Abstract
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has imposed an unprecedented health care crisis across the globe. Health care efforts across the world have been diverted to tackling the pandemic since early 2020. Hospitals and health care systems have undertaken major restructuring in an effort to deliver health care to an increasing number of patients affected by COVID-19. Although great focus has been placed on treating those individuals suffering from COVID-19, clinicians must simultaneously balance caring for patients who are not actively infected. In anticipation of an exponential increase in COVID-19 cases, health care systems developed strategies to channel available resources to meet the rapidly rising demands of COVID-19. This change was noticed significantly in the field of invasive cardiology as well. Many cardiac catheterization and electrophysiology (EP) laboratories canceled elective procedures to limit the burden on hospital resources and preserve personal protective equipment (PPE). Major societies published guidance statements delineating patient selection for procedures during the exponential phase of the pandemic growth. Patient care was triaged and those waiting for elective procedures were managed with expectant care or noninvasive approaches to preserve hospital resources and personnel. In the current article, we review the impact of the COVID-19 pandemic and its response to the volume of interventional cardiology (IC) and EP procedures across the world.
Keywords: Interventional cardiology, Electrophysiology, Procedures, Volume, COVID-19
Key points
-
•
Volume of percutaneous coronary intervention has declined by >50% in the early phase of the pandemic across both North America and Europe.
-
•
Largest decline in electrophysiology procedures was noted in elective catheter ablation procedures such as atrial fibrillation ablations.
-
•
Universal preprocedural testing is an important part of safe resumption of elective procedures.
-
•
Being prepared for further surges and waves of COVID is crucial for uninterrupted delivery of health care.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has imposed an unprecedented health care crisis across the globe. Health care efforts across the world have been diverted to tackling the pandemic since early 2020. Hospitals and health care systems have undertaken major restructuring in an effort to deliver health care to an increasing number of patients affected by COVID-19. Although great focus has been placed on treating those individuals suffering from COVID-19, clinicians must simultaneously balance caring for patients who are not actively infected. In anticipation of an exponential increase in COVID-19 cases, health care systems developed strategies to channel available resources to meet the rapidly rising demands of COVID-19. This change was noticed significantly in the field of invasive cardiology as well. Many cardiac catheterization and electrophysiology (EP) laboratories canceled elective procedures to limit the burden on hospital resources and preserve personal protective equipment (PPE). Major societies published guidance statements delineating patient selection for procedures during the exponential phase of the pandemic growth.1 Patient care was triaged and those waiting for elective procedures were managed with expectant care or noninvasive approaches to preserve hospital resources and personnel. In the current article, we review the impact of the COVID-19 pandemic and its response to the volume of interventional cardiology (IC) and EP procedures across the world.
Impact on Interventional Cardiology Procedures
Onset of the COVID-19 pandemic led to immediate cessation of multiple clinical services in the field of interventional cardiology for better resource allocation and avoidance of potential exposure, across various countries. The British Cardiovascular Interventional society conducted a retrospective study of all percutaneous coronary interventions (PCI) in the United Kingdom during the lockdown imposed by the pandemic and compared them to PCI volumes in the prepandemic period.2 They showed that PCI volumes fell down by 49% with the greatest decrease in PCI for stable angina (66% reduction). PCI for ST-elevation MI (STEMI) was also down by 33%. Interestingly, the decline in volume was higher in older patients and in minorities. In another study from the United Kingdom, Mohamed and colleagues evaluated trends in all inpatient cardiac procedures to understand national trends during the lockdown period.3 Data on interventional cardiac catheterization, PCI, electrophysiological (CIED implantation, catheter ablation), structural (TAVR), and surgical (CABG, SAVR, MVR) procedures were collected and compared with trends in preceding years. Overall procedural volume fell down by approximately 89% in April and May 2020 during the lockdown, with cardiac catheterization and CIED implantation being the most affected. In addition, after adjusting for baseline comorbidities, patients undergoing PCI, and CIED implantation in the lockdown period had higher odds of mortality. A 24% reduction (29% for NSTEMI and 18% for STEMI) in overall PCI volume for acute MI was also reported from a multicenter analysis from Ireland.4
Despite prioritization of STEMI care, when other interventional services were limited during the lockdown, a reduction was seen in STEMI activations and primary PCI procedures being performed, partly related to patient’s reluctance to seek medical care during an ongoing pandemic. A single-center cross-sectional study from Germany reported a 50% reduction in admissions and primary PCI for acute MI during the early part of the pandemic than the prepandemic level.5 More importantly, patients presenting with an acute MI during the pandemic had symptoms for a longer duration, presented with lower LV ejection fraction, had more immediate complications and 3 times higher mortality than the prepandemic levels. Similar results have been reported from other European countries such as Italy and Portugal.6 , 7 A systematic review pooling data from 32 studies showed significantly prolonged door to balloon time and worse inpatient mortality for primary PCI for STEMI during the pandemic than prepandemic times.8 To better understand STEMI care during the pandemic, multicenter registries were developed. The International Study on Acute Coronary Syndromes–ST-Elevation Myocardial Infarction (ISACS-STEMI) registry included data from 6609 patients that underwent primary PCI at 77 hospitals in 18 European countries.9 There was a significant reduction in the volume of primary PCI in 2020 than in 2019, along with significantly longer door to balloon times, and higher in-hospital mortality. The NACMI (North American COVID-19 and STEMI) prospective registry was developed to track STEMI management trends in patients with COVID-19.10 This prospective multicenter study showed that patients with COVID-19 presenting with STEMI were less likely to receive primary PCI than controls and had higher rates of a composite of death, stroke, recurrent MI, and need for repeat revascularization.
