Abstract
Labial adhesion is characterised by complete or partial fusion of the labia minora. It occurs rarely in postmenopausal women. Although various methods have been proposed, there is no established treatment for postmenopausal patients with labial adhesions due to its low prevalence in this age group. Severe cases require surgical intervention, and the postoperative recurrence rate is relatively high at 14–20%. In this study, a novel therapeutic method was designed to treat labial adhesions: a combination of Z- and Y-V-plasty. An 82-year-old woman was diagnosed with severe long labial adhesion during an episode of urinary tract infection. The labia could not be separated manually; hence, Z-plasty was performed on the ventral side and Y-V-plasty on the anal side under general anaesthesia. No recurrence was noted eight months postoperatively. This method is relatively easy and produced the desired therapeutic effect with decreased risk of recurrence. This is a novel approach for postmenopausal patients with severe labial adhesion.
Keywords: Labial adhesion, Postmenopausal labial adhesion, Labial separation, Z-plasty, Y-V-plasty
Highlights
-
•
Labial adhesions can manifest as urinary tract infections in postmenopausal women.
-
•
Labial adhesion in postmenopausal women is characterised by severe fusion.
-
•
Z- and YV plasty on ventral and anal sides, respectively, is a novel approach.
-
•
Z and YV plasty produced desired therapeutic effect and decreased re-adhesion risk.
1. Introduction
Labial adhesion is characterised by complete or partial fusion of the labia minora. It occurs mainly in prepubertal girls and is relatively rare in postmenopausal women [1]. The condition is related to low oestrogen levels, local chronic inflammation [2,3], and low sexual activity [4]. Patients with labial adhesions rarely complain of the symptoms unless the fusion is almost complete. Severe fusion manifests as various non-specific symptoms, such as urinary incontinence, dysuria, vulvar irritation, and urinary tract infections [5].
Steroid ointments are the standard treatment in prepubertal patients with labial adhesion [6]. However, there is no established treatment for postmenopausal patients with labial adhesions due to its low prevalence in this age group. Complete or severe fusion is often managed with surgical intervention, which shows a certain degree of therapeutic efficacy. However, the recurrence rate is relatively high at 14–20% [7].
This report illustrates a case of labial adhesion in an 82-year-old postmenopausal woman successfully managed using a new surgical technique: the combination of Z-plasty and Y-V-plasty.
2. Case Presentation
An 82-year-old woman was diagnosed with acute pyelonephritis and treated with antibiotics. She was referred for further consultation because a genital examination revealed labial adhesions, which were considered to be a risk factor for her urinary infection.
Physical examination revealed extensive fusion of both labia majora, except for a 2-mm opening near the posterior commissure (Fig. 1-1). Examination using a uterine sonde showed that the closure was superficial. The uterine sonde could be inserted from the opening up to 4 cm to the clitoris side and 1 cm to the anal side, which indicated the closure was superficial. Since manual separation was unsuccessful, surgical intervention was planned.
Fig. 1.
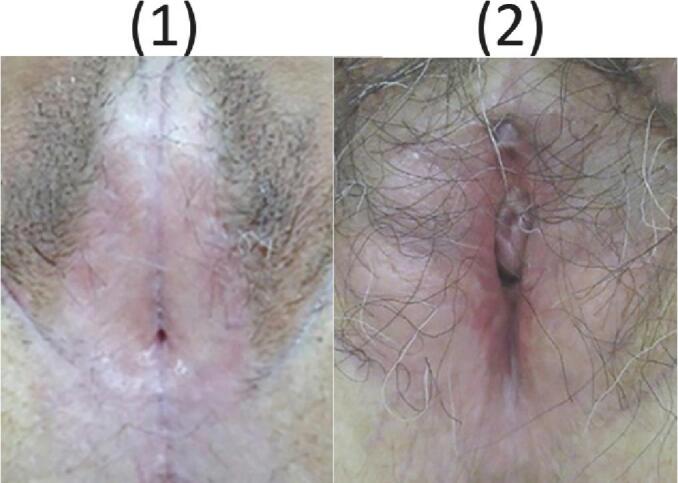
Case overview.
