people with schizophrenia were included for meta-analysis. The lifetime and point prevalence of SI were 34.5% (95% CI: 28.2−40.9%), and 29.9% (95% CI: 24.2−35.6%), respectively. The lifetime prevalence of SP was 44.3% and the point prevalence of SP ranged between 6.4 and 13%. Subgroup and meta-regression analyses revealed that source of patients, survey countries, and sample size were significantly associated with the point prevalence of SI, while male proportion and quality assessment scores were significantly associated with the lifetime and point prevalence of SI. Survey time and mean age were significantly associated with lifetime prevalence of SI. Both SI and SP are common in people living with schizophrenia, especially in males and inpatients. Routine screening and effective interventions for SI and SP should be implemented in this population.
Subject terms: Schizophrenia, Diseases
Introduction
Schizophrenia is a severe psychiatric disorder characterized by cognitive impairment and behavioral dysfunction [1]. Compared with the general population, people living with schizophrenia have a reduced life expectancy of 10–25 years [2] and higher premature mortality rates [3], with suicide as a common cause of death [3, 4]. Suicide is a critical global health challenge [5]. Suicidal behavior exists on a continuum, ranging from repeated thoughts of killing oneself (i.e., suicidal ideation, SI), making a plan for suicide (i.e., suicide plan, SP), suicide attempts (SA) to completed suicide [6, 7]. SI, SP, and SA are the strong predictors of completed suicide [7–12]. SI, SP, and SA are also common in people living with schizophrenia, but the epidemiological findings in this population are mixed [13, 14]. For instance, a meta-analysis of 19 studies on the prevalence of suicide-related behaviors in schizophrenia in China [15] found that the pooled lifetime prevalence of SI and SA were 25.8% (95% CI: 14.7−41.1%) and 14.6% (95% CI: 9.1−22.8%), respectively [15]. Another meta-analysis of 81 studies [16] on the risk of subsequent completed suicide found that people living with schizophrenia who reported SI had a 5.8-fold higher risk of future suicide than those without SI.
In order to develop and adopt effective measures and public education to reduce suicide risk and relevant negative health outcomes, exploring the epidemiology of suicidality in people living with schizophrenia is of great public health significance. A meta-analysis [17] showed the pooled lifetime prevalence of SA was 26.8% (95% CI: 22.1−31.9%) among people living with schizophrenia. In contrast, no meta-analysis was published for pooled SI, and the estimates within individual studies [18–23] ranging between 11.0% in China [23] and 51.4% in the USA [21]. This is the similar case for SP among people living with schizophrenia [24–26]. Therefore, we conducted this meta-analysis to examine the prevalence of SI and SP in people living with schizophrenia and identify key correlates (e.g. age, gender, and source of patients) of SI and SP within this population.
Methods
Search strategy
This meta-analysis was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and the Meta-analysis Of Observational studies in Epidemiology (MOOSE) [27] recommendations. The registration number of this protocol in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY) was INPLASY20200120142. Three researchers (WB, YYJ, and ZHL) independently searched relevant publications in PubMed, Web of Science, Embase, and PsycINFO from their respective inception to October 10, 2020 using the following search terms: suicid* ideation, suicid* idea, suicid* thought, suicid* plan, self-injurious behavior, self-harm, self-injury, schizophreni*, Dementia Praecox, epidemiology, prevalence, and rate.
Study selection
The same three researchers independently screened titles and abstracts of relevant publications first followed by reading full texts for eligibility. Any disagreement was resolved by consensus or a discussion with a senior researcher (YTX). To be eligible, the following inclusion criteria according to the PICOS acronym were made: Participants (P): People living with schizophrenia diagnosed according to study-defined diagnostic criteria (e.g. Diagnostic and Statistical Manual of Mental Disorders, third edition (DSM-III), DSM-IV, and the Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10)); Intervention (I): not applicable; Comparison (C): not applicable; Outcome (O): prevalence of SI and/or SP or relevant data that enabled calculations of the prevalence of SI/SP; Study design (S): cross-sectional or cohort studies (only the baseline data of cohort studies were extracted). Exclusion criteria included: (1) timeframe of prevalence of SI and/or SP was missing; (2) studies published in non-English; (3) in order to increase homogeneity [17], studies with mixed samples (e.g. schizoaffective or schizophrenia spectrum disorders) in which data on schizophrenia cannot be extracted were excluded. To avoid missing studies, reference list of included publications was searched manually. If multiple papers were published based on the same dataset, only the one with the largest sample size was included [28].
Data extraction and quality assessment
Data were independently extracted by the same three researchers (WB, YYJ, and ZHL), including the first author, publication year, survey period, country, study design, sample size, events of SI/SP, mean age, male proportion, mean onset age, first-episode (yes/no/mixed/not reported), source of participants (inpatient, outpatient, mixed or not report), duration of illness, severity of psychotic symptoms measured by standardized scales such as the Positive and Negative Syndrome Scale (PANSS) [29] scores, education level, diagnostic system for schizophrenia (DSM vs. ICD), assessment tool of SI/SP and timeframe. Study quality assessment was conducted using an eight-item assessment instrument for epidemiological studies with the total score ranging from 1 to 8 points [30, 31]. Study quality were collapsed into low (0–3 points), moderate (4–6 points), and high quality (7 and 8 points) [30]. Any uncertainty was resolved by consensus or a discussion with a senior researcher (YTX).
Statistical analysis
The pooled prevalence of SI/SP and corresponding 95% confidence interval (CI) was calculated using the random-effect model. Study heterogeneity was evaluated by I2 statistic, with I2 more than 50% indicating high heterogeneity [32]. Subgroup and meta-regression analyses were performed to explore the source of heterogeneity. Subgroup analyses were conducted when there were at least three studies in each subgroup [33]. Subgroup analyses were performed based on the following categorical variables: gender, source of patients, sampling method, type of countries (high-income vs. low- and middle-income countries according to the International Monetary Fund [34], measurement instrument for SI/SP, average education year (dichotomized using the median split method), and sample size (dichotomized using the median split method) [28]. Meta-regression analyses were conducted for continuous variables (including survey time, mean age, male proportion, quality assessment scores, and duration of illness) if the number of included studies was more than 10 [35]. Publication bias was examined by funnel plots and Begg’s test [36]. Sensitivity analysis was conducted to test the consistency of primary results by removing each study one by one. The significance level was set as P < 0.05 (two-tailed). Data analyses were conducted with STATA, Version 15.0 (StataCorp LLC, College Station, Texas, USA) and Comprehensive Meta-Analysis Version 2.0 (Biostat Inc., Englewood, New Jersey, USA).
