Abstract
Background
Inducible ischaemia is a strong marker of vascular vulnerability. Knowing the important role of the vascular tropism of COVID-19 to explain its severity, the presence of a prior inducible ischaemia may be a key pathogenetic determinant of COVID-19 severity.
Aims
To investigate the prognostic value of prior inducible ischaemia on stress cardiovascular magnetic resonance (CMR) to predict death in patients hospitalized for COVID-19.
Methods
We retrospectively analysed consecutive patients referred for stress perfusion CMR during 1/1/18–1/1/20 who were later hospitalized for COVID-19. The primary outcome was all-cause death, including in-hospital and post-hospitalization deaths, based on the electronic national death registry.
Results
Among the patients referred for stress CMR, 481 were hospitalized for COVID-19 (mean age 68.4 ± 9.6 years, 61.3% male) and completed the follow-up (median [interquartile range] 73 [36–101] days). There were 93 (19.3%) all-cause deaths, of which 13.7% occurred in hospital and 5.6% were post-hospitalization deaths. Age, male sex, hypertension, diabetes, known coronary artery disease (CAD), the presence of prior inducible ischaemia, the number of ischaemic segments, the presence of late gadolinium enhancement and left ventricular ejection fraction were significantly associated with all-cause death. In multivariable stepwise Cox regression analysis, age (hazard ratio [HR]: 1.04, 95% confidence interval [CI]: 1.01–1.07; P = 0.023), hypertension (HR: 2.77; 95% CI: 1.71–4.51; P < 0.001), diabetes (HR: 1.72; 95% CI: 1.08–2.74; P = 0.022), known CAD (HR: 1.78; 95% CI: 1.07–2.94; P = 0.025) and prior inducible ischaemia (HR 2.05; 95% CI: 1.27–3.33; P = 0.004) were independent predictors of all-cause death.
Conclusions
In COVID-19 patients, prior inducible ischaemia by stress CMR during the 2 years preceding the COVID-19 pandemic was independently associated with all-cause death.
Keywords: COVID-19, SARS-CoV-2, Cardiovascular magnetic resonance, Stress testing, Ischaemia
Résumé
Contexte
L’ischémie inductible est décrite comme un puissant marqueur de vulnérabilité vasculaire. Connaissant l’implication majeure du tropisme vasculaire du COVID-19 pour expliquer sa gravité clinique, la présence d’une ischémie inductible préalablement détectée pourrait être un déterminant pathogénique clé de la gravité du COVID-19.
Objectifs
Étudier la valeur pronostique d’une ischémie inductible détectée par imagerie de résonance magnétique (IRM) cardiovasculaire de stress dans les 2 ans précédents afin de prédire le décès chez des patients hospitalisés pour COVID-19.
Méthodes
Nous avons analysé rétrospectivement des patients consécutifs ayant subi une IRM cardiaque de stress entre le 1/1/2018 et le 1/1/2020 avant une hospitalisation pour infection à la COVID-19. Le critère de jugement principal était le décès toutes causes défini par le registre national électronique des décès, et comprenant les décès survenus à l’hôpital et après l’hospitalisation.
Résultats
Parmi les patients référés pour une IRM cardiovasculaire de stress, 481 ont été hospitalisés pour COVID-19 (âge moyen 68,4 ± 9,6 ans, 61,3 % d’hommes) et ont terminé le suivi (médiane [IQR] de 73 [36–101] jours). Il y a eu 93 (19,3 %) décès toutes causes, dont 13,7 % de décès à l’hôpital et 5,6 % de décès post-hospitalisation. L’âge, le sexe masculin, l’hypertension, le diabète, une maladie coronaire connue, la présence d’une ischémie inductible dans les 2 dernières années, le nombre de segments ischémiques, la présence d’une cicatrice myocardique et la fraction d’éjection ventriculaire gauche ont été significativement associés aux décès toutes causes. Dans l’analyse multivariée de Cox, l’âge (hazard ratio [HR] : 1,04, IC95 % : 1,01–1,07 ; p = 0,023), l’hypertension (HR : 2,77, IC95 % : 1,71–4,51 ; p < 0,001), le diabète (HR : 1,72, IC95 % : 1,08–2,74 ; p = 0,022), une maladie coronaire connue (HR : 1,78, IC95 % : 1,07–2,94 ; p = 0,025) et la présence d’une ischémie inductible dans les 2 dernières années (HR : 2,05, IC95 % : 1,27–3,33 ; p = 0,004) étaient des prédicteurs indépendants de décès toutes causes.
Conclusions
Chez les patients hospitalisés pour COVID-19, une ischémie inductible détectée par IRM cardiovasculaire de stress au cours des 2 dernières années précédant l’hospitalisation pour COVID-19 était indépendamment associée à la mortalité toute cause.
Mots clés: COVID-19, SARS-CoV-2, IRM cardiovasculaire, Test de stress, Ischémie
Background
The entire world has been profoundly affected by the COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), leading to a public health crisis of unprecedented magnitude [1]. SARS-CoV-2 not only affects the lungs, but also profoundly impacts the cardiovascular system, possibly mediated by alterations of the angiotensin-converting enzyme system [2]. Indeed, the cardiovascular effects of COVID-19 are key components of the disease, including direct myocardial injury [3], [4], [5], vascular endothelial inflammation associated with arterial and venous thromboembolism [6], [7], [8] and cardiac death [9]. Libby and Lüscher summarized this crucial role of the vascular tropism of COVID-19 in an impactful viewpoint [10]. Indeed, the endothelium plays a critical regulatory role in coagulation, inflammation, oxidative stress, vascular permeability and vasoactive functions. Several studies have shown the prognostic value of coagulation abnormalities [7], [11] and inflammation in COVID-19 patients [6]. Endothelial damage results in the dysregulation of these functions and is a cornerstone in the pathogenesis of severe forms of COVID-19 [10]. Accordingly, severe COVID-19 is more frequent in patients with cardiovascular disease (CVD), including coronary artery disease (CAD) [12], [13], [14].
Stress perfusion cardiovascular magnetic resonance (CMR) imaging has emerged as an accurate technique to assess the presence of myocardial ischaemia [15], [16]. The presence of inducible ischaemia is a powerful marker of vascular vulnerability [15], [17], [18], [19], [20], and is associated with morphological and functional alterations of the endothelial vasodilator/vasoconstrictor balance [21], portending a strong prognostic value [16], [22]. We hypothesized that the identification of inducible myocardial ischaemia in the months preceding a COVID-19 infection could help to stratify the severity of COVID-19.
This study aimed to investigate the prognostic value of prior inducible ischaemia on vasodilator stress perfusion CMR to predict death in patients hospitalized for COVID-19.
