Abstract
Introduction
This study compares recurrence rates and functional outcomes of patients who underwent anterior arthroscopic synovectomy versus combined anterior arthroscopic/posterior open synovectomy for diffuse pigmented villonodular synovitis (DPVNS).
Methods
41 patients were grouped by initial procedure and tracked for disease recurrence and functional outcomes (Lysholm Scale).
Results
24 patients (58.5%) had disease recurrence [16 (57.1%) arthroscopic, 8 (61.5%) combined, chi-square test p = 0.81]. The combined procedure mean Lysholm Score (75.4) exceeded the arthroscopic (68.1) (two-sample t-test p = 0.25).
Conclusions
There is no statistical evidence that the combined procedure harms functionality more than arthroscopic only or that recurrence rates differ between treatment methods.
Keywords: DPVNS, Tumor recurrence, Synovial membrane, Lysholm score
1. Introduction
Synovial joints in the human body contain a synovial membrane that encloses fluid within the joint. This fluid lubricates the joint creating an almost frictionless surface during movement. Pigmented villonodular synovitis (PVNS) is a disease characterized by the benign abnormal growth of the synovial membrane, causing swelling and inflammation of the joint. This condition, which most commonly affects the knee, can make mobility difficult and painful. There are two main classifications of PVNS: diffuse PVNS (DPVNS) which involves the entire synovium, and localized PVNS (LPVNS) which occurs in a single region of the joint. LPVNS can be reliably managed with simple excision of the localized mass, without a complete synovectomy. Numerous studies report low recurrence rates and complications associated with the treatment of LPVNS compared to DPVNS.1,2,3,4
DPVNS affects approximately 1.8 people per million and is more difficult to treat than LPVNS. Reported treatment outcomes vary greatly due to a myriad of factors including small sample populations, differing surgical techniques, and a wide range of patient demographics. Recurrence rates following attempts at surgical resection can be as high as 50% and present a significant health challenge.5 The disease often becomes more difficult to treat in patients who have a relapse, as continued recurrence can create chronic inflammation in the joint resulting in articular cartilage degeneration.6 Persistent disease can require total knee replacement to control the disease and improve pain and function.
For physicians treating DPVNS, the goal is to lower the long-term recurrence rates of the disease and improve pain and functionality of the knee joint, thereby improving the patient's quality of life. The principal treatment for DPVNS is to perform a complete synovectomy to eliminate the etiology of the inflammatory process. In addition to complete synovectomy, DPVNS can extend outside of the confines of the joint. The importance of eliminating extracapsular disease and its role in recurrence and functionality is unclear. Different combinations of surgical techniques have been utilized to treat DPVNS. The selection of a surgical technique must balance the morbidity of the procedure with the risk of recurrence. Arthroscopy is the least invasive surgical technique but can be particularly challenging to remove posterior disease, whereas the standard “open” surgery uses a larger incision to access the joint to remove the synovium. A third surgical strategy combines an anterior arthroscopic procedure with a posterior open procedure. In this approach, arthroscopy is performed first to remove as much of the synovial lining as possible, followed by open surgery of the posterior knee to remove any disease that has grown outside of the knee joint as well as the posterior synovium. It is well documented in the literature that a complete synovectomy provides lower recurrence rates compared to a partial synovectomy for patients with DPVNS.3,7,8 The recurrence rates for only arthroscopic procedures used to treat DPVNS range from 9% to 83%.3,4,7, 8, 9 Recurrence rates for the combined anterior arthroscopic and posterior open procedure range from 9% to 47%.4,8,9,10Direct comparison of the two surgical techniques is confounded by a potential selection bias of choosing the open surgical approach for patients with more extensive or extracapsular disease. After numerous recurrences and/or degeneration to the knee, a total knee arthroplasty is often the last resort. The rate of knee replacement in patients originally diagnosed with DPVNS is around 5%.7,10, 11, 12
Non-surgical treatment options have also been investigated for DPVNS. Radiation therapy has been used as monotherapy or combined with surgery. While limited studies have been conducted utilizing radiation as a primary form of treatment, the results show promise.13 Many practitioners remain concerned about the risk of radiation-associated malignancies as well as potential complications of radiation including arthrofibrosis, articular cartilage damage, and postoperative complications if total knee arthroplasty is required. Additional non-surgical treatment modalities for DPVNS include medications. Current clinical trials are investigating Imatinib Mesylate (Gleevec®), a tyrosine kinase inhibitor, as well as Emactuzumab and Cairalizumab, both of which are monoclonal antibodies that inhibit the CSF-1 receptor.14 At this time the long-term outcomes of patients treated with these agents is unknown and controversy remains as to the optimal treatment approach for patients with DPVNS.