Results
Search results, study characteristics, and quality assessment
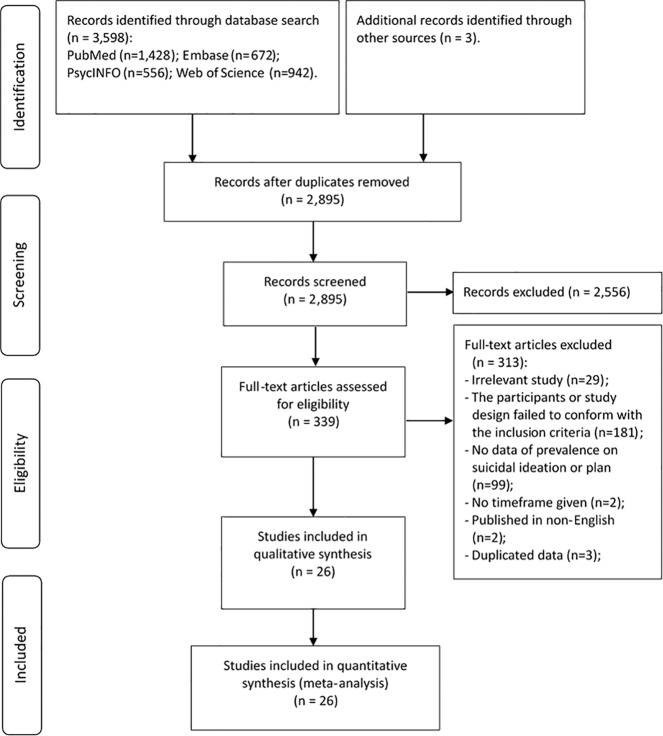
A total of 3601 publications were initially identified; of which, 26 studies covering 5079 people living with schizophrenia fulfilled the study criteria and were included (Fig. 1). Study characteristics are presented in Table 1. The sample size of the 26 studies ranged from 35 to 720 and the mean age ranged from 21.6 to 46.7 years. Most were cross-sectional studies (n = 25, 96%) and used non-probability sampling (n = 19, 73%). Most studies used the DSM system (n = 22, 85%) while two studies used the ICD-10, and another two studies used DSM or ICD.
Fig. 1. Flowchart of study selection.
This figure described the procedure of studies selection. Among 3601 publications identified through literature search, 26 studies met the inclusion criteria and were included.
Table 1.
Characteristics of included studied in the meta-analysis.
| No. | First author (publication year) | References | Country | Survey time | Study design | Sampling method | Sample size | Demographic information | Schizophrenia-related information | SI-related information | Quality assessment score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Source of patients | Mean age (years) | Male gender proportion (%) | Average education level (years) | Diagnostic criteriaa | Average onset age (years) | Average duration of illness (years) | Measure instrument | Timeframe of SI | |||||||||
| 1 | Acosta (2020) | [73] | Spain | 2012−2015 | Cohort | Non-probability sampling | 133 | Outpatient | 46.7 | 69.2 | Categorical data | ICD-10 | NR | 20.84 | Scale | Lifetime | 4 |
| 2 | Ainiyet (2014) | [37] | Poland | Sept. 2005−Jun. 2006 | Cross-sectional | Non-probability sampling | 148 | Inpatient | 32 | 46.63 | NR | DSM-IV | NR | 7 | Interview | 3-month | 4 |
| 3 | Dell’Osso (2012)b | [25] | Italy | NR | Cross-sectional | Non-probability sampling | 79 | Mixed | 36.28 | 69.6 | Categorical data | DSM-IV | NR | NR | Question | Lifetime | 5 |
| 4 | Duko (2018) | [74] | Ethiopia | Aug. 2016−Sept. 2016 | Cross-sectional | Probability sampling | 272 | NR | 33.71 | 68.8 | Categorical data | DSM-IV | NR | NR | Interview | Lifetime | 5 |
| 5 | Evren (2004) | [75] | Turkey | Aug. 2001−Jan. 2002 | Cross-sectional | Probability sampling | 60 | Mixed | 39.17 | 50 | 8.4 | DSM-IV | NR | 15.38 | Scale | Point | 5 |
| 6 | Fang (2019) | [19] | China | NR | Cross-sectional | NR | 174 | NR | 35.83 | 47.13 | 13.06 | DSM-IV | 23.6 | 12.23 | Scale | Point | 4 |
| 7 | Grover (2017) | [48] | India | NR | Cross-sectional | Non-probability sampling | 181 | Mixed | 34 | 53.6 | 11.6 | DSM-IV | 23.2 | 10.78 | NR | Point | 4 |
| 8 | Hintikka (1998) | [76] | Finland | May. 1993 | Cross-sectional | Probability sampling | 71 | Mixed | NR | NR | NR | DSM-III | NR | NR | Scale | Point | 6 |
| 9 | Hocaoglu (2009) | [77] | Turkey | Apr. 2006−Jun. 2006 | Cross-sectional | Non-probability sampling | 120 | Mixed | 36.7 | 52.5 | NR | DSM-IV | NR | NR | Scale | Lifetime | 4 |
| 10 | Hosseini (2012) | [78] | Iran | 2007−2008 | Cross-sectional | Non-probability sampling | 100 | Inpatient | 34.9 | 74 | NR | DSM-IV | 23.1 | 11.6 | Scale | Lifetime | 5 |
| 11 | Iancu (2010) | [79] | Israel | 2000 | Cross-sectional | Non-probability sampling | 68 | Inpatient | 39.4 | 100 | NR | DSM-IV | NR | 15 | Scale | Lifetime & point | 4 |
| 12 | Jovanović (2013) | [80] | Croatia | 2007−2010 | Cross-sectional | Non-probability sampling | 509 | NR | 33.71 | 47 | NR | DSM-IV | NR | 5.49 | Scale | Lifetime | 4 |
| 13 | Kao (2012) | [81] | China | NR | Cross-sectional | Non-probability sampling | 102 | Outpatient | 39.47 | 49.02 | 12.88 | DSM-IV | 24.14 | 16.2 | Scale | Point | 6 |
| 14 | Kibru (2020) | [82] | Ethiopia | May 2018−Jun. 2018 | Cross-sectional | Probability sampling | 409 | Outpatient | 22 | 62.3 | Categorical data | DSM-V | Categorical data | NR | Scale | Lifetime | 7 |
| 15 | Kim (2010) | [83] | Korea | NR | Cross-sectional | Non-probability sampling | 84 | Inpatient | 43 | 53.6 | 11.7 | DSM-IV | 24.5 | 12.9 | Question | Point | 4 |
| 16 | Kontaxakis (2004)b | [26] | Greece | Oct. 1996−Nov. 1997 | Cross-sectional | Non-probability sampling | 93 | Inpatient | 30.3 | 69 | 12.3 | DSM-IV | NR | 7.2 | Scale | Point | 4 |
| 17 | Minzenberg (2014) | [21] | USA | NR | Cross-sectional | Non-probability sampling | 35 | Outpatient | 21.55 | 82.86 | 12.81 | DSM-IV | NR | NR | Scale | Lifetime | 4 |
| 18 | Misiak (2015) | [84] | Poland | NR | Cross-sectional | Non-probability sampling | 100 | NR | 27.8 | 53 | Categorical data | DSM-IV | NR | NR | Scale | Lifetime | 4 |
| 19 | Pelizza (2020) | [18, 24] | Italy | Jan. 2013−Dec. 2018 | Cross-sectional | Non-probability sampling | 43 | NR | NR | NR | NR | DSM-IV | NR | NR | Scale | Lifetime | 4 |
| 20 | Prokopez (2020)b | [85] | Argentina | Jul. 2017−Feb. 2018 | Cross-sectional | Non-probability sampling | 100 | NR | 45.82 | 50 | 10 | DSM/ICD-10 | 22 (median) | 21.93 | Scale | Point | 4 |
| 21 | Radomsky (1999) | [38] | USA | Jan. 1, 1992−May 1, 1994 | Cross-sectional | Non-probability sampling | 454 | Inpatient | NR | 64.3 | NR | DSM-III | NR | NR | Hospital records | Lifetime & point & more than 1 month before admission | 4 |
| 22 | Ran (2004) | [23] | China | May 1, 2002−Aug. 20, 2002 | Cross-sectional | Non-probability sampling | 145 | Inpatient | 32.2 | 51 | Categorical data | DSM-IV | 25.7 | 6.6 | Scale | Lifetime | 6 |
| 23 | Schwartz (2001) | [86] | USA | NR | Cross-sectional | NR | 267 | Inpatient | 37.2 | 54 | NR | DSM-IV | NR | 14.4 | Interview | Point | 4 |
| 24 | Touriño (2018) | [20] | Spain | Mar. 2014−Jul. 2014 | Cross-sectional | Non-probability sampling | 71 | Outpatient | 40.07 | 80.28 | Categorical data | ICD-10 | NR | 17 (median) | Scale | Lifetime & 1 year | 4 |
| 25 | Yan (2013) | [22] | China | Jan. 2007 | Cross-sectional | Probability sampling | 540 | Outpatient | 42.8 | 49.4 | 10.4 | DSM-IV/ICD-10 | 25.7 | 17.08 | Scale | Point | 6 |
| 26 | YildiZ (2010) | [87] | Turkey | Mar. 1, 2006−Mar. 1, 2008 | Cross-sectional | Non-probability sampling | 720 | Outpatient | 35.5 | 50.3 | 8.7 | DSM-IV | 23.5 | 12 | Interview | Lifetime | 4 |
NR not reported, SI suicidal ideation.