Data on change in transcatheter aortic valve implantation volumes during the pandemic has been limited than studies evaluating PCI. Although experience from the United Kingdom showed no significant decline,3 a survey from Asia showed a 25% reduction in case of volume due to the pandemic.11
Impact on electrophysiology procedures
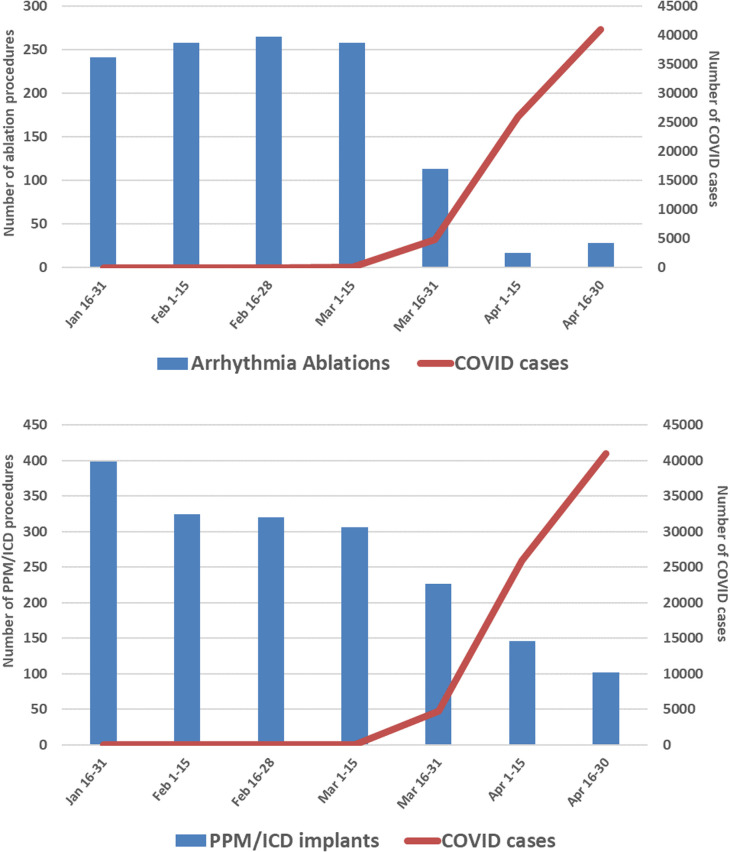
Response to the pandemic has also led to a reduction in EP procedures performed. During the surge of the pandemic, most EP programs only performed emergent procedures giving priority to ventricular tachycardia storms (ES), refractory device infections requiring lead/device extraction, urgent pacemaker and generator changes in PM-dependent patients A survey of 27 hospitals in the greater Philadelphia region evaluated the impact of COVID-19 on EP procedural volumes.12 Data on procedural volumes in this study were generated from manufacturer sales records. This study showed that the onset of COVID-19 cases in the geographic region was associated with a reduction in both catheter ablation and device implantation procedures (Fig. 1 ). Monthly arrhythmia ablation procedures decreased by 88.4% from a bi-weekly baseline of 241 procedures before the onset of the US COVID-19 outbreak to 28 in late April 2020. Similarly, pacemaker and implantable cardioverter-defibrillator procedures decreased by 74.4% (398–102 implants) over the same time interval.
Fig. 1.
Trends in EP procedural volumes in the greater Philadelphia region during the lockdown phase of the COVID-19 pandemic.
