Abstract
Background
The number of paediatric emergency department (ED) visits and hospital admissions was recorded in a tertiary referral centre during the first year of the COVID-19, March 2020–February 2021, and compared with those of the preceding year.
Methods
The number of visits and admissions and the reason of visit and admission were prospectively recorded from 15,087 patients’ files.
Results
A substantial decline in the total number of visits and increase in the admission rate were documented during the COVID-19 year compared to the preceding year (10691 vs 4396 patients, 22.59% vs 18.15% (OR: 1.316, CI 95%: 1.208–2.242, p < 0.0001), respectively). Fever and/or respiratory symptoms were the commonest reported symptoms in both periods. Possible explanations include: (i) restricted overall infection transmission due to confinement and self-protective measures, (ii) avoidance of unnecessary hospital visits in the absence of severe symptoms and (iii) reduced or delayed access to medical care due to parental fear of children’s exposure to COVID-19.
Conclusion
This study is the first worldwide to investigate the impact of COVID-19 on ED visits and admissions throughout the whole year of the pandemic, and to highlight the need for re-evaluation of future protective strategies to infections, adjustment of health-care systems and parental education so that medical care in a health-care setting is sought in a more appropriate manner.
Impact
A significant decline in paediatric ED visits and increase in the admission rate was observed during the first year of COVID-19 in a tertiary referral centre, possibly due to reduced overall infection transmission, limited ED overuse, but also ED underuse due to parental fear of children’s exposure to SARS-CoV-2.
COVID-19 may serve as an opportunity for societies to re-evaluate future strategies to infections, adjust health-care systems accordingly, and reinforce parents to seek medical care more appropriately.
Although the incidence of critical illness in children due to COVID-19 and in general is low, special attention should be devoted to identifying children at risk early.
Introduction
The novel Coronavirus Disease 2019 (COVID-19) outbreak represents a global pandemic, as declared by World Health Organization (WHO) in January 2020 (ref. 1), and has become the greatest challenge humanity has faced in the past decades. The first health, social and economic consequences are already evident, but, since we are in uncharted territory, it is estimated that many of the implicated crises remain unrecognized and are yet to become manifest.
According to the available epidemiological data, children seem to become infected less frequently than adults and if infected, they are less likely to become symptomatic or experience severe forms of the disease. Specifically, the prevalence of the disease in children <18 years old has been reported as 2.4% of all reported cases and the majority experience mild symptoms of shorter duration, and exhibit shorter detoxification time and a better prognosis than adults.2 The most common clinical manifestations reported in the paediatric population include fever and cough, accompanied in some cases by fatigue, myalgia, nasal congestion, sore throat, headache, vomiting, diarrhoea and abdominal pain.3 Vulnerability is inversely related to age.4
The first case of COVID-19 in Greece was confirmed in 26 February 2020 and it was then that the first preventive measures were applied and involved the closure of schools and the suspension of cultural events in the initially affected areas. On 10 March, due to the spread of the outbreak in different parts of the country, all the educational institutions were closed and containment measures were escalated, including closure of shops, suspension of religious practices, restriction of public and nonessential transport, whereas self-protection instructions were widely communicated. The first nationwide lockdown had a 2-month duration (until the end of April 2020). A 6-month period of relaxation of protective and social distancing measures followed (April to October 2020), but due to a significant increase in the number of people tested positive and in the number of deaths, a second lockdown was imposed from November 2020 to February 2021 in most parts of the country, including Western Greece.
During the COVID-19 pandemic, reduced rates of visits to the emergency departments (ED) of hospitals have been reported worldwide.5,6 The aim of this retrospective study was to investigate the effect of the COVID-19 pandemic on the paediatric ED visits and hospital admissions at a tertiary university hospital in Greece, by comparing 1-year data from the COVID-19 pandemic (March 2020 to February 2021), and data from the preceding year (March 2019–February 2020). The COVID-19 year includes two periods of strict lockdown (March–April 2020 and November 2020–February 2021), and a 6-month period of less stringent measures (May 2020–October 2020).