aDiagnostic criteria: DSM-III, Diagnostic and Statistical Manual of Mental Disorders, third edition; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; DSM-V, Diagnostic and Statistical Manual of Mental Disorders, 5th edition; ICD-10, the Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems.
bDell’Osso et al. reported the lifetime prevalence of suicidal plan (SP), Kontaxakis et al. and Prokopez et al. reported the point prevalence of SP.
Most studies used items from standardized scales (e.g. the Calgary Depression Scale for Schizophrenia (CDSS), the Hamilton Depression Scale (HAMD), and the Suicide Risk Scale (SRS)) on suicidality to measure SI/SP. In four studies, interviews were conducted to collect data on SI/SP, while in another two studies, standardized questions on SI/SP were used, and in another study, data on SI/SP were collected from hospital records (Table 1). Fourteen studies reported lifetime prevalence, 13 studies reported point prevalence, one study reported 3-month prevalence, one study reported 1-year prevalence, and one study reported prevalence of SI during more than 1-month period before inpatient admission. In contrast, one study reported the lifetime prevalence and two studies reported point prevalence of SP.
Scores of study quality assessment ranged from 4 to 7; of which, one study was rated as “high quality” (4%) and 25 were “moderate quality” (96%) (Supplementary Table S1). The data on severity of psychotic symptoms measured by the PANSS are shown in Supplementary Table S2.
Prevalence of suicidal ideation and suicide plan
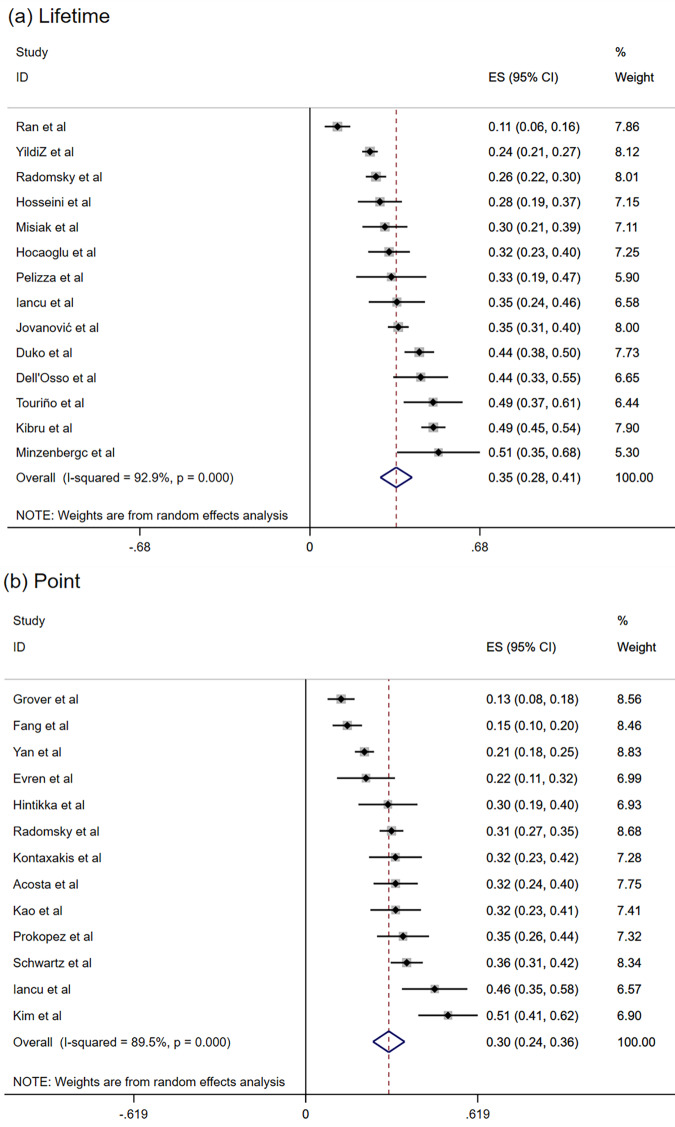
The pooled lifetime prevalence of SI was 34.5% (95% CI: 28.2−40.9%; I2 = 92.9%) (Fig. 2a), and the pooled point prevalence of SI was 29.9% (95% CI: 24.2−35.6%; I2 = 89.5%). The 3-month prevalence [37], 1-year prevalence [20], and prevalence of SI during more than 1 month period before admission [38] was 44.6%, 16.2%, and 19.6%, respectively. The lifetime prevalence of SP was 44.3% [25], and point prevalence of SP in two studies was 6.4% [26] and 13% [24], respectively.
Fig. 2. Forest plot of the prevalence of suicidal ideation (SI).
a Lifetime prevalence of SI; b Point prevalence of SI.
Subgroup and meta-regression analyses
The results of subgroup analyses are shown in Table 2. Source of participants, survey countries, and sample size were significantly associated with the point prevalence of SI (all P values < 0.05). In meta-regression analyses, survey time (β = 0.0428, z = 8.34, P < 0.001) and quality assessment scores (β = 0.2387, z = 6.69, P < 0.001) were positively associated with lifetime prevalence of SI, while mean age was negatively associated with lifetime prevalence of SI (β = −0.0464, z = −6.01, P < 0.001), and male proportion was positively associated with the lifetime (β = 0.0165, z = 4.81, P < 0.001) and the point prevalence of SI (β = 0.0196, z = 4.60, P < 0.001). Additionally, quality assessment scores were negatively associated with the point prevalence of SI (β = −0.1963, z = −3.74, P < 0.001).
