Abstract
Synovial chondromatosis is a benign metaplastic disease of the synovial joints, characterized by the development of cartilaginous nodules in the synovium. Treatment generally includes open or arthroscopic loose body removal combined with a synovectomy. An all-arthroscopic approach has been described to minimize complications and reduce morbidity while providing adequate control of local disease. The purpose of this Technical Note is to describe our techniques and technical pearls that allow for adequate excision of disease while minimizing complications and disease recurrence. The combination of patient positioning, the establishment of multiple arthroscopic portals to ensure optimal visualization and freedom of instruments, the use of a leg holder, and the use of a variety of surgical instruments to facilitate loose body removal and synovectomy is critical to optimize clinical outcomes and minimize complications. Although technically demanding, our described technique can help facilitate extensive loose body removal and complete synovectomy.
Technique Video
Surgical tips and techniques for systematic arthroscopic treatment of synovial chondromatosis of the knee. A case presentation outlining the clinical findings and relevant magnetic resonance imaging (sagittal and axial views) in a patient with this condition is provided. First, the relevant surface anatomy and the location of our arthroscopic portals are reviewed. Drainage of a significant knee effusion is then shown, whereby loose bodies can be found within the synovial fluid. A standard diagnostic arthroscopy is performed, and our technique of using multiple shavers, electrocautery, and various graspers to effectively remove embedded loose bodies within the synovium is described. To identify loose bodies and the nearby structures that must be protected, the compartments of the knee, intercondylar notch, and submeniscal regions are addressed. To access difficult regions of the knee, techniques such as shaving through the notch, using a modified Gillquist maneuver, and debriding with a trans-septal approach in the posterior aspect of the knee are reviewed. Finally, intraoperative images of our biopsy procedures and specimens are shown.
Synovial chondromatosis is a rare, benign metaplastic process of the synovial joints, characterized by the development of focal cartilage in the synovium and the formation of cartilaginous nodules.1,2 These nodules can detach from the synovium causing intra-articular loose bodies.3 Synovial chondromatosis is classified as primary or secondary. Primary synovial chondromatosis is an idiopathic, benign neoplastic process that predominantly affects male individuals in the third to fifth decade of life.2,3 Secondary synovial chondromatosis is characterized by metaplasia of synovial tissue into cartilaginous tissue without cytogenic aberrations. This form is typically associated with pre-existing degenerative, inflammatory, or traumatic pathology of the synovial joints.2,3 Milgram2 (1977) described 3 phases of proliferative changes: Phase 1 has active intrasynovial disease with no loose bodies, phase 2 has transitional lesions with active intrasynovial proliferation plus loose bodies, and phase 3 has several free osteochondral bodies with no intrasynovial disease.
Synovial chondromatosis can develop in any synovial joint but is most common in the knee, followed by the hip.2,3 Symptoms generally include pain, recurrent swelling, soft-tissue crepitus, locking, giving way, and palpable loose bodies.4 In the knee, loose bodies typically arise from diseased synovium in the anterior compartment (suprapatellar pouch, infrapatellar fat pad, and anterior interval); however, synovial disease can be diffuse and involve the posterior compartment.5,6
Treatment has been controversial but generally includes loose body removal combined with an open or arthroscopic synovectomy.4,6, 7, 8 Synovectomy has been recommended along with loose body removal because the recurrence rate is higher with loose body removal alone.4,7 With a delay in diagnosis and treatment, degenerative changes can occur within the knee, limiting management options.9,10 Arthroscopic loose body removal with synovectomy is associated with decreased morbidity compared with an open approach.11 Arthroscopic synovectomy allows diseased synovium to be identified accurately and removed without damage to macroscopically normal tissue.4 However, arthroscopic loose body removal with complete synovectomy is technically demanding and potentially dangerous given the proximity of the vessels to the posterior capsule.
Our technique for systematic arthroscopic excision for the treatment of synovial chondromatosis of the knee is described in this article and corresponding technique video (Video 1). This procedure allows for sufficient access and removal of disease in the vast majority of cases. Our aim is to describe techniques and technical pearls that allow for adequate excision of disease while minimizing complications and disease recurrence (Table 1).
Table 1.