Methods
Study population
Among patients referred for vasodilator stress perfusion CMR between 1 January 2018 and 1 January 2020 at our European Association of Cardiovascular Imaging (EACVI)-accredited CMR laboratory, we conducted a single centre longitudinal study with retrospective enrolment of consecutive patients hospitalized with a diagnosis of COVID-19 infection between 24 January 2020 (first case in France) and 30 June 2020. All patients referred for stress perfusion CMR between 1 January 2018 and 1 January 2020 were contacted directly or through their referring cardiologist to determine whether they had been hospitalized between 24 January and 30 June 2020. Medical reports were collected from the corresponding hospitals between 24 January and 30 July 2020.
As recommended by the World Health Organization, COVID-19 diagnosis was confirmed when the real-time reverse transcription polymerase chain reaction (RT–PCR) of nasal/pharyngeal swabs (or lower respiratory tract aspirates) were positive, or when chest computed tomography (CT) showed typical imaging characteristics in case of negative or inconclusive RT–PCR. Exclusion criteria for stress CMR examination have been previously published [17], [18], [19]. Baseline clinical data were collected from the medical report including medical history and clinical examination during hospitalization. Early coronary revascularization was defined as either coronary artery bypass grafting or percutaneous coronary intervention performed within 90 days after the CMR examination.
Informed written consent was obtained from all patients. The study was approved by the local ethics committee of our institution, was conducted in accordance with the Declaration of Helsinki and follows the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) reporting guideline.
Clinical outcomes
The primary outcome was all-cause death, including in-hospital and post-hospitalization deaths. The secondary outcomes were in-hospital death and post-hospitalization deaths. Death was identified using the electronic Institut National de la Statistique et des Études Économiques (French National Registry of Death).
CMR protocol and image analysis
The detailed stress CMR protocol has been previously published [17], [18], [19], [23], and is described in Text A.1. Left ventricular (LV) volumes and function were quantified on the short-axis cine stack (Syngo.via, Siemens Healthcare). Stress perfusion and late gadolinium enhancement (LGE) images were evaluated according to the 17-segment model of the American Heart Association [24]. The analysis of perfusion images was performed visually by one experienced cardiologist prior to the COVID-19 pandemic who was blinded to clinical and follow-up data. Prior inducible ischaemia was defined as a subendocardial perfusion defect that:
-
•
occurred in at least one myocardial segment;
-
•
persisted for at least three phases beyond peak contrast enhancement;
-
•
followed a coronary distribution;
-
•
occurred in the absence of co-location with LGE [15].
Prior myocardial infarction was defined by LGE with subendocardial or transmural distribution. The segment was considered viable if the LGE thickness was < 50% of the myocardial wall. The ischaemic burden was assessed using the number of ischaemic segments without taking into account the transmurality of the defect. The quantitative extent of LGE in the LV myocardium was automatically determined by a signal intensity > 5 standard deviations (SDs) above remote normal myocardium, manually adjusted and then summed over the entire LV myocardium to determine LGE as a percentage of the LV mass.
Statistical analysis
Continuous data are reported as means ± SDs for normally distributed data or as medians and interquartile ranges (IQRs) for non-normally distributed data, as assessed through graphical methods and the Shapiro–Wilk test for normality. The statistical significance of differences between patients with and without prior inducible ischaemia were calculated using the Student's t-test (for normally distributed data) or the Mann–Whitney test (for non-normally distributed data) for continuous variables, and the Pearson's Chi2 or Fisher's exact test for categorical variables. Cumulative incidence rates of all-cause death were estimated using the Kaplan–Meier method and compared with the log-rank test. Cox proportional hazards methods were used to identify the predictors of all-cause death among patients with and without prior inducible ischaemia. The assumption of proportional hazard ratio (HR) was visually assessed using Schoenfeld residuals. Martingale residuals were used to detect nonlinearity in continuous variables. Collinearity of variables tested in the multivariable model was assessed using the variance inflation factor (considered excessive if > 5) (Table A.1). The multivariable model for adjustment used a stepwise forward Cox regression strategy to select the strongest parsimonious set of clinical covariates for all-cause death, with a P-value ≤ 0.1 on univariable screening. In competitive risk analysis, cumulative incidence functions were used to display the proportion of patients with the event of interest or the competing event as time progressed, and the Fine and Gray regression model was used to measure the subdistribution hazard. A two-tailed P-value < 0.05 was considered statistically significant. Statistical analysis was performed using R software, version 3.3.1 (R Project for Statistical Computing).
Results
Study population
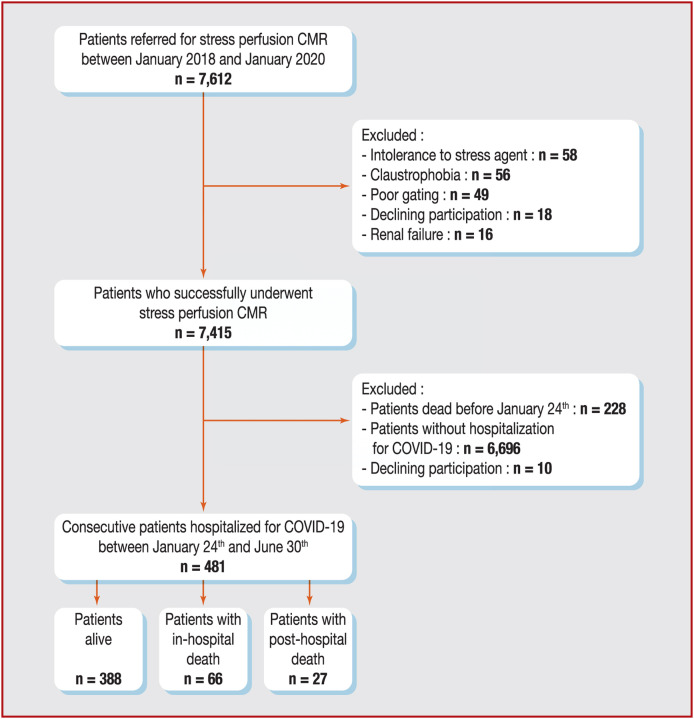
The flowchart of the study participants is depicted in Fig. 1 . Of 7415 patients who successfully completed stress CMR, 228 (3.1%) died before 24 January 2020, 6696 (90.3%) were excluded due to the absence of hospitalization for COVID-19 and 10 (0.1%) declined to participate. Baseline characteristics of the screened and excluded populations are described in Table A.2. Detailed safety results are presented in Text A.2.
Figure 1.
Flowchart of the study patients. CMR: cardiovascular magnetic resonance.
