Abstract
The spread of the novel coronavirus has led to unprecedented changes in daily living. College students (N = 205) completed a battery of questionnaires in April of 2020, after having completed similar measures 8, 5, and 2 months prior as part of a larger study. A repeated measures ANOVA suggested significantly greater depression and anxiety symptom severity during the pandemic than any other time during the 2019–2020 academic year. Two-thirds reported a level of distress above clinical cutoffs on the PHQ-9 and GAD-7. Pre-existing depression and anxiety symptom severity was associated with greater psychological distress during the pandemic. One quarter of students reported using substances to cope with the pandemic. Static and modifiable factors associated with psychological distress and controlling for pre-existing psychological distress were examined. Cognitive and behavioral avoidance, online social engagement, and problematic Internet use were associated with greater risk. Women and Latinx participants were more likely to experience elevated distress during the pandemic, even when controlling for distress prior to the pandemic.
Keywords: COVID-19, College students, Depression, Anxiety, distress
1. Introduction
The novel coronavirus (SARS-CoV-2) has taken an enormous toll since its spread began in December of 2019 (Zhou et al., 2020). The virus and resulting acute respiratory syndrome (COVID-19) resulted in nearly 1.1 million confirmed cases and over 50,000 deaths in the United States just over a month following the declaration of a state of national emergency in March 2020, according to data from the COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (Dong et al., 2020).
In addition to the effect of the virus on human health, social distancing measures and shelter-in-place orders haves led to unprecedented changes in daily life that have serious implications for mental health (Gruber et al., 2020; Kumar and Rajasekharan Nayar, 2021). Consistent with studies on the impact of previous pandemics, (e.g., SARS in 2003, Ebola in 2014; Brooks et al., 2020) the COVID-19 pandemic led to poorer mental health in the general public in early months by April of 2020 (Daly and Robinson, 2021). Predictors of psychological distress during the pandemic have included female gender, being a student, and physical health, while engaging in preventive measures (e.g., hand-washing, mask wearing) has been associated with lower distress (Moccia et al., 2020; Wang et al., 2020). Some trait-level individual characteristics such as anxious temperament have been associated with greater distress (Moccia et al., 2020).
1.1. College students
While college students may be at lower risk for serious complications associated with COVID-19, they face significant disruption following school closures and social distancing measures. Accordingly, reviews of college student mental health during the COVID-19 pandemic suggest a prevalence of depression and anxiety of 39% and 36%, respectively (Li et al., 2021). It has been suggested that emerging adulthood (ages 18–24) may represent a developmental stage with unique challenges imposed by COVID-19 (Gruber et al., 2020). These challenges may include disrupted social roles as a result of missing important experiences, returning to living with parents, and financial difficulties. These factors may explain greater risk of distress among this population compared to their non-student counterparts (Wang et al., 2020).
Quarantine and shelter-in-place measures may of be particular relevance to mental health during pandemics. Past pandemics and the related quarantine have been shown to be associated with negative psychological effects, although factors that confer risk for distress are less well established (Brooks et al., 2020). Among college students in China, urban residence, family income instability, not living with family, and relative or acquaintance with COVID-19 were found to be associated with more severe anxiety during the COVID-19 pandemic (Cao et al., 2020). Less is known about modifiable risk factors, or those that could be reasonably altered by the individual (e.g., Cairns et al., 2014). What's more, the majority of studies examining the psychological impact of pandemics are cross-sectional in nature or have taken place in the wake of the pandemic (Li et al., 2021). These factors limit the understanding of the magnitude of change in distress and pre-quarantine factors that confer risk. As such, the prospective examination of anxiety and depression following the COVID-19 spread is essential to understanding the scale of the psychological impact as well as risk and protective factors. The goal of the present study was to examine the early impact of COVID-19 in a convenience sample of participants enrolled in a separate study at the beginning of the 2019–2020 academic school year.
2. Method
2.1. Participants and procedures
Participants were college students at the University of Nevada, Reno who enrolled in a study beginning in August 2019 examining the effects of an intervention to prevent depression and anxiety. In the original study, students (N = 371) completed self-report measures assessing mental health status and health behavior on three occasions prior to disruptions that occurred as a result of the COVID-19 pandemic (August 2019, December 2019, February 2020). By the third data collection point (end of February 2020), 24 confirmed cases of COVID-19 were reported in the United States. A state of Emergency for the state of Nevada was declared on March 15th, and college students moved to remote instruction and operations shortly afterwards. Students in residential living were instructed to relocate off campus at this time. All participants completing the six-month follow up (N = 278) were invited to participate in an additional follow up on April 3rd, 2020, of which 205 participated. By the final date of collection (April 20th), 779,700 confirmed cases were reported by the COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (Dong et al., 2020). Participants were provided with contact information for the student counseling center, crisis call center, and additional psychological services available to students.
Participants were a mean age of 18.4 (SD = 0.99) and primarily (76.6%) female. Just over half of participants identified as White (54.1%), 18.5% identified as Asian/Pacific Islander, 16.1% Latinx, 4.4% identified as Black or African American, and 6.8% identified as other race/ethnicity. Of the sample, 37.6% reported an income below $49,999, 32.2% reported an income between $50,000 and $99,9999, and 29.8% reported an income over $100,000.