Table 2.
Subgroup and meta-regression analyses of lifetime and point prevalence of suicidal ideation in patients with schizophrenia.
| Subgroup analyses | ||||||||
|---|---|---|---|---|---|---|---|---|
| Subgroupsa | Categories (number of studies) | Events | Sample size | Prevalence (%) | 95% CI (%) | I2 (%) | P values within subgroups | Q (P values across subgroups) |
| Lifetime | ||||||||
| Gender | Male (6) | 188 | 509 | 36.9 | 31.0–43.2 | 0 | 0.518 | 0.092 (0.762) |
| Female (5) | 137 | 403 | 35.4 | 28.3–43.1 | 62.3 | 0.031 | ||
| Source of patients | Outpatients (4) | 427 | 1233 | 42.2 | 27.3–58.8 | 96.4 | <0.001 | 3.095 (0.079) |
| Inpatients (4) | 188 | 768 | 23.8 | 13.8–37.9 | 83.6 | <0.001 | ||
| Survey country | High-income (6) | 245 | 749 | 38.9 | 28.8–50.0 | 81.1 | <0.001 | 1.384 (0.239) |
| Low- or middle-income (8) | 786 | 2375 | 30.9 | 23.6–39.3 | 94.0 | <0.001 | ||
| Sample size | ≤110 (7) | 183 | 495 | 38.0 | 29.0–48.0 | 60.5 | 0.019 | 1.289 (0.256) |
| >110 (7) | 848 | 2629 | 30.8 | 23.4–39.3 | 95.2 | <0.001 | ||
| Measure of instrument | Scale (10) | 584 | 1599 | 34.2 | 27.3–41.9 | 88.1 | <0.001 | 0.010 (0.921) |
| Non-scale (4) | 447 | 1525 | 33.5 | 23.7–45.1 | 93.5 | <0.001 | ||
| Point | ||||||||
| Gender | Male (7) | 200 | 679 | 33.4 | 24.2–44.1 | 85.2 | <0.001 | 0.580 (0.446) |
| Female (6) | 135 | 547 | 27.8 | 18.9–38.9 | 79.7 | <0.001 | ||
| Source of patients | Outpatient (3) | 190 | 775 | 27.7 | 19.9–37.2 | 81.8 | 0.004 | 9.553 (0.008) |
| Inpatient (5) | 342 | 967 | 38.5 | 30.8–46.8 | 76.5 | 0.002 | ||
| Mixed (3) | 57 | 312 | 20.0 | 13.3−29.0 | 79.7 | 0.007 | ||
| Survey country | High-income (7) | 403 | 1171 | 36.4 | 30.1–43.3 | 67.5 | 0.005 | 10.725 (0.001) |
| Low- or middle-income (6) | 244 | 1157 | 22.0 | 17.0–27.8 | 83.2 | <0.001 | ||
| Sampling method | Probability sampling (3) | 148 | 671 | 23.7 | 15.4–34.8 | 22.7 | 0.331 | 2.018 (0.155) |
| Non-probability sampling (8) | 379 | 1216 | 32.9 | 26.2–40.3 | 85.5 | <0.001 | ||
| Average education year | ≤11.6 (4) | 185 | 881 | 21.7 | 13.2–33.5 | 83.8 | <0.001 | 1.283 (0.257) |
| >11.6 (4) | 132 | 453 | 31.1 | 19.9–45.2 | 91.4 | <0.001 | ||
| Sample size | ≤118 (7) | 207 | 579 | 35.4 | 27.6–43.9 | 68.3 | 0.004 | 4.499 (0.034) |
| >118 (6) | 443 | 1749 | 24.0 | 18.0–31.1 | 91.0 | <0.001 | ||
| Measure of instrument | Scale (9) | 347 | 1342 | 28.6 | 23.0–34.9 | 81.4 | <0.001 | 2.471 (0.116) |
| Non-scale (3) | 280 | 805 | 38.4 | 28.0–50.0 | 84.6 | 0.002 | ||
| Meta-regression analyses | ||||||
|---|---|---|---|---|---|---|
| Covariates | Coefficient | Standard error | 95% lower | 95% upper | z value | P value |
| Lifetime | ||||||
| Survey time | 0.0428 | 0.0051 | 0.0327 | 0.0529 | 8.34 | <0.001 |
| Male proportion | 0.0165 | 0.0034 | 0.0098 | 0.0232 | 4.81 | <0.001 |
| Mean age (years) | −0.0464 | 0.0077 | −0.0616 | −0.0313 | −6.01 | <0.001 |
| Study quality assessment | 0.2387 | 0.0357 | 0.1688 | 0.3086 | 6.69 | <0.001 |
| Point | ||||||
| Male proportion (%) | 0.0196 | 0.0043 | 0.0112 | 0.0279 | 4.60 | <0.001 |
| Mean age (years) | 0.0022 | 0.0125 | −0.0223 | 0.0267 | 0.18 | 0.860 |
| Duration of illness (years) | 0.0138 | 0.0152 | −0.0160 | 0.0437 | 0.91 | 0.363 |
| Study quality assessment | −0.1963 | 0.0525 | −0.2992 | −0.0934 | −3.74 | <0.001 |
CI confidence interval.
aContinuous variables in subgroup analyses were divided according to median splitting method.
Sensitivity analyses and publication bias
After removing studies one by one in sensitivity analyses, no outlying studies that could significantly change the primary results were found (Supplementary Fig. S1). Although funnel plots show slight asymmetry, Begg’s tests did not reveal significant publication bias (lifetime prevalence of SI: z = 1.31, P = 0.222; point prevalence of SI: z = 1.04, P = 0.300) (Supplementary Fig. S2).
Discussion
Suicidality such as SI and SP is common in individuals with severe mental health problems including schizophrenia [39], particularly in hospitalized patients, which is significantly associated with increased risk of suicide [16]. Effective interventions targeting patients with schizophrenia who are at high risk of SI and SP are a priority for reducing the likelihood of future suicide [40]. To the best of our knowledge, this was the first study that examined the prevalence of SI and SP among people living with schizophrenia globally. The pooled lifetime prevalence of SI was 34.5% (95% CI: 28.2−40.9%), which is higher than the corresponding figure (25.8%, 95% CI: 14.7–41.1%) among people living with schizophrenia in China [15]. Moreover, this figure is much higher than that in the global general population (9.2%) [41]. The pooled point prevalence of SI in this meta-analysis was 29.9% (95% CI: 24.2−35.6%) among people living with schizophrenia, which is higher than the figure in homeless people (17.8%, 95% CI: 10.7−28.1%) [42]. SI among people living with schizophrenia could be associated with severe psychiatric symptoms (e.g., depressive symptoms), heavy economic burden, and severe stigma and discrimination, all of which could increase the risk of suicide [3, 43–46]. No global figure on SP was previously reported; therefore, direction comparisons were not made. It is noteworthy that different demographic characteristics, illness stage, comorbidities, and treatments were associated with the epidemiology of suicidality including SI and SP [16, 47, 48]; therefore, direct comparisons of the findings between this meta-analysis and other studies should be made with caution.
