Abstract
Fewer respiratory syncytial virus infections were observed in 2020-2021 with interseasonal resurgence. Children were more likely to have severe disease with less known risk factors in comparison with controls from 2018-2019. The overall codetection rates were similar, but with higher parainfluenza, rhinovirus/enterovirus, and lower influenza proportions compared with previous seasons.
Keywords: COVID-19, Coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus2; RSV, respiratory syncytial virus
Coronavirus disease 2019 (COVID-19) had an impact on the epidemiology of respiratory syncytial virus (RSV) during the 2020-2021 winter season in the US.1 These epidemiologic changes could be related to interactions between respiratory viruses and/or ongoing COVID-19 mitigation efforts. We describe RSV infections at a children’s hospital during the first winter RSV season (2020-2021) since the advent of COVID-19 and compare the epidemiology of these infections with RSV infections in previous seasons. We hypothesized that the public health mitigation measures implemented in response to the pandemic would decrease the overall rates of medically attended RSV, similar to observations made for influenza and RSV in early 2020, but that the characteristics of these patients would be similar to the characteristics of patients with RSV in previous seasons.2
Methods
We conducted a retrospective review of children and adolescents with RSV who presented to the New York-Presbyterian Morgan Stanley Children’s Hospital Emergency Department and had a positive test for RSV on nasal swab samples tested by a multiplex reverse transcriptase polymerase chain reaction assay (FilmArray Panel, BioFire Diagnostics, Inc). Children attended only in the emergency department were offered testing with multiplex reverse transcriptase-polymerase chain reaction at the discretion of the treating physician. Testing availability for this assay did not change during the study period.
To assess changes in the epidemiology of medically attended RSV, we identified cases age 21 years or younger from November 1 to April 30 during 3 respiratory viral seasons (2018-2019, 2019-2020, and 2020-2021). A broader age group was selected to fully ascertain potential epidemiologic changes.
We compared the demographic and clinical characteristics of RSV cases identified during the 2020-2021 season and an equal number of randomly selected RSV cases from 2018-2019. The 2018-2019 season was selected instead of the 2019-2020 because state-wide mitigation measures were implemented in March 2020 and circulation of SARS-CoV-2 in New York City likely occurred before March 2020.3 We excluded patients with codetections of other respiratory pathogens from this analysis. For each patient, we collected presenting symptoms, clinical syndromes (bronchiolitis, croup, asthma/reactive airway disease exacerbation) noted in the electronic medical record by attending physicians, comorbidities (prematurity, cardiac disease, asthma/reactive airway disease), sick contacts if noted, and severity of disease (defined as inpatient hospitalization, oxygen saturation ≤94% at presentation, and/or the need for respiratory support).
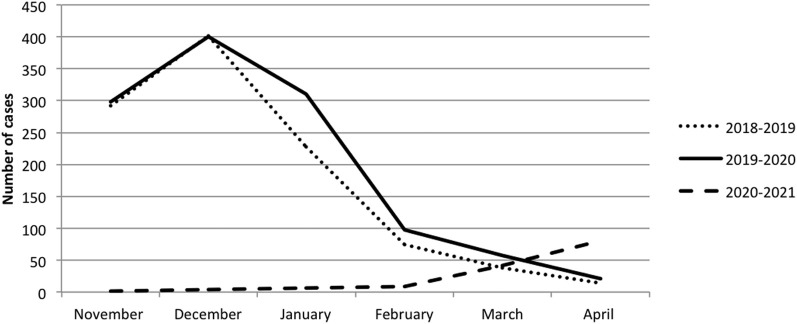
Second, we graphically compared the number and temporal distribution of cases between years. Last, we compared the overall proportion and distribution of other respiratory virus codetections among all 3 seasons. Categorical and continuous variables were compared using the Fisher exact, χ2, and Wilcoxon rank-sum test, as appropriate. The Columbia University Irving Medical Center Institutional Review Board approved the study.
Results
During the 2020-2021 season, 143 children and adolescents had medically attended RSV. Of these, 90 had only RSV detected. The overall number of RSV cases decreased in 2020-2021 compared with both the 2018-2019 and 2019-2020 seasons with differing epidemiologic curves (Figure ). Compared with RSV cases without codetection identified in 2018-2019 (n = 90), RSV cases in 2020-2021 (n = 90) had similar median age, proportions of prematurity, and cardiac disease, but less asthma/reactive airway disease and more croup at presentation (Table I ). Significantly more cases in 2020-2021 were hospitalized and required oxygen supplementation.
Figure.
Comparison of epidemiologic curves of medically attended RSV during 3 winter respiratory viral seasons (2018-2019, 2019-2020, and 2020-2021).
Table I.
Characteristics of patients with RSV during the 2020-2021 season vs the 2018-2019 season
| Characteristics | RSV cases (2020-2021), n = 90 | RSV cases (2018-2019), n = 90 | P value |
|---|---|---|---|
| Median age in months (IQR) | 9.5 (1-28) | 8.5 (4-24) | .61∗ |
| Age categories | .03 | ||
| ≤12 months | 49 (54.4%) | 58 (64.4%) | |
| 13-24 months | 17 (18.9%) | 14 (15.6%) | |
| 25-35 months | 8 (8.9%) | 1 (1.1%) | |
| 3-6 years | 11 (12.2%) | 13 (14.4%) | |
| 7-11 years | 5 (5.6%) | 1 (1.1%) | |
| 12-17 years | 0 (0%) | 3 (3.3%) | |
| Reported sick contacts | 40 (44.4%) | 34 (37.8%) | .36 |
| Comorbid conditions | |||
| Prematurity | 7 (7.8%) | 13 (14.4%) | .16 |
| Asthma/reactive airway disease | 4 (4.4%) | 13 (14.4%) | .02 |
| Congenital cardiac disease | 4 (4.4%) | 3 (3.3%) | .63 |
| Clinical syndromes | |||
| Bronchiolitis | 61 (67.8%) | 52 (57.8%) | .58 |
| Croup | 5 (5.6%) | 0 (0.0%) | .019 |
| Asthma exacerbation | 0 (0%) | 9 (10.0%) | .02 |
| Hospital admission | 59 (65.6%) | 42 (46.7%) | .01 |
| Hypoxemia/oxygen requirement | 44 (48.9%) | 25 (27.8%) | .04 |
Values are number (%).