2.2. Measures
2.2.1. Pre and post pandemic
2.2.1.1. Depression symptom severity
Depression symptom severity was assessed using a 9-item questionnaire that identifies DSM symptoms for Major Depressive Disorder (PHQ-9; Kroenke et al., 2001; α = 0.90, 0.901 ). Scoring 10 or above on the PHQ-9 is associated with a sensitivity of 88% and a specificity of 88% for Major Depressive Disorder.
2.2.1.2. Suicidal ideation
Suicidal ideation was assessed using the PHQ-9 item 9. This item asks participants to indicate how often they have experienced, “Thoughts that you would be better off dead or hurting yourself in some way.” Responses include “not at all” (0), “several days” (1), “more than half the days “(2), or “nearly every day” (3).
2.2.1.3. Anxiety symptom severity
Anxiety symptom severity was measured using a commonly used 7-item scale which evaluates symptoms for Generalized Anxiety Disorder (GAD-7; Spitzer et al., 2006; α = 0.93, 0.92). Scoring 10 or above on the GAD-7 is associated with a sensitivity of 89% and specificity of 82% for an anxiety disorder diagnosis.
2.2.1.4. Functional impairment due to mental health symptoms
Functional impairment due to mental health symptoms was assessed using the PHQ-9 question assessing impairment associated with symptoms. Responses include “not difficult at all” (0), “somewhat difficult” (1), “very difficult” (2) or “extremely difficult” (3).
2.2.1.5. Physical activity
Physical activity was measured using a single item (“How many times a week do you usually do 30 min of moderate physical activity or walking that increases your heart rate or makes you breath harder than normal? (for example, mowing the lawn, carrying light loads, bicycling at a regular pace, or playing doubles tennis).” Participants indicated, “none” “1–2 times/week”, “3–4 times/week”, or “> 5 times/week” (Marshall et al., 2005).
2.2.1.6. Social engagement
Social engagement was assessed using four items adapted from a scale assessing college student social contact (Kim et al., 2016; α = 0.88, 0.72). While Cronbach's alpha was acceptable at T3, (α = 0.78), unsurprisingly it was not acceptable at T3 (α = 0.57) as the first two items [“Attended gatherings with friends or family”, and “Attended organized events (e.g., school, work, other social group)]” were likely substantially impacted by COVID-19 and related disruptions and as such unrelated to the final two items (“Spent time with friends or family” and “Chatted with friends or family”). As such, only the second two items were used to examine in-person social contact.
2.2.1.7. Hours of sleep
Hours of sleep were assessed using the single item (“On the average, how many hours did you sleep each night during the past 4 weeks?”) from the Medical Outcomes Study Sleep measure (MOS; Hays et al., 2005).
2.2.1.8. Diet
Dietary patterns were assessed using a 10-item assessment of healthy dietary habits (e.g., “Do you try to eat less sweets and pastries?”; Zazpe et al., 2011; α = 0.76, 0.80). Scores range from 0 to 10, with higher scores indicating a greater number of eating habits designated as healthy.
2.2.1.9. Perceived malleability of emotions
Beliefs about the malleability of emotions was measured using a 4-item scale developed by Tamir and colleagues (2007; α = 0.79, 0.80). High scores represent a belief that one's emotions are malleable whereas low scores indicate the belief that one's emotions are fixed and unchangeable (Schroder et al., 2016; Tamir, 2007). Believing emotions to be malleable been found to be associated with less psychological distress in several studies (Ford et al., 2018; Kneeland and Dovidio, 2019; Tamir, 2007).
2.2.1.10. Cognitive and behavioral avoidance
Cognitive and behavioral avoidance was measured using a 31-item scale known as the Cognitive-Behavioral Avoidance Scale (CBAS; Ottenbreit and Dobson, 2004; α = 0.96, 0.96). The scale covers four aspects of avoidance, including cognitive avoidance, behavioral avoidance, social and non-social avoidance. Items (e.g., “In order to avoid feelings of disappointment, I just try not to get too serious about work/school” and “I tend to make up excuses to get out of social activities”) are rated on a five-point scale (1 = “Not at all true for me” to 5 = “Extremely true for me”).
2.2.1.11. Experiential avoidance
Experiential avoidance was measured using the 7-item Acceptance and Action Questionnaire (AAQ-II; Bond et al., 2015; α = 0.94, 0.93). Higher scores indicate greater experiential avoidance, which represents difficulty in accepting painful emotional experiences (Hayes et al., 2006). Experiential avoidance has been conceptualized as a transdiagnostic process associated with the development of anxiety and depression (Levin et al., 2014).
2.2.2. Post-pandemic only
2.2.2.1. COVID-19 disruption
Participants were asked the extent that COVID-19 and related impacts have disrupted their daily activities (1 = “None at all,” to 5 = “A great deal”). Participants indicated the degree to which COVID-19 had a negative impact on their health, other people in their lives, their finances, their education, employment and relationships (1 ‘Strongly disagree”, 5 = “Strongly agree”). Participants indicated the extent to which they are worried about future consequences of COVID-19 across these same six domains.
2.2.2.2. COVID-19 protective behavior changes
Participants indicated the extent to which they engaged in protective behaviors including increasing handwashing, increasing hand sanitizer use, avoiding close contact with people who are sick, avoiding close contact with people who are not sick, avoiding spending time with people outside the home, covering their faces when coughing or sneezing, and cleaning/disinfecting surfaces (1 = “None at all”, 5 = “A great deal”).