(From Pothineni NVK, Santangeli P, Deo R, Marchlinski FE, Hyman MC. COVID-19 and electrophysiology procedures-review, reset, reboot!!!. J Interv Card Electrophysiol. 2020;59(2):303-305. https://doi.org/10.1007/s10840-020-00871-2; with permission)
Li and colleagues evaluated EP procedural volumes at three centers during a surge of COVID-19 in China, Italy, and United Kingdom.13 In all three centers, all elective EP procedures were canceled with an overall volume being less than 5% of normal volumes. In addition, all EP personnel were deployed for delivering emergency care out of EP. Arbelo and colleagues reported a reduction in overall cardiac implantable electronic device (CIED) volumes in Spain as well during this period.14 In this study, data from 9 hospitals spanning 2017 to 2020 in the Catalonia province were aggregated. Compared with the pre–COVID-19 period, an absolute decrease of 56.5% was observed (54.7% in PM and 63.7% in ICD) in CIED implantation rates. Interestingly, there were no statistically significant differences in the type of PM or ICD implanted. An analysis of all cardiac procedures in the United Kingdom also revealed an 89% and 56% reduction in catheter ablation and CIED implantation procedures in April 2020 compared with similar time periods in preceding years.3 Similar reductions in CIED volumes from Germany and Italy have been reported as well.15 , 16
Resumption of procedures – precautions and universal testing
Following periods of lockdown in various geographic regions, the resumption of elective procedures presented a challenge. Although measures to screen for symptomatic individuals for COVID-19 were widely available, the risk of asymptomatic carriers transmitting the infection to health care workers and other patients remained. Several infection control precautions were undertaken at many centers to combat this risk. As more tests became available, universal testing of patients had led to a safer resumption of elective services.
A prospective study of universal testing of all patients undergoing interventional and EP procedures has provided insight into a strategy of safe resumptions of elective procedures.17 In this study conducted at the University of Pennsylvania, the following measures were instituted—universal surgical masks and temperature screening for all employees and patients, automated telephone preprocedure symptom screening for patients, strict restrictions on visitors for inpatients and outpatients, and universal preprocedure PCR testing to detect SARS-CoV-2 virus in patients undergoing elective or urgent procedures. Additional precautions to prevent cross-contamination were implemented at all feasible sites (Table 1 ). All in-patients undergoing cardiac catheterization or EP procedures underwent nasopharyngeal swabs for SARS-CoV-2 PCR testing performed at the hospital whereby the procedure was being performed. Outpatients were encouraged to undergo preprocedural testing at a satellite clinic 24 hours before the scheduled procedure to offload burden at the main hospital.
Table 1.
Representative example of precautions in the interventional and electrophysiology laboratories during the resumption of elective cases
| Risk | Proposed Measures |
|---|---|
| Coming and leaving in same scrubs Common computer Consent Contact |
It is prohibited to come to work and leave with the same scrubs. Only work on personal laptops. Avoid sharing of computers (keyboards – difficult to clean) Transition to verbal/e-consent PPE as needed (gloves/mask) |
| Collecting PPE Lead aprons Control room equipment Anesthesia recovery |
Individualized packs Wipe and store in personal space Wipe Prucka before and after the case. Wear gloves to operate Prucka. Wait in the control area, no computer work allowed |
| Provider contact Masking |
Limited provider contact unless absolutely necessary All patients with masks in recovery and transfer |
| Break room | Limited to 2 people at a time for social distancing |
Over a study period of 1 month, a total of 215 patients underwent 252 elective or urgent procedures (128 catheterization and 124 EP procedures). 56% of procedures were performed on outpatients. Among 111 outpatients, 53 (47.7%) underwent testing at an off-site facility. All catheterization procedures were performed under moderate sedation; 30.6% of EP procedures were conducted under general anesthesia. Of 215 patients tested, 2 (0.9%) tested positive for SARS-CoV-2. No patients who tested negative at the time of their procedure subsequently tested positive for SARS-CoV-2, and no staff members developed any symptoms concerning COVID-19 during the universal testing period. During a follow-up telephone survey, two-thirds of patients reported that preprocedural testing did not change their comfort level in getting the procedure performed, and the rest reported increased comfort.
