Over 200 million people globally have been infected with the severe acute respiratory syndrome coronavirus 2, also known as coronavirus disease 2019 (COVID-19).1 Some COVID-19 survivors recover from acute infection yet suffer from persistent symptoms including fatigue, anxiety, and depression.2 New, chronic gastrointestinal (GI) symptoms are also commonly reported after COVID-19.3, 4, 5, 6, 7 There is an established association between mental health symptoms and chronic GI symptoms, especially irritable bowel syndrome (IBS).8 , 9 However, the association between mental health symptoms and chronic GI symptoms after COVID-19 has not been fully explored.
The Columbia University Institutional Review Board approved this study. This survey study, nested within a prospective cohort of COVID-19 survivors with a minimum of 6 months of follow-up, assessed the hypothesis that mental health symptoms both before and after COVID-19 infection would be associated with post–COVID-19 chronic GI symptoms (see Supplementary Methods for full study details). Of 1783 patients surveyed, 749 (42%) responded (67% women; median age, 43 years). The cohort comprised 61% white, 9.6% black, and 20% other races (with 9.6% choosing not to answer) and 28% Hispanic and 70% non-Hispanic (with 2% choosing not to answer). The survey was completed in English by 93% of respondents and in Spanish by 6.8%. Fifteen percent of patients had been hospitalized for COVID-19, with 1.7% requiring mechanical ventilation.
Six months after COVID-19 diagnosis, 220 patients (29%) reported GI symptoms self-perceived to be related to COVID-19. These included 72 (9.6%) with diarrhea, 83 (11%) with constipation, 70 (9.4%) with abdominal pain, 53 (7.1%) with nausea/vomiting, and 122 (16%) with heartburn (Table 1 ). A GI symptom was the most bothersome current symptom in 83 patients (11%).
Table 1.
Prevalence, Severity, and Frequency of Specific GI Symptoms 6 Months After COVID-19 Diagnosis (N = 749)
| Diarrhea | Constipation | Abdominal pain | Nausea/vomiting | Reflux or heartburn | Any GI symptom | |
|---|---|---|---|---|---|---|
| Mental health symptomsa | ||||||
| None | 20 (27.8) | 18 (21.7) | 13 (18.6) | 8 (15.1) | 33 (27.1) | 67 (30.5) |
| Pre–COVID-19 only | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Post–COVID-19 only | 42 (58.3) | 55 (66.3) | 48 (68.6) | 38 (71.7) | 76 (62.3) | 134 (60.9) |
| Pre– and post–COVID-19 | 10 (13.9) | 10 (12.1) | 9 (12.9) | 7 (13.2) | 13 (10.7) | 19 (8.6) |
| Overall reporting symptom | 72 (9.6) | 83 (11.1) | 70 (9.4) | 53 (7.1) | 122 (16.3) | 220 (29.4) |
| Most bothersome symptom | 10 (1.3) | 25 (3.3) | 18 (2.4) | 11 (1.5) | 46 (6.1) | 83 (11.1) |
| Severity (% reporting each severity among all patients with the symptom) | ||||||
| Very mild | 24 (33.3) | 29 (34.9) | 23 (32.9) | 23 (43.4) | 45 (36.9) | 85 (38.6) |
| Mild | 25 (34.7) | 25 (30.1) | 18 (25.7) | 16 (30.2) | 33 (27.1) | 61 (27.7) |
| Moderate | 13 (18.1) | 8 (9.6) | 15 (21.4) | 4 (7.6) | 22 (18.0) | 32 (14.6) |
| Severe | 8 (11.1) | 12 (14.5) | 7 (10.0) | 7 (13.2) | 12 (9.8) | 25 (11.4) |
| Very severe | 2 (2.8) | 9 (10.8) | 7 (10.0) | 3 (5.7) | 10 (8.2) | 17 (7.7) |
| Frequency (% reporting each frequency among all patients with the symptom)b | ||||||
| (n = 67) | (n = 82) | (n = 67) | (n = 47) | (n = 121) | (n = 214) | |
| Occasionally | 28 (41.8) | 20 (24.4) | 24 (35.8) | 23 (48.9) | 30 (24.8) | 63 (29.4) |
| Sometimes | 23 (34.3) | 30 (36.5) | 27 (40.3) | 16 (34.0) | 40 (33.1) | 72 (33.6) |
| Often | 13 (19.4) | 18 (22.0) | 11 (16.4) | 7 (14.9) | 36 (29.8) | 52 (24.3) |
| Always | 3 (4.5) | 14 (17.1) | 5 (7.5) | 1 (2.1) | 15 (12.4) | 27 (12.6) |
NOTE. Values are n (%).