2.2.2.3. Using substances to cope with COVID-19
An item of the Brief COPE (B-COPE; Carver, 1997) was used to examine the use of substances to cope with the pandemic. The full B-COPE scale includes 28-items assessing responses to stressful situations. The prompt was modified to specify, “These items deal with ways you've been coping with the COVID-19 spread and related impact on your life.” Substance use was assessed with the question “I've been using alcohol or other drugs to help me get through it.” Responses include 0 (“I haven't been doing this at all”), 1 (“I've been doing this a little bit”), 2 (“I've been doing this a medium amount), and 3 (“I've been doing this a lot”).
2.2.2.4. Seeking help to cope with COVID-19
An item of the Brief COPE (B-COPE; Carver, 1997) was used to examine help seeking. Help seeking was assessed with the question “I've been getting help and advice from other people.” Responses include 0 (“I haven't been doing this at all”), 1 (“I've been doing this a little bit”), 2 (“I've been doing this a medium amount), and 3 (“I've been doing this a lot”).
2.2.2.5. Housing
Participants were asked about their living circumstances (e.g., with family, roommates, alone, or other) and the number of individuals currently living in the household.
2.2.2.6. Online social engagement
The scale of in-person engagement (Kim et al., 2016) was modified to include the 5 items assessing virtual social engagement (e.g., “The following questions are about how often you have engaged in social activities VIRTUALLY OR ONLINE in the past week”). Participants were asked, “How often have you… used videochat (Zoom, Skype, Facetime) to attend gatherings with friends or family”, “Used videochat (Zoom, Skype, Facetime) to attend organized events (e.g., school, work, other)”, “Texted friends or family”, “Called friends or family” and, “Used social media to interact with friends or family.” Participants responded using a 5-point scale (1 = “Very rarely” to 5 = “Very frequently”). The scale did not have adequate reliability (α = 0.66) with the inclusion of the two videochat items. As such, these items were excluded, resulting in adequate reliability (α = 0.74).
2.2.2.7. Problematic internet use
Internet use was assessed using the Problematic Internet Use Questionnaire-Short Form (PIUQ-SF-6; Demetrovics et al., 2016; α = 0.81). This 6-item scale assesses problematic internet use amongst participants, specifically pertaining to how their internet habits cause negative impacts on their daily lives and wellbeing. Items (e.g., How often do you spend time online when you'd rather sleep?”) are rated on a 5-point scale (1 = “never” to 5 = “always/almost always”).
2.2.2.8. Perceived benefits related to adversity
Perceived benefits of the pandemic were assessed using the General Benefit Finding Scale (Cassidy et al., 2014; α = 0.96). Participants were asked to indicate on a 5-point Likert scale how much each of the 27 items were true for them. These items assess the ability of participants to find perceived benefits in the face of adversity (e.g., “In the last month, the spread of COVID-19 and related disruptions to my life… Led me to be more accepting of things.”).
2.2.2.9. Stress
Stress was assessed using the vulnerability subscale of the Perceived Stress Scale (PSS; Wickrama et al., 2013; α = 0.87). This measure consists of 7 items assessing the psychological vulnerability of participants (e.g., How often have you felt difficulties were piling up so high that you could not overcome them?”). Participants rated each item on a 5-point scale of (0 “never” to 4 = “very often”). Higher scores represent greater psychological vulnerability
3. Results
3.1. Anxiety and depression clinical cutoffs following COVID-19
In April of 2020 (T4), 59.0% and 51.2% were above the clinical cutoff score for depression on the PHQ-9 and GAD-7, respectively. Close to half (42.9%) were above clinical cutoffs for both anxiety and depression. More than two-thirds of the sample (67.3%) were above a clinical cutoff on either the PHQ-9 and GAD-7. This prevalence represents a drastic increase in symptom severity in February of 2020 (See Table 1 ). Pre-pandemic (T3), 128, or 62.1% of the sample were below the clinical cutoff score of 10 on the PHQ-9. Of this group, 53 (41.4%) were above this threshold at following COVID-19. Of the 137 (66.5%) participants below GAD-7 cutoffs in February, 50 (36.5%) were above the cutoff in April. Following the pandemic, 22.9% of students reported experiencing suicidal ideation within the past two weeks, and 38.5% reported significant impairment as a result of distress.
Table 1.
Prevalence of clinical cutoff scores pre and post COVID-19 pandemic (n = 205).
| Pre-Pandemic (T3) | Post-Pandemic (T4) | |
|---|---|---|
| GAD-7 ≥ 10 | 67 (32.7%) | 105 (51.2%) |
| PHQ-9 ≥ 10 | 75 (27.1%) | 121 (59%) |
| Both GAD-7 and PHQ-9 ≥ 10 | 56 (27.3%) | 88 (42.9%) |
| Either GAD-7 or PHQ-9 ≥ 10 | 87 (42.4%) | 138 (67.3%) |
| PHQ-9 Item 9 ≥ 1 | 51 (25.0%) | 47 (22.9%) |
| PHQ-9 Impairment | 46 (22.4%) | 79 (38.5%) |
T3: February 2020, T4: April 2020. PHQ-9 Item 9 scores ≥ 1 indicate report of suicidal ideation or thoughts of self-harm on at least several days in the past 2 weeks. PHQ-9 impairment scores ≥ 2 indicate significant impairment.