Impact on trainees
Not surprisingly, reduction in procedural volumes during the COVID-19 pandemic has impacted the training of fellows enrolled in interventional and EP training programs. Singla and colleagues conducted a survey of all EP fellows and program directors in the United States to assess the impact of the pandemic on EP training and education.18 Out of 99 fellows that responded, 98% reported a decrease in their procedural volume and 55% of fellows reported a period of furlough or quarantine during the acute surge of COVID-19. A similar survey of 14 interventional cardiology programs in New York City also reported a significant reduction in catheterization procedures performed by fellows.19 In this survey, more than two-thirds of interventional program directors opined that the pandemic has moderately to severely impacted fellowship training. 21% felt that fellows would graduate without performing 250 percutaneous coronary interventions (PCI), which is considered a minimum cut-off for graduation. A third of fellows and program directors felt that fellowship training should be extended to those impacted by the pandemic. Shah and colleagues conducted a larger survey through the Society for Cardiovascular Interventions and Angiography to which 135 interventional fellows responded.20 By March 2020, only 43% of the respondents reported performing greater than 250 PCIs. With continued pandemic restrictions on elective procedures until the end of the fellowship, only 70% felt they would reach the minimum procedural volume cut-off for graduation. In addition to procedural volumes, trainees have also felt significant challenges due to the cancellation of in-person academic conferences and transition to purely web-based education. Job opportunities have dwindled down due to financial constraints imposed by the pandemic as well. Finally, the influence of the pandemic on fellow well-being cannot be ignored.21
Future preparedness
The development of a vaccine that is highly effective against moderate to severe COVID-19 has been a remarkable achievement. Increased vaccine uptake has led to a major reduction in hospitalizations for COVID-19 and enabled reopening to a state of near normalcy across the world. However, waves and surges of COVID-19 are expected to happen due to ongoing mutations in the virus and development of variants.22 For instance, the current delta variant leading to surges in some parts of the United States has led to a rapid rise in hospitalizations again, overwhelming health care resources in some hospitals.23 Although health care systems are more equipped to handle surges than the onset of the pandemic, these surges can lead to the cancellation of elective procedures again, impacting interventional and EP volumes as well. Lessons learnt from early 2020 can be used to better plan for effective and uninterrupted delivery of routine health care for chronic conditions, whereas handling the acute needs of an ongoing pandemic. There is no doubt that societal and governmental efforts to improve vaccine delivery and overall vaccination rates are pivotal to allow health care systems to effectively function.
Clinics care points
-
•
Evaluation of local variations in COVID 19 cases and prioritization of resources should be implemented in anticipation of surges of infection.
-
•
Remote monitoring of cardiac devices should be emphasized across all EP practices for better uninterrupted delivery of care in the event of further surges.
-
•
Routine preprocedural testing and safety measures such as masking and encouraging vaccination should be routinely implemented until the pandemic resolves.
-
•
Lessons learnt from the impact on procedures during the pandemic should be used for future planning.
Acknowledgments
Disclosure
None related to this article.
Footnotes
Funding Sources: None.
References
- 1.Lakkireddy D.R., Chung M.K., Gopinathannair R., et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Circulation. 2020 May 26;141(21):e823–e831. doi: 10.1161/CIRCULATIONAHA.120.047063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwok C.S., Gale C.P., Curzen N., et al. Impact of the COVID-19 pandemic on percutaneous coronary intervention in England: insights from the British Cardiovascular Intervention Society PCI Database Cohort. Circ Cardiovasc Interv. 2020;13(11):e009654. doi: 10.1161/CIRCINTERVENTIONS.120.009654. [DOI] [PubMed] [Google Scholar]
