Abstract
Superior capsule reconstruction (SCR) can be performed using fascia lata, dermal allograft, and long head of the biceps tendon (LHBT). We present a Technical Note combining dermal allograft and autologous LHBT, reconstructing the superior capsule’s actual anatomical thickness and augmenting with single-stranded LHBT. The glenoid side consists of intact LHBT insertion and is covered with dermal allograft. The lateral side comprises posteriorly transpositioned LHBT, dermal allograft, and repairable remnant cuff. First, 1 suture-based anchor is used to fix the biceps 5 to 8 mm posterior to the bicipital groove, and tenotomy is done distal to it, while the glenoid side of the biceps is preserved. Second, 2 suture-based anchors are used to fix the dermal allograft at the glenoid side by 1 double-pulley and 2 mattress sutures. Third, 2 SwiveLock anchors are used to fix allograft’s lateral side by 2 reverse mattress sutures. The tension and coverage of the graft can be determined by the position of the SwiveLock anchors. In this way, fewer anchors are needed than the conventional dermal allograft SCR and larger footprint coverage can be achieved than LHBT SCR. A better spacer effect may be achieved by combining both biological grafts’ thickness, mimicking the intact shoulder’s true anatomy.
Technique Video
This video demonstrates our preferred technique for arthroscopic capsular reconstruction with acetabular sided anchors for patients undergoing revision hip arthroscopy for capsular insufficiency. Before proceeding with this technique, it is essential to treat any other pathology in the central and peripheral compartment of the hip and ensure adequate capsular reduction to the acetabular rim to determine feasibility of repair.
Superior capsule reconstruction (SCR) was first introduced using fascia lata,1 continuously evolving with dermal allograft,2 and long head of the biceps tendon (LHBT),3 with different thicknesses, configurations, and related biomechanical properties.1,4, 5, 6 We propose a technical modification combining dermal allograft and autologous LHBT, reconstructing the superior capsule’s actual anatomical thickness, and augmenting with single-stranded LHBT. The glenoid side consists of intact LHBT insertion and is covered with dermal allograft. The lateral side comprises the posteriorly transpositioned LHBT, dermal allograft, and repairable remnant cuff.
Operative Technique (With Video Illustration)
Patient Preparation and Arthroscopic Portals
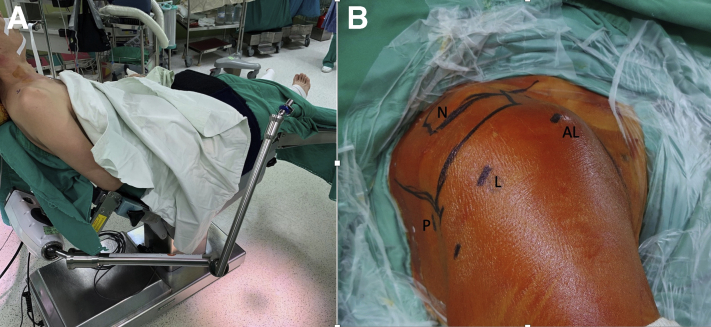
The indications and contraindications for an arthroscopic anatomical dermal allograft and autologous LHBT SCR are listed in Table 1. All patients receive general anesthesia with interscalene nerve block and are placed in the beach-chair position with a traction device (Fig 1A). Normally, 4 arthroscopic portals are necessary: posterior, lateral, anterolateral, and Neviaser (Fig 1B). If the subscapularis is torn and needs to be repaired, an additional anterior portal will be made.
Table 1.