The goals of our study are as follows:
-
1.
To determine the recurrence rates, functional outcomes, and complication rates of patients who have undergone a combined anterior arthroscopic synovectomy and posterior open synovectomy.
-
2.
To determine whether extracapsular posterior disease requiring an open posterior surgical approach portends a worse prognosis with regard to functional outcomes and local recurrence.
-
3.
To determine functional outcomes for patients who have extracapsular posterior disease and elect not to have the additional open posterior surgery to remove it in addition to the arthroscopic removal of the intraarticular disease.
Based on a review of the literature as well as the assumption that greater posterior and extracapsular disease removal can occur with an aggressive open approach, we hypothesize that recurrence rates will be lower for the combined arthroscopic synovectomy and posterior open synovectomy compared with the use of an arthroscopic synovectomy alone.4,8, 9, 10 We hypothesize, however, that the combined procedure will have worse functional outcomes due to the greater surgical morbidity associated with the open procedure. Furthermore, we expect patients with extracapsular disease will have higher recurrence rates and worse functionality due to the more extensive nature of their disease.
2. Methods
Following IRB approval we conducted a retrospective search for all patients treated with total synovectomy of the knee at our institution between 2003 and 2018. Patients were included in the study if they:
-
1)
Had a diagnosis of DPVNS confirmed by review of the pathology report, clinical records, and imaging.
-
2)
Underwent a complete arthroscopic synovectomy alone or in combination with open posterior resection to treat their DPVNS.
-
3)
Had a minimum of 12 months follow-up from their initial procedure.
-
4)
Had a minimum of one MRI obtained postoperatively to evaluate for recurrence.
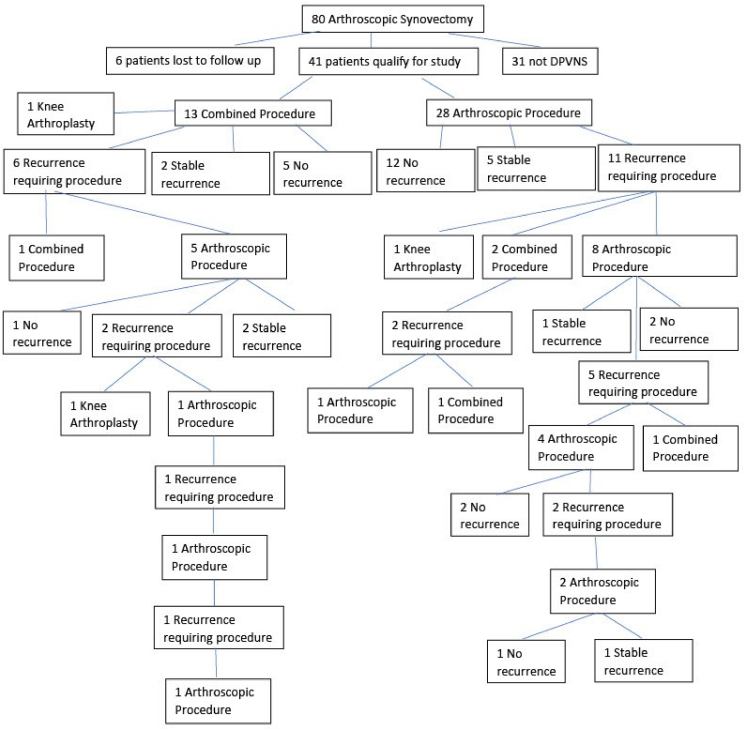
Patients with LPVNS were excluded from the study. Chart review included review of patient follow-up visits, MRIs, and additional procedures performed. Patients who had prior knee surgery were included in the study and prior procedure(s) documented. Of the unique 80 patients identified as having anterior arthroscopic knee synovectomy, 31 were treated for reasons other than DPVNS and 8 patients were lost to follow-up resulting in 41 patients qualifying for the study (Fig. 1).
Fig. 1.
DPVNS Study Patient Flow.
Notes: “Stable recurrence” reflects that the patient had an asymptomatic recurrence or symptomatic recurrence and elected to not have surgery. One patient progressed from having a combined procedure to a total knee arthroplasty without having recurrence due to degenerative changes.
