Abstract
In this Technical Note, we discuss the combined hip arthroscopy and periacetabular osteotomy (PAO) for the treatment of symptomatic hip dysplasia, with a focus on the technique we use for the PAO. We identify modifications that can be made during the arthroscopic portion of the procedure to assist in the PAO dissection, including arthroscopic capsular closure and arthroscopic elevation of the iliocapsularis muscle off the capsule, which allows for expedited open exposure during the PAO.
Technique Video
This video demonstrates the authors technique of combined hip arthroscopy and periacetabular osteotomy, with a focus on arthroscopic modifications to improve and expedite the PAO exposure.
The Bernese periacetabular osteotomy (PAO) was first described in 1988 by Dr. Reinhold Ganz1 and remains today a very effective means of treating symptomatic dysplasia in the skeletally mature patient.2 It has been reported to have a 90% survivorship at 10 years, a 60% survivorship at 20 years,3 and a 29% survivorship at 30 years4 and the technique continues to evolve in ways that we hope will improve survivorship and patient satisfaction even further.3
The PAO technique as a stand-alone procedure has been described in detail,3,5 as well as the PAO in conjunction with hip arthroscopy,6, 7, 8, 9 and even an endoscopy-assisted PAO.10,11 Patients with symptomatic dysplasia have a very high incidence of intra-articular cartilage or labral damage, reported as high as 78% of prearthritic hips (in female adolescents aged 12-19 years) having cartilage damage and 78% having labral tears.12 It is for that reason that combining the PAO with concomitant hip arthroscopy can be a useful strategy to address all extra- and intra-articular pathology in one surgical setting in appropriately selected individuals with symptomatic hip pathology. There is also a high prevalence of cam deformity in patients with dysplasia, reported in one study to be 22% in dysplastic hips with Tönnis grade 0 or 1 and 50% in dysplastic hips with Tönnis grade 2, compared with 4.2% in nondysplastic hips.13 Cam decompression can be accomplished arthroscopically or after completion of the PAO in an open fashion. Both approaches are described in our technique. Notably, the addition of hip arthroscopy to PAO does not appear to increase complication rates when compared with PAO alone.14
Surgical Technique (With Video Illustration)
The described PAO technique can be applied to the PAO as a stand-alone surgery. However, within this Technical Note, we will highlight specific tips and tricks that apply to the PAO performed in combination with a hip arthroscopy. In the PAO/hip arthroscopy combined case, the hip arthroscopy takes place first.
Patient Indications and Preoperative Workup
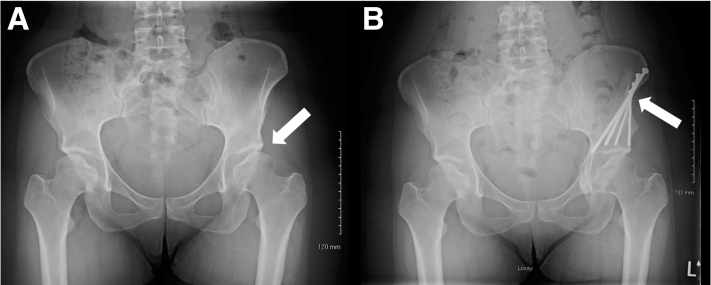
Patients are indicated for PAO if they are diagnosed with symptomatic hip dysplasia and have failed conservative measures. Preoperative workup includes radiographs (standing anteroposterior (AP) pelvis, false profile, 45° Dunn lateral, and Von Rosen), noncontrast hip magnetic resonance (MR) imaging (unless the patient has had previous hip surgery, in which case an MR arthrogram is obtained), and a low-dose 3-dimensional computed tomography scan per our hip-preservation reconstruction protocols (Fig 1). If the preoperative MR imaging demonstrates labral or other intra-articular pathology, which is symptomatic based on history and clinical examination, the patient will also be indicated for a concomitant hip arthroscopy surgery.
Fig 1.
(A) Standing anteroposterior pelvis (affected left hip marked with an arrow); (B) 45° Dunn lateral; (C) false profile; (D) Von Rosen radiographic views of the affected left hip; (E) sagittal fat-saturated magnetic resonance imaging of the affected left hip demonstrating labral tear (arrow); and (F) 3-dimensional computed tomography per our institutions hip preservation protocol, demonstrating left hip dysplasia (∗), a labral tear (arrow), and a cam lesion (@).