3.2. Changes in anxiety and depression symptom severity following COVID-19
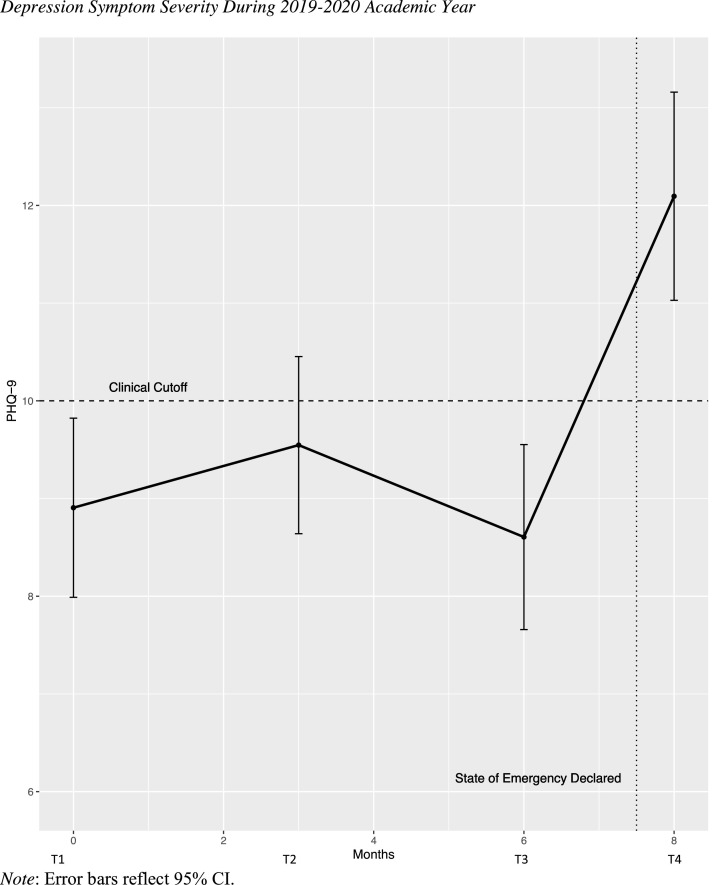
A repeated measures ANOVA was conducted to examine depression and anxiety symptom severity post-COVID-19 to symptom severity 2, 5, and 8 months prior. A significant effect of time was found for depression symptom severity, F(3, 167) = 22.90, p < .001, ηp2 = 0.29. Pairwise comparisons suggested that post-COVID-19 levels of depression was the only time that differed significantly (p < .05) from any other time (Table 2 ). The mean PHQ-9 score in April (T4) was 12.09 (SE = 0.54, 95% CI [11.03, 13.16]), greater than T1 (M = 8.91, SE = 0.46, 95% CI [7.99, 9.82]), T2 (M = 9.55, SE = 0.46, 95% CI [8.64, 10.45]), and T3 (M = 8.61, SE = 0.48, 95% CI [7.66, 9.55]). Results are presented in Fig. 1 .
Table 2.
Pairwise comparisons of mean depression and anxiety symptom severity during the 2019–2020 academic year.
| 95% CIDiff | ||||||
|---|---|---|---|---|---|---|
| MDiff | SEDiff | p | Lower | Upper | ||
| PHQ-9 | ||||||
| T4 vs. T1 | 3.19 | 0.51 | < .001 | 2.18 | 4.20 | |
| T4 vs. T2 | 2.55 | 0.49 | < .001 | 1.59 | 3.50 | |
| T4 vs. T3 | 3.49 | 0.43 | < .001 | 2.64 | 4.34 | |
| GAD-7 | ||||||
| T4 vs. T1 | 1.42 | 0.41 | .001 | 0.61 | 2.23 | |
| T4 vs. T2 | 1.99 | 0.40 | < .001 | 1.19 | 2.78 | |
| T4 vs. T3 | 2.38 | 0.40 | < .001 | 1.59 | 3.18 | |
Note. T1: August 2019, T2: December 2019, T3: February 2020, T4: April 2020.
Fig. 1.
Depression symptom severity during 2019–2020 academic year
Note: Error bars reflect 95% CI.
A significant effect of time was found for anxiety symptom severity, F(3, 167) = 13.00, p < .001, ηp2 = 0.19. Pairwise comparisons indicated that T1 did not differ from T2 (p = .143). T3 (February) differed from T1, (MDiff = −0.97, p = .016) with participants reporting a mean of 8.29 (95% CI [7.43, 9.15]) at the beginning of the school year and 7.32 (95% CI [6.38, 8.27]) at 6 months into the academic year. Results are presented in Fig. 2 . Post-COVID-19 levels of anxiety (M = 9.71, 95% CI [8.77, 10.64] were significantly higher than all other time points in the year (Table 2).
Fig. 2.
Anxiety symptom severity during 2019–2020 academic year
Note: Error bars reflect 95% CI.