Row percentages stratified by mental health symptoms are as follows: None, 67/459 (14.6%) with GI symptoms; Pre–COVID-19 only, 0/10 (0%) with GI symptoms; Post–COVID-19 only, 134/251 (53.4%) with GI symptoms; Pre– and post–COVID-19, 19/29 (65.5%) with GI symptoms.
Values of n are lower because some respondents who reported a symptom did not report frequency.
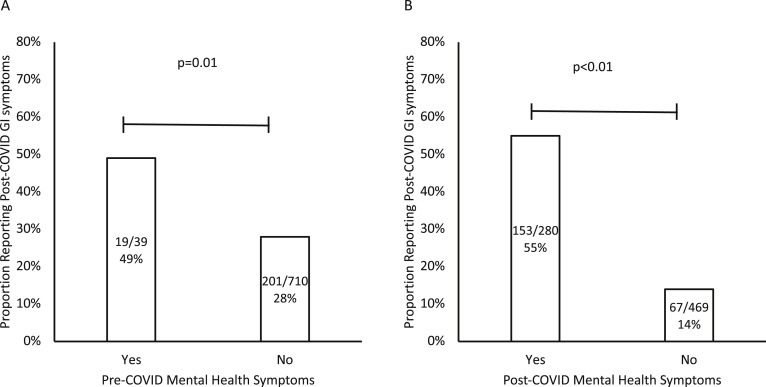
Thirty-nine patients (5.2%) reported pre–COVID-19 mental health symptoms (which were not further classified in the survey), and 280 (37%) reported post–COVID-19 mental health symptoms (27% with sadness, 34% with anxiety). Patients with pre–COVID-19 mental health symptoms were more likely than those without to report GI symptoms post–COVID-19 (49% vs 28%, respectively; P = .01) (Table 1 and Supplementary Figure 1A). Similarly, patients who reported sadness or anxiety post–COVID-19 were more likely to also have GI symptoms post–COVID-19 (55% with sadness/anxiety vs 14% without, P < .01) (Table 1 and Supplementary Figure 1B). Of the 39 patients reporting pre–COVID-19 mental health symptoms, 29 (74%) reported current anxiety or sadness and 19 (49%) reported current GI symptoms, all of whom also reported current sadness or anxiety. The likelihood of sadness or anxiety increased with more severe GI symptoms (Cochran-Armitage test for trend P = .02).
Supplementary Figure 1.
Prevalence of post–COVID-19 GI symptoms (A) in patients with and without pre–COVID-19 mental health symptoms and (B) in patients with and without post–COVID-19 mental health symptoms.
On multivariable logistic regression, the presence of both pre– and post–COVID-19 mental health symptoms was significantly associated with post–COVID-19 GI symptoms (adjusted odds ratio [aOR], 16.5; 95% confidence interval [CI], 6.97–38.9), as was post–COVID-19 mental health symptoms alone (aOR, 6.16; 95% CI, 4.21–9.01) (Supplementary Table 1).
Neither black race nor Hispanic ethnicity was associated with GI symptoms after COVID-19, although preference for the Spanish language was (aOR, 2.55; 95% CI, 1.14–5.73). This discrepancy may represent subtle differences in translation or unmeasured factors—such as access to care, socioeconomic status, or strength of social networks—that fundamentally differ between Hispanics who do or do not prefer Spanish.
Of 33 patients with abdominal pain that started after COVID-19 who answered additional questions pertaining to IBS, 13 (39%) reported having pain at least weekly that was associated with a change in stool form or frequency, with onset at least 6 months prior, and thus met Rome IV criteria for IBS. Women were no more likely than men to report post–COVID-19 GI symptoms (P = .63) or to meet criteria for IBS (P = .56).
Of 110 patients hospitalized with COVID-19, 51% reported post–COVID-19 GI symptoms compared with 26% of nonhospitalized patients (P < .01). This association remained significant on multivariable analysis (aOR, 2.30; 95% CI, 1.38–3.84), suggesting that more severe infection may be an important risk factor for post–COVID-19 GI symptoms.