The Indications and Contraindications for an Arthroscopic Anatomical Dermal Allograft and Autologous LHBT SCR
| Indications | |
| Irreparable posterosuperior massive rotator cuff tears with Hamada stage 2 or less | |
| The supraspinatus tendon is intraoperatively irreducible (Patte stage III) | |
| Preoperative good active and passive range of motion without external rotation lag sign, pseudoparalysis, or pseudoparesis | |
| Goutallier stage 3 or 4 muscle fatty infiltration | |
| Existing LHBT | |
| Contraindications | |
| Irreparable posterosuperior massive rotator cuff tears with Hamada stage 3 or greater | |
| Significant glenoid or humerus bone defects | |
| Absence of deltoid, latissimus dorsi, or pectoralis function | |
| Absent LHBT | |
| Shoulder stiffness |
LHBT, long head of the biceps tendon; SCR, superior capsule reconstruction.
Fig 1.
Patient position and arthroscopic portals, right shoulder. (A) All patients had general anesthesia with interscalene nerve block and were placed in the beach-chair position with a traction device. (B) Normally 4 arthroscopic portals are needed. (AL, anterolateral portal; L, lateral portal; N, Neviaser portal; P, posterior portal.)
SCR With LHBT
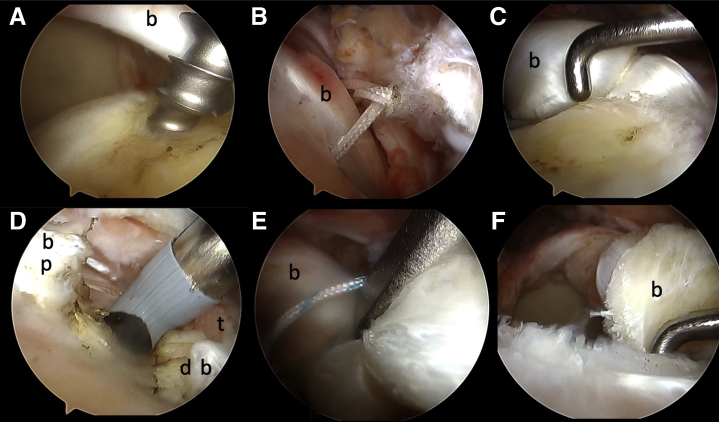
Viewing from lateral portal, a double-loaded or triple-loaded suture-based anchor is passed from anterolateral portal and inserted 5 to 8 mm posterior to the bicipital groove and near the cartilage of humerus (Fig 2A). We use a suture manipulator and Cuff Hook (Stryker, San Jose, CA) to perform 2 or 3 “lasso-loop” (Fig 2 B and C) according to the type of anchor used.1 In brief, one lasso-loop is made first. Then, the radiofrequency cautery