Subgroup analyses revealed that point prevalence of SI among inpatients with schizophrenia (38.5%, 95% CI: 30.8−46.8%) was higher than those in other settings (e.g., outpatients: 27.7%, 95% CI: 19.9−37.2%; mixed in- and outpatients: 20.0%, 95% CI: 13.3−29.0%). Hospitalized patients usually suffer from more severe psychiatric symptoms, particularly depressive symptoms, which is associated with higher risk of suicidality [43, 44]. The point prevalence of SI was higher in studies with small sample sizes. It should be noteworthy that small sample size is usually associated with unstable findings in epidemiological surveys [49, 50]; therefore, this finding suggests selection bias in small samples that should be taken into account in future studies. The point prevalence of SI in high-income countries (36.4%, 95% CI: 30.1−43.3%) was higher than the corresponding figure in low- and middle-income countries (22.0%, 95% CI: 17.0−27.8%). The discrepancy in SI across countries could be partly explained by different socioeconomic factors and health service systems [51–55]. For instance, suicide screening and reporting systems are usually well established in high-income countries; therefore, SI in these countries are more likely to be identified. A cohort study of psychiatric patients found that higher income individuals were associated with a higher risk of suicide (hazard ratio (HR): 2.21, 95% CI: 2.06–2.35) [51]. Another study involving 17 countries found that the prevalence of SI in patients with mood disorders in high-income countries (OR = 4.7, 95% CI: 4.2−5.2) was higher than that in low- and middle-income countries (OR = 3.4, 95% CI: 2.8−4.1) [41].
Meta-regression analyses revealed that the lifetime prevalence of SI was positively associated with survey year, which could be due to several reasons. First, schizophrenia has gained growing attention globally because of its heavy social and economic burden [3, 56], resulting in increasing reported prevalence of suicidality including SI. Second, certain contributing factors of suicidality, such as alcohol and substance abuse, have been increasing over time [57–59], which could increase the likelihood of SI. Third, reports on suicide of celebrities in the media have increased in recent decades [60–62]. A meta-analysis found the risk of suicide increased by 13% (95% CI: 8−18%) in the general population after the suicide of a celebrity was reported in the media [63]. Therefore, extensive media reports on suicide of celebrities in recent years may have increased the prevalence of suicidality among people living with schizophrenia. The mean age of people living with schizophrenia was negatively associated with the lifetime prevalence of SI, which is consistent with previous findings [64, 65]. Compared to older patients, younger patients usually face greater social and survival stress in daily life and are more likely to contact online suicide-related information [65], both of which could increase the risk of suicidality. Meta-regression analyses revealed that male gender was positively associated with both and lifetime point prevalence of SI in schizophrenia patients, which confirms previous findings that male gender is a risk factor of suicide in both among people living with schizophrenia [66] and the general population [49]. A meta-analysis of 35 studies found that compared with female patients, males living with schizophrenia had a higher risk of suicide (OR = 1.34, 95% CI: 1.14–1.58) [66]. Males living with schizophrenia usually experienced more stigma [45], and had higher unemployment rate [67, 68], higher rate of alcohol and substance use [69], and higher levels of impulsivity and aggression [70], all of which are associated with higher suicide risk [66]. In meta-regression analyses, we also observed that quality scores were positively associated with the lifetime prevalence of SI, but negatively associated with the point prevalence of SI. It should be noted that the number of included studies was small in the two analyses (n = 14 and n = 13, respectively), which may reduce the statistical power of the findings. Additionally, the possibility of recall bias in the assessment of lifetime SI could not be excluded. In high-quality studies good training on the use of instruments, random sampling, and strict quality control are usually adopted. These factors may reduce the risk of false positive rates, and may also result in a relatively lower prevalence of suicidality compared to poor quality studies.
The strengths of this systematic review and meta-analysis are the large number of included studies across different countries globally, the large sample size, and use of sophisticated analyses such as subgroup, meta-regression, and sensitivity analyses. However, several limitations should be noted. First, heterogeneity could not be avoided when conducting the meta-analysis of epidemiological studies [71, 72], although subgroup analyses and meta-regression analyses were conducted. Second, some factors related to SI, such as illness severity, comorbid depression, severity of psychotic symptoms, and use of antipsychotics, were not examined due to insufficient data in the included studies. Third, data of SI were retrospectively collected in some studies, which may lead to recall bias. Fourth, only published studies were included in this meta-analysis due to a lack of access to unpublished data, which may have biased our findings to an uncertain extent. Finally, the prevalence of SP was not synthesized due to limited number of studies.
In conclusion, both SI and SP were common among people living with schizophrenia, especially in males and inpatients. Considering the close associations of SI and SP with future suicide, routine screening on suicidality should be carried out to identify those at high risk in order to provide timely treatments to those in need.
Supplementary information
Acknowledgements
The study was supported by the National Science and Technology Major Project for Investigational New Drug (2018ZX09201-014), the Beijing Municipal Science & Technology Commission (No. Z181100001518005), Scientific Research Common Programof Beijing Municipal Commission of Education (KM202010025011), Beijing Municipal Science & Tech Commission (Z191100006619061) and the University of Macau (MYRG2019-00066-FHS).
Author contributions
Study design: WB, QEZ, YTX. Data collection, analysis and interpretation: WB, ZHL, YYJ, QEZ, WWR. Drafting of the manuscript: WB, QEZ, YTX. Critical revision of the manuscript: TC, BJH. Approval of the final version for publication: all co-authors.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: W. Bai, Z.H. Liu, Y.Y. Jiang, Q.E. Zhang.
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-021-01671-6.
References
- 1.Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388:86–97. doi: 10.1016/s0140-6736(15)01121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dickerson F, Stallings C, Origoni A, Schroeder J, Khushalani S, Yolken R. Mortality in schizophrenia: clinical and serological predictors. Schizophrenia Bull. 2014;40:796–803. doi: 10.1093/schbul/sbt113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laursen TM. Causes of premature mortality in schizophrenia: a review of literature published in 2018. Curr Opin Psychiatry. 2019;32:388–93. doi: 10.1097/yco.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 4.Piotrowski P, M. Gondek T, Królicka-Deręgowska A, Misiak B, Adamowski T, Kiejna A. Causes of mortality in schizophrenia: an updated review of European studies. Psychiatr Danubina. 2017;29:108–20. doi: 10.24869/psyd.2017.108. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Suicide in the world: global health estimates, https://www.who.int/teams/mental-health-and-substance-use/suicide-data (2019).