Overall, 481/7415 patients (6.5%) hospitalized for COVID-19 constituted our study cohort. Among those, 404 patients (84.0%) were SARS-CoV-2 RT–PCR positive and 382 patients (79.4%) presented typical COVID-19 findings on chest CT images. Patient characteristics and CMR data are presented in Table 1 . Among the 481 patients (mean age 68.4 ± 9.6 years, 61.3% male), 39.5% had hypertension, 23.3% diabetes and 10.2% were obese. Of note, 44.5% of patients had known CAD, 10.0% a history of atrial fibrillation (AF) and 2.7% hospitalization for heart failure. The overall study cohort had a mean left ventricular ejection fraction (LVEF) of 50.7% ± 11.3. LGE was detected in 178 patients (37.0%), and the presence of prior inducible ischaemia was identified in 74 patients (15.4%). Among the 178 patients with LGE, 172 (96.6%) had ischaemic LGE distribution and only 6 (3.4%) had non-ischaemic (non-subendocardial) LGE distribution. The median (IQR) time between the depiction of prior inducible ischaemia and hospitalization for COVID-19 was 11 (6–14) months. Patients with prior inducible ischaemia were significantly older (72.6 ± 6.9 vs. 67.7 ± 9.8 years) and more frequently had hypertension (73.0% vs. 33.4%), known CAD (64.9% vs. 40.8%) and history of AF (21.6% vs. 7.9%) (all P < 0.001) than patients without prior inducible ischaemia. The prevalence of LGE was also higher in patients with versus without inducible ischaemia (60.8% vs. 32.7%; P < 0.001). Of the 74 patients with inducible ischaemia, 58 (78.4%) underwent coronary angiography and revascularization within 90 days after CMR. Overall, 48/58 patients underwent ‘complete’ revascularization within 90 days of CMR.
Table 1.
Baseline and CMR characteristics of patients hospitalized for COVID-19 without and with prior inducible myocardial ischaemia.
| All hospitalized COVID-19 patients (n = 481) |
No prior inducible ischaemia (n = 407) |
Prior inducible ischaemia (n = 74) |
P | |
|---|---|---|---|---|
| Age (years) | 68.4 ± 9.6 | 67.7 ± 9.8 | 72.6 ± 6.9 | < 0.001 |
| Males | 295 (61.3) | 247 (60.7) | 48 (64.9) | 0.58 |
| BMI (kg/m2) | 27.7 ± 5.3 | 27.8 ± 5.5 | 27.2 ± 4.0 | 0.24 |
| Cardiovascular risk factors | ||||
| Diabetes | 112 (23.3) | 90 (22.1) | 22 (29.7) | 0.20 |
| Hypertension | 190 (39.5) | 136 (33.4) | 54 (73.0) | < 0.001 |
| Dyslipidaemia | 66 (13.7) | 39 (9.6) | 27 (36.5) | < 0.001 |
| Current or previous smoking | 101 (21.0) | 88 (21.6) | 13 (17.6) | 0.53 |
| Family history of CAD | 147 (30.6) | 132 (32.4) | 15 (20.3) | 0.051 |
| Obesitya | 49 (10.2) | 40 (9.8) | 9 (12.2) | 0.69 |
| Medical history of CVD | ||||
| Known CAD | 214 (44.5) | 166 (40.8) | 48 (64.9) | < 0.001 |
| Previous PCI | 199 (41.4) | 160 (39.3) | 39 (52.7) | 0.043 |
| Previous CABG | 4 (0.8) | 1 (0.2) | 3 (4.1) | 0.013 |
| Known myocardial infarction | 89 (18.5) | 75 (18.4) | 14 (18.9) | 1.00 |
| Peripheral atheroma | 43 (8.9) | 33 (8.1) | 10 (13.5) | 0.20 |
| Ischaemic stroke | 26 (5.4) | 20 (4.9) | 6 (8.1) | 0.27 |
| Pacemaker | 2 (0.4) | 0 (0.0) | 2 (2.7) | 0.023 |
| Renal failureb | 2 (0.4) | 2 (0.5) | 0 (0.0) | 1.00 |
| History of HF hospitalization | 13 (2.7) | 11 (2.7) | 2 (2.7) | 1.00 |
| History of AF | 48 (10.0) | 32 (7.9) | 16 (21.6) | < 0.001 |
| Indications for stress CMR (multiple possible) | ||||
| High cardiovascular riskc | 273 (56.8) | 215 (52.8) | 58 (78.4) | < 0.001 |
| Symptomatic angina | 87 (18.1) | 71 (17.4) | 16 (21.6) | 0.49 |
| Dyspnoea | 111 (23.1) | 99 (24.3) | 12 (16.2) | 0.17 |
| Inconclusive stress test | 108 (22.5) | 99 (24.3) | 9 (12.2) | 0.031 |
| Inconclusive CCTAd | 34 (7.1) | 34 (8.4) | 0 (0.0) | 0.020 |
| PCI or CABG control | 203 (42.2) | 161 (39.6) | 42 (56.8) | 0.009 |
| Cardiac rhythm | < 0.001 | |||
| Sinus rhythm | 431 (89.6) | 374 (91.9) | 57 (77.0) | |
| AF/supraventricular arrhythmias | 50 (10.4) | 33 (8.1) | 17 (23.0) | |
| LVEF (%) | 50.7 ± 11.3 | 50.3 ± 11.5 | 52.7 ± 10.1 | 0.069 |
| LV end-diastolic volume index (mL/m2) | 79.7 ± 21.8 | 80.3 ± 22.0 | 76.8 ± 20.8 | 0.19 |
| LV end-systolic volume index (mL/m2) | 39.2 ± 17.0 | 39.9 ± 16.9 | 35.3 ± 17.4 | 0.038 |
| LV mass (g/m2) | 74.6 ± 7.1 | 74.7 ± 7.1 | 74.5 ± 7.2 | 0.62 |
| RVEF (%) | 56.6 ± 11.4 | 56.3 ± 11.3 | 58.2 ± 12.9 | 0.33 |
| LGE | 178 (37.0) | 133 (32.7) | 45 (60.8) | < 0.001 |
| LGE with viabilitye | 58 (12.1) | 34 (8.4) | 24 (32.4) | < 0.001 |
| Number of LGE segments | 0.9 ± 1.5 | 0.8 ± 1.4 | 1.7 ± 1.9 | < 0.001 |
| LGE mass (% of LV mass) | 5.8 ± 8.9 | 5.1 ± 8.6 | 9.8 ± 12.1 | < 0.001 |
| Number of ischaemic segments | 0.4 ± 1.1 | 0.0 ± 0.0 | 2.5 ± 1.7 | < 0.001 |
| Heart rate at baseline (bpm) | 68 ± 12 | 68 ± 12 | 70 ± 13 | 0.71 |
| Heart rate at stress (bpm) | 80 ± 9 | 80 ± 9 | 83 ± 11 | 0.57 |
| RPP at baseline (mmHg × bpm) | 8.9 (7.3–10.4) | 8.9 (7.3–10.4) | 9.1 (7.5–11.0) | 0.62 |
| RPP at stress (mmHg × bpm) | 10.5 (9.1–12.5) | 10.4 (9.0–12.4) | 10.9 (9.5–12.8) | 0.39 |
| Early revascularization < 3 months after CMR | 58 (12.1) | 0 (0.0) | 58 (78.4) | < 0.001 |
Data are expressed as n (%), mean ± SD or median (IQR).