device is used to cut the fixed biceps tendon at the entrance of the bicipital groove (Fig 2D) as biceps tenotomy, keeping the integrity of the transverse humeral ligament. No further tenodesis is performed regarding the distal part of the LHBT. The other sutures of the anchor will be used to finish the second and third lasso-loop. Tension of the LHBT can be made by penetrating the intra-articular LHBT in a more medial position by the second and third lasso-loop (Fig 2E). Finally, the proximal attachment of the biceps on the glenoid side is preserved, providing the native fixation. The lateral part of the LHBT is rerouted posteriorly, proving a strong spacer effect (Fig 2F).2
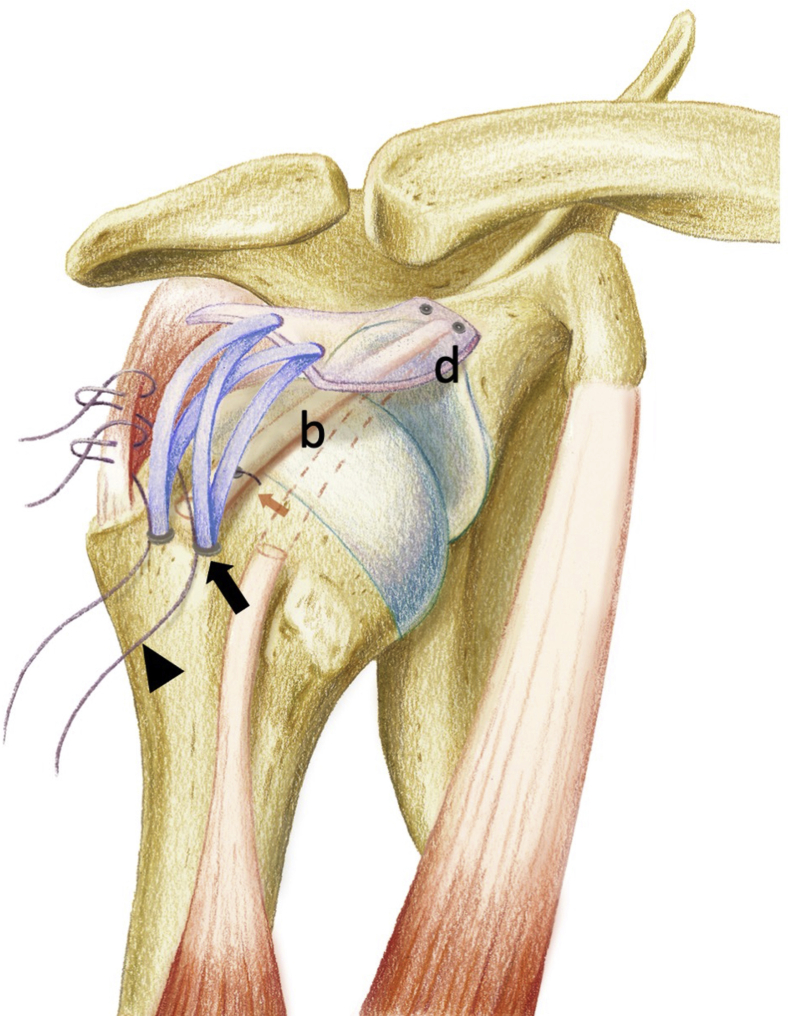
Fig 2.
Superior capsule reconstruction with long head of the biceps. Viewing from lateral portal, right shoulder. (A) A suture-based anchor is passed from anterolateral portal and inserted 5-8 mm posterior to the bicipital groove, and near the cartilage of humerus. (B-C) One lasso-loop is made and fixed provisionally. (D) A radiofrequency cautery device is used to cut the fixed biceps tendon at the entrance of the bicipital groove as biceps tenotomy, keeping the integrity of transverse humeral ligament. (E) Tension of the LHBT can be made by penetrating the intra-articular LHBT in a more medial position by the second and third lasso-loop. (F) The proximal attachment of the biceps on the glenoid side is preserved, providing the native fixation. The lateral part of the LHBT is rerouted posteriorly, proving a strong spacer effect. (b, biceps; d, distal part of biceps; LHBT, long head of the biceps tendon; p, proximal part of biceps; t, transverse ligament.)