Surgical Pearls and Pitfalls
| Pearls |
| The use of a leg holder increases access to various compartments by providing the ability to adjust the amount of knee flexion with control. |
| The establishment and use of multiple portals, including superomedial, superolateral, accessory posteromedial, and accessory posterolateral portals, are often required. |
| To visualize and debride difficult areas in the posteromedial and posterolateral compartments, adjusting the knee to varying degrees of flexion and extension can be beneficial. |
| The use of Kelly forceps, Kocher graspers, and surgical snaps provide more robust options for removal of the synovial tissue and loose bodies in comparison to standard arthroscopic graspers. |
| It is important to visualize the submeniscal and intercruciate regions because these are frequent areas of loose bodies and diseased tissue. However, care must be taken to avoid damage or detachment of the meniscus and cruciate ligaments. |
| Visualization through the posteromedial and posterolateral portals and debridement through the notch provide improved access for intercruciate disease. |
| The use of 3 shavers (4.5 mm, 5.5 mm, and curved) and a system that enables the easy transition from a 30° to 70° arthroscope ensures that all areas of varying difficulty are adequately visualized and debrided. |
| Pitfalls |
| Improper leg holder positioning or tourniquet placement can limit access and visualization throughout the procedure. |
| Inadequate visualization increases the risk of leaving symptomatic disease and recurrence. |
| Loose body removal and extensive debridement along the posterior condyles may be limited if the posterior portals are established too distal and close to the joint line. |
| The use of a single shaver risks inadequate debridement and remaining diseased synovium. Shavers often become blocked, which impacts surgical efficiency if only 1 shaver is used. |
Surgical Technique
Step 1: Patient Positioning and Setup
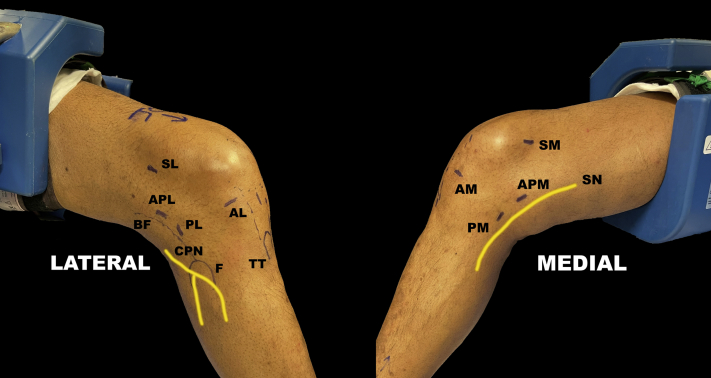
Once the patient has been safely anesthetized, he or she is positioned supine with a high tourniquet. The operative leg is placed into the leg holder (Acufex; Smith & Nephew, Andover, MA) that is secured proximally to ensure anterior and posterior access to the knee, as well as adequate room for instrument manipulation, and to maximize the flexion angle throughout the operation. The foot of the bed is lowered, and the contralateral leg is positioned in a lithotomy boot with the hip and knee flexed to less than 90° and in slight hip abduction. The surface anatomy of the knee is then identified, and the surgical portals are marked accordingly (Fig 1). In addition to standard anteromedial and anterolateral portals, superomedial, superolateral, posteromedial, posterolateral, accessory posteromedial, and accessory posterolateral portals are identified and marked. Posterolateral and accessory posterolateral portals are marked anterior to the biceps femoris tendon to prevent iatrogenic injury to the common peroneal nerve. Optional accessory portals include a transpatellar tendon portal, which is particularly useful to place instruments between the cruciate ligaments. Accessory anterior superolateral and superomedial portals are also useful with extensive disease in the suprapatellar pouch.
Fig 1.
Surface anatomy and portal placement in right knee. The patient is positioned supine with the use of a leg holder. Views from both the lateral and medial aspects of the right knee are shown. (AL, anterolateral; AM, anteromedial; APL, accessory posterolateral; APM, accessory posteromedial; BF, biceps femoris; CPN, common peroneal nerve; F, fibula; PL, posterolateral; PM, posteromedial; SL, superolateral; SM, superomedial; SN, saphenous nerve; TT, tibial tuberosity).