AF: atrial fibrillation; BMI: body mass index; CABG: coronary artery bypass grafting; CAD: coronary artery disease; CCTA: coronary computed tomography angiography; CMR: cardiac magnetic resonance; CVD: cardiovascular disease; HF: heart failure; IQR: interquartile range; LGE: late gadolinium enhancement; LV: left ventricular; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; RPP: rate-pressure product (systolic blood pressure [mmHg] × heart rate [bpm])/1000; RVEF: right ventricular ejection fraction; SD: standard deviation.
Defined by BMI ≥ 30 kg/m2.
Defined by glomerular filtration rate < 60 mL/min/1.73 m2.
Defined by Framingham Risk Score > 20% risk of CAD at 10 years.
Defined by coronary stenosis of unknown significance on CCTA.
Defined by LGE with < 50% transmurality.
Primary and secondary outcomes
After a median (IQR) follow-up of 73 (36–101) days following hospitalization for COVID-19, the all-cause death rate was 19.3%. Among the 481 patients hospitalized for COVID-19, 66 patients died in hospital (13.7%). The median (IQR) delay between admission and in-hospital death was 6 (3–9) days and the median length of hospitalization was 7 (5–13) days. Of the 415 patients who were discharged alive from the hospital, 27 died after discharge (6.5%). The median (IQR) time between discharge and death was 29 (18–60) days. Baseline characteristics of patients by death status are described in Table A.3.
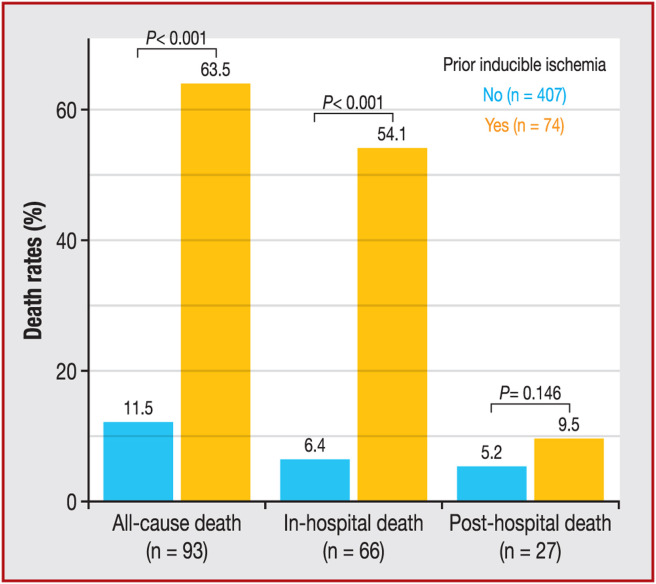
The rate of all-cause death was significantly higher among patients with versus without prior inducible ischaemia (63.5% vs. 11.5%; P < 0.001; Fig. 2 ). The in-hospital death rate was also higher among patients with versus without inducible ischaemia (54.1% vs. 6.4%; P < 0.001; Fig. 2).
Figure 2.
Death rates (all-cause, in-hospital and post-hospital) stratified by presence/absence of prior inducible ischaemia.
Among the 6706 patients excluded patients who were still alive after 24 January 2020, 94 (1.4%) died between 24 January and 31 July 2020.
Prognostic value of inducible myocardial ischaemia among COVID-19 patients
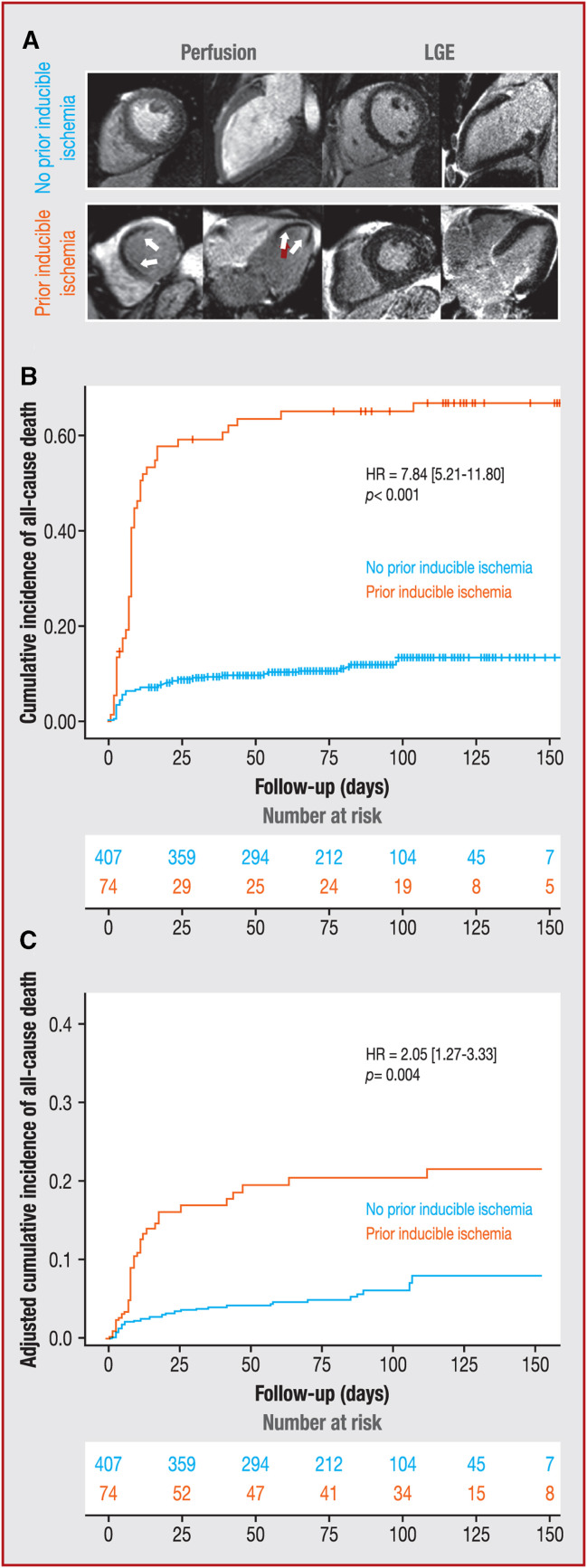
The univariable analysis of baseline individuals and CMR characteristics for the prediction of all-cause death is presented in Table 2 . Age, male sex, hypertension, diabetes, known CAD, presence and number of segments with inducible ischaemia, presence of LGE and LVEF were significantly associated with all-cause death. Using Kaplan–Meier analysis, the presence of prior inducible ischaemia (HR: 7.84, 95% CI: 5.21–11.80; P < 0.001; Fig. 3 A, B) and LGE (HR: 1.56, 95% CI: 1.04–2.34; P = 0.032; Table 2) were associated with the occurrence of all-cause death and.