3.3. Predicting psychological distress
Multiple linear regression analysis was used to examine predictors of depression symptom severity, anxiety symptom severity, and perceived stress during the COVID-19 pandemic, controlling for psychological distress prior to the impact of COVID-19. Predictors included demographic variables (i.e. gender, race/ethnicity, income), living circumstances (with family, number of individuals in the home), health behaviors (social contact, online social contact, internet use, moderate physical activity, diet, and sleep quality [hours slept per night]). The model also included psychological variables including perceived malleability of emotion, cognitive and behavioral avoidance, and experiential avoidance.
When controlling for pre-existing depression and anxiety symptom severity, female gender was associated with increases in perceived stress (β = 0.14, p = .030). Relative to their White counterparts, Asian or Asian-American-identifying participants reported lower levels of depression (β = −0.15, p = .011) and anxiety (β = −0.15, p = .013). Participants identifying as Latinx reported greater depression symptom severity (β = 0.12, p = .044).
For health behaviors, greater online social contact (texting, phone calls, and social media use) was significantly associated with higher PHQ-9 scores (β = 0.12, p = .027). Increases in problematic internet use was associated with increases in anxiety symptom severity (β = 0.18, p = .005) and approaching significance for greater depression symptom severity (β = 0.12, p = .055).
In examining the psychological factors that might predict psychological well-being, cognitive and behavioral avoidance was associated with more distress across all outcomes. Increased avoidance was associated with greater depression symptom severity (β = 0.28, p = .001), anxiety symptom severity (β = 0.21, p = .015), and perceived stress (β = 0.27, p = .003). Results are presented in Table 3 .
Table 3.
Predictors of psychological distress during COVID-19 controlling for pre-COVID-19 distress.
| Psychological Distress During the COVID-19 Pandemic (April 2020 [T4]) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Depression (PHQ-9) | Anxiety (GAD-7) | Stress (PSS) | ||||||||
| b | β | p | b | β | p | b | β | p | ||
| Demographics | ||||||||||
| Female (vs. Male) | 0.46 | 0.03 | .620 | 1.62 | 0.12 | .053 | 0.27 | 0.14 | .030 | |
| Latinx (vs. White) | 2.22 | 0.12 | .044 | −0.59 | −0.04 | .550 | −0.09 | −0.04 | .540 | |
| Black (vs. White) | −1.32 | −0.03 | .528 | −0.94 | −0.03 | .618 | 0.29 | 0.06 | .316 | |
| Asian (vs. White) | −2.60 | −0.15 | .011 | −2.27 | −0.15 | .013 | −0.04 | −0.02 | .779 | |
| Other (vs. White) | −1.08 | −0.04 | .451 | −0.46 | −0.02 | .725 | −0.05 | −0.02 | .797 | |
| Income middle (vs. low) | −1.01 | −0.07 | .265 | 1.16 | 0.09 | .155 | −0.12 | −0.07 | .317 | |
| Income high (vs. low) | −1.14 | −0.08 | .211 | 0.64 | 0.05 | .436 | 0.14 | 0.08 | .269 | |
| T4 Housing Circumstances | ||||||||||
| Living with family | 0.12 | 0.01 | .905 | −0.38 | −0.02 | .680 | −0.20 | −0.09 | .156 | |
| Household size | 0.13 | 0.03 | .636 | −0.01 | 0.00 | .971 | 0.06 | 0.11 | .118 | |
| T4 Health Behaviors | ||||||||||
| Healthy diet | 0.29 | 0.10 | .085 | 0.03 | 0.01 | .848 | −0.01 | −0.04 | .523 | |
| PA 1–2x/week (vs. none) | −0.07 | −0.01 | .954 | 0.39 | 0.03 | .715 | −0.05 | −0.03 | .763 | |
| PA 3–4x/week (vs. none) | 1.83 | 0.13 | .115 | 0.17 | 0.01 | .869 | 0.20 | 0.12 | .195 | |
| PA > 5x/week (vs. none) | 0.05 | 0.00 | .971 | 0.28 | 0.02 | .806 | 0.27 | 0.14 | .121 | |
| Hours of sleep | −0.03 | −0.08 | .143 | −0.02 | −0.07 | .217 | 0.00 | 0.02 | .790 | |
| Social contact | −0.16 | −0.03 | .628 | −0.06 | −0.01 | .843 | 0.02 | 0.02 | .739 | |
| Online social contact | 1.00 | 0.12 | .027 | 0.58 | 0.08 | .152 | 0.10 | 0.10 | .111 | |
| Problematic Internet use | 0.97 | 0.12 | .055 | 1.30 | 0.18 | .005 | 0.09 | 0.09 | .200 | |
| T4 Psychological Variables | ||||||||||
| Cog beh avoidance | 0.08 | 0.28 | .001 | 0.05 | 0.21 | .015 | 0.01 | 0.28 | .003 | |
| Experiential avoidance | 0.04 | 0.05 | .542 | 0.02 | 0.04 | .677 | 0.02 | 0.19 | .058 | |
| Emotion malleability beliefs | −0.18 | −0.03 | .653 | 0.04 | 0.01 | .913 | −0.07 | −0.08 | .221 | |
| Perceived benefits | −0.88 | −0.11 | .058 | −0.36 | −0.05 | .394 | −0.01 | −0.02 | .817 | |
| R2 = 0.60, AR2 = 0.54 | R2 = 0.55, AR2 = 0.49 | R2 = 0.46, AR2 = 0.38 | ||||||||
Note: Analyses control for pre-COVID-19 mental health (PHQ-9 and GAD-7 in February 2020 [T3]). All models were significant, p <0.001.