Patients and methods
In total, 15,087 visits at the paediatric ED of the University General Hospital of Patras in Greece and 2993 paediatric ward admissions in total were retrospectively analysed. The study period was 2 years and was divided into two 1-year periods: (i) the pre-COVID-19 year (March 2019–February 2020) and (ii) the COVID-19 year (March 2020–February 2021). The number of visits during the two periods, the reason of visit, the number of admissions to the paediatric ward, the admission rate and the reason for admission, were recorded. The study was approved by the Research Ethics Committee of the University General Hospital of Patras and is in accordance with the ethical standards of the Helsinki declaration of 1975, as revised in 1983.
The University General Hospital of Patras is a teaching hospital that provides tertiary services for the geographical area of the Region of Western Greece (population coverage ≈ 1,000,000), admits patients 4 days a week and has become a referral centre for COVID-19. Surgical cases, such as trauma and bone fractures, are not managed in this hospital.
Statistical analysis
In this prospective study we examined the number of ED admissions and the subsequent admission rate for hospitalization during COVID-19 pandemic (March 2020 to February 2021) and the year before (March 2019 to February 2020). In order to examine the presence of a difference between the admission rates for hospitalization before and during the COVID-19 pandemic we used the Fisher’s exact test expressed as odds ratio (OR) with a 95% confidence interval (CI). All tests were two-tailed and statistical significance was considered for p values <0.05. All statistical analyses were performed using GraphPad Prism (version 5.00 for Windows, GraphPad Software, San Diego, CA).
Results
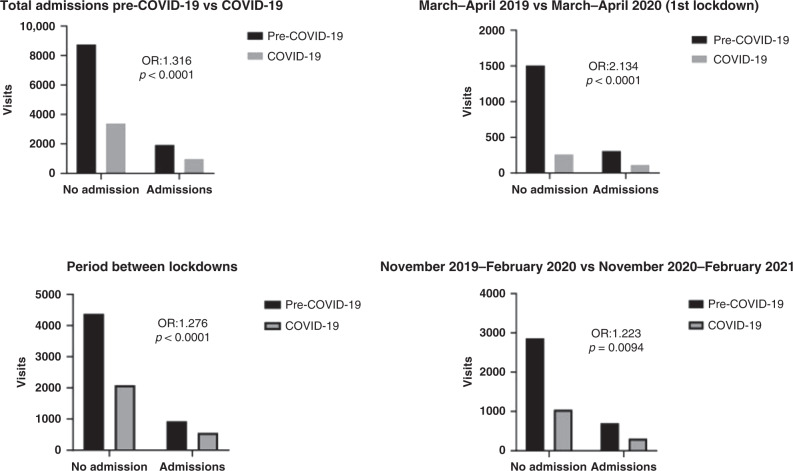
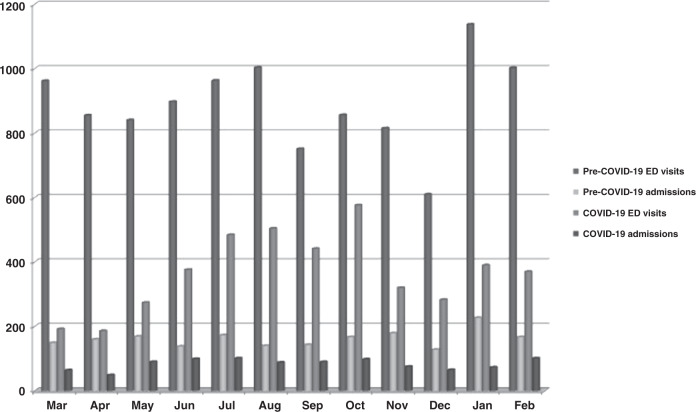
In total, 10,691 children visited the paediatric ED of the hospital during the pre-COVID-19 year (March 2019–February 2020) and among those, 1940 children needed hospitalization (Table 1). During the year March 2020–February 2021, 4396 children were examined in the paediatric ED and 993 of them were admitted to the paediatric ward (Table 1). The admission rate of the COVID-19 year was significantly higher compared to that of the pre-COVID-19 year (22.59% vs 18.15%, OR: 1.316, CI 95%: 1.208–2.242, p < 0.0001) (Fig. 2). The monthly distribution of ED visits and admissions is depicted in Fig. 1. The most common reason for visiting the ED during the COVID-19 and pre-COVID-19 year was fever and/or respiratory symptoms accounting for 65.10% and 62.80% of the total ED visits, respectively, followed by gastrointestinal symptoms (10.30% and 10.60%, respectively). The main reasons for admission were again fever and/or respiratory symptoms (70.40% for the COVID-19 year and 55% for the pre-COVID-19 year), followed by gastrointestinal symptoms (8.70% and 13.20%, respectively). The predominant clinical manifestations of the children that were seen in the paediatric ED and were admitted to the paediatric ward during the COVID-19 year and the pre-COVID-19 year are shown in Table 2.