(1) Preoperative photograph: Both labia majora were extensively fused together. There was a pinhole (about 2 mm in diameter) at the fused midline. The clitoris, vestibule, labia minora, and external urethral meatus were unidentifiable. A sonde could be inserted for 4 cm from the pinhole to the clitoris side and for 1 cm from the pinhole to the anal side. (2) Photograph four months after surgery: The thread was removed one month and four months after surgery. The vulva appeared normal; no recurrence was noted.
The patient was placed in a lithotomy position, and the operation was performed under general anaesthesia. Dissection was performed along the adhesion line, enabling examination of the clitoris, external urethral orifice, and vagina. An atheroma was also found on the right side of the clitoris and was removed during separation.
First, a Z-plasty was performed on the ventral side, followed by a Y-V-plasty on the anal side to prevent recurrence. The mucosal tissue fused in a narrow ellipse was excised from the bilateral labia majora, and these areas were used as the central limbs of the “Z.” Next, two limbs of equal length were designed and incisions made to create the lateral limbs of the “Z” (Fig. 2, Fig. 1). The triangular tissue flaps were rotated and crossed over each other (Fig. 2-2). Finally, the incisions were closed using 3–0 absorbent sutures.
Fig. 2.
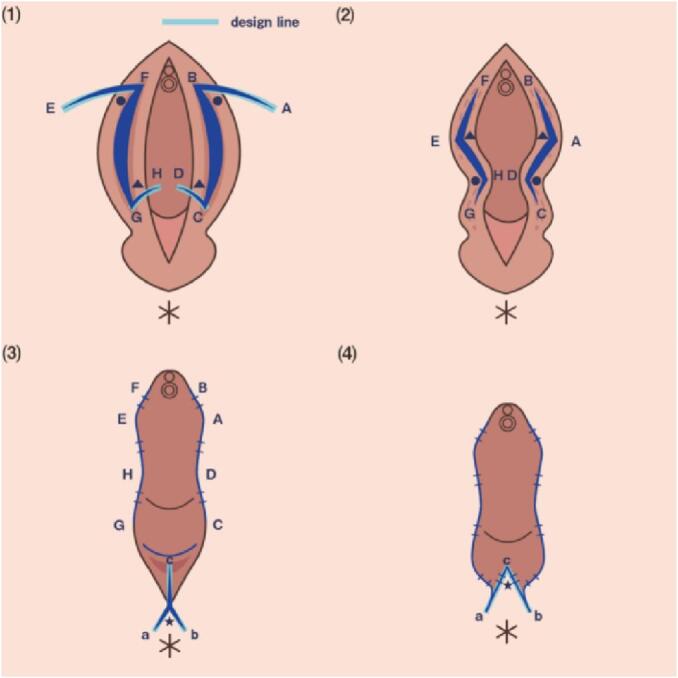
Surgical procedure.
(1) Before Z-plasty: mucosal tissue that was fused in a narrow ellipse from both labia majora was excised to create the central limbs of the “Z” (B-C(F-G). Next, incisions were made to create the lateral limbs of the “Z” (A-B(E-F) and C-D(G-H)). (2) After Z-plasty, the triangular tissue flaps were rotated and crossed over each other (from A-B-C-D(E-F-G-H) to B-A-D-C(F-E-H-G)). (3) Before Y-V plasty, a bow-shaped incision was made in the perineal skin (Fig. 2–3: bow-shaped dark skin-coloured part) to remove the scar tissue and generate an “inverted V-shaped” scar, with the apex near the posterior commissure. An incision was then extended from V's apex toward the ventral to generate an “inverted Y-shaped” wound. (4) After Y-V plasty: the flap was sutured with 3–0 absorbent sutures and reconstructed using an “inverted V-shape.”