3.4. Predicting post-covid-19 distress from pre-covid-19 factors
The same health behaviors and psychological variables reported prior to the COVID-19 spread (T3) and related impact were then examined as predictors of psychological distress during the pandemic. Controlling for demographic variables, pre-existing symptom severity at T3 were related to symptom severity during the outbreak (T4), with T3 depression severity predicting levels of depression symptoms at T4 (β = 0.54, p < .001), and only T3 anxiety symptom severity (β = 0.39, p < .001) associated with T4 anxiety levels. For perceived stress, cognitive and behavioral avoidance at T3 was a significant predictor of stress at T4, with greater avoidance associated with more stress (β = 0.25, p = .008). Results are presented in Table 4 .
Table 4.
Pre-COVID-19 predictors of psychological distress during COVID-19.
| Psychological Distress During the COVID-19 Pandemic (April 2020 [T4]) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Depression (PHQ-9) | Anxiety (GAD-7) | Stress (PSS) | ||||||||
| b | β | p | b | β | p | b | β | p | ||
| T3 Psychological Distress | ||||||||||
| PHQ-9 | 0.63 | 0.55 | <.001 | 0.19 | 0.19 | .053 | 0.01 | 0.08 | .486 | |
| GAD-7 | 0.01 | 0.01 | .952 | 0.45 | 0.44 | <.001 | 0.02 | 0.11 | .324 | |
| T3 Health Behaviors | ||||||||||
| Social contact | 0.22 | 0.03 | .645 | −0.05 | −0.01 | .907 | −0.01 | −0.01 | .840 | |
| Hours of Sleep | −0.02 | −0.06 | .263 | −0.01 | −0.03 | .568 | 0.00 | −0.03 | .709 | |
| Healthy Diet | 0.04 | 0.02 | .804 | 0.03 | 0.01 | .829 | −0.02 | −0.07 | .354 | |
| PA 1–2x/week (vs. none) | −1.00 | −0.07 | .275 | −0.47 | −0.04 | .560 | 0.06 | 0.04 | .650 | |
| PA 3–4x/week (vs. none) | −0.59 | −0.03 | .594 | 1.11 | 0.07 | .258 | 0.07 | 0.04 | .637 | |
| PA > 5x/week (vs. none) | −2.08 | −0.08 | .182 | −1.74 | −0.08 | .204 | 0.16 | 0.05 | .449 | |
| T3 Psychological Variables | ||||||||||
| Cog Beh Avoidance | 0.02 | 0.07 | .344 | 0.03 | 0.12 | .118 | 0.01 | 0.25 | .008 | |
| Emotion Malleability Beliefs | −0.30 | −0.04 | .506 | 0.22 | 0.03 | .581 | −0.03 | −0.03 | .673 | |
| Experiential Avoidance | 0.04 | 0.07 | .399 | −0.02 | −0.04 | .693 | 0.01 | 0.09 | .388 | |
| R2 = 0.52, AR2 = 0.46 | R2 = 0.51, AR2 = 0.45 | R2 = 0.34, AR2 = 0.26 | ||||||||
Note: Analyses controlled for gender, race, income, and housing. All models were significant, p < .001. T3: February 2020, T4: April 2020.
3.5. COVID-19 disruption and protective behavior changes
More than half (56.1%) of participants reported a great deal of disruption to daily activities, with 28.3% reporting “a lot,” of disruption, 12.7% reporting “a moderate amount,” 2.5% reporting “a little,” and 0.5% reporting none at all. Education was the area reported by the largest number as significantly impacted, with 93.3% reported a significant negative impact on their education (See Table 5 ). Nearly all participants (94.7%) reported worry about the effect of COVID-19 on others in their lives and on their education (89.8%).
Table 5.
Self-reported impact of COVID-19.
| Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat agree | Strongly agree | ||
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| The COVID-19 spread has already had a significant negative effect on… | ||||||
| My health | 30 (14.6) | 29 (14.1) | 39 (19.0) | 89 (43.4) | 18 (8.8) | |
| Others I know | 7 (3.4) | 10 (4.9) | 20 (9.8) | 86 (42.0) | 81 (39.5) | |
| My financial circumstances | 12 (5.9) | 18 (8.8) | 30 (14.6) | 76 (37.1) | 69 (33.7) | |
| My education | 5 (2.4) | 3 (1.5) | 6 (2.9) | 52 (25.4) | 139 (67.8) | |
| My employment | 28 (13.7) | 13 (6.3) | 52 (25.4) | 33 (16.1) | 79 (38.5) | |
| My relationships | 8 (3.9) | 25 (12.2) | 37 (18.0) | 82 (40.0) | 53 (25.9) | |
| I am worried about the effect of COVID-19 on… | ||||||
| My health | 12 (5.9) | 20 (9.8) | 13 (6.3) | 88 (42.9) | 72 (35.1) | |
| Others I know | 0 (0.0) | 9 (4.4) | 2 (1.0) | 51 (24.9) | 143 (69.8) | |
| My financial circumstances | 10 (4.9) | 11 (5.4) | 23 (11.2) | 53 (25.9) | 108 (52.7) | |
| My education | 3 (1.5) | 7 (3.4) | 10 (4.9) | 39 (19.0) | 146 (71.2) | |
| My employment | 13 (6.3) | 18 (8.8) | 34 (16.6) | 39 (19.0) | 101 (49.3) | |
| My relationships | 8 (3.9) | 17 (8.3) | 23 (11.2) | 67 (32.7) | 90 (43.9) | |
| Behavior Change in Past Month | None at all | A little | A moderate amount | A lot | A great deal | |
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Increased handwashing | 3 (1.5) | 14 (6.8) | 34 (16.6) | 64 (31.2) | 90 (43.9) | |
| Increased hand sanitizer use | 23 (11.2) | 29 (14.1) | 45 (22.0) | 53 (25.9) | 55 (6.8) | |
| Avoiding close contact with people who are sick | 2 (1.0) | 6 (2.9) | 19 (9.3) | 55 (26.8) | 123 (60.0) | |
| Avoiding close contact with people who are healthy | 10 (4.9) | 24 (11.7) | 55 (26.8) | 63 (30.7) | 52 (25.4) | |
| Avoiding spending time with people outside of my home | 3 (1.5) | 17 (8.3) | 20 (9.8) | 46 (22.4) | 119 (58.0) | |
| Cover my face when I cough or sneeze | 19 (9.3) | 15 (7.3) | 27 (13.2) | 46 (22.4) | 98 (7.8) | |
| Cleaning/disinfecting surfaces | 3 (1.5) | 30 (14.6) | 39 (19.0) | 44 (21.5) | 89 (43.7) | |
| Coping with COVID-19 | None | A little bit | A medium amount | A lot | Not reported | |
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Using alcohol and other drugs to cope | 157 (76.6) | 22 (10.7) | 14 (6.8) | 6 (2.9) | 6 (2.9) | |
| Seeking Help from Others | ||||||
| Full sample (n = 205) | 50 (24.4) | 88 (42.9) | 44 (21.5) | 18 (8.8) | 5 (2.4) | |
| Of sample above clinical cutoff (n = 138) | 35 (25.4) | 57 (41.3) | 31 (22.5) | 14 (10.1) | 1 (0.7) | |
Clinical cutoff: ≥ 10 on GAD-7 or PHQ-9.
Participants reported engaging in protective behavior, with the majority of participants reporting at least a moderate amount of change, such as increasing handwashing (91.8%), and avoiding close contact with people who are sick (96.1%). Results are presented in Table 5.
Independent samples t-tests were conducted to examine differences in COVID-19-related disruption at T4. Women reported greater disruption to daily activities (M = 4.45, SD = 0.75) than did their male counterparts (M = 4.13, SD = 1.04), t(202) = −2.32, p = .022). Women also reported greater negative impact on their own health (M = 3.30, SD = 1.17) than did men (M = 2.74, SD = 1.29) t(202) = −2.78, p = .006, as well as a more negative financial impact (M = 3.93, SD = 1.10) than did men (M = 3.53, SD = 1.10), t(202) = −2.08, p = .039. Women also reported more worry about their own health (M = 4.04, SD = 1.09) than men (M = 3.47, SD = 1.25). A one-way ANOVA was conducted to examine differences in race/ethnicity in on COVID-19-related disruption and worry. No differences were found (all ps > 0.05).
3.6. Coping with COVID-19
Most students (76.6%) denied any use of alcohol or other drugs to cope with the pandemic and related impacts. Of concern, many students (25.4%) experiencing distress denied any help seeking from social or professional sources. See Table 5.
4. Discussion
The present study examined the course of anxiety and depression symptom severity among college students during the 2019–2020 academic year, before and after the COVID-19 pandemic and related impacts. Findings suggest a high prevalence of distress among college students. More than two thirds exceeded a clinical cutoff score on either the GAD-7 or PHQ-9. Distress in April of 2020 was higher than at any other time during the academic year. Mean PHQ-9 and GAD-7 scores increased by approximately four points from February to April of 2020. Student reported significant impairment associated with this distress. These findings are consistent with past studies showing high distress among students during the COVID-19 pandemic (Wang et al., 2020; Li et al., 2021) and demonstrates the magnitude of this distress compared with any other time during the academic year. Nearly one quarter of students reported suicidal ideation or thoughts about self-harm, although this did not appear to be an increase from pre-pandemic rates. Pre-existing mental health was a risk factor for distress during the early stages of the COVID-19 pandemic, with PHQ-9 and GAD-7 scores in February predicting greater distress in April. Of concern, of the group of students experiencing distress, one quarter denied seeking help from personal or professional sources. As such, it is critical to increase efforts to increase help-seeking among students, particularly those with pre-existing mental health concerns.
In keeping with prior work, women were more likely to experience greater anxiety symptom severity and greater stress, and Latinx students reported higher depression symptom severity (Moccia et al., 2020; Wang et al., 2020; Lin et al., 2021). This finding is particularly notable, however, as analyses controlled for mental health symptom severity before the pandemic, suggesting an outsized impact on these groups. For college women, this result could be explained by self-report of disruption and impact on their health and financial circumstances. While Latinx students did not report greater disruption than other groups, the Latinx population in the United States has experienced inequities in health, mental health, and access to care that may have been exacerbated by the pandemic (Macias Gil et al., 2020; Purtle, 2020).