Glenoid Preparation and Anchor Placement
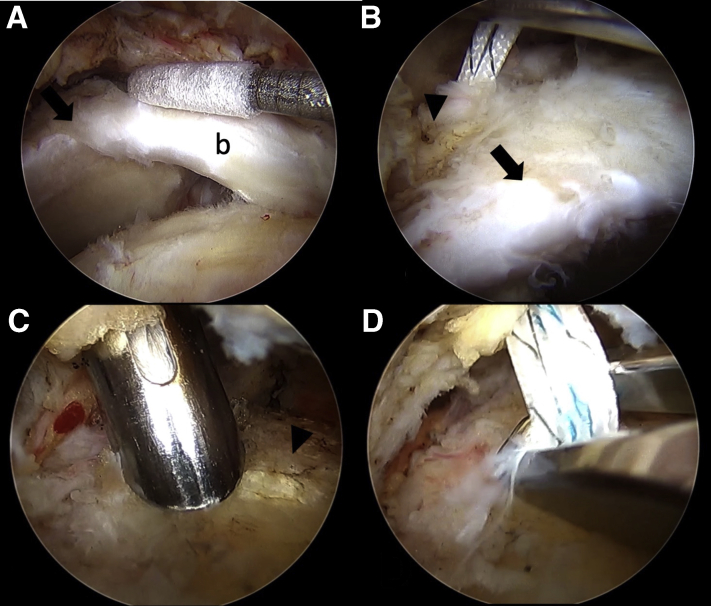
The bone bed on the superior glenoid is prepared to a bleeding surface. Care must be taken to preserve the proximal attachment of the LHBT on the glenoid, which is close to the native capsular attachment site. Unlike Burkhart et al.,3 who debrided and removed most of the meaningful bone attachments of the LHBT on the glenoid and created an unstable biceps root, the idea of the current technique is to maintain the intra-articular biceps tissue along with a dermal allograft, which will be covered on top of the intra-articular biceps autograft (Fig 3A). The anterosuperior glenoid anchor is placed at the coracoid base, just anteromedial to the origin of the LHBT. The posterosuperior glenoid anchor is placed at the posteromedial margin of the glenoid (Fig 3B). Both anchors are placed 3 mm medial to the corner of the glenoid to optimize the contact area between graft and bone and not penetrate the articular surface. Yet, they have to be lateral enough to avoid jeopardizing the suprascapular nerve. We use a Neviaser portal to introduce 2 anchors on the glenoid side. Double-loaded, all-suture anchors (1.8-mm Y-Knot Flex; CONMED Linvatec, Largo, FL) (Fig 3C) are preferred because of their flexibility during introduction into the glenohumeral joint. All sutures from the 2 glenoid anchors are then shuttled to the anterolateral portal for further usage (Fig 3D).
Fig 3.
Glenoid preparation and anchor placement. Viewing from lateral portal, right shoulder. (A) The intra-articular biceps tissue on the glenoid side is preserved. (B) The anterosuperior glenoid anchor is placed at the coracoid base, just anteromedial to the origin of the LHBT. The posterosuperior glenoid anchor is placed at the posteromedial margin of the glenoid. (C) Double-loaded, all suture anchors (1.8-mm Y-Knot Flex; CONMED Linvatec) are preferred because of their flexibility during introduction into the glenohumeral joint. (D) All sutures from the 2 glenoid anchors are shuttled to the anterolateral portal for further usage. Arrow, superior labrum; Arrowhead, glenoid. (b, biceps; LHBT, long head of the biceps tendon.)
Dermal Allograft Preparation
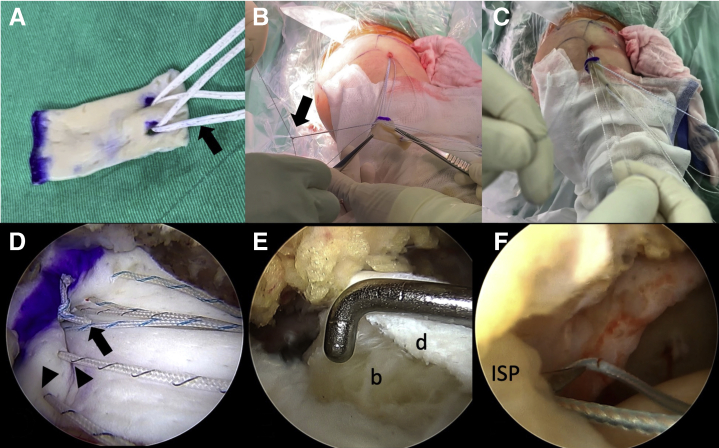
The size of the decellularized dermal allograft (LifeNet Health OrACELL, Virginia Beach, VA) is 2 × 4 cm with a thickness of 1.26 to 1.75 mm. A calibrated probe is used to measure the size of the defect spanning from the medial-to-lateral as well as anterior-to-posterior the distance between each pair of suture anchors. The graft is not cut, trying to provide as much soft-tissue coverage as possible. Four anchors (2 double-loaded anchors at glenoid side, and 2 BioComposite SwiveLock C anchors [Arthrex, Naples, FL] at greater tuberosity) are used to fix the dermal allograft. Two FiberTapes (Arthrex) are first retrieved from 2 SwiveLock C anchor, providing 2 reverse mattress sutures (Fig 4A).