The Y-V-plasty was performed by making a bow-shaped incision in the perineal skin (Fig. 2–3: bow-shaped dark skin-coloured part) to remove scar tissue. This created an “inverted V-shaped” scar, the apex of which was near the posterior commissure. The incision was then extended from the V's apex to generate an “inverted Y-shaped” wound. The flap was sutured with 3–0 absorbent sutures and was reconstructed in an “inverted V-shape” (Fig. 2–4).
The total operative time was 2 h 47 min, and the estimated blood loss was approximately 25 mL. The patient started ambulating and eating on postoperative day 1. The indwelling catheter was removed on postoperative day 5, and the patient was discharged on postoperative day 9.
Postoperatively, she was instructed to maintain proper genital hygiene and to use topical steroids and petrolatum jelly once daily for two months to prevent re-adhesion. She had had no recurrence eight months after the procedure (Fig. 1, Fig. 2).
The patient had the mental and physical capacity to provide consent for publication herself and written informed consent was obtained from the patient for publication of this case report.
3. Discussion
This postmenopausal woman with severe labial adhesion was successfully managed using a combination of standard plastic surgery techniques, namely Z-plasty and Y-V-plasty. To the best of our knowledge, this is the first report of the adoption of these two methods for labial adhesion.
Labial adhesion is defined as the complete or partial adherence of the labia minora. It usually occurs in prepubertal girls, with an incidence rate of 1.8% [8]. There are a limited number of case reports on postmenopausal labial fusion, and the prevalence in the elderly population remains unknown. Although topical oestrogen with vulvar hygiene is regarded as a first-line treatment for prepubertal girls and has been known to yield favourable outcomes [7], this treatment often has no therapeutic effects in postmenopausal women [9]. Moreover, labial agglutination interferes with gynaecological examinations, such as Pap smear tests or ultrasound, leading to the inability to diagnose vaginal pathological conditions [5]. Thus, surgical intervention is more likely in older patients with severe disease. Previous studies revealed that manual and surgical separations led to a high recurrence rate, of 14–20% [7]. Due to the high recurrence rate, some patients require multiple interventions, which adversely affects their quality of life.
Some case reports indicated that sharp dissection and suturing alone might lead to morbidity and scarring and also recurrence. It is crucial not only to maintain sufficient spacing between labia majora but also to release tension between them to avoid recurrence. Therefore, several surgical methods have been developed to prevent re-adhesion (Table 1). Kaplan et al. described a separation method using serial Hegar dilators, which minimises the area of sharp dissection [10]. Another report mentioned a two-step method in which uterine cervical dilators were used to separate the lower part of the adhesion area, followed by separation using fine curved forceps from inside the adhesion [11].
Table 1.
Literature review for labial adhesion treatments including the current method.
| Method | Advantage | Disadvantage | Follow-up period (month) |
|---|---|---|---|
| Conservative treatment 1, 4, 6, 8, 10, 12 | Minimally invasive. | Longer treatment period. Less effective. |
NA |
| Separation manually or using a device1, 3, 4, 8, 9, 10 | Minimally invasive. | Risk of re-adhesion. | 1–12 |
| Heineke–Mikulicz suturing technique11 | Minimally invasive. Preventable recurrence. |
Suture failure. Unadaptable to long adhesion. |
6 |
| Vulvo perineal flap12 | Preventable recurrence. Cosmetically natural. |
Highly invasive & high perioperative complication rate. | 18 |
| Z-plasty alone13 | Preventable recurrence. | Cosmetically unnatural. Unadaptable to long adhesion. |
11 |
| Y-V plasty alone15 | Cosmetically natural. | Risk of re-adhesion. | NA |
| The combination of Z and Y-V plasty | Minimally invasive. Preventable recurrence. Adaptable to long adhesion. |
Cosmetically unnatural. Many suture points. Possibility of suture failure. |
8 |
Several methods of reconstruction have been reported recently and have also shown favourable outcomes. Takemura et al. demonstrated the use of the Heineke-Mikulicz suturing technique, a well-known method to enlarge the diameter of narrowed bowel segments, to treat adhesion. It is a minimally invasive technique that can effectively treat labial adhesion. They performed a longitudinal incision along the adhesion line and closed it transversely, giving a normal spacing between the labia majora [12]. However, as one of the drawbacks of this method, it cannot be used for long adhesion in patients with severe adhesion. The Heineke-Mikulicz suturing technique leads to increased wound tension and increased risk of wound dehiscence. Reconstruction using a vulvoperineal flap was also reported as another treatment for postmenopausal women with severe labial adhesion [13]. This method can prevent recurrence and also yields a cosmetically natural-looking vulvar area. A key drawback of this surgery is the risk of perioperative complications such as flap ischaemia, protracted wound healing, and infection. Moreover, since this procedure is relatively invasive and technically complicated, its use as a general and routine treatment is questionable.