Overall, these results highlight the potential bidirectionality of mental health and chronic GI symptoms after COVID-19, as has previously been observed in non–COVID-19 studies. Anxiety or sadness may exacerbate functional GI symptoms, and functional GI symptoms may lead to anxiety or sadness.10 Alternatively, a common underlying mechanism could explain both GI and mental health symptoms. This study, which involved an assessment made at a single time point, cannot fully determine the temporality between mental health and GI symptoms after COVID-19. This may be a fruitful area for future studies that can use longitudinal assessment strategies to tease apart the causal chain of events and evaluate strategies to improve long-term GI outcomes after COVID-19. Although all patients with chronic GI symptoms should receive screening for comorbid mental health symptoms, this study provides specific evidence that screening COVID-19 survivors will be high yield.
The study has some limitations. The response rate was 42%, raising the possibility of response bias, but, reassuringly, the estimate of prevalence for new GI symptoms after COVID-19 (29%) fell squarely in the middle of the range of 16%–40% from a retrospective study.7 Although post–COVID-19 symptoms were assessed prospectively, reporting of mental health symptoms before COVID-19 was assessed retrospectively and may have been under-reported because of recall bias related to the stigma of such symptoms. Because the survey instrument from which these data were generated was focused primarily on new physical symptoms after COVID-19, there was limited detail on the characteristics of current mental health symptoms. Importantly, the association found between mental health symptoms and GI symptoms after COVID-19 is not necessarily causal. It is possible that post–COVID-19 GI symptoms may be partially due to heightened stress and anxiety arising from pandemic-related lifestyle changes rather than the direct consequence of severe acute respiratory syndrome coronavirus 2 infection. In future studies, a control group assessing the incidence of new GI symptoms in patients who tested negative for COVID would help to clarify this question.
In summary, we observed very strong associations between mental health symptoms and post–COVID-19 GI symptoms. Nearly one-third of patients (29%) reported at least 1 new GI symptom after COVID-19. These were not trivial, because over 10% of the cohort reported a GI symptom as their most bothersome COVID-19–related condition.
Acknowledgment
The authors thank Sheila O'Byrne for her assistance with the Columbia University COVID-19 Biobank (CUB) data.
CRediT Authorship Contributions
John William Blackett, MD (Conceptualization: Equal; Data curation: Equal; Formal analysis: Lead; Investigation: Lead; Writing – original draft: Lead; Writing – review & editing: Equal). Milton Wainberg, MD (Conceptualization: Supporting; Investigation: Supporting; Writing – review & editing: Equal). Mitchell S. V. Elkind, MD, MS, MPhil (Conceptualization: Equal; Investigation: Supporting; Supervision: Supporting; Writing – review & editing: Equal). Daniel E. Freedberg, MD, MS (Conceptualization: Equal; Data curation: Supporting; Investigation: Supporting; Supervision: Lead; Writing – original draft: Equal; Writing – review & editing: Equal).
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding None
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org and at https://doi.org/10.1053/j.gastro.2021.10.040.
Supplementary Methods
This was a prospective, nested case-control study among 1783 patients diagnosed with COVID-19 at a single center in New York City. Patients with a positive severe acute respiratory syndrome coronavirus 2 polymerase chain reaction test at Columbia University Irving Medical Center who survived and consented to follow-up were prospectively enrolled in a COVID-19 cohort from April to November 2020.
Six months after their diagnosis, they received an electronic survey regarding ongoing self-perceived COVID-19–related symptoms and pre–COVID-19 mental health symptoms. Specifically, they were asked whether they experienced emotional, mental health, or psychosocial symptoms before they were diagnosed with COVID-19. For all current symptoms, they were asked about the presence, severity (very mild, mild, moderate, severe, or very severe), and frequency (occasionally, sometimes, often, always) of a wide range of symptoms. Current GI symptoms queried in the survey were abdominal pain, nausea/vomiting, heartburn/reflux, diarrhea, or constipation. Current mental health symptoms were sadness and anxiety. Patients who experienced abdominal pain were also asked whether the pain occurred at least weekly, whether it was associated with a change in stool form or stool frequency, whether it started after COVID-19, and whether it had been present at least 6 months.