Fig 4.
Preparation, shuttling, and fixation of the dermal allograft, right shoulder, viewing from lateral portal. (A) Two FiberTapes (Arthrex) are first retrieved from 2 SwiveLock C anchors, providing 2 reverse mattress sutures (arrow). (B) One double-pulley suture construct and 2 mattress sutures are made on the medial side of the dermal allograft from the sutures of the 2 glenoid anchors outside the joint (arrow). (C) The graft and all sutures are introduced into subacromial space by pulling the free ends of the 2 suture pairs of double-pulley until it touches the glenoid beds. (D) Viewing from lateral portal, 6-throw surgeon’s knots are made both for the double-pulley construct (arrow) and the 2 mattress sutures (arrowheads). (E) The combination of biceps and dermal allograft provides a thick biological spacer in the subacromial space. (F). The No. 2 FiberWire sutures from 2 SwiveLock anchors are used to repair the torn infraspinatus. (b, biceps; d, dermal allograft; ISP, infraspinatus.)
Shuttling and Fixation of the Dermal Allograft
Before the dermal allograft is introduced into the glenohumeral joint, 2 glenoid anchors are placed as mentioned previously. Unlike the technique proposed by Burkhart et al.,3 no medial row anchors are used in this technique. Instead, we use the SpeedFix method (Arthrex), avoiding too many anchors in the supraspinatus footprint’s enthesis. First, one double-pulley suture construct and 2 mattress sutures are made on the medial side of the dermal allograft from the sutures of the 2 glenoid anchors outside the joint (Fig 4B). The double-pulley suture will be used to bring the graft into the subacromial space. Second, the graft and all sutures (1 double-pulley and 2 mattress sutures medially, and 2 reverse mattress sutures with FiberTape laterally) are introduced into subacromial space by pulling the free ends of the 2 suture pairs of double-pulley until it touches the glenoid beds (Fig 4C). Once the graft is in contact with the superior glenoid, the 6-throw surgeon’s knot will be made by the knot pusher both for the double-pulley construct and the 2 mattress sutures (Fig 4D). Third, after 2 sockets are punched into the anterolateral and posterolateral greater tuberosity, the reverse mattress sutures are tensioned, and 2 SwiveLock anchors are placed into the bone socket fixing the sutures and graft. This completes the SpeedFix configuration on the lateral tuberosity. In this technique, the graft’s tension and coverage can be determined by the position of the 2 SwiveLock anchors. Normally, the posterior rerouted biceps tendon is now beneath the reconstructed dermal allograft. The combination of biceps and dermal allograft provides a thick biological spacer (the thickness of the biceps plus dermal allograft, Fig 4E) in the subacromial space. Fourth, the remaining No. 2 FiberWire sutures (Arthrex) from 2 SwiveLock anchors can be used to repair the torn infraspinatus or partially repair supraspinatus with lasso-loop4 stitches (Fig 4F). The infraspinatus tendon is not repaired with the dermal allograft’s posterior margin to prevent overtension of the graft and surrounding tissues. In general, the infraspinatus tendon will cover above the dermal allograft after fixing the lasso-loop sutures. The final construct is shown in Figure 5. The whole surgical procedure is shown in Video 1. The pearls and pitfalls of the surgical steps are shown in Table 2. The advantages, risks, and limitations of this technique are shown in Table 3.
Fig 5.