Step 2: Anterior Loose Body Removal and Synovectomy
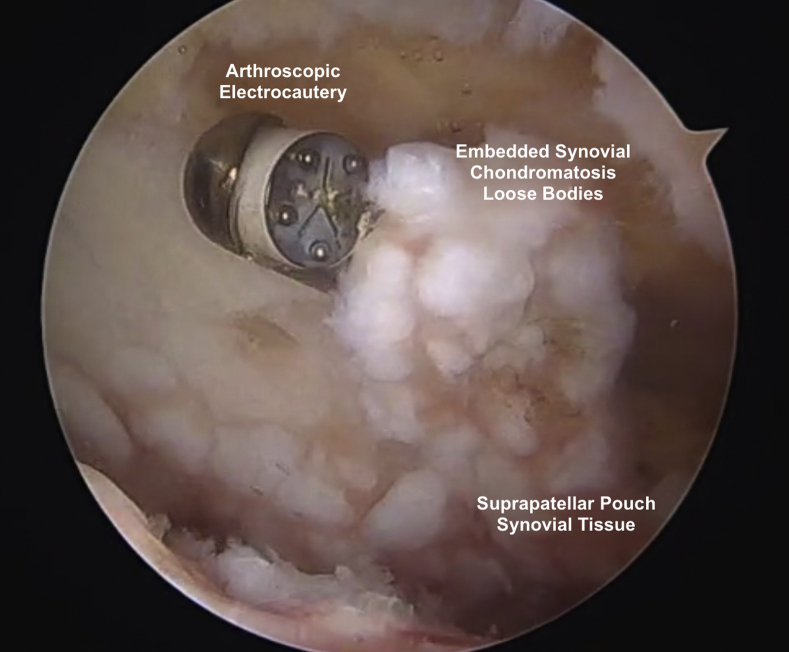
A No. 11 blade is used to establish standard anteromedial and anterolateral portals. The effusion, often accompanied by a number of loose bodies, is drained through the sheath of the arthroscope. Superomedial and superolateral portals are established to ensure adequate outflow and to be used as additional viewing and working portals. Additional proximal accessory portals may be necessary if there is chronic disease extending proximally in the suprapatellar pouch. A standard diagnostic arthroscopy is performed using a 30° arthroscope, and initial biopsy specimens are obtained. A systematic debridement is then conducted to improve visualization and optimize working space. This begins in the suprapatellar pouch before both the medial and lateral gutters are addressed. Cycling between surgical instruments and using all established portals as both viewing and working portals ensure that all areas are visualized, loose bodies are removed, and synovectomy is performed. For areas that are difficult to access, a 70° arthroscope and curved shaver (Dyonics 4.5-mm Curved Incisor Plus Elite Blade; Smith & Nephew) are frequently required. Smaller loose bodies can be removed with shavers. It is useful, if not necessary, to have multiple shavers (Fig 2) with different diameters and curves to access difficult areas and to exchange shavers when blocked (Dyonics 5.5-mm Full Radius Blade, Platinum Series [Smith & Nephew]; Dyonics 4.5-mm Incisor Plus Blade, Platinum Series [Smith & Nephew]; and Dyonics 4.5-mm Curved Incisor Plus Elite Blade). Larger loose bodies are removed using a combination of arthroscopic graspers, hemostat forceps, Kelly forceps, and Kocher graspers. Loose bodies are often embedded in the synovium; the synovium can be released with a shaver or arthroscopic cautery and removed with a Kocher grasper (Fig 3).
Fig 2.
Multiple shavers are used to ensure adequacy of debridement: (1) Dyonics 5.5-mm Full Radius Blade, Platinum Series; (2) Dyonics 4.5-mm Incisor Plus Blade, Platinum Series; and (3) Dyonics 4.5-mm Curved Incisor Plus Elite Blade.
Fig 3.
Arthroscopic view from standard anterolateral portal in right knee. Synovial tissue found within the suprapatellar pouch is often embedded with loose bodies. A combination of arthroscopic shavers and electrocautery can be used to release this tissue, which can then be removed with a Kelly forceps or Kocher grasper.