Hip Arthroscopy Immediately Preceding PAO
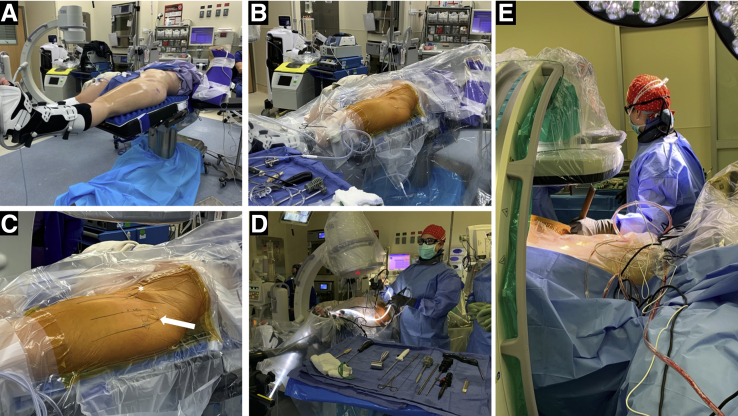
For the combined hip arthroscopy and PAO, the patient is placed supine on a traction table (Fig 2). The first author’s current preference is postless traction,15 but a post can be used for traction as well. A number of modifications are made in the hip arthroscopy that immediately precedes a PAO, as detailed in Spiker et al.’s “Modifications to Hip Arthroscopy Technique when Performing Combined Hip Arthroscopy & Periacetabular Osteotomy.8” Additional modifications in the hip arthroscopy technique when performed directly preceding an open PAO are listed in Table 1. While the cam can be addressed open, it is the first author’s preference to address the cam arthroscopically, fully repair the capsulotomy/capsulotomies arthroscopically, and perform a portion of the PAO dissection arthroscopically as well (Table 2). Once the capsulotomy/capsulotomies are completely repaired, thus restoring tension to the hip capsule, the radiofrequency ablation device is used to dissect the iliocapsularis muscle off the capsule (Video 1). Careful attention is paid to ensure the dissection is performed above the capsule, thus maintaining the integrity of the capsule. This dissection is carried medially until the psoas bursa is identified. Proximally, the iliocapsularis is dissected off the medial edge of the direct head of the rectus tendon as far as can be safely visualized (Video 1); the remaining fibers of the iliocapsularis attached to the rectus will be dissected from the medial rectus tendon during the open PAO exposure. Upon completion of the hip arthroscopy portion of the procedure, portals are closed with interrupted nylon suture. It is the first author’s current preference to perform the hip arthroscopy and PAO on the same radiolucent, postless traction table, thereby minimizing turnover time between the 2 procedures (Table 3).
Fig 2.
(A-D) Positioning for left hip arthroscopy. It is the first author’s current preference to use postless traction, but a post can be used for hip arthroscopy traction as well. The greater trochanter and anterior superior iliac spine are marked in (C), with an arrow and asterisk respectively. (E) Positioning and draping for the periacetabular osteotomy portion of the case.
Table 1.
Modifications in Hip Arthroscopy Procedure Directly Preceding PAO
| Central compartment |
| Perform an interportal capsulotomy that is as small as possible and located laterally (staying lateral to the direct head of the rectus origin if possible). |
| For labral repair, if 2 portals provide an adequate trajectory for suture anchor placement, 2 portals can be used (especially if the cam does not need to be addressed or will be addressed with an open capsulotomy after the PAO). |
| For labral repair, if a more distal-to-proximal trajectory is needed, as is often the case with a dysplastic acetabulum, a distal anterolateral accessory (DALA) portal can be created. This is the portal through which the first author prefers instruments when resecting the cam lesion if this is done arthroscopically. |
| For labral repair, the decision on whether to use simple suture repair or mattress suture repair is often dependent on the morphology and quality of the labral tissue. |
| Careful evaluation of the articular cartilage, on both the acetabular and femoral side, is performed. If cartilage wear is more significant than was estimated based on preoperative imaging, this may be the decision point on whether proceeding with the PAO is indicated. |
| Peripheral compartment |
| Traction is removed and the hip is flexed to 30-45°. Tension on the traction boots is released. |
| If there is no cam lesion to be addressed, or if the cam will be addressed via an open incision after the PAO, no additional peripheral compartment work is necessary. The interportal capsulotomy can be closed arthroscopically or via open repair after the PAO is completed. |
| If a cam lesion is present and will be addressed arthroscopically, instruments are inserted through the DALA portal. A T-capsulotomy can be made with a radiofrequency ablation device through this portal, if needed. The cam can then be resected with the burr. |
| It is the first author’s choice to close the T-capsulotomy and interportal capsulotomies arthroscopically to restore the tension to the hip capsule before performing further dissection in preparation for the PAO. |
| Dissection of the iliocapsularis off the hip capsule is performed with the radiofrequency ablation device. Care is taken to perform this dissection to minimize damage to the capsule as well as the iliocapsularis (Video 1). |
| The iliocapsularis dissection is carried medially off the capsule until the psoas bursa is identified. Proximally, the iliocapsularis is dissected off the medial edge of the direct head of the rectus tendon as far as can be safely visualized (Video 1); the remaining fibers of the iliocapsularis attached to the rectus will be dissected from the medial rectus tendon during the open PAO exposure. |
PAO, periacetabular osteotomy.