Table 2.
Univariable analysis of clinical and CMR characteristics for all-cause death (n = 481).
| HR (95% CI) | P | |
|---|---|---|
| Age (per 1-year increase) | 1.08 (1.05–1.11) | < 0.001 |
| Male sex | 1.75 (1.09–2.79) | 0.019 |
| BMI (per 1-kg/m2 increase) | 0.96 (0.90–1.01) | 0.056 |
| Obesity | 0.60 (0.28–1.30) | 0.20 |
| Hypertension | 4.35 (2.77–6.85) | < 0.001 |
| Diabetes | 1.94 (1.27–2.97) | 0.002 |
| Dyslipidaemia | 1.26 (0.75–2.12) | 0.38 |
| Current or previous smoking | 0.84 (0.49–1.42) | 0.51 |
| Family history of CAD | 0.78 (0.49–1.23) | 0.28 |
| Renal failure | 4.13 (0.57–29.80) | 0.16 |
| History of hospitalization for HF | 1.45 (0.45–4.59) | 0.53 |
| History of AF | 1.48 (0.85–2.57) | 0.17 |
| Known CAD | 1.98 (1.30–3.02) | 0.001 |
| Known myocardial infarction | 0.89 (0.51–1.54) | 0.67 |
| Prior inducible myocardial ischaemia | 7.84 (5.21–11.80) | < 0.001 |
| Number of segments of prior myocardial ischaemia (per 1-segment increase) | 1.43 (1.31–1.56) | < 0.001 |
| LGE | 1.56 (1.04–2.34) | 0.032 |
| Number of segments of LGE (per 1-segment increase) | 1.08 (0.96–1.21) | 0.20 |
| LGE mass (% of LV mass) | 1.09 (0.96–1.24) | 0.19 |
| LVEF (per 5% increase) | 0.69 (0.61–0.79) | < 0.001 |
| LV end-diastolic volume index (per 10 mL/m2 increase) | 1.26 (0.73–2.18) | 0.40 |
| RVEF (per 5% increase) | 0.92 (0.75–1.15) | 0.49 |
| Early revascularization < 3 months after CMR | 1.26 (0.78–2.04) | 0.34 |
AF: atrial fibrillation; BMI: body mass index; CAD: coronary artery disease; CI: confidence interval; CMR: cardiac magnetic resonance; HF: heart failure; HR: hazard ratio; LGE: late gadolinium enhancement; LV: left ventricular; LVEF: left ventricular ejection fraction; RVEF: right ventricular ejection fraction.
Figure 3.
A. Examples of recent stress CMR scans in patients hospitalized for COVID-19: top panel: 52-year-old male with diabetes and hypertension; stress CMR revealed no perfusion defect and no LGE, ruling out a diagnosis of CAD; bottom panel: 69-year-old female with diabetes and obesity referred for atypical chest pain; stress CMR showed a subendocardial perfusion defect of the antero-septal wall on first-pass perfusion images (white arrows) without myocardial scar on LGE, indicative of inducible myocardial ischaemia; coronary angiography revealed a high-grade stenosis of the LAD. B and C. Kaplan–Meier curves for all-cause death stratified by the presence of prior inducible ischaemia in B. univariable analysis and C. after adjustment. CAD: coronary artery disease; CI: confidence interval; CMR: cardiovascular magnetic resonance; HR: hazard ratio; LAD: left anterior descending; LGE: late gadolinium enhancement.
In the multivariable stepwise Cox regression (Table 3 ), age (HR: 1.04, 95% CI: 1.01–1.07; P = 0.023), hypertension (HR: 2.77, 95% CI: 1.71–4.51; P < 0.001), diabetes (HR: 1.72, 95% CI: 1.08–2.74; P = 0.022), known CAD (HR: 1.78, 95% CI: 1.07–2.94; P = 0.025) and the presence of prior inducible ischaemia (HR: 2.05, 95% CI: 1.27–3.33; P = 0.004; Fig. 3C) were independently associated with all-cause death. In addition, prior inducible ischaemia remained independently associated with all-cause death after adjustment for early revascularization (HR: 1.67, 95% CI: 1.03–2.66; P = 0.041).
Table 3.
Multivariable Cox regression analysis for all-cause death (n = 481).
| HR (95% CI) | P | |
|---|---|---|
| Model 1a | ||
| Age (per 1-year increase) | 1.04 (1.01–1.07) | 0.023 |
| Male sex | 1.35 (0.78–2.33) | 0.23 |
| BMI (per 1-kg/m2 increase) | 0.93 (0.86–1.00) | 0.054 |
| Hypertension | 2.77 (1.71–4.51) | < 0.001 |
| Diabetes | 1.72 (1.08–2.74) | 0.022 |
| Known CAD | 1.78 (1.07–2.94) | 0.025 |
| LVEF (per 5% increase) | 1.07 (0.95–1.21) | 0.25 |
| LGE | 1.43 (0.89–2.28) | 0.14 |
| Prior inducible myocardial ischaemia | 2.05 (1.27–3.33) | 0.004 |
| Model 2b | ||
| Early revascularization within 90 days after CMR | 1.20 (0.58–2.37) | 0.51 |
| Prior inducible myocardial ischaemia | 1.67 (1.03–2.66) | 0.041 |
BMI: body mass index; CAD: coronary artery disease; CI: confidence interval; CMR: cardiac magnetic resonance; HR: hazard ratio; LGE: late gadolinium enhancement; LVEF: left ventricular ejection fraction.
Covariates in model 1 by stepwise variable selection with entry and exit criteria set at the P ≤ 0.1 level: age, male, BMI, hypertension, diabetes, known CAD, LVEF, presence of LGE and prior inducible myocardial ischaemia.
Covariates in model 2: model 1 + early revascularization within 90 days after CMR.