The final construct of anatomical dermal allograft and autologous biceps long head superior capsule reconstruction for irreparable posterosuperior rotator cuff tears, right shoulder. Two suture-based anchors are placed in the glenoid side to fix the medial border of the dermal allograft. One suture-based anchor is placed 5-8 mm posterior to the bicipital groove to fix the biceps as superior capsule reconstruction with the long head of the biceps. Two SwiveLock C anchors are used to fix the lateral part of the dermal allograft by fixing the 2 reverse mattress sutures (FiberTape, blue). Two No. 2 sutures from the SwiveLock C anchors can be used to repair the infraspinatus. (orange arrow, suture-based anchor used for biceps SCR; blank arrow, SwiveLock C anchor used to fix dermal allograft with FiberTape suture; arrowhead, FiberWire suture from SwiveLock C anchor, used to fix infraspinatus. (b, biceps; d, dermal allograft.).
Table 2.
Surgical Steps, Tips, Pearls, and Pitfalls of Described Technique
| Surgical Steps | Tips and Pearls | Pitfalls |
|---|---|---|
| Arthroscopic portals |
|
|
|
||
| SCR with LHBT |
|
|
|
||
|
||
|
||
|
||
|
||
|
||
| Glenoid preparation and anchor placement |
|
|
|
|
|
|
||
|
||
|
||
| Dermal allograft preparation |
|
|
|
||
|
||
| Shuttling and fixation of the dermal allograft |
|
|
|
|
|
|
||
|
||
|
||
|
LHBT, long head of the biceps tendon.
Table 3.
Advantages, Risks, and Limitations of Anatomical Dermal Allograft and Autologous Biceps Long Head SCR for Irreparable Posterosuperior Rotator Cuff Tears
| Advantages |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Risks |
|
|
|
|
|
|
|
| Limitations |
|
|
|
|
|
|
LHBT, long head of the biceps tendon; SCR, superior capsule reconstruction.
Discussion
The optimal graft choice of SCR is still controversial because of the potential donor-site morbidity, graft reactions, graft failures, and complex techniques.5 The advantages of autologous fascia lata SCR6 are the cost and thickness of the introduced graft. However, the thicker the graft, the more complex the surgical technique. Six suture anchors and a graft 6 to 8 mm thick are warranted for favorable outcomes. A PassPort cannula (Arthrex) or 10-mL syringe is needed to insert the graft into the subacromial space, causing additional cost and bigger wounds.7 The advantages of dermal allograft SCR3 are no donor-site morbidity and easier to introduce the thinner graft (from 1 to 3 mm).8 However, 6 anchors are still mandatory, and graft failures are common on the glenoidal side in allografts than with autografts.5 The other trend toward augmenting the massive irreparable rotator cuff using the autologous LHBT as a graft for SCR is appealing because it is available locally and free of additional costs, is less technically demanding, and provides an average thickness of LHBT comparable with the fascia lata graft. Another potential advantage of using the proximally attached LHBT is its remaining biological viability, which could avoid glenoidal graft failure and improve healing at the interface between the graft and the incorporated remnant rotator cuff.9
However, the quality of LHBT is not always adequate to provide a sufficient “spacer effect” because it is frequently absent or seriously degenerated in cases of chronic irreparable rotator cuff tears.10 Therefore, we developed a modified technique using both dermal allograft and LHBT to recreate a superior capsule. It may provide a better spacer effect by combing the thickness of LHBT and dermal allograft together. Fewer anchors are needed than a conventional dermal allograft. It also provides better footprint coverage than LHBT SCR alone. The glenoidal part of LHBT is preserved and will be covered by the glenoid part of the dermal allograft above. As the healing within homogeneous tissues (bone-to-bone or tendon-to-tendon) shows better healing quality than that taking place between the heterogeneous tissues (bone-to-tendon),11 this technique provides less failure both in the glenoidal and humeral side. In conclusion, we developed a technique to provide dermal allograft and LHBT SCR at the same time, with fewer anchors needed than conventional dermal allograft SCR and larger footprint coverage than LHBT SCR. A better spacer effect may be achieved by combining both biological grafts’ thickness, mimicking the true anatomy of the intact shoulder.