Table 1.
ED visits, admissions and admission rate during the studied periods.
| Time periods | ED visits (n) | Admissions (n) | Admission rate (%) |
|---|---|---|---|
| Pre-COVID-19 (March 2019–February 2020) | 10,691 | 1940 | 18.1 |
| COVID-19 (March 2020–February 2021) | 4053 | 919 | 22.7 |
| March–April 2019 | 1817 | 309 | 17 |
| March–April 2020 (1st lockdown) | 378 | 115 | 30.4 |
| May–October 2019 | 5310 | 930 | 17.5 |
| May–October 2020 (between lockdowns) | 2655 | 566 | 21.3 |
| November 2019–February 2020 | 3564 | 701 | 19.7 |
| November 2020–February 2021 (2nd lockdown) | 1020 | 240 | 23.5 |
Fig. 2. Number of children who visited the paediatric Emergency Department and required (admissions) or did not require (no admission) admission to the paediatric ward.
Number of children who visited the paediatric Emergency Department and required (admissions) or did not require (no admission) admission to the paediatric ward during the whole COVID-19 year, the 1st lockdown, the 2nd lockdown, the period between the two lockdowns and the relative periods one year before.
Fig. 1. Monthly distribution of paediatric emergency department visits and admissions.
Monthly distribution of paediatric emergency department visits and admissions during the COVID-19 and pre-COVID-19 years. Mar March, Apr April, Jun June, Jul July, Aug August, Sep September, Oct October, Nov November, Dec December, Jan January, Feb February.
Table 2.
Presented clinical symptoms in children visiting the ED and on admission.
| Clinical symptoms | ED visits | Admissions | ||
|---|---|---|---|---|
| Pre-COVID-19 year (%) | COVID-19 year (%) | Pre-COVID-19 year (%) | COVID-19 year (%) | |
| Fever and/or respiratory | 62.8 | 65.1 | 55 | 70.4 |
| Gastrointestinal | 10.6 | 10.3 | 70.4 | 8.7 |
| Dermatological | 5.2 | 3.8 | 2.2 | 0.9 |
| Neurological | 2.9 | 3.8 | 9.2 | 4.3 |
| Musculoskeletal | 1.5 | 0.8 | 1 | 0.9 |
| Type 1 diabetes mellitus | 0.3 | 0.5 | 1.4 | 1.7 |
| Psychiatric | 0.2 | 0.3 | 0 | 0.9 |
| Other | 8.6 | 15.4 | 17.9 | 12.2 |
During the initial lockdown period of the first pandemic outbreak (March–April 2020), 378 children visited the paediatric ED. In all, 30.42% of the children examined (115 children) were admitted to the paediatric ward. During the same 2-month period in 2019 (March–April), 1817 children were examined in the paediatric ED of the hospital and 309 of the examined children required admission (Table 1). The admission rate of the first lockdown was significantly higher than the corresponding rate during March–April 2020 (30.42% vs 17.01%, OR: 2.134, CI 95%: 1.66–2.735, p value < 0.0001) (Fig. 2).