Step 3: Establishment of Posteromedial Portals and Posteromedial Synovectomy
The modified Gillquist maneuver is used to access the posteromedial compartment between the medial femoral condyle and posterior cruciate ligament (PCL).12 The arthroscope is placed through the anteromedial portal without the arthroscope sheath. The trocar and arthroscopic sheath are passed under direct visualization through the anterolateral portal between the medial femoral condyle and PCL. The trocar can then be removed, and the arthroscope can be inserted through the sheath into the posteromedial compartment. An outside-in technique is used to establish a posteromedial portal. Care must be taken to ensure that the portal is not positioned too posteriorly to minimize risk to the saphenous nerve and vein. A spinal needle is used to localize portal placement posterior to the medial femoral condyle and proximal to the joint line. A No. 11 or 15 blade is used to cut skin only, and a straight hemostat is used to follow the trajectory of the spinal needle and bluntly dissect into the posteromedial compartment. An accessory posteromedial portal, typically made more proximally, is often necessary to provide additional access for both viewing and debridement. Viewing through the posteromedial portal while working posteriorly through the notch is often helpful. Cycling between 30° and 70° arthroscopes and the use of both anterolateral (to place arthroscope or curved shaver posteromedially) and posteromedial portals help facilitate adequate removal of loose bodies and thorough synovectomy. A surgical assistant can adjust the knee flexion angle to allow for surgical instruments to reach challenging areas such as the superior aspect of the posterior compartment. Intercruciate loose bodies can be removed by inserting surgical instruments through a transpatellar tendon portal. Using both straight and curved shavers while viewing from the posteromedial (or posterolateral) portal is helpful in this scenario.
Step 4: Establishment of Posterolateral Portals and Posterolateral Synovectomy
The posterolateral compartment is accessed using the modified Gillquist maneuver between the lateral femoral condyle and the anterior cruciate ligament.12 An outside-in technique is again used to establish a posterolateral portal. It is important to place the spinal needle proximal to the joint line and anterior to the biceps femoris tendon to avoid injury to the common peroneal nerve. A second accessory posterolateral portal is frequently required to improve visualization and maximize instrument maneuverability. Again, a 70° arthroscope and a combination of shavers, hemostats, and Kelly forceps are often required to ensure adequate loose body removal and synovectomy.
Step 5: Trans-septal Posterior Approach
To address the synovial chondromatosis centrally in the posterior compartment, a trans-septal approach is used to ensure adequate resection. The posteromedial compartment can be visualized through the notch using a 70° arthroscope. With the knee flexed to displace the popliteal artery posteriorly, a shaver inserted through the posteromedial portal is then used to work from medial to lateral until it falls through the septum. It is critical to stay against the posteromedial femoral condyle under direct vision until this occurs (Fig 4). To ensure that the neurovascular bundle is protected, the septum is perforated at the distal portion, just posterior to the PCL with the knee in a position of flexion. Once the septum is perforated, it is helpful to work through the posteromedial portals and view through the posterolateral portals and vice versa (Fig 5).
Fig 4.
Arthroscopic view from posterolateral portal in right knee. A trans-septal approach is used by inserting the shaver through the posteromedial portal and debriding from medial to lateral.
Fig 5.
A trans-septal approach can be used to debride the posterior aspect of the right knee. It is helpful to use the posteromedial portal for debridement and the posterolateral portal for viewing or vice versa.
Discussion
Synovial chondromatosis is a rare, benign metaplastic process of the synovial joints, characterized by the development of focal cartilage in the synovium and the formation of cartilaginous nodules.1,2 Prompt diagnosis and adequate treatment are paramount; a delay in initial diagnosis—or inadequate initial treatment—can result in significant degenerative changes.9,10 Total knee arthroplasty has been performed to improve patients’ pain and function in the setting of end-stage degenerative disease but is associated with a high complication rate.10
Although controversy remains over the optimal treatment, it generally includes loose body removal combined with an open or arthroscopic synovectomy.4,6, 7, 8 Synovectomy has been recommended along with loose body removal because the recurrence rate is higher with loose body removal alone.4,7 Traditional open synovectomy requires an extensive posterior approach and may lead to persistent joint stiffness and prolonged rehabilitation.4 This is often combined with an arthroscopic anterior synovectomy and loose body removal to provide complete access in disseminated disease.4 A comprehensive all-arthroscopic approach has been described to minimize complications and reduce postoperative morbidity while providing adequate control of local disease.4,7,8,13 Although an all-arthroscopic approach is technically demanding, the technical pearls described in this article can help facilitate extensive loose body removal and complete synovectomy while minimizing complications and recurrent disease.