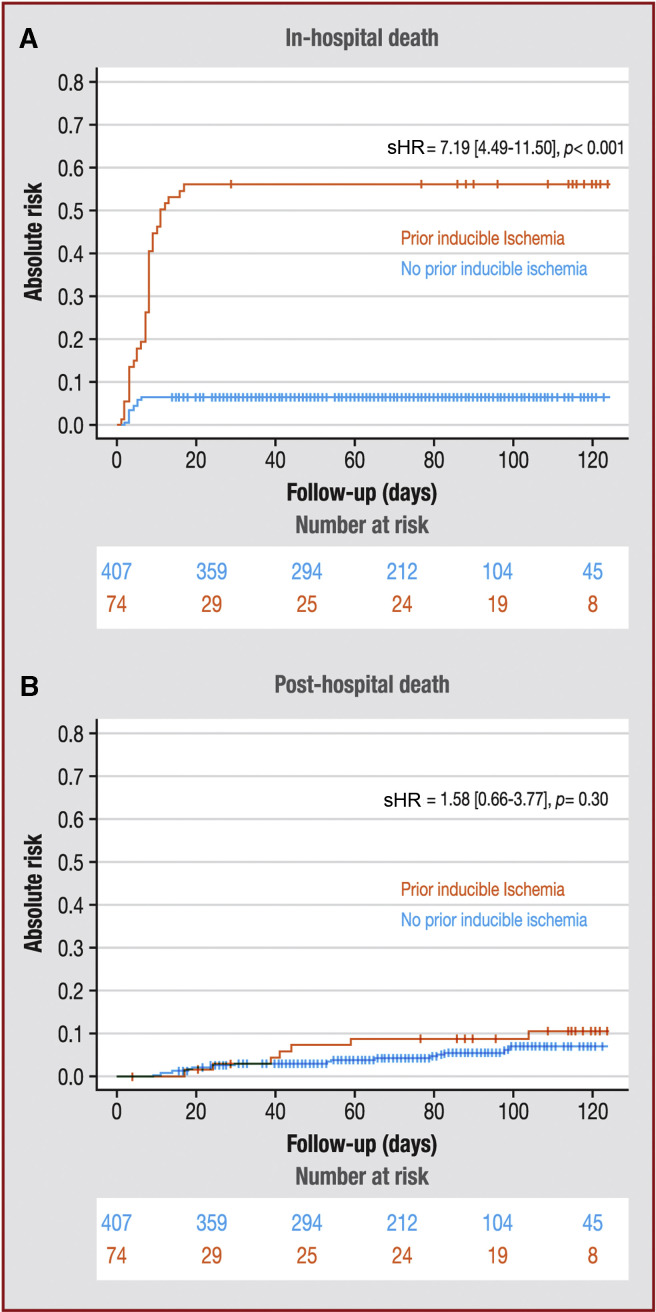
The univariable and multivariable analysis using competitive risk models for prediction of in-hospital and post-hospitalization death are presented in Table 4 . Age, lower BMI, diabetes, hypertension, dyslipidaemia, presence of prior inducible ischaemia, number of ischaemic segments and presence of LGE were associated with in-hospital death in univariable analysis. Using Fine and Gray analysis, the presence of inducible ischaemia was associated with the occurrence of in-hospital death (subdistribution HR [sHR]: 7.19, 95% CI: 4.49–11.50; P < 0.001; Fig. 4 A). In multivariable analysis, the presence of prior inducible ischaemia (sHR: 5.95, 95% CI: 3.39–10.4; P < 0.001), hypertension (sHR: 3.12, 95% CI: 1.67–5.83; P < 0.001) and a lower LVEF value (sHR: 0.98, 95% CI: 0.96–0.99; P = 0.001) were independently associated with in-hospital death (Table 4). The extent of ischaemia was also independently associated with in-hospital death (sHR: 1.30, 95% CI: 1.12–1.47; P = 0.006; Table 4).
Table 4.
Univariable and multivariable competing risk regression analysis for in-hospital death and post-hospitalization death (n = 481).
| In-hospital death (n = 66) |
Post-hospitalization death (n = 27) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Univariable analysis |
Multivariable analysisa |
Univariable analysis |
Multivariable analysisb |
|||||
| sHRc (95% CI) | P | sHRc (95% CI) | P | sHRc (95% CI) | P | sHRc (95% CI) | P | |
| Age (per 1-year increase) | 1.07 (1.04–1.10) | < 0.001 | 1.01 (0.98–1.04) | 0.41 | 1.09 (1.04–1.13) | < 0.001 | 1.08 (1.03–1.14) | < 0.001 |
| Male sex | 1.38 (0.81–2.35) | 0.24 | 2.83 (1.07–7.47) | 0.036 | ||||
| BMI (per 1-kg/m2 increase) | 0.94 (0.89–0.99) | 0.012 | 0.94 (0.88–1.01) | 0.10 | 0.98 (0.92–1.04) | 0.43 | ||
| Diabetes | 1.74 (1.05–2.89) | 0.032 | 1.95 (0.89–4.26) | 0.094 | ||||
| Hypertension | 5.31 (2.98–9.47) | < 0.001 | 3.12 (1.67–5.83) | < 0.001 | 2.20 (1.02–4.74) | 0.044 | ||
| Dyslipidaemia | 1.85 (1.11–3.09) | 0.018 | 0.23 (0.03–1.67) | 0.15 | ||||
| Current or previous smoking | 0.76 (0.40–1.44) | 0.40 | 0.88 (0.34–2.32) | 0.80 | ||||
| Family history of CAD | 0.66 (0.37–1.16) | 0.15 | 1.22 (0.54–2.72) | 0.63 | ||||
| History of HF hospitalization | 1.37 (0.32–5.82) | 0.67 | 1.48 (0.20–10.90) | 0.70 | ||||
| History of AF | 1.00 (0.47–2.10) | 0.99 | 3.09 (1.32–7.19) | 0.009 | 3.00 (1.29–7.03) | 0.012 | ||
| Prior inducible ischaemia | 7.19 (4.49–11.50) | < 0.001 | 5.95 (3.39–10.4) | < 0.001 | 1.58 (0.66–3.77) | 0.30 | ||
| Number of segments with inducible ischaemia (per 1-segment increase) | 1.42 (1.25–1.60) | < 0.001 | 1.30 (1.12–1.47) | 0.006 | 1.31 (1.07–1.59) | 0.008 | 1.38 (1.11–1.71) | 0.007 |
| LGE | 1.69 (1.05–2.73) | 0.03 | 1.34 (0.85–2.10) | 0.21 | 1.13 (0.53–2.44) | 0.75 | ||
| Number of segments with LGE (per 1-segment increase) | 1.09 (0.96–1.24) | 0.19 | 1.03 (0.83–1.28) | 0.76 | ||||
| LVEF (per 5% increase) | 0.66 (0.60–0.85) | < 0.001 | 0.98 (0.96–0.99) | 0.001 | 0.84 (0.68–1.04) | 0.45 | ||
| LV end-diastolic volume index (per 10 mL/m2 increase) | 1.16 (0.62–2.01) | 0.77 | 1.48 (0.85–2.57) | 0.17 | ||||
| RVEF (per 5% increase) | 0.89 (0.73–1.12) | 0.61 | 0.93 (0.75–1.17) | 0.52 | ||||
AF: atrial fibrillation; BMI: body mass index; CAD: coronary artery disease; CI: confidence interval; HF: heart failure; IQR: interquartile range; LGE: late gadolinium enhancement; LV: left ventricular; LVEF: left ventricular ejection fraction; RVEF: right ventricular ejection fraction; sHR: subdistribution hazard ratio.