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The whole surgical procedure. A 67-year-old female patient had a Patte 3 supraspinatus tear and grade 3 fatty infiltration with preserved cartilage and biceps. Two medial row suture-based anchors and 2 SwiveLock anchors are used to fix the 2-mm thick dermal allograft. We make 2 reverse mattress sutures on the lateral side of the graft by the FiberTapes from SwiveLock anchors. Viewing from the posterior portal, an irreparable posterosuperior cuff is confirmed. The biceps is mobile posteriorly. A suture-based anchor is inserted 5 mm posterior to the bicipital groove. One loop of the suture is made around the biceps and taken out the shoulder to make a loop. We use a Cuff Hook to penetrate the biceps and take the other limb of the suture. After the knot is tied, the biceps is posteriorly rerouted provisionally. Then, we cut the distal part of the knot, preserving the transverse humeral ligament. Care must be taken not to injure the subscapularis. The second suture can be passed through the biceps in the more medial part, providing extra tension. After fixing all knots, we can see the biceps is permanently and posteriorly rerouted, providing a good spacer in the subacromial space. Then, we insert 2 glenoid anchors through Neviaser portal, 3 mm medial to proximal biceps insertion on the glenoid. All-suture anchors are preferred because of the flexibility. After retrieving all sutures to the anterolateral portal, a probe is used to measure the defect size from glenoid to supraspinatus footprint. Make sure to tension the suture tapes in order not to strangulate them when knot tying. The final tension of the dermal allograft can be now, determined by where to put the 2 SwiveLock anchors. This method can provide stable glenoid fixation of the dermal allograft. Now the biceps lies beneath dermal allograft. Tensioning the reverse mattress sutures, 2 SwiveLock are then inserted into the greater tuberosity. After fixing the dermal allograft, it will lie above the posterior rerouted biceps, proving a good spacer effect because of the thickness of both grafts. Normally, it is larger than 8 mm. The infraspinatus can be repaired by the two No. 2 sutures from the SwiveLock anchors. Pulling the infraspinatus anteriorly, the huge cuff defect is covered by infraspinatus, dermal allograft, and biceps. Viewing from the glenohumeral joint, the gap of massive cuff tear is restored. The final construct of the whole procedure is shown in the illustration. In conclusion, we have developed a technique to provide dermal allograft and LHBT SCR at the same time. Fewer anchors are needed than conventional dermal allograft SCR. A larger footprint coverage can be achieved than LHBT SCR. A better spacer effect may be achieved by combining both biological grafts’ thickness, mimicking the true anatomy of the intact shoulder. (LHBT, long head of the biceps tendon; SCR, superior capsule reconstruction.)
References
- 1.Boutsiadis A., Chen S., Jiang C., Lenoir H., Delsol P., Barth J. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: "The Chinese Way". Arthrosc Tech. 2017;6:e1559–e1566. doi: 10.1016/j.eats.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh S., Reeves J., Langohr G.D.G., Johnson J.A., Athwal G.S. The subacromial balloon spacer versus superior capsular reconstruction in the treatment of irreparable rotator cuff tears: A biomechanical assessment. Arthroscopy. 2019;35:382–389. doi: 10.1016/j.arthro.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart S.S., Denard P.J., Adams C.R., Brady P.C., Hartzler R.U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: "The lasso-loop stitch. Arthroscopy. 2006;22 doi: 10.1016/j.arthro.2006.05.021. 1246.e1241-1243. [DOI] [PubMed] [Google Scholar]
- 5.Berthold D.P., Muench L.N., Dyrna F., et al. Comparison of different fixation techniques of the long head of the biceps tendon in superior capsule reconstruction for irreparable posterosuperior rotator cuff tears: A dynamic biomechanical evaluation. Am J Sports Med. 2021;49:305–313. doi: 10.1177/0363546520981559. [DOI] [PubMed] [Google Scholar]