Table 2.
Advantages, Risks, and Limitations
| Advantages |
| Combining hip arthroscopy with PAO allows all intra-articular pathology to be addressed in the same surgical setting as acetabular reorientation. |
| The authors’ preferred technique of performing arthroscopic cam decompression, capsule closure, and dissection of the iliocapsularis off the capsule allows for time saved during the open PAO portion of the procedure. |
| Risks |
| Arthroscopic surgery can result in extra fluid extravasation and additional time of the procedure. |
| The patient must be transferred from the traction table to a radiolucent table, unless a single table technique is used. |
| Limitations: |
| The ability to perform the combined hip arthroscopy and open PAO requires a team of surgeons or a surgeon who can perform both the hip arthroscopy and open PAO. |
PAO, periacetabular osteotomy.
Table 3.
Equipment Required for Hip Arthroscopy Portion of Combined Hip Arthroscopy and PAO
| Hip arthroscopy |
| Crossflow Arthroscopy Pump (Stryker) |
| Pivot Guardian Distraction System (Stryker) |
| Suture passer: SlingShot, NanoPass (Stryker) |
| Suture: ORTHOCORD |
| Radiofrequency ablator: SERFAS (Stryker) |
| Shaver: 4-mm Tomcat (Stryker) |
| Beaver blade: Samurai (Pivot Medical) |
| Cannula: Transport (Pivot Medical) |
| Entry needles: Portal entry kit (Stryker) |
| Scope cannulas: FlowPort (Stryker) |
| Capsule cutting: Samurai Full Radius (Stryker) |
| Labral repair suture passer: NanoPass Crescent (Stryker) |
| Labral anchors: NanoTack Flex (Stryker) |
| Labral anchor drill bit: NanoTack Flex (Stryker) |
| Working cannula: 6.5-mm × 90-mm Dri-Lok (Stryker) |
| Capsule closure device: SlingShot 45° (Stryker) |
| Capsule closure suture: 1.2-mm Xbraid tape (Stryker) |
| Shaver blade: 3.5-mm dual edge (Stryker) |
| Burr: 5.5-mm round (Stryker) |
| PAO |
| Long osteotome: 15-in curved (Life Instruments) |
| Chandler elevator: 30-mm wide (Zimmer) |
| Cregos: 7.1-mm slightly curved, 7.1-mm acutely curved, 14.2-mm acutely curved (Zimmer) |
| 3/32 K-wire: 2.4-mm smooth (APEX Medical) |
| Lane elevator: with ring handle (Life Instruments) |
| Kocher Retractor: 8-inch, 9-inch, 10-inch (Smith & Nephew) |
PAO, periacetabular osteotomy.
Patient Positioning for PAO
The patient is supine on the radiolucent, postless traction table. The nonoperative leg is well padded and secured, ensuring that there is enough room on the table for a radiolucent triangle to be placed beneath the operative leg. Alternatively, if a postless radiolucent traction table is used for both the hip arthroscopy and PAO, the operative leg can be flexed/extended or adducted/abducted while in the traction boot (Fig 2). As a radiolucent, postless traction table is used for the arthroscopy portion of the case, the patient does not need to be re-prepped or draped for the PAO. At the beginning of the case, the arms are placed to the side of the patient. If the arms are crossed over the chest, they may block the appropriate placement of osteotomes during the posterior column cut. The arm on the operative side is carefully positioned to allow enough room for the surgeon to stand between the C-arm and arm board when the C-arm is used to visualize the “false profile” view during ischial and posterior column osteotomies and screw placement (Table 4).