Methods using Z-plasty [14] have also been reported amply in the literature. Bun et al. reported the use of Z-plasty, a standard procedure in plastic surgery, to repair and prolong linear scars, to prevent re-adhesions. This procedure is relatively simple; therefore, Z-plasty was first considered over other procedures. However, it turned out to be impossible because the patient's adhesion was fairly long, making it difficult to make a Z line. Therefore, Y-V-plasty was performed in addition to Z-plasty. Y-V-plasty has been used in cases of congenital adrenal hyperplasia [15], to correct long adhesions.
One of the advantages of this method is that it can be used even if the adhesion is long, as it allows for reconstruction along two separate areas: the clitoris and anal sides. Combining the two different plasty methods enabled us to manage the long and severe tension-free adhesion with a normal distance between the labia majora. Furthermore, since these techniques are relatively simple and easy to perform, they can be used by general gynaecologists in their day-to-day practice. However, this is the first report on the use of this technique to treat labial adhesion, and further studies with more patients are recommended to confirm the efficacy of this technique.
There are also two key concerns associated with this method. The first is the cosmetic aspect. Multiple plasty attempts can make the labia look aesthetically unacceptable until the wound is healed. Second, the number of suture points can vary. The difficulty in performing the procedure varies on a case-by-case basis. However, many suture points require more design, longer surgery time, and may lead to suture failure. With regular use, an easy technique that addresses these concerns can be developed.
In conclusion, this report illustrates a novel surgical method that can be used to treat labial adhesions: the combination of Z- and Y-V-plasty. This method is relatively easy to perform and yielded a desirable therapeutic effect, with decreased risk of recurrence. This may be a novel approach for treating postmenopausal patients with severe labial adhesions.
Acknowledgments
Contributors
Tomoko Maeda was involved in patient care and in the study design, wrote the original draft, and critically revised and edited the manuscript.
Mari Deguchi was involved in patient care and in the study design, wrote the original draft, and critically revised and edited the manuscript.
Tsukuru Amano was involved in the study design, and critically revised and edited the manuscript.
Shunichiro Tsuji critically revised and edited the manuscript.
Kyoko Kasahara critically revised and edited the manuscript.
Takashi Murakami was involved in the study design, and critically revised and edited the manuscript.
All authors read and agreed to the published version of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
The authors received no funding from an external source for the publication of this case report.
Patient consent
Obtained.
Provenance and peer review
This article was peer reviewed.
Acknowledgements
The authors would like to thank the plastic surgery team of the Shiga University of Medical Science Hospital for their helpful advice regarding the surgical procedure, and the Golden Ratio Group (https://golden-ratio.co.jp/) for helping to prepare Figure 2 in this report.