During the second pandemic wave in Greece (November 2020–February 2021), which resulted in a second strict lockdown in the area, 1363 children visited the ED and 314 (23.04%) were hospitalized. During the period November 2019–February 2020, which reflects the months before the severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) was detected in the country, 3564 children visited the Paediatric ED and 701 required admission (Table 1). A significant increase was observed in the admission rate of the second lockdown compared to that of the same period 1 year before (23.04% vs 19.67%, OR:1.223, CI 95%: 1.052–2.132, p = 0.0094) (Fig. 2).
During the 6-month period between the two strict lockdowns in Greece (May 2020–October 2020), when the protective measures were de-escalated but still existent, 2655 children were examined in the paediatric ED and 566 of them were admitted to the paediatric ward. During the same 6-month period 1 year earlier, 5310 children were examined in the ED and 930 of them were admitted to the paediatric ward (Table 1). The admission rate of the period between the two lockdowns was significantly higher than that of the same months 1 year before (21.32% vs 17.51%, OR:1276, CI 95%: 1136–1433, p < 0.0001) (Fig. 2).
The admission rate of the first lockdown was significantly higher than that of the second lockdown (30.42% vs 23.04%, OR: 1.461, CI 95%: 1.130–1.879, p = 0.0037). Interestingly, the diagnoses on admission showed no difference between the first and the second lockdown. The most common diagnoses involved the respiratory system (70.40% of the admissions during the first wave and 72.80% during the second wave), followed by the gastrointestinal system (8.7% vs 7% for the first and second wave, respectively).
Of importance, the overall number of children tested positive at the hospital from March 2020 to the end of February were 80 out of the 597 that were tested in total (13.4%). Of those tested positive, only 25 (31.2%) were admitted to the paediatric ward. During March 2020–April 2020, 60 tests were performed and none was found positive. During May 2020–October 2020, 238 tests were performed in children and 11 were found positive (4.6%), whereas during the second lockdown period (November 2020–February 2021), 69 children were found positive out of 299 tests performed in children (23%). The number of tests performed was increased based on the testing criteria for SARS-CoV-2 which became less strict by May 2020 and included a wider range of symptoms in the paediatric population.
Discussion
The main findings of the present study include a substantial decline (by approximately 59%) in the paediatric ED visits during the 1-year period after SARS-CoV-2 manifested in Greece, compared to the preceding year. This decrease involves the whole range of medical conditions seen in the hospital. Interestingly, the admission rate into the paediatric ward during the COVID-19 year was significantly higher compared to that of the pre-COVID-19 year despite the reduced number of the paediatric emergency department visits (24.9% increase). In both studied periods, fever and/or respiratory symptoms were the predominant reason for visiting the ED (Pre-COVID-19: 62.80%, COVID-19: 65.10%) and for hospitalization (Pre-COVID-19: 55%, COVID-19: 70.40%), which is in agreement with data from other studies.7
During the initial peak period of the COVID-19 pandemic in Greece (March–April 2020), the number of paediatric ED visits was again significantly reduced compared to the same 2-month period in 2019 (by approximately 62%), whereas the likelihood for admission, as expressed by the admission rate, was significantly increased. Of interest, since only 60 of the children that visited the paediatric ED met the initial criteria for SARS-CoV-2 testing and all were negative, the admissions to the paediatric ward during this period were not related to COVID-19 (non-COVID-19 admissions). Similar results were observed during the second pandemic wave and lockdown period (November 2020–February 2021) as compared to the same months 1 year earlier (November 2019–February 2020); the visits to the paediatric ED were reduced by 61.80%, but the admission rate was increased by 16.80%.