Table 4.
C-arm Position and Leg Position During the Hip Arthroscopy and PAO Portion of the Case
| Leg Position | C-Arm Position | Portion of the Case |
|---|---|---|
| Hip arthroscopy | ||
| Straight, in traction | C-arm perpendicular to patient, straight AP | Central compartment work (labral repair, evaluation of articular cartilage) |
| Hip flexed 30-45o, traction removed | C-arm perpendicular to patient, rolled 15° under patient | Peripheral compartment work (cam decompression, elevation of iliocapsularis off capsule) |
| PAO | ||
| Straight | Not needed | Initial exposure |
| Flexed, knee over small radiolucent triangle∗ | Not needed | Medial exposure, to relax psoas tendon |
| Flexed, knee over small radiolucent triangle∗ | Not needed | Pubic osteotomy |
| Flexed, knee over small radiolucent triangle∗ | C-arm perpendicular to patient, straight AP and false profile | Ischial osteotomy, confirming location of osteotome and false profile confirming depth of osteotomy |
| Flexed, knee over small radiolucent triangle∗ | Not needed | Supracetabular osteotomy (performed after marking location of planned posterior column osteotomy) |
| Flexed, knee over small radiolucent triangle∗ | C-arm perpendicular to patient, false profile | Posterior column osteotomy |
| Flexed, knee over small radiolucent triangle,∗ leg abducted | C-arm perpendicular to patient, false profile | Lateral portion of posterior column osteotomy |
| Flexed, knee over small radiolucent triangle∗ | C-arm perpendicular to patient, straight AP (which matches preoperative standing AP pelvis) and false profile | Fragment fixation |
| Straight, with toes internally rotated 15° | Flat film | Confirming preliminary fixation |
AP, anteroposterior; PAO, periacetabular osteotomy.
When using a radiolucent postless traction table, the operative leg can also be flexed and extended while positioned in the traction boot, with extra padding.
Approach
Before the PAO incision is made, we administer 1 g of tranexamic acid to minimize bleeding (this is re-dosed 3 hours later). We use a bikini incision (Fig 3), starting at the medial most aspect approximately 2 cm below and 2 cm medial to the anterior superior iliac spine (ASIS), following a slightly curved trajectory just lateral to the iliac crest more superolaterally. The incision is carried through subcutaneous fat and Scarpa’s fascia. The ASIS osteotomy is marked (approximately 1 cm from tip of ASIS), and the inferior edge of the external oblique insertion on the iliac crest is marked. The external obliques are then elevated off the brim with an electrocautery device (Fig 3) The superficial fascia over the tensor fascia lata is incised. The tensor fascia lata is bluntly dissected free from the fascia and pulled laterally and the incision is carried proximally to the planed ASIS osteotomy site (Fig 3). The ASIS is osteotomized with a half inch osteotome, creating a wafer of bone that can later be sewn back to the ASIS. An electrocautery device is used to carry the dissection into the brim, elevating the iliacus subperiosteally. Once the RF is reached at the anterior inferior iliac spine (AIIS), the head of the RF is kept attached to the AIIS, and the dissection is carried medially (with the hip now flexed), subperiosteally, until the psoas tendon sheath is reached and pulled medially with a retractor.
Fig 3.
In this left hip: (A) planned incision for PAO; (B) identification of the lateral femoral cutaneous nerve (LCFN), marked with an arrow; this image shows a retractor in the interval between the TFL and RF, which was previously used to elevate the iliocapsularis off of the capsule—this is now not necessary if the iliocapsularis is arthroscopically elevated off of the capsule. (C) An anterior superior iliac spine osteotomy is created with a wafer of bone attached to the sartorius for future repair. A subperiosteal dissection is carried down the inner table toward the pelvic brim. (ASIS, anterior superior iliac spine; RF, rectus femoris; TFL, tensor fascia lata.)