- 6.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 7.Mihata T., Lee T.Q., Watanabe C., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 9.Denard P.J., Dai X., Hanypsiak B.T., Burkhart S.S. Anatomy of the biceps tendon: implications for restoring physiological length-tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28:1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 10.Pauzenberger L., Hurley E.T. Editorial Commentary: Finally, something positive about the long head of the biceps tendon?!—Shoulder superior capsular reconstruction. Arthroscopy. 2018;34:2601–2603. doi: 10.1016/j.arthro.2018.06.039. [DOI] [PubMed] [Google Scholar]
- 11.Leung K.S., Chong W.S., Chow D.H., et al. A comparative study on the biomechanical and histological properties of bone-to-bone, bone-to-tendon, and tendon-to-tendon healing: An Achilles tendon–calcaneus model in goats. Am J Sports Med. 2015;43:1413–1421. doi: 10.1177/0363546515576904. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates our preferred technique for arthroscopic capsular reconstruction with acetabular sided anchors for patients undergoing revision hip arthroscopy for capsular insufficiency. Before proceeding with this technique, it is essential to treat any other pathology in the central and peripheral compartment of the hip and ensure adequate capsular reduction to the acetabular rim to determine feasibility of repair.
The whole surgical procedure. A 67-year-old female patient had a Patte 3 supraspinatus tear and grade 3 fatty infiltration with preserved cartilage and biceps. Two medial row suture-based anchors and 2 SwiveLock anchors are used to fix the 2-mm thick dermal allograft. We make 2 reverse mattress sutures on the lateral side of the graft by the FiberTapes from SwiveLock anchors. Viewing from the posterior portal, an irreparable posterosuperior cuff is confirmed. The biceps is mobile posteriorly. A suture-based anchor is inserted 5 mm posterior to the bicipital groove. One loop of the suture is made around the biceps and taken out the shoulder to make a loop. We use a Cuff Hook to penetrate the biceps and take the other limb of the suture. After the knot is tied, the biceps is posteriorly rerouted provisionally. Then, we cut the distal part of the knot, preserving the transverse humeral ligament. Care must be taken not to injure the subscapularis. The second suture can be passed through the biceps in the more medial part, providing extra tension. After fixing all knots, we can see the biceps is permanently and posteriorly rerouted, providing a good spacer in the subacromial space. Then, we insert 2 glenoid anchors through Neviaser portal, 3 mm medial to proximal biceps insertion on the glenoid. All-suture anchors are preferred because of the flexibility. After retrieving all sutures to the anterolateral portal, a probe is used to measure the defect size from glenoid to supraspinatus footprint. Make sure to tension the suture tapes in order not to strangulate them when knot tying. The final tension of the dermal allograft can be now, determined by where to put the 2 SwiveLock anchors. This method can provide stable glenoid fixation of the dermal allograft. Now the biceps lies beneath dermal allograft. Tensioning the reverse mattress sutures, 2 SwiveLock are then inserted into the greater tuberosity. After fixing the dermal allograft, it will lie above the posterior rerouted biceps, proving a good spacer effect because of the thickness of both grafts. Normally, it is larger than 8 mm. The infraspinatus can be repaired by the two No. 2 sutures from the SwiveLock anchors. Pulling the infraspinatus anteriorly, the huge cuff defect is covered by infraspinatus, dermal allograft, and biceps. Viewing from the glenohumeral joint, the gap of massive cuff tear is restored. The final construct of the whole procedure is shown in the illustration. In conclusion, we have developed a technique to provide dermal allograft and LHBT SCR at the same time. Fewer anchors are needed than conventional dermal allograft SCR. A larger footprint coverage can be achieved than LHBT SCR. A better spacer effect may be achieved by combining both biological grafts’ thickness, mimicking the true anatomy of the intact shoulder. (LHBT, long head of the biceps tendon; SCR, superior capsule reconstruction.)