- 3.Mohamed M.O., Banerjee A., Clarke S., et al. Impact of COVID-19 on cardiac procedure activity in England and associated 30-day mortality. Eur Heart J Qual Care Clin Outcomes. 2021;7(3):247–256. doi: 10.1093/ehjqcco/qcaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connolly N.P., Simpkin A., Mylotte D., et al. Impact on percutaneous coronary intervention for acute coronary syndromes during the COVID-19 outbreak in a non-overwhelmed European healthcare system: COVID-19 ACS-PCI experience in Ireland. BMJ Open. 2021;11(4):e045590. doi: 10.1136/bmjopen-2020-045590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Primessnig U., Pieske B.M., Sherif M. Increased mortality and worse cardiac outcome of acute myocardial infarction during the early COVID-19 pandemic. ESC Heart Fail. 2021;8(1):333–343. doi: 10.1002/ehf2.13075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azul Freitas A., Baptista R., Gonçalves V., et al. Impact of SARS-CoV-2 pandemic on ST-elevation myocardial infarction admissions and outcomes in a Portuguese primary percutaneous coronary intervention center: preliminary data. Rev Port Cardiol. 2021;40(7):465–471. doi: 10.1016/j.repce.2021.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D'Ascenzo F., De Filippo O., Borin A., et al. Impact of COVID-19 pandemic and infection on in hospital survival for patients presenting with acute coronary syndromes: a multicenter registry. Int J Cardiol. 2021;332:227–234. doi: 10.1016/j.ijcard.2021.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chew N.W., Ow Z.G.W., Teo V.X.Y., et al. The global Effect of the COVID-19 pandemic on STEMI care: a systematic review and meta-analysis. Can J Cardiol. 2021;37(9):1450–1459. doi: 10.1016/j.cjca.2021.04.003. S0828-282X(21)00179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Luca G., Cercek M., Jensen L.O., et al. Impact of COVID-19 pandemic and diabetes on mechanical reperfusion in patients with STEMI: insights from the ISACS STEMI COVID 19 Registry. Cardiovasc Diabetol. 2020;19(1):215. doi: 10.1186/s12933-020-01196-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia S., Dehghani P., Grines C., et al. Initial findings from the North American COVID-19 myocardial infarction registry. J Am Coll Cardiol. 2021;77(16):1994–2003. doi: 10.1016/j.jacc.2021.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tay E.L., Hayashida K., Chen M., et al. Transcatheter aortic valve implantation during the COVID-19 pandemic: clinical expert opinion and consensus statement for Asia. J Card Surg. 2020;35(9):2142–2146. doi: 10.1111/jocs.14722. [DOI] [PubMed] [Google Scholar]
- 12.Pothineni N.V.K., Santangeli P., Deo R., et al. COVID-19 and electrophysiology procedures-review, reset, reboot. J Interv Card Electrophysiol. 2020;59(2):303–305. doi: 10.1007/s10840-020-00871-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li J., Mazzone P., Leung L.W.M., et al. Electrophysiology in the time of coronavirus: coping with the great wave. Europace. 2020;22(12):1841–1847. doi: 10.1093/europace/euaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arbelo E., Angera I., Trucco E., et al. Reduction in new cardiac electronic device implantations in Catalonia during COVID-19. Europace. 2021;23(3):456–463. doi: 10.1093/europace/euab011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bollmann A., Hohenstein S., Meier-Hellmann A., et al. On behalf of Helios hospitals Group. Emergency hospital admissions and interventional treatments for heart failure and cardiac arrhythmias in Germany during the Covid-19 outbreak: insights from the German-wide Helios hospital network. Eur Heart J Qual Care Clin Outcomes. 2020;6:221–222. doi: 10.1093/ehjqcco/qcaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Compagnucci P., Volpato G., Pascucci R., et al. Impact of the COVID-19 pandemic on a Tertiary-Level Electrophysiology Laboratory in Italy. Circ Arrhythm Electrophysiol. 2020;13(9):e008774. doi: 10.1161/CIRCEP.120.008774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pothineni N.V.K., Starkey S., Conn K., et al. Patient and staff perceptions of universal severe acute respiratory syndrome coronavirus 2 screening prior to cardiac catheterization and electrophysiology laboratory procedures. Circ Cardiovasc Interv. 2020;13(12):e009975. doi: 10.1161/CIRCINTERVENTIONS.120.009975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singla V.K., Jain S., Ganeshan R., et al. The impact of the COVID-19 pandemic on cardiac electrophysiology training: a survey study. J Cardiovasc Electrophysiol. 2021;32(1):9–15. doi: 10.1111/jce.14805. [DOI] [PubMed] [Google Scholar]
- 19.Gupta T., Nazif T.M., Vahl T.P., et al. Impact of the COVID-19 pandemic on interventional cardiology fellowship training in the New York metropolitan area: a perspective from the United States epicenter. Catheter Cardiovasc Interv. 2021;97(2):201–205. doi: 10.1002/ccd.28977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah S., Castro-Dominguez Y., Gupta T., et al. Impact of the COVID-19 pandemic on interventional cardiology training in the United States. Catheter Cardiovasc Interv. 2020;96(5):997–1005. doi: 10.1002/ccd.29198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kadavath S., Hawwas D., Strobel A., et al. How the COVID-19 pandemic has affected cardiology fellow training. Am J Cardiol. 2021;151:114–117. doi: 10.1016/j.amjcard.2021.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Planas D., Veyer D., Baidaliuk A., et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021 doi: 10.1038/s41586-021-03777-9. [DOI] [PubMed] [Google Scholar]
- 23.Available at: https://www.wsj.com/articles/u-s-covid-19-hospitalizations-rise-as-delta-variant-spreads-11625780656. Accessed July 22, 2021.