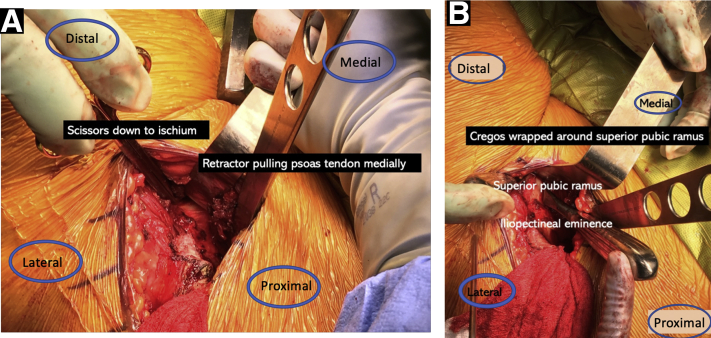
The Pubic Cut
Once the pubic ramus is reached, a spiked retractor is placed medially on the pubic ramus to retract the psoas tendon medially. Cregos are used to subperiosteally dissect around the superior posterior ramus and are kept in place to block the saw (Fig 4). An oscillating saw is used to cut the pubic ramus approximately 1.5 to 2 cm medial to the pectineal eminence. A small wedge of bone is taken here, and a stepped osteotome can be used to complete the cut.
Fig 4.
In this left hip: (A) the psoas tendon is retracted medially, revealing the plane between the capsule on the medial aspect of the femoral neck and the psoas bursa; (B) Crego retractors placed around the superior pubic ramus to protect the obturator canal just before performing the pubic osteotomy.
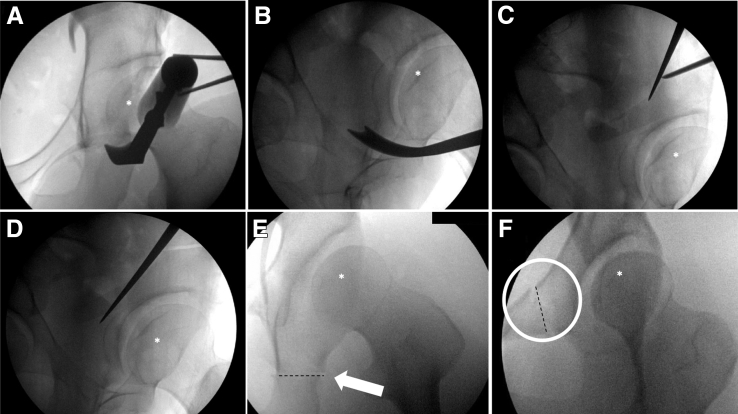
The Ischial Cut
The plane beneath the psoas fascia, but superficial to the hip capsule is dissected. Long curved mayo scissors are inserted above the capsule, wrapping around the inferior femoral neck, to the posterior structure of the ischium (Fig 4). The curved osteotome is inserted here and using fluoroscopic guidance (AP and false-profile view) the ischial cut is made, being careful to maintain the integrity of the posterior column (Fig 5).
Fig 5.
(A) Anteroposterior and (B) false-profile views used during the ischial cut for left hip periacetabular osteotomy; (C) marking the supra-acetabular and posterior column cuts; and (D) making the posterior column cut., (E) The completed ischial cut marked with an arrow and a dashed line. (F) the completed pubic cut marked with a circle and a dashed line. The femoral head is marked in each of the images (A-F) with an asterisk.
The Supracetabular Cut
The posterior column and supraacetabular osteotomies are marked with a straight osteotome using the false-profile view (Fig 5). A subgluteal window is created at the lateral ilium, and a Hohmann retractor is placed around the lateral ilium to protect the abductors from the saw. An oscillating saw is then used to complete the supraacetabular cut. It is after this cut that bleeding from the nutrient vessel can be expected.
The Posterior Column Cut
Using both the AP and false-profile views, the straight osteotome is advanced down the posterior column, maintaining the integrity of the posterior column (Fig 5). Once the osteotome is distal to the joint, an angled osteotome is used to complete the cut (Fig 5), connecting the osteotomy to the prior ischial osteotomy. A long curved osteotome can be used to completely connect these osteotomies (Fig 5).