All of the knee arthroscopic synovectomies were performed by a single, fellowship-trained sports medicine surgeon comfortable with the posterior arthroscopic approach to remove intracapsular posterior disease. The posterior knee open DPVNS resections were performed by one of three different fellowship-trained musculoskeletal oncologists. Surgical approach and treatment decisions were made by the managing surgeons based on a combination of factors including disease extent, previous surgeries, and patient preference. Patients with disease confined to the joint capsule underwent an arthroscopic only approach including removal of posterior intracapsular disease through the scope via posterior portals. Patients with extensive symptomatic disease outside of the posterior capsule including large Baker's cysts filled with DPVNS generally underwent an arthroscopic approach followed by open posterior resection of disease. Patients with minimal posterior extracapsular disease without symptoms and/or patients felt to be at high risk of morbidity or complications from an open posterior approach such as morbidly obese patients were advised to have an arthroscopic approach alone leaving the asymptomatic posterior extracapsular disease. The arthroscopic synovectomy surgeries were completed using standard anteromedial, anterolateral and superolateral portals and rarely a superomedial portal. Posterolateral and posteromedial portals were created as needed to reach disease in the posterolateral and posteromedial knee. The combined procedures began with a supine arthroscopic approach which then transitioned to the prone open posterior approach, using a curvilinear incision. The goal of the open surgery was to remove all gross disease.
Patients were placed into two groups based on their initial procedure: arthroscopic alone or arthroscopic plus open posterior “combined” approach (Table 1A, Table 1B). These categories include patients that had both intracapsular and extracapsular DPVNS. This study did not investigate an open anterior and open posterior surgical technique as it was not used at our institution during the time period of this study due to the surgeon's belief that this approach results in significant morbidity. Demographic characteristics were determined for the two groups as well as the recurrence rates, time to recurrence, and total number of recurrences. Any prior surgeries, either to treat DPVNS or a different knee injury, were recorded. Patient surveillance varied depending on the severity of the disease and symptoms, but postoperative MRIs were typically ordered at 6 months, 12 months, and then on a yearly basis. Recurrence was defined as disease appearing on MRI regardless of symptoms. If a patient was asymptomatic and showed no recurrence on MRI after four years, the patient was discharged to follow-up on an as needed basis.
Table 1A.
Initial DPVNS patient characteristics (index procedure).
| Arthroscopic Patients | Combined Patients | |
|---|---|---|
| n | 28 | 13 |
| Age (Mean (SD)) | 34.4 (14.8) | 30.3 (14) |
| Sex = M (%) | 10 (36%) | 9 (69%) |
| Race (%) | ||
| African American | 5 (18%) | 1 (8%) |
| Caucasian | 22 (79%) | 12 (92%) |
| Other | 1 (4%) | 0 (0%) |
| Prior Surgery (%) | 10 (36%) | 5 (38%) |
| # with extra-articular disease | 4 | 5 |
| Recurrence Prior Surgery | 8 | 5 |
| Any Recurrence = Yes (%) | 16 (57%) | 8 (62%) |
| Symptomatic Recurrence | 11 | 6 |
| Asymptomatic Stable Recurrence | 5 | 2 |
| Mean Days to First Recurrence (SD) | 750 (610) | 799 (913) |
| Total Recurrences (%) | ||
| 0 | 12 (43%) | 5(38%) |
| 1 | 8 (29%) | 4 (31%) |
| 2 | 6 (21%) | 3 (23%) |
| 3 | 1 (4%) | 0 (0%) |
| 4 | 1 (4%) | 1 (8%) |
| Total Arthroplasty | 1 | 2 |
Table 1B.
Comparison of patients with and without prior surgery.
| Arthroscopic |
Combined |
|||
|---|---|---|---|---|
| Prior Surgery | No Prior Surgery | Prior Surgery | No Prior Surgery | |
| N | 10 | 18 | 5 | 8 |
| Recurrence (%) | 8 (80%) | 8 (44%) | 5 (100%) | 3 (38%) |
| Lysholm Score | ||||
| N | 4 | 9 | 2 | 5 |
| Mean (SD) Score | 63.3 (3.8) | 73.8 (24.4) | 64.5 (7.8) | 74.8 (15.2) |
Study patients were contacted by phone to answer a series of questions related to pain, swelling, activity, further surgery/recurrence, and medications. Phone calls also included Lysholm knee score questionnaire and determination if the patient had any follow-up care outside of our institution or outside our visible electronic medical record. The Lysholm Knee Scoring Scale is an eight question survey used to quantify knee function on a scale of 0–100 (higher score equates to more functional knee). Of the 41 patients in the study, 20 agreed to participate in the Lysholm survey. Two patients were reached by phone but chose to not answer the survey questions. Nineteen patients were unable to be contacted and were purely chart review.
Fig. 1 is a flow diagram describing the treatment paths of study participants. Recurrence rates were compared between patients whose index procedure was athroscopic (57%, 16/28) versus combined (62%, 8/13) using a chi square test for proportions. Lysholm scores were compared for patients who had a combined procedure (n = 8) versus those with only arthroscopic procedure(s) (n = 12) using a two-sample t-test.