Notably, in the second lockdown, during which the number of positive tests and of deaths in the Greek population was significantly higher than during the first lockdown period (Supplemental Digital Content 1),8 the number of children that visited the paediatric ED was higher compared to the first lockdown (monthly ED visits: 255 during the second lockdown vs 189 during the first lockdown). This may be explained by the increased number of positive tests and deaths in the general and paediatric population throughout the country during the second wave compared to the first, which may have increased parental anxiety regarding their child being positive and at risk for severe illness. A significant percentage of parents indeed reported that the main reason for visiting the paediatric ED was to have their child tested for SARS-CoV-2, even in the absence of severe symptoms. Unfortunately, the precise percentage was not recorded. In addition to the increased infection rate, as previously mentioned, the testing criteria for SARS-CoV-2 included a wider range of symptoms during the second lockdown; hence, more children were eligible to be tested. Another possible explanation, from a different perspective, could be that a proportion of the parents could have a more relaxed attitude towards the disease during the second pandemic wave and were not as worried about their child being exposed to the virus in the hospital as during the first wave. Similarly to the first lockdown, during the second lockdown the likelihood for admission was again increased when compared to the relative months 1 year before, albeit to a smaller degree. Interestingly, the likelihood for admission during the first lockdown was significantly higher than that of the second lockdown.
When the period between the two lockdowns, during which less restrictive measures were in effect, was studied and compared with the same months of the previous year, the findings were similar; however, the differences in the ED visit and admission rates were smaller; the number of the ED visits was reduced by 50% and the admission rate was increased by 21.70%. Therefore, even when less tight preventative measures were in effect, the visit rate was lower and the admission rate higher to that of the pre-COVID-19 period.
Similar results exhibiting a sharp reduction in the rate of ED visits and hospital admissions have been reported by several studies conducted in adults9,10 and in children. When data from March 2020–April 2020 were studied in a paediatric population in the US, a reduction in the ED visits by 42% was observed.11 According to another study from the US, the ED visit rate in children <14 years old was reduced by 45.7% during the period March 2020–August 2020 compared to a 3-year comparator period.12 Another US study that compared data from January 2020 to June 2020 with those from January 2019 to June 2019 showed a marked decline in the paediatric ED visits, particularly those that occurred due to respiratory or gastrointestinal symptoms, which was more profound compared to the adults.13 Numerous more recent studies from Europe and other parts of the world have also reported a marked reduction in paediatric ED visits, suggesting the presence of a uniform pattern worldwide.14–20
The findings of the present study may be approached in various ways. Firstly, the application of confinement and self-protective measures, including quarantine, social distancing, and self-hygiene measures, in an effort to reduce the magnitude of the epidemic peaks of the COVID-19, has resulted, as expected, in restricted transmission of infections in general. This may explain to a significant degree the observed reduction in the rate of ED visits, particularly during the first pandemic wave when the measures were strictly followed. Based on this observation, independent of whether COVID-19 remains a health hazard in the following years, societies should consider adhering to stricter protective measures and social distancing strategies than previously, albeit not to the degree this was needed during the COVID-19 pandemic. It should not be ignored that transmission of other infections also increases morbidity and mortality, posing people at avoidable health risks and unnecessarily increasing the burden on health-care systems. Avoiding unnecessary exposure to crowded environments, particularly when symptoms of an infection are present, and following self-protective measures, could be widely communicated and become a routine practice.