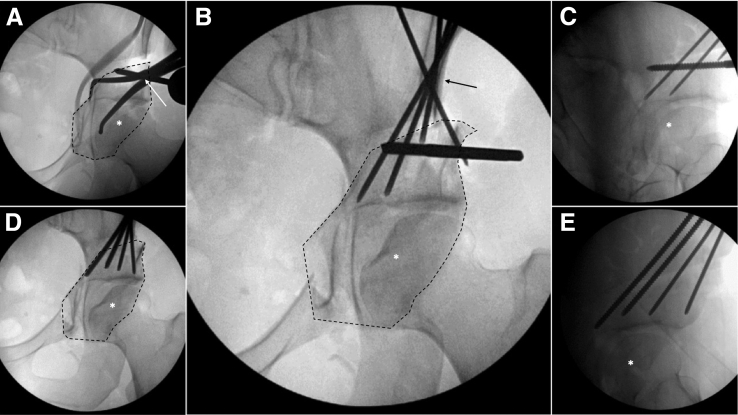
Mobilizing the Fragment
An angled osteotome can be directed laterally to complete the posterolateral osteotomy of the fragment. Care is taken when completing the lateral most aspects of the osteotomy not to damage the abductors and to keep in mind the location of the sciatic nerve. The leg can be abducted to distance the sciatic nerve from the osteotomy. A Shanz pin is placed at the superior aspect of the fragment, and a large Weber clamp is placed around the pubic root (Fig 6A).
Fig 6.
Left hip intraoperative fluoroscopic images demonstrating: (A) Shanz pin and Weber clamp, marked with an arrow in place, mobilizing the fragment (outlined); (B) anteroposterior (AP) pelvis 2.4-mm K wires in place, provisionally fixing the fragment (outlined) in its new orientation; (C) a false profile view demonstrating the 2.4-mm K wires provisionally fixing the fragment in place; (D) AP, with the fragment outlined, and (E) false-profile views demonstrating screws in place (two 3.5-mm screws anteriorly and two 4.5-mm screws posteriorly). The femoral head is marked in each of the images (A-E) with an asterisk.
Changing Acetabular Orientation
The goals of reorientation are to appropriately lateralize the fragment while maintaining anteversion of the fragment. We also medialize the joint by appropriately seating the fragment medially. The Shanz pin and Weber clamp can be used to mobilize the fragment and obtain the appropriate lateral coverage, anteversion and medialization of the fragment (Fig 6A). Additionally, medially directed pressure at the greater trochanter (while simultaneously moving the fragment) as well as a ball spike placed on the fragment to direct it can aid in fragment orientation.
Fixation
Temporary fixation is achieved with 2.4-mm Kirschner wires (Fig 6 B and C). The AP pelvis is mimicked on fluoroscopy to match the patient’s preoperative standing AP pelvis radiograph (Fig 7 A and B). This can be achieved by placing the table in Trendelenburg/reverse Trendelenburg or airplaning the table left or right. The fluoroscopy also can be moved to create more inlet/outlet or over/under views. Once the position is confirmed, it is the authors’ preference to place a total of 4 noncannulated screws, with the anterior two 3.5 mm and the posterior two 4.5 mm. Additional screws or variations in the size of the screws can be made as needed (Fig 6 D and E).
Fig 7.
Side-by-side (A) pre- and (B) postoperative standing anteroposterior pelvis radiograph with (A) the affected left hip and (B) periacetabular osteotomy screws marked by an arrow.
Additional Procedures
Hip motion is assessed at the completion of the PAO before closure. Subspine decompression can be performed if subspine impingement is noted by using a burr beneath the origin of the rectus femoris on the AIIS. If the cam decompression was not performed arthroscopically, it can now be performed by retracting the rectus tendon and extending the capsulotomy.
Closure
Capsule closure can be performed with a UR6 curved needle if not performed arthroscopically. Retraction of the rectus will allow for visualization of the capsulotomy. It is the first author’s preference to close the capsule arthroscopically. The ASIS wafer is sutured back to the intact iliac crest by heavy nonabsorbable suture. The external oblique and tensor fascia is closed with 0-VICRYL suture, and a layered closure is used, reapproximating Scarpa’s fascia as well as the subcutaneous tissue. A 3-0 MONOCRYL absorbable suture is used for skin closure, with Steri-Strips placed on top.
Postoperative Rehabilitation
Patients usually remain in the hospital for 2 nights. The epidural is removed postoperative day 1. Ketorolac is available for the first 24 hours for pain control. Acetaminophin is available for the duration of the inpatient stay. Opioids are prescribed as needed. For deep-vein thrombosis chemoprophylaxis, heparin is given subcutaneously while the epidural is in place. Enoxaparin is given subcutaneously while the patient is in the hospital after the epidural is removed. Compression stockings and sequential compression devices are used during the inpatient stay. The patient is discharged home with compression stockings for 4 weeks and aspirin BID for 4 weeks. Continuous passive motion is used for 2 hours, 3 times per day, beginning at 30-70° and advancing to 0-90° as tolerated. Indomethacin 75 mg is used starting on postoperative day 1 for 4 days for heterotopic ossification prophylaxis after completion of ketorolac. Gastrointestinal chemoprophylaxis is prescribed for 30 days. We allow partial weight-bearing (20% of body weight) on the operative leg for 6 weeks, using crutches for ambulation.