3. Results
The mean follow-up time for patients in the study was 57.66 months (±37.97, range 12–144). At the end of our study, 20 of the 41 patients (48.8%) were still attending follow-up visits and actively being surveilled for DPVNS. 21 of the 41 patients (51.2%) were being seen on an as needed basis, forgoing surgery for an asymptomatic/stable recurrence, or demonstrating no evidence of recurrent disease on imaging with absence of symptoms for 4 years.
Patient characteristics and outcomes from the initial procedure are presented in Table 1A. 24 patients (58.5%) had a recurrence [16 (57%) arthroscopic only and 8 (62%) combined procedure]. Patients with recurrences were treated with either a combined procedure, arthroscopic procedure, or knee replacement. The average time to first recurrence was 26.1 months (±23.95, median 17.46, range 4.37–100.04). Of the patients who recurred, half (n = 12) had multiple recurrences. Overall, the 41 patients in the study collectively had a total of 51 arthroscopic procedures and 18 combined arthroscopic/open procedures. The appendix provides types of surgeries and average time to recurrence for additional surgeries that were performed on the subset of patients with recurrences listed in Table 1A.
Table 1B compares recurrence rates and functional outcomes for patients who had prior surgery on their knee to treat DPVNS or other knee pathology to patients without prior operations. The recurrence rates were higher for patients with prior surgery. Functional outcomes were worse for patients with prior surgery.
Of the 24 people that had recurrences, 14 (58.3%) had their first recurrence within two years of follow-up, 7 had their first recurrence between years 2–4 of follow-up (29.7%), and 3 had their first recurrence past year 4 of follow-up (12.5%). The mean age for non-recurrent patients was 33.1 and mean age for recurrent patients was 32.9.
Three patients who underwent combined procedures on their knee had post-operative complications. The complications included one patient with cellulitis and two patients with fever and severe pain. No arthroscopic only surgeries had complications. Of the three patients who progressed to total knee arthroplasty, two had a prior combined procedure.
Table 2A presents summary statistics of the Lysholm scores computed for each treatment approach. The average time between the patient's last surgery and the date they were reached by phone was 54.8 months (range 9–148 months). The mean Lysholm score for patients with the combined procedure (75.4) exceeded that for patients with the arthroscopic procedure (68.1); however, this difference was not statistically significant (p = 0.37). Furthermore, the patients with a combined procedure were also younger, on average, than those with the arthroscopic procedure (34.9 years vs. 40.7 years).
Table 2A.
Lysholm Scores by Procedure (Combined = ever had a combined).
| Arthroscopic Patients | Combined Patients | |
|---|---|---|
| n | 12 | 8 |
| Mean Lysholm Scores (SD) | 68.1 (19.5) | 75.4 (16.1) |
| Mean months between last surgery and call (SD) | 60.3 (50.3) | 46.6 (46.7) |
| Age at time of contact (SD) | 40.7(10.9) | 34.9 (15.1) |
| Sex = M (%) | 3 (25%) | 5 (63%) |
| Race (%) | ||
| African American | 2 (17%) | 0 (0%) |
| Caucasian | 9 (75%) | 8 (100%) |
| Other | 1 (8%) | 0 (0%) |
Note: The Lysholm Knee Scoring Scale was chosen due to its ease of use over the phone and its ability to assess knee function in a concise manner. The Lysholm Knee Scoring Scale assesses pain, swelling, and activity. This scale has eight main sections: limp, cane or crutches, locking sensation in the knee, giving way sensation from the knee, pain, swelling, climbing stairs, and squatting. Point totals were given for each section and the patient's responses added to equal a score between 0 (worst) and 100 (best). For reference, according to Briggs et al. the average Lysholm Scale Knee Score for people with healthy knees is estimated to be 94.15
The combined approach was used primarily to treat patients with extensive extracapsular disease. Lysholm scores and recurrence rates for patients with extracapsular disease are summarized in Table 3. Four patients chose to have only arthroscopy on their knee to treat the intracapsular disease and left the extracapsular disease alone (Table 3).
Table 3.