References
- 1.Singh P., Han H.C. Labial adhesions in postmenopausal women: presentation and management. Int. Urogynecol. J. 2019;30:1429–1432. doi: 10.1007/s00192-018-3821-1. [DOI] [PubMed] [Google Scholar]
- 2.Mikos T., Lioupis M., Grimbizis G.F. Postmenopausal complete labial fusion and pseudo-incontinence: A case series. Case Rep. Women's Heal. 2019;21 doi: 10.1016/j.crwh.2019.e00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choung C.J., Hodgkinson C.P. Labial adhesions presenting au urinary incontinence in postmenopausal woman. Obstet. Gynecol. 1984;64:81–84. doi: 10.1097/00006250-198409001-00020. [DOI] [PubMed] [Google Scholar]
- 4.Ong N.C.S., Dwyer P.L. Labial fusion causing voiding difficulty and urinary incontinence. Aust. New Zeal. J. Obstet. Gynaecol. 1999;39:391–393. doi: 10.1111/j.1479-828X.1999.tb03429.x. [DOI] [PubMed] [Google Scholar]
- 5.Lu B.J., Chin H.Y., Chu C.Y., Wang J.T.J. Postmenopausal labial agglutination mimics urinary incontinence and hidden vaginal lesion. J. Obstet. Gynaecol. Res. 2018;44:801–805. doi: 10.1111/jog.13556. [DOI] [PubMed] [Google Scholar]
- 6.Norbeck J.C., Ritchey M.R., Bloom D.A. Labial fusion causing upper urinary tract obstruction. Urology. 1993;42:209–211. doi: 10.1016/0090-4295(93)90650-Y. [DOI] [PubMed] [Google Scholar]
- 7.Schober J., Dulabon L., Martin-Alguacil N., Kow L.M., Pfaff D. Significance of topical topical estrogens estrogens to labial labial fusion fusion and vaginal vaginal Introital introital integrityintegrity. J. Pediatr. Adolesc. Gynecol. 2006;19:337–339. doi: 10.1016/j.jpag.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 8.LeungEUNG A.K.C., RobsonOBSON W.L.M., Tay-UybocoAY-UYBOCO J. The incidence of labial fusion in children. J. Paediatr. Child Health. 1993;29:235–236. doi: 10.1111/j.1440-1754.1993.tb00495.x. [DOI] [PubMed] [Google Scholar]
- 9.Pulvino J.Q., Flynn M.K., Buchsbaum G.M. Urinary incontinence secondary to severe labial agglutination. Int. Urogynecol. J. 2008;19:253–256. doi: 10.1007/s00192-007-0415-8. Published online. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan F., Alvarez J., Dwyer P. Nonsurgical separation of complete labial fusion using a Hegar dilator in postmenopausal women. Int. Urogynecol. J. 2015;26:297–298. doi: 10.1007/s00192-014-2535-2. [DOI] [PubMed] [Google Scholar]
- 11.Hatada Y. Two-step surgical approach to labial adhesions in a postmenopausal woman. Acta Obstet. Gynecol. Scand. 2003;82:1054–1055. doi: 10.1034/j.1600-0412.2003.00028.x. [DOI] [PubMed] [Google Scholar]
- 12.Takemaru M., Aramaki-Hattori N., Tsue C., Kishi K. Labial adhesions adhesions causing causing recurrent recurrent urinaryurinary-tract tract infections infections in an elderly elderly woman. Case Rep. Med. 2019;2019 doi: 10.1155/2019/7584983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takimoto M., Sato T., Ichioka S. Reconstruction for labial adhesion in postmenopausal woman using vulvoperineal flap. Case Rep. Plast. Surg. Hand Surg. 2019;6:136–139. doi: 10.1080/23320885.2019.1602474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bun M., Miyake A., Osaki Y., Okada M. A case of recurrent labial adhesion treated with Z-plasty in a postmenopausal woman. Adv. Obstet. Gynecol. 2019;71:247–252. doi: 10.11437/SANPUNOSINPO.71.247. [DOI] [Google Scholar]
- 15.Kitahara S., Higashi Y., Tsujii T. Results of genitoplasty for virilized genitalia of 41 females with congenital adrenal hyperplasia. Japanese J. Urol. 1996;87:1289–1296. doi: 10.5980/jpnjurol1989.87.1289. [DOI] [PubMed] [Google Scholar]