Covariates in the model by stepwise variable selection with entry and exit criteria set at the P ≤ 0.01 level were: age, BMI, hypertension, presence of LGE, LVEF and presence of prior inducible ischaemia or number of segments of prior inducible ischaemia. Of note, the presence of prior ischaemia and the number of segments of prior inducible ischaemia were not included simultaneously in the model, but were each calculated in their respective models to be investigated individually.
Covariates in the model by stepwise variable selection with entry and exit criteria set at the P ≤ 0.01 level were: age, history of AF and number of segments of prior inducible ischaemia.
HR of the subdistribution hazard function.
Figure 4.
Competitive risk analysis: cumulative incidence functions of A. in-hospital death and B. post-hospitalization death, stratified by presence/absence of prior inducible myocardial ischaemia. CI: confidence interval; sHR: subdistribution hazard ratio.
Age, male sex, hypertension, history of atrial fibrillation (AF) and number of ischaemic segments value were associated with post-hospitalization death in univariable analysis (Table 4). Using Fine and Gray analysis, the presence of inducible ischaemia was not associated with the occurrence of post-hospitalization death (Fig. 4A–B). In multivariable analysis, age (sHR: 1.08, 95% CI: 1.03–1.14; P < 0.001), a history of AF (sHR: 3.00, 95% CI: 1.29–7.03; P = 0.012) and the number of segments with prior ischaemia (sHR: 1.38, 95% CI: 1.11–1.71; P = 0.007) remained significantly associated with post-hospitalization death (Table 4).
Discussion
In this retrospective cohort of patients previously referred for vasodilator stress perfusion CMR, the study demonstrates that:
-
•
the prevalence of patients hospitalized for COVID-19 was 6.5%, of whom 15.4% had prior inducible myocardial ischaemia over the past 2 years;
-
•
after a median follow-up of 73 days, the rate of all-cause death among patients hospitalized for COVID-19 was 19.3%, most of which (71.0%) occurred in hospital;
-
•
among the patients who were discharged from hospital, the rate of post-hospitalization death was 6.5%;
-
•
age, hypertension, diabetes, known CAD and the presence of prior inducible ischaemia were independent predictors of all-cause death;
-
•
hypertension, lower LVEF, the presence of prior inducible ischaemia and the number of segments of prior inducible ischaemia were independently associated with in-hospital death;
-
•
age, history of AF and the number of segments of prior inducible ischaemia were independent predictors of post-hospitalization death.
This study therefore demonstrates the prognostic value of prior inducible myocardial ischaemia by stress CMR to predict all-cause death in patients hospitalized for COVID-19.
As our population is at high cardiovascular risk, the prevalence of patients hospitalized for COVID-19 in this study (6.5%) is slightly higher than in the general population of the severely affected large Paris Metropolitan Area. Despite the heterogeneity between healthcare systems and populations, our in-hospital death rate (13.7%) was comparable to other published series of patients hospitalized for COVID-19 [6], [11], [14], [25], [26]. Long-term mortality data for COVID-19 are currently lacking [27], but a recent study showed that 78% of patients recently recovered from COVID-19 had abnormal findings on CMR a median of 71 days after diagnosis [28].
The current findings confirm that hypertension is a strong predictor of death in hospitalized patients with COVID-19, as suggested by Gao et al. [29]. Other severity risk factors for COVID-19 such as age, diabetes, cardiovascular disease [14], [25], [26], and known CAD [30] were independent prognostic factors of all-cause death in the current study. In addition, age, a history of AF and the number of ischaemic segments were the only independent predictors of post-hospitalization death.
Importantly, the only factor independently associated with all-cause death was prior inducible myocardial ischaemia within the last 2 years. The presence of prior inducible myocardial ischaemia by stress CMR over the last 2 years was independently associated with all-cause in-hospital death, and the extent of prior inducible myocardial ischaemia was independently associated with post-hospitalization death. Inducible myocardial ischaemia is an important marker of vascular vulnerability and atherosclerosis [15], [17], [18], [19], [20], associated with decreased endothelial function and vasodilation capabilities [21]. The current findings suggest a potential role of the endothelium in the pathophysiology of COVID-19, including inappropriate vasoconstriction process contributing to ischaemic tissue damage in lungs, heart, brain and kidneys [10]. However, there are alternative mechanisms by which myocardial ischaemia might mediate the relationship between COVID-19 and all-cause death, such as physiologic reserve and the ability to withstand haemodynamic damage or hypoxaemia in severe COVID-19 cases. This data adds some evidence that pre-existing clinical CAD with associated morphological and functional endothelial alterations may exacerbate the severity of the immune and inflammatory response of the endothelium and vasculature pericytes due to COVID-19. Although similar findings would likely have been obtained with other imaging modalities, such as stress echocardiography or nuclear imaging, further investigations are necessary. In keeping with this hypothesis, Dillinger et al. have shown that coronary calcium score as a biomarker of CAD was independently associated with worse COVID-19 prognosis in 147 patients hospitalized for COVID-19 [31]. The role of endothelial function is highlighted by the fact that prior CAD, hypertension and diabetes were prognostic factors in the study. These factors could contribute to disease severity through impaired antioxidant defences of the endothelium or generation of reactive oxygen species [10].
The current findings do not suggest that stress CMR should be performed in patients hospitalized for COVID-19, rather they demonstrate that documented prior myocardial ischaemia within 2 years is a powerful independent additional factor that helps to stratify the risk of death in patients hospitalized for COVID-19.
Study limitations
Data collection was retrospective in a single centre. However, the relatively short time between hospitalization and the gathering of data reduced the proportion of missing data (2.7%). The aim of the study was to assess whether the presence of prior inducible myocardial ischaemia was associated with death independently of other prognostic factors. Moreover, the fact that most of the patients who had ischaemia were revascularized prior to hospitalization for COVID-19 did not allow us to assess the prognostic value of the presence of persistent ischaemia at the beginning of hospitalization. Moreover, this study only included patients who were hospitalized for COVID-19 and it was not designed to identify whether patients with prior inducible ischaemia have worse outcomes when hospitalized for COVID-19. The findings of this study also need to be confirmed by further studies due to the limited number of patients, which results in limited statistical power in multivariable analysis. As the analysis focuses on post-hospitalization deaths, there is a difference in follow-up between patients with and without prior inducible ischaemia causing a risk of attrition bias. Finally, this retrospective study could not capture all the confounding factors regarding the association between management decisions after the stress CMR examination and patient risks, due to the lack of information on the management of these patients between the CMR examination and their hospitalization for COVID-19.