Recurrence Rates and Lysholm Scores for Patients with Surgery to Treat the Extracapsular DPVNS (Surgical categorization based on Index Procedure).
| Arthroscopic – Intracapsular + Extracapsular | Arthroscopic – Intracapsular | Combined procedures – Intracapsular + Extracapsular DPVNS | |
|---|---|---|---|
| n | 4 | 24 | 13 |
| Age (Mean (SD)) | 41.5 (10.3) | 33.2 (15.3) | 30.3 (14.0) |
| Sex = M (%) | 1 (25%) | 9 (38%) | 9 (69%) |
| Recurrence (%) | 3 (75%) | 13 (54%) | 8 (62%) |
| Intracapsular Only | 3 | 10 | 4 |
| Intracapsular and Extracapsular | N/A | 3 | 4 |
| Lysholm Score Data | |||
| n | 1 (25%) | 12 (50%%) | 7 (54%) |
| Mean (SD) Score | 63.0 | 71.2(21) | 71.9 (13.7) |
| Mean (SD) Months between Most Recent Surgery and Call | 10 | 57.5 (49) | 39.4 (47.2) |
Due to the low incidence of cases of DPVNS and correspondingly the relatively small sample size used in this study, the study is not powered to detect a small change in recurrence rates between the two groups. The difference between the recurrence rates in Table 1A was not statistically significant, measured by a chi square test for proportions (p = 0.81). The difference between the Lysholm scores in Table 2A was also not statistically significant measured by a two sample t-test (p = 0.37).
4. Discussion
The first goal of our study was to determine the recurrence rates, functional outcomes, and complication rates of patients who underwent a combined anterior arthroscopic synovectomy and posterior open synovectomy versus those patients who underwent arthroscopic synovectomy alone. Our study found no significant difference in recurrence rates between the 2 techniques (57% vs. 62%, p = 0.81, Table 1A, Table 1B). Similarly, the mean Lysholm scores were not significantly different between the 2 approaches (75.4 combined vs. 68.1 arthroscopic only, p = 0.37, Table 2A, Table 2B). Although the ages of the patients in the two cohorts were different (mean 47 years old for arthroscopic only versus 34.9 for combined) we do not feel that this difference in age would have a meaningful impact on scores. Overall complication rates were low with 3 relatively minor issues. The low recurrence rate beyond year 4 of follow-up provides justification for monitoring patients on an as needed basis past year 4.
Table 2B.
Lysholm Scores by Procedure (Combined = index procedure was combined).
| Arthroscopic Patients | Combined Patients | |
|---|---|---|
| n | 13 | 7 |
| Mean Lysholm Scores (SD) | 70.54 (20.7) | 71.86 (13.7) |
| Mean months between last surgery and call (SD) | 57.9 (49.0) | 49.0 (49.9) |
| Age at time of contact (SD) | 45.7 (9.7) | 36.3 (15.7) |
| Sex = M (%) | 4 (31%) | 4 (57%) |
| Race (%) | ||
| African American | 2 (15%) | 0 (0%) |
| Caucasian | 10 (77%) | 7 (100%) |
| Other | 1 (8%) | 0 (0%) |
Our second goal was to determine whether extracapsular posterior disease portends a worse prognosis with regard to functional outcomes and local recurrence regardless of surgical approach. Our study suggests that patients with extracapsular disease do not have significantly higher rates of local recurrence and have similar functional outcomes to patients with isolated intracapsular disease (Table 3). The majority of the extracapsular disease was treated with the combined approach in order to remove as much DPVNS as possible. The recurrence rate for extracapsular patients is elevated, but this is likely due to the vast spread of disease that is less contained than the intracapsular disease. Furthermore, 50% of recurrences for combined extracapsular procedures were only intracapsular. An important finding of our study is that while extracapsular disease may be difficult to treat, requiring a more invasive surgical approach and yielding higher rates of recurrence, there is no evidence to suggest that future knee function and pain will be negatively impacted or that the presence of extracapsular disease results in a higher need for total knee arthroplasty.
The third goal of this study was to determine the functional outcomes for patients who have extracapsular posterior disease and elect not to remove it with open surgery. Although we only identified 4 patients who met this criteria, and only one with Lysholm scores, this score (63) compares favorably to the other groups and at least suggests that extracapsular disease can be reasonably well-tolerated. Additional patient numbers are required to provide more meaningful answers to this question.