Wilcoxon signed-rank test.
The overall proportion of viral codetections was similar across the 3 seasons, but the distribution of some pathogens differed (Table II; available at www.jpeds.com). Rhinovirus/enterovirus was most commonly codetected in all 3 seasons, with the highest proportion of rhinovirus/enterovirus noted in 2020-2021. Parainfluenza viruses were detected at a significantly higher rate in 2020-2021 than previous seasons.
Discussion
Lower numbers of medically attended RSV were observed in the first winter since the onset of the COVID-19 pandemic in New York City, as described in the southern hemisphere.4 Possibly consistent with our hypothesis, that anti-severe acute respiratory syndrome coronavirus (SARS-CoV-2) mitigation measures were instrumental in this decrease, current and comparator season were similar in multiple aspects (median age, bronchiolitis as the predominant syndrome, and proportion of viral codetections). However, there were some epidemiologic differences. Despite lack of known risk factors, a greater proportion of children had severe disease in 2020-2021. This finding could potentially reflect families’ avoiding emergency room care for milder illness during the pandemic. Lower rates of asthma exacerbations have been noted during COVID-19, so it is intriguing that in the 2020-2021 RSV cohort, asthma was a less common presentation.5
Differences in the distribution of some codetected viruses were observed. Parainfluenza was significantly higher and lower proportions of influenza and higher proportions of rhinovirus/enterovirus were observed. This could arise from the varying impact of mitigation measures on transmission of specific viruses or the interaction of SARS-CoV-2 with these viruses in the larger population. The increase in RSV cases at the end of winter into early spring has been observed throughout New York state and suggests interseasonal RSV resurgence associated with the relaxation of COVID-19 preventive efforts similar to observations in Australia.1 , 6 This finding has implications for the duration of palivizumab prophylaxis that may need to be tailored more specifically to local epidemiology of RSV. In our institution, palivizumab prophylaxis was extended as per the recommendation of the department of health. Limitations of this study include possible differences in health seeking behavior or testing biases between seasons. Ongoing RSV surveillance is essential to fully explore the continuing impact of the COVID-19 pandemic.
Footnotes
The authors declare no conflicts of interest.
Appendix
Table II.
Codetection of another respiratory virus with RSV each season∗
| Season 2018-2019 | Season 2019-2020 | Season 2020-2021 | |
|---|---|---|---|
| Total cases positive for RSV | 1036 | 1162 | 143 |
| Codetection of another respiratory virus | 354 (34.2%) | 368 (31.7%) | 50 (34.9%) |
| Rhinovirus/enterovirus | 157 (15.2%) | 148 (12.7%)† | 29 (20.3%) |
| Influenza | 30 (2.9%) | 41 (3.5%) | 0 (0%) |
| Coronavirus | 96 (9.3%) | 108 (9.3%) | 11 (7.7%) |
| Parainfluenza | 19 (1.8%)† | 13 (1.1%)† | 8 (5.6%) |
| Human metapneumovirus | 13 (1.3%) | 6 (0.5%) | 0 (0%) |
| Adenovirus | 67 (6.5%) | 87 (7.5%) | 13 (9.1%) |
| SARS-CoV-2 | 0 (0%) | 0 (0%) | 1 (1.6%) |
RSV, respiratory syncytial virus; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Children had coinfections with >1 virus.
Comparator season proportion significantly different from the 2020 to the 2021 season (P < .05).
References
- 1.The National Respiratory and Enteric Virus Surveillance System (NREVSS)-Respiratory Syncytial Virus Surveillance RSV State Trends Web site. https://www.cdc.gov/surveillance/nrevss/rsv/state.html - NY
- 2.Sherman A.C., Babiker A., Sieben A.J., Pyden A., Steinberg J., Kraft C.S., et al. The effect of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) mitigation strategies on seasonal respiratory viruses: a tale of 2 large metropolitan centers in the United States. Clin Infect Dis. 2021;72:e154–e157. doi: 10.1093/cid/ciaa1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stadlbauer D., Tan J., Jiang K., Hernandez M.M., Fabre S., Amanat F., et al. Repeated cross-sectional sero-monitoring of SARS-CoV-2 in New York City. Nature. 2021;590:146–150. doi: 10.1038/s41586-020-2912-6. [DOI] [PubMed] [Google Scholar]
- 4.Yeoh D.K., Foley D.A., Minney-Smith C.A., Martin A.C., Mace A.O., Sikazwe C.T., et al. The impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72:2199–2202. doi: 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah S.A., Quint J.K., Nwaru B.I., Sheikh A. Impact of COVID-19 national lockdown on asthma exacerbations: interrupted time-series analysis of English primary care data. Thorax. 2021;76:860–866. doi: 10.1136/thoraxjnl-2020-216512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foley D.A., Yeoh D.K., Minney-Smith C.A., Martin A.C., Mace A.O., Sikazwe C.T., et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021;73:e2829–e2830. doi: 10.1093/cid/ciaa1906. [DOI] [PMC free article] [PubMed] [Google Scholar]