Secondly, in addition to reduced infection rates due to the measures imposed during the COVID-19 pandemic, the reduced visits in the paediatric ED could partly be explained by the reticence of parents to risk their children’s exposure to COVID-19 in a health-care setting. As a result, in the presence of symptoms of mild or moderate severity, hospital visits may have been avoided. This is also suggested by the significantly higher admission rate in the post COVID-19 year compared to the pre-COVID-19 year, which implies that children that visited the ED after March 2020 were more likely to have severe symptoms, hence to be hospitalized, whereas in the preceding year a higher percentage of children with milder symptoms that did not require hospital admission visited the ED. It is well known that there is an overuse of the Health Systems in many countries, which creates a drain of resources.15 Inappropriate resource utilization compromises the systems’ ability to deliver quality primary care services to all patients and this may worsen the health outcomes of children suffering from acute conditions (e.g. due to increased waiting times, exhaustion of clinicians), not to mention the increase in the health-care cost. Therefore, expansion of triage in all hospitals is of major importance, investing in primary health care, as well as establishing preventive care visits and improving access of non-urgent cases to alternative out-of-hospital sites. In the case of children with chronic diseases, adequate outpatient follow-up is critical. Furthermore, guidance of the parents is needed in order to increase their confidence and empower them to manage their children’s conditions where appropriate, avoiding unnecessary visits to the hospital. However, it must be stressed that defining appropriate care is challenging and requires a more systematic approach.
At the other end of the continuum, one aspect that should not be neglected is the underuse of health services, since reduced or delayed access to health care can be life-risking and detrimental to paediatric health, particularly for children with co-morbidities or with a severe acute medical condition. Delayed access to medical care due to parental fear of exposure to COVID-19 has been reported by Lazzerini et al.21 Hence, in addition to educating parents against overuse of the health-care system, awareness should also be raised about early access to health care in the instance of severe symptoms in previously healthy children or even minor symptoms in high-risk paediatric populations, as delayed access may pose children at a higher risk for unwanted health outcomes than COVID-19. Using triage help lines and virtual visits could also help towards ameliorating the aforementioned risks.
In addition to the altered use of the health-care system due to parental apprehension about children’s exposure to the SARS-CoV-2, provision of limited health care should also be taken into consideration, as part of reorganization of the paediatric services. Specifically, the outpatient services of the hospital were closed during both the first and second pandemic wave in an effort to reduce intra-person contamination. Furthermore, primary care paediatricians limited clinical care of children with infections in order to avoid exposure to the virus and due to practical limitations, such as insufficient personal protective equipment or inability to isolate suspected patients. As a result, phone and virtual consultations increased in private practice, changing the pattern of health-care utilization.
Limitations
The present study has some limitations, including that the age, the sex, other sociodemographic characteristics as well as co-morbidities of the children that visited the ED and of those that were hospitalized were not studied. In addition, this is a single centre study and the University General Hospital of Patras does not provide paediatric surgical care; therefore, surgical cases, such as orthopaedic or trauma cases, were not included in the study. Finally, although the main reason for admission to the Paediatric ward is mentioned, i.e. fever and/or respiratory symptoms, more specific diagnoses were not recorded and this is another limitation of the study.
Conclusion
To the best of our knowledge, thus far this study is one among very few worldwide to report on the impact of the COVID-19 pandemic on the ED visits and admission rate in a paediatric population analysing data of the whole period (1-year period) after COVID-19 became manifest in Europe. The presented data suggest that besides re-evaluating future protective strategies to infections, societies could see this pandemic as an opportunity to adjust health-care systems accordingly, and to reinforce parents to seek medical care through the ED in a more appropriate manner, so that the right care is provided at the right place, at the right time. Early identification of critically ill children due to COVID-19 and in general is also of the utmost importance, particularly in the presence of underlying co-morbidities.
Supplementary information
Author contributions
E.K. contributed substantially to conception and design, data acquisition, analysis and interpretation and drafting of the article. D.G. contributed to data analysis and interpretation, and drafting of the article. M.P. participated in data analysis and interpretation, statistical analysis and drafting of the article. S.F. contributed to data analysis and interpretation and critically revised the article. A.V. contributed to the study design, data interpretation and article revision. G.D. contributed to conception and design, data interpretation and critical revision of the article. All authors approved the final version of the article to be published.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41390-021-01815-w.