The recurrence rate for the combined anterior arthroscopic and posterior open approach (61.5% for first procedure) is higher than many reports in the literature.3,4,7, 8, 9, 10 The arthroscopic recurrence rate (57.1% for 1st procedure), however, is consistent with other studies.3,4,7, 8, 9, 10 There are a few possible explanations for the higher recurrence rates in our study compared to the literature. First, fifteen of our forty-one patients (37%) had prior surgery on their knee including seven patients with recurrent DPVNS at presentation. Other studies tend to exclude patients who have had prior synovectomies on their knee as having a prior recurrence may portend more aggressive tumor biology and is believed to make a further recurrence more likely. These prior surgical patients (including both PVNS and non-PVNS) had higher rates of initial recurrence than those without a prior surgery (100% vs. 38% for combined, 80% vs. 44% for arthroscopic, 87% vs. 42% overall). These patients also had worse functional outcomes demonstrated by lower Lysholm scores. This data suggests that prior knee pathology may increase the likelihood of recurrent DPVNS and worse functional outcomes. Although an interesting finding, the role prior surgical intervention has on the rate of recurrence remains unclear. Second, the research team was liberal in what was defined as a recurrence. Any area of tumor that appeared in the knee on the MRI was considered a recurrence of DPVNS, even if the tumor was stable and asymptomatic. For a number of these patients, if an MRI had not been obtained, they would have been presumed to have no recurrence based on their symptomatology. A third possible explanation is that three different surgeons performed the posterior portion of the combined procedure and this could have altered the results as inevitably the surgeons’ techniques varied to some degree. A final potential reason for the high recurrence rates is the complex nature of the cases treated. A relatively large percentage of patients referred to our tertiary center had a failed previous surgery and had extensive extracapsular disease as demonstrated by the fact that 31.7% of the patients in the study were initially treated with a combined procedure. The indications for this procedure are described above, but patients who were treated in this fashion had more extensive disease making the open portion of the procedure necessary.
The most recent meta-analysis by Mollon et al., in 2015 found an overall recurrence rate of 27.7% (37.8% for arthroscopic, 13.9% for combined) after following 448 patients that had surgical treatment for DPVNS.18 This study, however, only reviewed 37 cases of people treated with the combined arthroscopic and open procedure. This small sample size in a meta-analysis suggests that more data needs to be collected on the combined procedure before a definitive conclusion can be made on its overall effectiveness. A study by Colman et al., in 2012 examined 11 patients with a combined arthroscopic and open procedure and found a recurrence rate of 9%. They excluded patients that had a prior synovectomy and had a minimum follow-up of 3 months which likely contributed to their lower recurrence rate. They also reviewed 26 patients that had an all arthroscopic procedure and found a recurrence rate of 62%, however some patients had only a partial synovectomy which may explain the high recurrence rate.
We hypothesized that our study would reveal lower average Lysholm scores in the combined surgical patients due to the greater extent of disease at presentation as well as the greater surgical morbidity associated with an open posterior approach to the knee. This is a critically important question for patients and surgeons to understand as a main goal of PVNS treatment is to improve knee symptoms in order to provide patients a better quality of life. Surprisingly, although not statistically significant, the average combined Lysholm scores exceeded the arthroscopic scores (75.4 vs. 68.1) This result suggests that the combined procedure, when necessary to remove bulky posterior extracapsular disease, while more invasive and associated with potentially prolonged recovery times, as well as an increased risk of minor complications, will not harm long-term knee function more than an arthroscopic procedure. One potential explanation for the higher than expected scores for the combined patients was that the average age was lower than the arthroscopic patients. These patients may perform better due to less natural decline in function that accompanies age. However, in a study published by Briggs et al., in 2009, they found no demonstrated correlation between Lysholm score and age or gender.16
Three patients in the study progressed to a total knee arthroplasty (6.5%). The current literature describes rates of knee replacement from 2% to 10%.7,10, 11, 12 The recurrence rates in our study are high, but the rate of knee arthroplasty remains consistent with other data. None of the patients who underwent total knee arthroplasty in the study population developed post-operative complications.
5. Limitations
There were a number of limitations in this investigation. As a single institutional study, the treatment algorithm was relatively consistent but the small overall number of patients in the study limits the strength of the conclusions. Furthermore, the study would have been strengthened if Lysholm scores were obtained from patients prior to surgical intervention to provide a baseline for comparison. Additional Lysholm testing at regular intervals following surgery would also add to the understanding of function over time and how it is affected by local recurrence and surgical approach. Another limitation is that three different physicians performed the posterior portion of the combined procedures. The surgeons may have had different techniques or skill levels that resulted in different recurrence rates and functional outcomes. An additional limitation is the limited follow-up. Due to the relatively low number of DPVNS cases, there is considerable variability in the patient's follow-up interval at the time their outcomes were evaluated. It is unclear how many patients with shorter follow-up may develop recurrent disease or experience a decline in function and require a knee arthroplasty in the future. A final limitation is the Lysholm scoring scale used to assess functional outcomes. This scoring system was chosen due to its ease of use over the phone as well as the wide scope of functional outcomes it questions. Many patients, however, were hesitant to provide an exact score and instead gave a range as their initial answer. Upon further prodding patients were able to give a specific score, but the scoring system or method of phone communication may potentially have made patients more indecisive. A prospective study incorporating more structured surveillance with imaging and functional outcomes measures would add value.