Demographic factors of age, sex, race, and ethnicity and clinical information related to the initial COVID-19 infection including hospitalization or mechanical ventilation requirement were also collected. The proportion of patients experiencing GI symptoms was compared among patients with and without pre– and post–COVID-19 mental health symptoms using χ2 testing. A multivariable logistic regression model was used to identify independent predictors of GI symptoms 6 months after COVID diagnosis.
Supplemental Table 1.
Multivariable Logistic Regression Model of Predictors Associated With New GI Symptoms After COVID-19
| Predictor | No. of cases with GI symptoms/no. at risk (%) | Adjusted odds ratio | 95% confidence interval |
|---|---|---|---|
| Mental health symptoms | |||
| Neither pre–COVID-19 nor post–COVID-19 | 67/459 (14.6) | 1 (reference) | … |
| Pre–COVID-19 onlya | 0/10 (0) | Unable | NA |
| Post–COVID-19 only | 134/251 (53.4) | 6.16 | 4.21–9.01 |
| Both pre–COVID-19 and post–COVID-19 | 19/29 (65.5) | 16.5 | 6.97–38.9 |
| Sex | |||
| Male | 70/248 (28.2) | 1 (reference) | |
| Female | 150/501 (29.9) | 1.03 | 0.69–1.53 |
| Age | |||
| Under 30 y | 26/110 (23.6) | 1 (reference) | |
| 30–39 y | 48/204 (23.5) | 1.36 | 0.73–2.55 |
| 40–59 y | 101/272 (37.1) | 2.29 | 1.27–4.12 |
| ≥60 | 45/163 (27.6) | 1.79 | 0.92–3.48 |
| Race | |||
| White | 113/454 (24.9) | 1 (reference) | |
| Black | 23/72 (31.9) | 0.97 | 0.51–1.84 |
| Asian/Pacific Islander | 25/73 (34.3) | 2.40 | 1.30–4.44 |
| Native American | 4/8 (50.0) | 5.81 | 1.01–33.59 |
| Other | 29/70 (41.4) | 1.23 | 0.59–2.56 |
| Did not answer | 26/72 (36.1) | 1.45 | 0.68–3.09 |
| Ethnicity | |||
| Non-Hispanic | 138/524 (26.3) | 1 (reference) | |
| Hispanic | 80/208 (38.5) | 1.15 | 0.68–1.94 |
| Did not answer | 2/17 (11.8) | 0.15 | 0.03–0.85 |
| Language | |||
| English | 189/698 (27.1) | 1 (reference) | |
| Spanish | 31/51 (60.8) | 2.55 | 1.14–5.73 |
| Hospitalized | |||
| No | 164/639 (25.7) | 1 (reference) | |
| Yes | 56/110 (50.9) | 2.30 | 1.38–3.84 |
The independent association between pre–COVID-19 mental health symptoms and post–COVID-19 GI symptoms cannot be computed because 19 patients had pre–COVID-19 mental health symptoms and post–COVID-19 GI symptoms and all 19 (100%) also had post–COVID-19 mental health symptoms.
References
- 1.Johns Hopkins COVID-19 Dashboard 2021. https://coronavirus.jhu.edu/map.html.
- 2.Huang C., et al. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nobel Y.R., et al. Gastroenterology. 2020;159:373–375. doi: 10.1053/j.gastro.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halpin S.J., et al. J Med Virol. 2021;93:1013–1022. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- 5.Carvalho-Schneider C., et al. Clin Microbiol Infect. 2021;27:258–263. doi: 10.1016/j.cmi.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong Z.Y., et al. J Clin Gastroenterol. 2021;55:67–76. doi: 10.1097/MCG.0000000000001424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blackett J.W., et al. Neurogastroenterol Motil. 2021 Sep 1:e14251. doi: 10.1111/nmo.14251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zamani M., et al. Aliment Pharmacol Ther. 2019;50:132–143. doi: 10.1111/apt.15325. [DOI] [PubMed] [Google Scholar]
- 9.Vu J., et al. Neurogastroenterol Motil. 2014;26:1323–1332. doi: 10.1111/nmo.12396. [DOI] [PubMed] [Google Scholar]
- 10.Jones M.P., et al. Clin Gastroenterol Hepatol. 2017;15:1014–1020. doi: 10.1016/j.cgh.2016.12.032. [DOI] [PubMed] [Google Scholar]