Conclusions
In patients hospitalized with COVID-19, the presence of prior inducible myocardial ischaemia by stress CMR over the last 2 years was independently associated with all-cause in-hospital, and the extent of prior inducible myocardial ischaemia was independently associated with post-hospitalization death, suggesting a possible involvement of vasculature and endothelial dysfunction in the severity of COVID-19.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Disclosure of interest
S. T. Employee of Siemens Healthcare. The other authors declare that they have no competing interest.
Author contributions
All authors participated in the discussion of the concept of the study. T. P. and J. G. conceived the study design. T. P., F. S., T. H., S. C., T. U., P. G. and J. G. obtained CMR images and analysed CMR scans. T. P., J. G. and J. L. analysed the data and drafted the manuscript with critical revision. J. G. and S. T. technically defined the CMR protocol and reviewed the technical CMR part of the manuscript. As authors, we attest to each of our substantial contributions to the manuscript and revision. All authors read and approved the final manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article or its supplementary information files.
Acknowledgements
We thank the medical, paramedical and research staff of hôpital privé J.-Cartier involved and other partner hospitals in the care of COVID-19 patients during this pandemic. M. Zago provided statistical assistance.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.acvd.2021.10.004.
Appendix A. Supplementary data
References
- 1.Pinney S.P., Giustino G., Halperin J.L., et al. Coronavirus historical perspective, disease mechanisms, and clinical outcomes: JACC focus seminar. J Am Coll Cardiol. 2020;76:1999–2010. doi: 10.1016/j.jacc.2020.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y., Tse G., Li G., Lip G.Y.H., Liu T. ACE inhibitors and angiotensin II receptor blockers may have different impact on prognosis of COVID-19. J Am Coll Cardiol. 2020;76:2041. doi: 10.1016/j.jacc.2020.07.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garot J., Amour J., Pezel T., et al. SARS-CoV-2 fulminant myocarditis. JACC Case Rep. 2020;2:1342–1346. doi: 10.1016/j.jaccas.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uriel N., Sayer G., Clerkin K.J. Myocardial injury in COVID-19 patients: the beginning or the end? J Am Coll Cardiol. 2020;76:547–549. doi: 10.1016/j.jacc.2020.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lala A., Johnson K.W., Januzzi J.L., et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fauvel C., Weizman O., Trimaille A., et al. Pulmonary embolism in COVID-19 patients: a French multicentre cohort study. Eur Heart J. 2020;41:3058–3068. doi: 10.1093/eurheartj/ehaa500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McBane R.D., 2nd. Thromboembolism and the pandemic. J Am Coll Cardiol. 2020;76:2073–2075. doi: 10.1016/j.jacc.2020.09.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piazza G., Campia U., Hurwitz S., et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol. 2020;76:2060–2072. doi: 10.1016/j.jacc.2020.08.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inciardi R.M., Adamo M., Lupi L., et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41:1821–1829. doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Libby P., Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41:3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nadkarni G.N., Lala A., Bagiella E., et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:1815–1826. doi: 10.1016/j.jacc.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi S., Qin M., Shen B., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo T., Fan Y., Chen M., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alvarez-Garcia J., Lee S., Gupta A., et al. Prognostic impact of prior heart failure in patients hospitalized with COVID-19. J Am Coll Cardiol. 2020;76:2334–2348. doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwong R.Y., Ge Y., Steel K., et al. Cardiac magnetic resonance stress perfusion imaging for evaluation of patients with chest pain. J Am Coll Cardiol. 2019;74:1741–1755. doi: 10.1016/j.jacc.2019.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heitner J.F., Kim R.J., Kim H.W., et al. Prognostic value of vasodilator stress cardiac magnetic resonance imaging: a multicenter study with 48,000 patient-years of follow-up. JAMA Cardiol. 2019;4:256–264. doi: 10.1001/jamacardio.2019.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pezel T., Sanguineti F., Kinnel M., et al. Prognostic value of dipyridamole stress perfusion cardiovascular magnetic resonance in elderly patients > 75 years with suspected coronary artery disease. Eur Heart J Cardiovasc Imaging. 2021;22:904–911. doi: 10.1093/ehjci/jeaa193. [DOI] [PubMed] [Google Scholar]
- 18.Kinnel M., Garot J., Pezel T., et al. Prognostic value of vasodilator stress perfusion CMR in morbidly obese patients (BMI ≥ 40 kg/m2) without known CAD. JACC Cardiovasc Imaging. 2020;13:1276–1277. doi: 10.1016/j.jcmg.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Pezel T., Sanguineti F., Kinnel M., et al. Safety and prognostic value of vasodilator stress cardiovascular magnetic resonance in patients with heart failure and reduced ejection fraction. Circ Cardiovasc Imaging. 2020;13:e010599. doi: 10.1161/CIRCIMAGING.120.010599. [DOI] [PubMed] [Google Scholar]
- 20.Antiochos P., Ge Y., Steel K., et al. Imaging of clinically unrecognized myocardial fibrosis in patients with suspected coronary artery disease. J Am Coll Cardiol. 2020;76:945–957. doi: 10.1016/j.jacc.2020.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oemar B.S., Tschudi M.R., Godoy N., Brovkovich V., Malinski T., Luscher T.F. Reduced endothelial nitric oxide synthase expression and production in human atherosclerosis. Circulation. 1998;97:2494–2498. doi: 10.1161/01.cir.97.25.2494. [DOI] [PubMed] [Google Scholar]
- 22.Marcos-Garces V., Gavara J., Monmeneu J.V., et al. Vasodilator stress CMR and all-cause mortality in stable ischemic heart disease: a large retrospective registry. JACC Cardiovasc Imaging. 2020;13:1674–1686. doi: 10.1016/j.jcmg.2020.02.027. [DOI] [PubMed] [Google Scholar]
- 23.Pezel T., Sanguineti F., Kinnel M., et al. Feasibility and prognostic value of vasodilator stress perfusion CMR in patients with atrial fibrillation. JACC Cardiovasc Imaging. 2021;14:379–389. doi: 10.1016/j.jcmg.2020.07.041. [DOI] [PubMed] [Google Scholar]
- 24.Cerqueira M.D., Weissman N.J., Dilsizian V., et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–542. doi: 10.1161/hc0402.102975. [DOI] [PubMed] [Google Scholar]
- 25.Grasselli G., Zangrillo A., Zanella A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yelin D., Wirtheim E., Vetter P., et al. Long-term consequences of COVID-19: research needs. Lancet Infect Dis. 2020;20:1115–1117. doi: 10.1016/S1473-3099(20)30701-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puntmann V.O., Carerj M.L., Wieters I., et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao C., Cai Y., Zhang K., et al. Association of hypertension and antihypertensive treatment with COVID-19 mortality: a retrospective observational study. Eur Heart J. 2020;41:2058–2066. doi: 10.1093/eurheartj/ehaa433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dillinger J.G., Benmessaoud F.A., Pezel T., et al. Coronary artery calcification and complications in patients with COVID-19. JACC Cardiovasc Imaging. 2020;13:2468–2470. doi: 10.1016/j.jcmg.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article or its supplementary information files.