6. Conclusions
The goal of this study was to determine how recurrence rates and functional knee outcomes varied between the use of a combined anterior arthroscopic and posterior open synovectomy compared with an arthroscopic approach. The initial hypothesis was that there would be lower recurrence rates for the combined procedure due to greater surgical debridement as well as lower Lysholm scores due to greater surgical trauma associated with an open approach. Interestingly, our study found no statistical difference in recurrence rates (Table 1A, Table 1B) or functional scores (Table 2A, Table 2B) for the combined vs. arthroscopic approach.
A secondary goal of this study was to determine if patients with extracapsular posterior disease have a worse prognosis. Having extracapsular posterior disease did not portend a worse prognosis as the rates of recurrence were only marginally higher than the rate of recurrence for the overall group. Furthermore, the mean Lysholm score of patients with extracapsular disease did not vary significantly from the group as a whole suggesting that if an open posterior approach in addition to arthroscopic synovectomy is required patients can have similar functional outcomes. Our study did not have enough patients to provide meaningful guidance regarding whether asymptomatic extracapsular disease should be removed. Interestingly, for the patients with extracapusular disease in our study, 50% recurred with intracapsular disease only.
This study, along with others published on this topic, can help serve as a baseline for recurrence and functional results to compare the outcomes of new systemic therapies emerging to treat DPVNS. Challenges with DPVNS include the rarity of the disease, the variability in extent of disease at presentation, and the difficulty therefore to perform a prospective study to analyze treatment options. A potential next step would be to increase the length of the study and obtain Lysholm scores pre-treatment and at regular intervals post-operation to provide more data for analysis.
Table A1.
Describe patient characteristics at time of 2nd Surgery:
| Total Knee Arthroplasty | Arthroscopic | Combined | |
|---|---|---|---|
| n | 2 | 13 | 3 |
| Age at time of Surgery (Mean (SD)) | 43.69 (N/A) | 32.57 (10.47) | 32.68 (12.86) |
| Sex = M (%) | 2 (100) | 8 (61.5) | 3 (60.0) |
| Race (%) | |||
| African American | 1 (50) | 0 (0) | 0 (0) |
| Caucasian | 1 (50) | 12 (92.3) | 3 (100) |
| Other | 0 (0) | 1 (7.7) | 0 (0) |
| Any Recurrence = Yes (%) | 0 (0) | 10 (76.9) | 2 (66.7) |
| Type of 2nd Surgery | Mean Recurrence Days (SD) |
|---|---|
| Arthroscopic | 662.3 (553.6) |
| Combined | 1932 (389.0) |
Table A2.
Describe patient characteristics at time of 3rd Surgery:
| Total Knee Arthroplasty | Arthroscopic | Combined | |
|---|---|---|---|
| n | 1 | 6 | 2 |
| Age at time of Surgery (Mean (SD)) | 41.8 (N/A) | 40.1 (11.66) | 48.8(13.1) |
| Sex = M (%) | 1 (100) | 3 (50.0) | 1 (50.0) |
| Race (%) | |||
| African American | 0 (0) | 0 (0) | 0 (0) |
| Caucasian | 1 (100) | 5 (83.3) | 2 (100) |
| Other | 0 (0) | 1 (16.7) | 0 (0.0) |
| Any Recurrence = Yes (%) | 0 (0) | 3 (50.0) | 0 (0) |
| Type of 3rd Surgery | Mean Recurrence Days (SD) |
|---|---|
| Arthroscopic | 384.33 (278.20) |
Table A3.
Describe patient characteristics at time of 4th Surgery:
| Arthroscopic | |
|---|---|
| n | 3 |
| Age at time of Surgery (Mean (SD)) | 46.77 (8.76) |
| Sex = M (%) | 2 (66.7) |
| Race (%) | |
| African American | 0 (0) |
| Caucasian | 2 (66.7) |
| Other | 1 (33.3) |
| Any Recurrence = Yes (%) | 2 (66.7) |
| Type of 4th Surgery | Mean Recurrence Days (SD) |
|---|---|
| Arthroscopic | 194.5 (8.5) |
Table A4.
Describe patient characteristics at time of 5th Surgery:
| Arthroscopic | |
|---|---|
| n | 1 |
| Age at time of Surgery (Mean (SD)) | 56.66 (N/A) |
| Sex = M (%) | 1 (100) |
| Race (%) | |
| African American | 0 (0) |
| Caucasian | 1 (100) |
| Other | 0 (0) |
| Any Recurrence = Yes (%) | 0 (0) |
| Type of 5th Surgery | Mean Recurrence Days (SD) |
|---|---|
| Arthroscopic | N/A |
CRediT authorship contribution statement
Alexander Kerschner: Conceptualization, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing, Visualization. David King: Conceptualization, Methodology, Writing – review & editing, Supervision. Carole Vetter: Conceptualization, Writing – review & editing, Supervision.