- 6.McKinnon B, Gariépy G, Sentenac M, Elgar FJ. Adolescent suicidal behaviours in 32 low- and middle-income countries. Bull World Health Organ. 2016;94:340–50f. doi: 10.2471/blt.15.163295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu ZZ, Wang ZY, Bo QG, Qi ZB, Xu RJ, Jia CX, et al. Suicidal behaviours among Chinese adolescents exposed to suicide attempt or death. Epidemiol Psychiatr Sci. 2018;29:e12.. doi: 10.1017/s2045796018000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knipe D, Metcalfe C, Hawton K, Pearson M, Dawson A, Jayamanne S, et al. Risk of suicide and repeat self-harm after hospital attendance for non-fatal self-harm in Sri Lanka: a cohort study. ancet Psychiatry. 2019;6:659–66. doi: 10.1016/s2215-0366(19)30214-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geulayov G, Casey D, Bale L, Brand F, Clements C, Farooq B, et al. Suicide following presentation to hospital for non-fatal self-harm in the Multicentre Study of Self-harm: a long-term follow-up study. ancet Psychiatry. 2019;6:1021–30. doi: 10.1016/s2215-0366(19)30402-x. [DOI] [PubMed] [Google Scholar]
- 10.Runeson B, Haglund A, Lichtenstein P, Tidemalm D. Suicide risk after nonfatal self-harm: a national cohort study, 2000−2008. J Clin Psychiatry. 2016;77:240–6. doi: 10.4088/JCP.14m09453. [DOI] [PubMed] [Google Scholar]
- 11.Banwari GH, Vankar GK, Parikh MN. Comparison of suicide attempts in schizophrenia and major depressive disorder: an exploratory study. Asia Pac Psychiatry. 2013;5:309–15. doi: 10.1111/j.1758-5872.2012.00188.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee Y, Lin PY, Yeh WC, Chiu NM, Hung CF, Huang TY, et al. Repeated suicide attempts among suicidal cases: outcome of one-year follow-up. Asia-Pac Psychiatry. 2012;4:174–80. doi: 10.1111/j.1758-5872.2012.00189.x. [DOI] [Google Scholar]
- 13.Scott LN, Pilkonis PA, Hipwell AE, Keenan K, Stepp SD. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: a multi-wave prospective study. Compr Psychiatry. 2015;58:1–10. doi: 10.1016/j.comppsych.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marangell LB, Bauer MS, Dennehy EB, Wisniewski SR, Allen MH, Miklowitz DJ, et al. Prospective predictors of suicide and suicide attempts in 1,556 patients with bipolar disorders followed for up to 2 years. Bipolar Disord. 2006;8:566–75. doi: 10.1111/j.1399-5618.2006.00369.x. [DOI] [PubMed] [Google Scholar]
- 15.Dong M, Wang SB, Wang F, Zhang L, Ungvari GS, Ng CH, et al. Suicide-related behaviours in schizophrenia in China: a comprehensive meta-analysis. Epidemiol Psychiatr Sci. 2019;28:290–9. doi: 10.1017/s2045796017000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hubers A, Moaddine S, Peersmann S, Stijnen T, van Duijn E, van der Mast RC, et al. Suicidal ideation and subsequent completed suicide in both psychiatric and non-psychiatric populations: a meta-analysis. Epidemiol Psychiatr Sci. 2018;27:186–98. doi: 10.1017/s2045796016001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu L, Dong M, Zhang L, Zhu XM, Ungvari GS, Ng CH, et al. Prevalence of suicide attempts in individuals with schizophrenia: a meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2019;29:e39. doi: 10.1017/s2045796019000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pelizza L, Pellegrini C, Quattrone E, Azzali S, Landi G, Pellegrini P, et al. Suicidal ideation in patients experiencing a first-episode psychosis: findings from the 2-year follow-up of the “Parma Early Psychosis” Program. Suicide Life-Threatening Behav. 2020;50:838–55. doi: 10.1111/sltb.12625. [DOI] [PubMed] [Google Scholar]
- 19.Fang XY, Yan C, Wang YW, Chen Z. Identification of risk factors for suicidal ideation in patients with schizophrenia. Psychiatry Res. 2019;271:195–9. doi: 10.1016/j.psychres.2018.11.051. [DOI] [PubMed] [Google Scholar]
- 20.Touriño R, Acosta FJ, Giráldez A, Álvarez J, González JM, Abelleira C, et al. Suicidal risk, hopelessness and depression in patients with schizophrenia and internalized stigma. Actas espanolas de psiquiatria. 2018;46:33–41. [PubMed] [Google Scholar]
- 21.Minzenberg MJ, Lesh TA, Niendam TA, Yoon JH, Rhoades RN, Carter CS. Frontal cortex control dysfunction related to long-term suicide risk in recent-onset schizophrenia. Schizophrenia Res. 2014;157:19–25. doi: 10.1016/j.schres.2014.05.039. [DOI] [PubMed] [Google Scholar]
- 22.Yan F, Xiang YT, Hou YZ, Ungvari GS, Dixon LB, Chan SS, et al. Suicide attempt and suicidal ideation and their associations with demographic and clinical correlates and quality of life in Chinese schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2013;48:447–54. doi: 10.1007/s00127-012-0555-0. [DOI] [PubMed] [Google Scholar]
- 23.Ran MS, Wu QH, Conwell Y, Chen EYH, Chan CLW. Suicidal behavior among inpatients with schizophrenia and mood disorders in Chengdu, China. Suicide Life-Threatening Behav. 2004;34:311–9. doi: 10.1521/suli.34.3.311.42784. [DOI] [PubMed] [Google Scholar]
- 24.Pelizza L, Pellegrini C, Quattrone E, Azzali S, Landi G, Pellegrini P, Leuci E. The history of multiple adverse childhood experiences in patients with schizophrenia is associated with more severe symptomatology and suicidal behavior with gender-specific characteristics. Arch Suicide Res. 2020;293:113411–21. doi: 10.1080/13811118.2020.1820411. [DOI] [PubMed] [Google Scholar]
- 25.Dell’Osso L, Giulia C, Marina C, Ciro C, Paolo G, Claudia C. Sexual obsessions and suicidal behaviors in patients with mood disorders, panic disorder and schizophrenia. Ann Gen Psychiatry. 2012. 10.1186/1744-859x-11-27. [DOI] [PMC free article] [PubMed]
- 26.Kontaxakis V, Havaki-Kontaxaki B, Margariti M, Stamouli S, Kollias C, Christodoulou G. Suicidal ideation in inpatients with acute schizophrenia. Can J Psychiatry. 2004;49:476–9. doi: 10.1177/070674370404900709. [DOI] [PubMed] [Google Scholar]
- 27.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 28.Dong M, Zeng LN, Lu L, Li XH, Ungvari GS, Ng CH, et al. Prevalence of suicide attempt in individuals with major depressive disorder: a meta-analysis of observational surveys. Psychol Med. 2019;49:1691–704. doi: 10.1017/s0033291718002301. [DOI] [PubMed] [Google Scholar]
- 29.Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 30.Boyle MH. Guidelines for evaluating prevalence studies. Evid-Based Ment Health. 1998;1:37–9. doi: 10.1136/ebmh.1.2.37. [DOI] [Google Scholar]
- 31.Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Epidemiol Psychiatr Sci. 1998;19:170–6. doi: 10.1017/s2045796019000313. [DOI] [PubMed] [Google Scholar]
- 32.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Epidemiol Psychiatr Sci. 2003;327:557–60. doi: 10.1017/s2045796019000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bai W, Li Y, Niu Y, Ding Y, Yu X, Zhu B, et al. Association between ambient air pollution and pregnancy complications: a systematic review and meta-analysis of cohort studies. Environ Res. 2020;185:109471.. doi: 10.1016/j.envres.2020.109471. [DOI] [PubMed] [Google Scholar]
- 34.International Monetary Fund. IMF country information. 2020. https://www.imf.org/en/countries.