Discussion (With Video Illustration)
PAO is a very effective treatment for developmental dysplasia of the hip in the skeletally mature patient and has been shown to positively alter the natural history of developmental dysplasia of the hip.2,16 The combination of hip arthroscopy with PAO allows the surgeon to address all intra-articular pathology in one surgical setting, with excellent outcomes, no effect on PAO radiographic correction achievement, and no increase in surgical complications.14,17,18
In this Technical Note, we focus on our preferred technique for the PAO and additionally describe modifications that can be applied to the hip arthroscopy portion of the case to allow for an easier dissection during the PAO, specifically minimizing the size of the interportal capsulotomy, consideration of arthroscopic capsule closure, and dissection of the iliocapsularis off the capsule medial to the psoas bursa (Table 5). Dysplastic hips have a high incidence of intra-articular cartilage damage (as high as 78%12 in cam lesions in patients with hip dysplasia, described to be as high as 50% in dysplastic patients with Tönnis grade 2), and therefore the addition of hip arthroscopy can allow the surgeon to address all intra-articular pathology in the same surgical setting as the PAO.
Table 5.
Pearls and Pitfalls
| Pearls | Pitfalls | |
|---|---|---|
| Hip arthroscopy |
|
Separate traction table must be used with separate prepping and draping (although a single table for both procedures has been described previously and in our technique)15 |
| Arthroscopic cam resection | Arthroscopic cam resection can be performed immediately after central compartment work is performed | Adds additional time to the arthroscopic portion of the case, including additional fluid extravasation |
| Arthroscopic capsule closure | Arthroscopic capsule closure can be performed | Adds additional time to the arthroscopic portion of the case, including additional fluid extravasation |
| Arthroscopic dissection of iliocapsularis off capsule | Allows for direct visualization of the iliocapsularis and is easily addressed after capsule closure (Video 1) |
|
| PAO | A proven procedure to address hip dysplasia with long term outcomes reflecting a reversal in the natural history of hip dysplasia | Separate radiolucent table must be used with separate prepping and draping (though a single table for both procedures has been described previously and in our technique)15 |
| Open cam resection | Open cam resection can be performed after completion of the PAO by performing a capsulotomy through the already exposed capsule |
|
| Open capsule closure |
|
|
PAO, periacetabular osteotomy.
The combined arthroscopic and open portions of this surgery allow flexibility in addressing coexisting cam lesions and performing capsule closure. These 2 portions of the procedure can be performed arthroscopically or open based on surgeon preference. We discuss both approaches in our technique, though the first author’s preference is to perform both arthroscopically. The maximum alpha angle in dysplastic hips is at the 2-o’clock position,13 which can sometimes be difficult to access through an open incision. Capsule closure can be performed open after completion of the PAO but does require retraction to identify the capsulotomy, and extra care must be taken not to incorporate the labrum in the repair of the proximal capsular flap. When capsule closure is performed arthroscopically it can restore the capsular tension before performing the iliocapsularis dissection off the capsule medially to the psoas bursa. The iliocapsularis dissection, if not performed arthroscopically, can be performed via the open approach, but visualization is significantly better when performed arthroscopically and does not require excessive retraction as it does with the open approach (Video 1). The PAO technique is highlighted in this manuscript and can be augmented by the addition of arthroscopy as described herein.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.C.G. reports personal fees from Synthes, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the authors’ technique of combined hip arthroscopy and periacetabular osteotomy, with a focus on arthroscopic modifications to improve and expedite the PAO exposure.