To reduce the potential for recurrence, removal of loose bodies along with synovectomy has been recommended.2,7 Ogilvie-Harris and Saleh7 (1994) compared arthroscopic removal of loose bodies alone versus arthroscopic removal with synovectomy. Patients undergoing isolated arthroscopic loose body removal had a recurrence rate of 60% (3 of 5) compared with 0% of patients (0 of 8) who underwent concurrent loose body excision and synovectomy. The authors recommended close follow-up in patients treated with isolated loose body excision and a low threshold for subsequent synovectomy in the setting of recurrence. Adjuvant radiotherapy has also been proposed in the setting of recurrent disease; however, there is limited evidence supporting its use and efficacy.14
Owing to difficulty in accessing the posterior compartment arthroscopically, open approaches have traditionally been used to excise loose bodies of the posterior compartment.15,16 For arthroscopic treatment of posterior disease, the use of accessory posterior portals and a trans-septal technique has been described to provide adequate surgical access while protecting the popliteal neurovascular bundle.6 Release of the posterior capsule and knee flexion greater than 90° are required to protect the vessels.6 A trans-septal technique is useful in the setting of disease present within the pouch of the posterior septum or near the septum to ensure adequate exposure and freedom of surgical instruments. An arthroscopic system that allows for easy exchange between 30° and 70° arthroscopes, such as a sterile camera head or arthroscope drape that facilitates quick camera exchange, is helpful to improve visualization.
Systematic arthroscopic treatment of synovial chondromatosis of the knee is technically demanding but can be replicated by following the steps in this article. Positioning the patient with a proximally placed leg holder to facilitate various degrees of knee flexion, establishing multiple portals to ensure optimal visualization and freedom of surgical instruments, and using multiple surgical instruments to facilitate loose body removal and synovectomy are critical to optimize clinical outcomes and minimize complications.
Footnotes
L.J.W. and T.M.H. contributed equally to this work.
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical tips and techniques for systematic arthroscopic treatment of synovial chondromatosis of the knee. A case presentation outlining the clinical findings and relevant magnetic resonance imaging (sagittal and axial views) in a patient with this condition is provided. First, the relevant surface anatomy and the location of our arthroscopic portals are reviewed. Drainage of a significant knee effusion is then shown, whereby loose bodies can be found within the synovial fluid. A standard diagnostic arthroscopy is performed, and our technique of using multiple shavers, electrocautery, and various graspers to effectively remove embedded loose bodies within the synovium is described. To identify loose bodies and the nearby structures that must be protected, the compartments of the knee, intercondylar notch, and submeniscal regions are addressed. To access difficult regions of the knee, techniques such as shaving through the notch, using a modified Gillquist maneuver, and debriding with a trans-septal approach in the posterior aspect of the knee are reviewed. Finally, intraoperative images of our biopsy procedures and specimens are shown.
References
- 1.McCarthy C., Anderson W.J., Vlychou M., et al. Primary synovial chondromatosis: A reassessment of malignant potential in 155 cases. Skeletal Radiol. 2016;45:755–762. doi: 10.1007/s00256-016-2353-3. [DOI] [PubMed] [Google Scholar]
- 2.Milgram J.W. Synovial osteochondromatosis: A histopathological study of thirty cases. J Bone Joint Surg Am. 1977;59:792–801. [PubMed] [Google Scholar]
- 3.Singh S., Neelakandan K., Sood C., Krishnan J. Disseminated synovial chondromatosis of the knee treated by open radical synovectomy using combined anterior and posterior approaches. J Clin Orthop Trauma. 2014;5:157–160. doi: 10.1016/j.jcot.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coolican M.R., Dandy D.J. Arthroscopic management of synovial chondromatosis of the knee. Findings and results in 18 cases. J Bone Joint Surg Br. 1989;71:498–500. doi: 10.1302/0301-620X.71B3.2722947. [DOI] [PubMed] [Google Scholar]
- 5.Bozkurt M., Ugurlu M., Dogan M., Tosun N. Synovial chondromatosis of four compartments of the knee: Medial and lateral tibiofemoral spaces, patellofemoral joint and proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2007;15:753–755. doi: 10.1007/s00167-006-0249-9. [DOI] [PubMed] [Google Scholar]