- 35.Higgins JP, Green, S. Cochrane handbook for systematic reviews of interventions: Cochrane book series. United States: The Cochrane Library; 2008.
- 36.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 37.Ainiyet B, Rybakowski JK. Suicidal behavior in schizophrenia may be related to low lipid levels. Med Sci Monit: Int Med J Exp Clin Res. 2014;20:1486–90. doi: 10.12659/msm.890884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Radomsky ED, Haas GL, Mann JJ, Sweeney JA. Suicidal behavior in patients with schizophrenia and other psychotic disorders. Am J Psychiatry. 1999;156:1590–5. doi: 10.1176/ajp.156.10.1590. [DOI] [PubMed] [Google Scholar]
- 39.Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust NZ J Psychiatry. 2015;49:1087–206. doi: 10.1177/0004867415617657. [DOI] [PubMed] [Google Scholar]
- 40.Witt K, Potts J, Hubers A, Grunebaum MF, Murrough JW, Loo C, et al. Ketamine for suicidal ideation in adults with psychiatric disorders: a systematic review and meta-analysis of treatment trials. Aust NZ J Psychiatry. 2020;54:29–45. doi: 10.1177/0004867419883341. [DOI] [PubMed] [Google Scholar]
- 41.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry: J Ment Sci. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ayano G, Tsegay L, Abraha M, Yohannes K. Suicidal ideation and attempt among homeless people: a systematic review and meta-analysis. Psychiatr Q. 2019;90:829–42. doi: 10.1007/s11126-019-09667-8. [DOI] [PubMed] [Google Scholar]
- 43.Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81–90. doi: 10.1177/1359786810385490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sher L, Kahn RS. Suicide in schizophrenia: an educational overview. Medicina. 2019;55:361.. doi: 10.3390/medicina55070361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Masedo Gutiérrez AI, Grandón Fernández P, Bustos C, Moreno-Küstner B. Considerations about the assessment of stigma towards persons with schizophrenia: the question of gender. Asian J Psychiatry. 2017;28:148–9. doi: 10.1016/j.ajp.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 46.Naguy A. Depression in schizophrenia—a good or bad omen? Asia Pac Psychiatry. 2018;10:e12312.. doi: 10.1111/appy.12312. [DOI] [PubMed] [Google Scholar]
- 47.Lien YJ, Chang HA, Kao YC, Tzeng NS, Yeh CB, Loh CH. Self-stigma mediates the impact of insight on current suicide ideation in suicide attempters with schizophrenia: results of a moderated mediation approach. Suicide Life-Threatening Behav. 2018;48:661–676. doi: 10.1111/sltb.12384. [DOI] [PubMed] [Google Scholar]
- 48.Grover S, Dua D, Chakrabarti S, Avasthi A. Obsessive compulsive symptoms/disorder in patients with schizophrenia: prevalence, relationship with other symptom dimensions and impact on functioning. Psychiatry Res. 2017;250:277–284. doi: 10.1016/j.psychres.2017.01.067. [DOI] [PubMed] [Google Scholar]
- 49.Cao XL, Zhong BL, Xiang YT, Ungvari GS, Lai KY, Chiu HF, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. Int J Psychiatry Med. 2015;49:296–308. doi: 10.1177/0091217415589306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dong M, Lu L, Zhang L, Zhang Q, Ungvari GS, Ng CH, et al. Prevalence of suicide attempts in bipolar disorder: a systematic review and meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2019;29:e63. doi: 10.1017/s2045796019000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agerbo E. High income, employment, postgraduate education, and marriage: a suicidal cocktail among psychiatric patients. Arch Gen Psychiatry. 2007;64:1377–84. doi: 10.1001/archpsyc.64.12.1377. [DOI] [PubMed] [Google Scholar]
- 52.Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychological Bull. 2017;143:187–232. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- 53.Haghparast-Bidgoli H, Rinaldi G, Shahnavazi H, Bouraghi H, Kiadaliri AA. Socio-demographic and economics factors associated with suicide mortality in Iran, 2001−2010: application of a decomposition model. Int J Equity Health. 2018;17:77.. doi: 10.1186/s12939-018-0794-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chang Q, Wu D, Rong H, Wu Z, Tao W, Liu H, et al. Suicide ideation, suicide attempts, their sociodemographic and clinical associates among the elderly Chinese patients with schizophrenia spectrum disorders. J Affect Disord. 2019;256:611–7. doi: 10.1016/j.jad.2019.06.069. [DOI] [PubMed] [Google Scholar]
- 55.Erausquin JT, McCoy TP, Bartlett R, Park E. Trajectories of suicide ideation and attempts from early adolescence to mid-adulthood: associations with race/ethnicity. J Youth Adolescence. 2019;48:1796–805. doi: 10.1007/s10964-019-01074-3. [DOI] [PubMed] [Google Scholar]
- 56.Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophrenia Bull. 2018;44:1195–203. doi: 10.1093/schbul/sby058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee KH, Jun JS, Kim YJ, Roh S, Moon SS, Bukonda N, et al. Mental health, substance abuse, and suicide among homeless adults. J Evid-Inf Soc Work. 2017;14:229–42. doi: 10.1080/23761407.2017.1316221. [DOI] [PubMed] [Google Scholar]
- 58.Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol Med. 2017;47:949–57. doi: 10.1017/s0033291716002841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shiels MS, Tatalovich Z, Chen Y, Haozous EA, Hartge P, Nápoles AM, et al. Trends in mortality from drug poisonings, suicide, and alcohol-induced deaths in the United States from 2000 to 2017. JAMA Netw Open. 2020;3:e2016217. doi: 10.1001/jamanetworkopen.2020.16217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ju Ji N, Young Lee W, Seok Noh M, Yip PS. The impact of indiscriminate media coverage of a celebrity suicide on a society with a high suicide rate: epidemiological findings on copycat suicides from South Korea. J Affect Disord. 2014;156:56–61. doi: 10.1016/j.jad.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 61.Andriessen K, Rahman B, Draper B, Dudley M, Mitchell PB. Prevalence of exposure to suicide: a meta-analysis of population-based studies. J Psychiatr Res. 2017;88:113–20. doi: 10.1016/j.jpsychires.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 62.Choi YJ, Oh H. Does media coverage of a celebrity suicide trigger copycat suicides?: Evidence from Korean cases. J Media Econ. 2016;29:92–105. doi: 10.1080/08997764.2016.1170020. [DOI] [Google Scholar]