Acknowledgements
The corresponding author would like to gratefully acknowledge financial support from the Medical College of Wisconsin to support this research.
Contributor Information
Alexander Kerschner, Email: alkerschner@mcw.edu.
David King, Email: cvetter@mcw.edu.
Carole Vetter, Email: dking@mcw.edu.
References
- 1.Lee B.I., Yoo J.E., Lee S.H., Min K.D. Localized pigmented villonodular synovitis of the knee: arthroscopic treatment. Arthroscopy. 1998;14(7):764–768. doi: 10.1016/s0749-8063(98)70108-2. [DOI] [PubMed] [Google Scholar]
- 2.Mancini G.B., Lazzeri S., Bruno G., Pucci G. Localized pigmented villonodular synovitis of the knee. Arthroscopy. 1998;14(5):532–536. doi: 10.1016/s0749-8063(98)70086-6. [DOI] [PubMed] [Google Scholar]
- 3.De Ponti A., Sansone V., Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2003;19(6):602–607. doi: 10.1016/s0749-8063(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 4.Patel K.H., Gikas P.D., Pollock R.C. Pigmented villonodular synovitis of the knee: a retrospective analysis of 214 cases at a UK tertiary referral centre. Knee. 2017;24(4):808–815. doi: 10.1016/j.knee.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Temponi E.F., Barros A.A.G., Paganini V.O., Barbosa V.A.K., Badet R., Carvalho Júnior L.H. Diffuse pigmented villonodular synovitis in knee joint: diagnosis and treatment. Rev Bras Ortop. 2017;52(4):450–457. doi: 10.1016/j.rboe.2017.06.008. Published 2017 Jun 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verspoor F.G., Zee A.A., Hannink G., van der Geest I.C., Veth R.P., Schreuder H.W. Long-term follow-up results of primary and recurrent pigmented villonodular synovitis. Rheumatology. 2014;53(11):2063–2070. doi: 10.1093/rheumatology/keu230. [DOI] [PubMed] [Google Scholar]
- 7.Ogilvie-Harris D.J., McLean J., Zarnett M.E. Pigmented villonodular synovitis of the knee. The results of total arthroscopic synovectomy, partial, arthroscopic synovectomy, and arthroscopic local excision. J Bone Joint Surg Am. 1992;74(1):119–123. [PubMed] [Google Scholar]
- 8.Sharma V., Cheng E.Y. Outcomes after excision of pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 2009;467(11):2852–2858. doi: 10.1007/s11999-009-0922-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Capellen C.F., Tiling R., Klein A. Lowering the recurrence rate in pigmented villonodular synovitis: a series of 120 resections. Rheumatology. 2018;57(8):1448–1452. doi: 10.1093/rheumatology/key133. [DOI] [PubMed] [Google Scholar]
- 10.Colman M.W., Ye J., Weiss K.R., Goodman M.A., McGough R.L., 3rd Does combined open and arthroscopic synovectomy for diffuse PVNS of the knee improve recurrence rates? Clin Orthop Relat Res. 2013;471(3):883–890. doi: 10.1007/s11999-012-2589-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aurégan J.C., Klouche S., Bohu Y., Lefèvre N., Herman S., Hardy P. Treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2014;30(10):1327–1341. doi: 10.1016/j.arthro.2014.04.101. [DOI] [PubMed] [Google Scholar]
- 12.Mollon B., Lee A., Busse J.W. The effect of surgical synovectomy and radiotherapy on the rate of recurrence of pigmented villonodular synovitis of the knee: an individual patient meta-analysis. Bone Joint Lett J. 2015;97-B(4):550–557. doi: 10.1302/0301-620X.97B4.34907. [DOI] [PubMed] [Google Scholar]
- 13.Park G., Kim Y.S., Kim J.H. Low-dose external beam radiotherapy as a postoperative treatment for patients with diffuse pigmented villonodular synovitis of the knee: 4 recurrences in 23 patients followed for mean 9 years. Acta Orthop. 2012;83(3):256–260. doi: 10.3109/17453674.2012.678803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cassier P.A., Italiano A., Gomez-Roca C.A. CSF1R inhibition with emactuzumab in locally advanced diffuse-type tenosynovial giant cell tumours of the soft tissue: a dose-escalation and dose-expansion phase 1 study. Lancet Oncol. 2015;16(8):949–956. doi: 10.1016/S1470-2045(15)00132-1. [DOI] [PubMed] [Google Scholar]
- 15.Briggs K.K., Steadman J.R., Hay C.J., Hines S.L. Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med. 2009;37(5):898–901. doi: 10.1177/0363546508330149. [DOI] [PubMed] [Google Scholar]