- 6.Kyung B.S., Lee S.H., Han S.B., Park J.H., Kim C.H., Lee D.H. Arthroscopic treatment of synovial chondromatosis at the knee posterior septum using a trans-septal approach: Report of two cases. Knee. 2012;19:732–735. doi: 10.1016/j.knee.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Ogilvie-Harris D.J., Saleh K. Generalized synovial chondromatosis of the knee: A comparison of removal of the loose bodies alone with arthroscopic synovectomy. Arthroscopy. 1994;10:166–170. doi: 10.1016/s0749-8063(05)80088-x. [DOI] [PubMed] [Google Scholar]
- 8.Shpitzer T., Ganel A., Engelberg S. Surgery for synovial chondromatosis. 26 cases followed up for 6 years. Acta Orthop Scand. 1990;61:567–569. doi: 10.3109/17453679008993585. [DOI] [PubMed] [Google Scholar]
- 9.Ackerman D., Lett P., Galat D.D., Jr., Parvizi J., Stuart M.J. Results of total hip and total knee arthroplasties in patients with synovial chondromatosis. J Arthroplasty. 2008;23:395–400. doi: 10.1016/j.arth.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 10.Houdek M.T., Wyles C.C., Rose P.S., Stuart M.J., Sim F.H., Taunton M.J. High rate of local recurrence and complications following total knee arthroplasty in the setting of synovial chondromatosis. J Arthroplasty. 2017;32:2147–2150. doi: 10.1016/j.arth.2017.02.040. [DOI] [PubMed] [Google Scholar]
- 11.Sim F.H. Synovial proliferative disorders: Role of synovectomy. Arthroscopy. 1985;1:198–204. doi: 10.1016/s0749-8063(85)80012-8. [DOI] [PubMed] [Google Scholar]
- 12.Lee J.Y., Chia Z.Y., Jiang L., Ang B., Chang P. A review of the Gillquist maneuver: Modifications for a safer and easily reproducible approach for knee transintercondylar notch posterior compartment arthroscopy. Arthrosc Tech. 2020;9:e435–e438. doi: 10.1016/j.eats.2019.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dorfmann H., De Bie B., Bonvarlet J.P., Boyer T. Arthroscopic treatment of synovial chondromatosis of the knee. Arthroscopy. 1989;5:48–51. doi: 10.1016/0749-8063(89)90091-1. [DOI] [PubMed] [Google Scholar]
- 14.Chong C.C., Kneebone A., Kirsh G. Radiotherapy in the management of recurrent synovial chondromatosis. Australas Radiol. 2007;51:95–98. doi: 10.1111/j.1440-1673.2006.01669.x. [DOI] [PubMed] [Google Scholar]
- 15.Mubashir A., Bickerstaff D.R. Synovial osteochondromatosis of the cruciate ligament. Arthroscopy. 1998;14:627–629. doi: 10.1016/s0749-8063(98)70062-3. [DOI] [PubMed] [Google Scholar]
- 16.Church J.S., Breidahl W.H., Janes G.C. Recurrent synovial chondromatosis of the knee after radical synovectomy and arthrodesis. J Bone Joint Surg Br. 2006;88:673–675. doi: 10.1302/0301-620X.88B5.17579. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical tips and techniques for systematic arthroscopic treatment of synovial chondromatosis of the knee. A case presentation outlining the clinical findings and relevant magnetic resonance imaging (sagittal and axial views) in a patient with this condition is provided. First, the relevant surface anatomy and the location of our arthroscopic portals are reviewed. Drainage of a significant knee effusion is then shown, whereby loose bodies can be found within the synovial fluid. A standard diagnostic arthroscopy is performed, and our technique of using multiple shavers, electrocautery, and various graspers to effectively remove embedded loose bodies within the synovium is described. To identify loose bodies and the nearby structures that must be protected, the compartments of the knee, intercondylar notch, and submeniscal regions are addressed. To access difficult regions of the knee, techniques such as shaving through the notch, using a modified Gillquist maneuver, and debriding with a trans-septal approach in the posterior aspect of the knee are reviewed. Finally, intraoperative images of our biopsy procedures and specimens are shown.
Surgical tips and techniques for systematic arthroscopic treatment of synovial chondromatosis of the knee. A case presentation outlining the clinical findings and relevant magnetic resonance imaging (sagittal and axial views) in a patient with this condition is provided. First, the relevant surface anatomy and the location of our arthroscopic portals are reviewed. Drainage of a significant knee effusion is then shown, whereby loose bodies can be found within the synovial fluid. A standard diagnostic arthroscopy is performed, and our technique of using multiple shavers, electrocautery, and various graspers to effectively remove embedded loose bodies within the synovium is described. To identify loose bodies and the nearby structures that must be protected, the compartments of the knee, intercondylar notch, and submeniscal regions are addressed. To access difficult regions of the knee, techniques such as shaving through the notch, using a modified Gillquist maneuver, and debriding with a trans-septal approach in the posterior aspect of the knee are reviewed. Finally, intraoperative images of our biopsy procedures and specimens are shown.