- 63.Niederkrotenthaler T, Braun M, Pirkis J, Till B, Stack S, Sinyor M, et al. Association between suicide reporting in the media and suicide: systematic review and meta-analysis. BMJ (Clin Res Ed) 2020;368:m575. doi: 10.1136/bmj.m575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Martini M, da Fonseca RC, de Sousa MH, de Azambuja Farias C, Cardoso TA, Kunz M, et al. Age and sex trends for suicide in Brazil between 2000 and 2016. Soc Psychiatry Psychiatr Epidemiol. 2019;54:857–60. doi: 10.1007/s00127-019-01689-8. [DOI] [PubMed] [Google Scholar]
- 65.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005−2017. J Abnorm Psychol. 2019;128:185–99. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 66.Cassidy RM, Yang F, Kapczinski F, Passos IC. Risk factors for suicidality in patients with schizophrenia: a systematic review, meta-analysis, and meta-regression of 96 studies. Schizophrenia Bull. 2018;44:787–97. doi: 10.1093/schbul/sbx131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Osváth P, Kelemen G, Erdös MB, Vörös V, Fekete S. The main factors of repetition: review of some results of the Pecs Center in the WHO/EURO Multicentre Study on Suicidal Behaviour. Crisis. 2003;24:151–4. doi: 10.1027//0227-5910.24.4.151. [DOI] [PubMed] [Google Scholar]
- 68.Rodrigues AP, Sousa-Uva M, Fonseca R, Marques S, Pina N, Matias-Dias C. Depression and unemployment incidence rate evolution in Portugal, 1995−2013: General Practitioner Sentinel Network data. Rev de saude publica. 2017;51:98. doi: 10.11606/s1518-8787.2017051006675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ahsan MS, Mullick MS, Begum K, Arafat SM, Shah MA, Podder BR, et al. Substance use among the patients with first episode psychosis. Mymensingh Med J: MMJ. 2018;27:313–20. [PubMed] [Google Scholar]
- 70.Wang J, Zhang SM, Zhong SL, Mellsop G, Guo HJ, Li QG, et al. Gender differences among homicide offenders with schizophrenia in Hunan Province, China. Psychiatry Res. 2019;271:124–30. doi: 10.1016/j.psychres.2018.11.039. [DOI] [PubMed] [Google Scholar]
- 71.Long J, Huang G, Liang W, Liang B, Chen Q, Xie J, et al. The prevalence of schizophrenia in mainland China: evidence from epidemiological surveys. Acta Psychiatr Scandinavica. 2014;130:244–56. doi: 10.1111/acps.12296. [DOI] [PubMed] [Google Scholar]
- 72.Zhou JS, Zhong BL, Xiang YT, Chen Q, Cao XL, Correll CU, et al. Prevalence of aggression in hospitalized patients with schizophrenia in China: a meta-analysis. Asia Pac Psychiatry. 2016;8:60–9. doi: 10.1111/appy.12209. [DOI] [PubMed] [Google Scholar]
- 73.Acosta FJ, Navarro S, Cabrera B, Ramallo-Fariña Y, Martínez N. Painful insight vs. usable insight in schizophrenia. Do they have different influences on suicidal behavior? Schizophrenia Research. 2020;220:147–54. doi: 10.1016/j.schres. [DOI] [PubMed] [Google Scholar]
- 74.Duko B & Ayano G. Suicidal ideation and attempts among people with severe mental disorder, Addis Ababa, Ethiopia,comparative cross-sectional study. Annals of General Psychiatry. 2018;17(1). 10.1186/s12991-018-0193-3 [DOI] [PMC free article] [PubMed]
- 75.Evren C, Evren B. Characteristics of schizophrenic patients with a history of suicide attempt. International Journal of Psychiatry in Clinical Practice. 2004;8:227–34. doi: 10.1080/13651500410005658. [DOI] [PubMed] [Google Scholar]
- 76.Hintikka J, et al. Risk factors for suicidal ideation in psychiatric patients. Social Psychiatry and Psychiatric Epidemiology. 1998;33:235–40. doi: 10.1007/s001270050049. [DOI] [PubMed] [Google Scholar]
- 77.Hocaoglu C, Babuc ZT. Suicidal ideation in patients with schizophrenia. The Israel journal of psychiatry and relatedsciences. 2009;46:195–203. [PubMed] [Google Scholar]
- 78.Hosseini SH, Zarghami M, Moudi S, Mohammadpour AR. Frequency and severity of obsessive-compulsivesymptoms/disorders, violence and suicidal in schizophrenic patients. Iranian Red Crescent Medical Journal. 2012;14:345–51. [PMC free article] [PubMed] [Google Scholar]
- 79.Iancu I, Bodner E, Roitman S, Piccone Sapir A, Poreh A, Kotler M, et al. Impulsivity, Aggression and Suicide Risk among Male Schizophrenia Patients. Psychopathology. 2010;43:223–9. doi: 10.1159/000313520. [DOI] [PubMed] [Google Scholar]
- 80.Jovanović N, Podlesek A, Medved V, Grubišin J, Mihaljevic-Peleš A, Goran T, et al. Association between psychopathology and suicidal behavior in schizophrenia: A cross-sectional study of509 participants. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2013;34:374–81. doi: 10.1027/0227-5910/a000211. [DOI] [PubMed] [Google Scholar]
- 81.Kao YC, Liu YP, Cheng TH, Chou MK. Subjective quality of life and suicidal behavior among Taiwanese schizophreniapatients. Social psychiatry and psychiatric epidemiology. 2012;47:523–32. doi: 10.1007/s00127-011-0361-0. [DOI] [PubMed] [Google Scholar]
- 82.Kibru B, Tesfaw G. The Prevalence and Correlates of Social Anxiety Symptoms among People with Schizophrenia inEthiopia: An Institution-Based Cross-Sectional Study. Early intervention in psychiatry. 2020;2020:3934680.. doi: 10.1155/2020/3934680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kim S-J, Mun J-W, Bae K-Y, Kim J-M, Kim S-Y, et al. Psychosocial factors contributing to suicidal ideation in hospitalized schizophrenia patients in Korea. Psychiatry investigation. 2010;7:79–85. doi: 10.4306/pi.2010.7.2.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Misiak B, Kiejna A, Frydecka D. Higher total cholesterol level is associated with suicidal ideation in first-episodeschizophrenia females. Psychiatry research. 2015;226:383–8. doi: 10.1016/j.psychres.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 85.Prokopez C, et al. The history of multiple adverse childhood experiences in patients with schizophrenia is associated withmore severe symptomatology and suicidal behavior with gender-specific characteristics. Archives of suicide research: official journal of the International Academy for Suicide Research. 2020;293:113411.. doi: 10.1016/j.psychres.2020.113411. [DOI] [PubMed] [Google Scholar]
- 86.Schwartz RC, Cohen BN. Psychosocial correlates of suicidal intent among patients with schizophrenia. Comprehensivepsychiatry. 2001;42:118–23. doi: 10.1053/comp.2001.21222. [DOI] [PubMed] [Google Scholar]
- 87.YildiZ M, Yazici A, Boke O. Demographic and Clinical Characteristics in Schizophrenia: A Multi Center Cross-sectionalCase Record Study. Turk Psikiyatri Dergisi. 2010;21:213–24. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.