References
- 1.Ganz R., Klaue K., Vinh T.S., Mast J.W. A new periacetabular osteotomy for the treatment of hip dysplasias: Technique and preliminary results. 1988. Clin Orthop Relat Res. 2004;(418):3–8. [PubMed] [Google Scholar]
- 2.Clohisy J.C., Ackerman J., Baca G., et al. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J Bone Joint Surg. 2017;99:33–41. doi: 10.2106/JBJS.15.00798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Büchler L., Beck M. Periacetabular osteotomy: A review of swiss experience. Curr Rev Musculoskelet Med. 2014;7:330–336. doi: 10.1007/s12178-014-9232-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lerch T.D., Steppacher S.D., Liechti E.F., Tannast M., Siebenrock K.A. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res. 2017;475:1154–1168. doi: 10.1007/s11999-016-5169-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganz R., Klaue K., Vinh T.S., Mast J.W. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;(232):26–36. [PubMed] [Google Scholar]
- 6.Domb B., LaReau J., Redmond J.M., Redmond J.M. Combined hip arthroscopy and periacetabular osteotomy: Indications, advantages, technique, and complications. Arthrosc Tech. 2014;3:e95–e100. doi: 10.1016/j.eats.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maldonado D.R., LaReau J.M., Lall A.C., Battaglia M.R., Mohr M.R., Domb B.G. Concomitant arthroscopy with labral reconstruction and periacetabular osteotomy for hip dysplasia. Arthrosc Tech. 2018;7:e1141–e1147. doi: 10.1016/j.eats.2018.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spiker A.M.A.M., Gumersell K.R.K.R., Sink E.L.E.L., Kelly B.T.B.T. Modifications to the hip arthroscopy technique when performing combined hip arthroscopy and periacetabular osteotomy. Arthrosc Tech. 2017;6:e1857–e1863. doi: 10.1016/j.eats.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Domb B.G., Lareau J.M., Hammarstedt J.E., Gupta A., Stake C.E., Redmond J.M. Concomitant hip arthroscopy and periacetabular osteotomy. Arthroscopy. 2015;31:2199–2206. doi: 10.1016/j.arthro.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Matsuda D.K., Martin H.D., Parvizi J. Endoscopy-assisted periacetabular osteotomy. Arthrosc Tech. 2016;5:e275–e280. doi: 10.1016/j.eats.2016.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsuda D.K., Matsuda N.A. Endoscopic hip osteotomies: Less invasive approaches to peri-acetabular, proximal femoral and pubic symphyseal procedures. J hip Preserv Surg. 2015;2:108–115. doi: 10.1093/jhps/hnv025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujii M., Nakashima Y., Jingushi S., et al. Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9–13. doi: 10.1097/BPO.0b013e318190a0be. [DOI] [PubMed] [Google Scholar]
- 13.Kohno Y., Nakashima Y., Hatano T., et al. High prevalence of cam deformity in dysplastic hips: A three-dimensional CT study. J Orthop Res. 2016;34:1613–1619. doi: 10.1002/jor.23147. [DOI] [PubMed] [Google Scholar]
- 14.Sabbag C.M., Nepple J.J., Pascual-Garrido C., Lalchandani G.R., Clohisy J.C., Sierra R.J. The addition of hip arthroscopy to periacetabular osteotomy does not increase complication rates: A prospective case series. Am J Sports Med. 2019;47:543–551. doi: 10.1177/0363546518820528. [DOI] [PubMed] [Google Scholar]
- 15.Woyski D., Olson S., Lewis B. Single table concomitant post-less hip arthroscopy combined with periacetabular osteotomy for hip dysplasia. Arthrosc Tech. 2019;8:e1569–e1578. doi: 10.1016/j.eats.2019.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wyles C.C., Vargas J.S., Heidenreich M.J., et al. Natural history of the dysplastic hip following modern periacetabular osteotomy. J Bone Joint Surg Am. 2019;101:932–938. doi: 10.2106/JBJS.18.00983. [DOI] [PubMed] [Google Scholar]
- 17.Ricciardi B.F., Mayer S.W., Fields K.G., Wentzel C., Kelly B.T., Sink E.L. Patient characteristics and early functional outcomes of combined arthroscopic labral refixation and periacetabular osteotomy for symptomatic acetabular dysplasia. Am J Sports Med. 2016;44:2518–2525. doi: 10.1177/0363546516651829. [DOI] [PubMed] [Google Scholar]
- 18.Maldonado D.R., LaReau J.M., Perets I., et al. Outcomes of hip arthroscopy with concomitant periacetabular osteotomy, minimum 5-year follow-up. Arthroscopy. 2019;35:826–834. doi: 10.1016/j.arthro.2018.10.143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the authors technique of combined hip arthroscopy and periacetabular osteotomy, with a focus on arthroscopic modifications to improve and expedite the PAO exposure.
This video demonstrates the authors’ technique of combined hip arthroscopy and periacetabular osteotomy, with a focus on arthroscopic modifications to improve and expedite the PAO exposure.