References
- 1.WHO Director-General’s statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (2020).
- 2.National Health Commission of the People’s Republic of China. China‐WHO new coronavirus pneumonia COVID‐19 joint inspection report [EB/OL] (accessed February 29, 2020, 2020); http://www.nhc.gov.cn/jkj/s3578/202002/87fd92510d094e4b9bad597608f5cc2c.shtml.
- 3.Fu L, et al. Clinical characteristics of coronavirus disease 2019 in China. J. Infect. 2020;80:656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong, Y. et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 10.1542/peds.2020-0702 (2020).
- 5.Yan H, et al. Changes in pediatric healthcare utilization in Hunan Province, China, during the COVID-19 pandemic: a multi-center cross-sectional study. Transl. Pediatr. 2021;10:870–881. doi: 10.21037/tp-20-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dopfer C, et al. COVID-19 related reduction in pediatric emergency healthcare utilization—a concerning trend. BMC Pediatr. 2020;20:427. doi: 10.1186/s12887-020-02303-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality. Overview of pediatric emergency department visits. HCUP Statistic Brief #242 (accessed: September 28, 2020, 2015); https://www.hcup-us.ahrq.gov/reports/statbriefs/sb242-Pediatric-ED-Visits-2015.jsp.
- 8.Roser, M., Ritchie, H., Ortiz-Ospina, E. & Hasell, J. Coronavirus Pandemic (COVID-19). OurWorldInData.org. https://ourworldindata.org/coronavirus (2020).
- 9.Kuitunen I, et al. The effect of national lockdown due to COVID-19 on emergency department visits. Scand. J. Trauma Resusc. Emerg. Med. 2020;28:114. doi: 10.1186/s13049-020-00810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020;38:1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartnett KP, Kite-Powell A, DeVies J. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. Mmwr. Morb. Mortal. Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DeLaroche, A. M. et al. Pediatric Emergency Department visits at US Children’s Hospitals during the COVID-19 pandemic. Pediatrics10.1542/peds.2020-039628 (2020). [DOI] [PubMed]
- 13.Pines JM, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am. J. Emerg. Med. 2021;41:201–204. doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kruizinga MD, et al. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur. J. Pediatr. 2021;180:2271–2279. doi: 10.1007/s00431-021-04015-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaehn P, et al. Differential trends of admissions in accident and emergency departments during the COVID-19 pandemic in Germany. BMC Emerg. Med. 2021;21:42. doi: 10.1186/s12873-021-00436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liguoro I, et al. The impact of COVID-19 in a tertiary care pediatric emergency department. Eur. J. Pediatr. 2021;180:1497–1504. doi: 10.1007/s00431-020-03909-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhedin SA, et al. Reduction in paediatric emergency visits during the COVID-19 pandemic in a region with open preschools and schools. Acta Paediatr. 2021;110:2802–2804. doi: 10.1111/apa.15978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raffaldi I, et al. Pediatric admissions to emergency departments of North-Western Italy during COVID-19 pandemic: a retrospective observational study. Lancet Reg. Health Eur. 2021;5:100081. doi: 10.1016/j.lanepe.2021.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finkelstein Y, et al. Effect of the COVID-19 Pandemic on patient volumes, acuity, and outcomes in Pediatric Emergency Deparments: a nationwide study. Pediatr. Emerg. Care. 2021;37:427–434. doi: 10.1097/PEC.0000000000002484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erlichman M, Zalut T, Schwartz S, Weiser G. The ongoing indirect effect of the COVID-19 pandemic on a pediatric emergency department. PLoS. ONE. 2021;6:e0251003. doi: 10.1371/journal.pone.0251003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lazzerini M, et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child. Adolesc. Health. 2020;4:10–11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.