When controlling for pre-existing distress, online social contact and problematic internet use were associated with greater distress. These findings are consistent with a relationship between problematic internet use and greater depression symptom severity (Demetrovics et al., 2016). These findings could reflect a relationship between pandemic-related media exposure and distress. For instance, in response to the Ebola crises, media prior to the crises, greater media exposure to Ebola-related news, and prior mental health diagnoses were all associated with greater Ebola-related worry, distress and impairment (Thompson et al., 2017). It is also possible that students engaging in more online social contact had a greater need for accessing social support, perhaps suggesting a greater disruption imposed by social distancing practices.
The most consistent predictor of distress was cognitive and behavioral avoidance, which predicted depression, anxiety and distress during the pandemic. This finding is consistent with research suggesting avoidance increases risk for both depression and anxiety (Hofmann, 2007; Ottenbreit and Dobson, 2008). Of course, avoidance of exposure to the coronavirus is part of the public health measures necessary to address the pandemic. However, items on the Cognitive and Behavioral Avoidance scale reflect avoidance of both safe situations and also avoidance of difficult thoughts (Ottenbreit and Dobson, 2004). Furthermore, avoidance prior to the pandemic also predicted greater stress during the pandemic, suggesting that the tendency to avoid difficult situations conferred risk even prior to mandatory social distancing. It may be important for clinicians to consider maladaptive patterns of avoidance in assessing risk for distress.
Other health behaviors that have been are associated with risk for depression and anxiety such as poor sleep quality, low physical activity, low social engagement, and unhealthy dietary patterns (Cairns et al., 2014; Emerson et al., 2018; Zimmermann et al., 2020) were not associated with greater distress. Similarly, while believing emotions to be malleable has been shown to predict distress in college students across the college transition (Kneeland and Dovidio, 2019; Levin et al., 2012; Tamir et al., 2007), endorsement of this belief as not associated with distress during the pandemic. It may be that these factors did not serve as protective factors immediately following the onset of the COVID-19 pandemic but could confer benefit in the long-term.
4.1. Limitations
This study has several important limitations. Given the observational nature of the study, it is not possible to draw causal conclusions regarding the effect of the COVID-19 pandemic. A strength of this study, however, was the ability to examine predictors when controlling for pre-existing mental health, thereby strengthening the causal direction of the interpretation. In addition, the primary purpose of the study was to examine the effect of an intervention on depression and anxiety in August 2019. While the intervention did not appear to have an impact on depression or anxiety at T4, it did influence the intended construct of perceived malleability of emotion at this time. As such, it is possible that students not given this intervention may have responded differently. In addition, while seeking help to cope with the pandemic was assessed, it is unclear the extent to which this included professional help-seeking. Efforts to increase access to mental health services during the pandemic are essential, as some evidence suggests that professional help-seeking has not increased despite increases in distress among youth (Upton et al., 2021).
The study was also limited by the potential for self-selection bias. The sample included only those participants who responded to a follow-up eight months following study enrollment. The sample was disproportionately female (76.2%), which is also generally true of college students on the whole (65.0% women; ACHA, 2018), although may be a larger share in the present study. These aspects may limit the generalizability of the results. Furthermore, the generalizability to other populations beyond college students is unclear. College students likely face consequences of the pandemic, such as moving home after living independently, that may differ from the general population.
4.2. Conclusion
The present study examined college student mental health over the course of the 2019–2020 academic year, prior to and during the COVID-19 pandemic. The multifaceted stressors accompanying the COVID-19 pandemic may be particularly likely to negatively impact mental health at a large scale due to the high degree of uncertainty, disruption to daily life, and economic impact (Gruber et al., 2020; Kumar and Rajasekharan Nayar, 2021). Results suggested a strikingly high prevalence of and increase in depression and anxiety among a college student sample. Certain groups may be at elevated risk for mental health concerns, including individuals with pre-existing psychological distress, women, and Latinx-identifying students. These results highlight the critical need to address inequities in mental health and mental health care, as individuals from minoritized groups have experienced a disproportionate impact of the pandemic on mental health. The present study also identified behaviors associated with greater distress during the pandemic, including online social contact, problematic internet use, and cognitive and behavioral avoidance. These factors may be important targets for intervention.
CRediT author statement
Martha Zimmermann: Conceptualization, Methodology, Data Analysis, Writing- Original Draft Preparation. Casandra Bledsoe: Conceptualization, Data Curation, Writing- Original Draft Preparation. Anthony Papa: Conceptualization, Writing – Review & Editing, Supervision.
Declaration of Competing Interest
Martha Zimmermann, Casandra Bledsoe, and Anthony Papa have no conflicts of interest to disclose.
Footnotes
α represents T3 and T3, respectively
References
- ACHA. (2018). American college health association-national college health assessment ii: university of nevada reno executive summary. Hanover, MD.
- Kumar A., Nayar R. COVID 19 and its mental health consequences. J. Mental Health. 2021;30(1):1–2. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- Bond F.W., Hayes S.C., Carpenter K.M., Orcutt H.K., Waltz T., Baer R.A., …, Waltz T. Preliminary psychometric properties of the acceptance and action questionnaire – ii : a revised measure of psychological flexibility and preliminary psychometric properties of the acceptance and action questionnaire – ii : a revised measure of psychologic. Behav. Ther. 2015;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am. Ed. 2020 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns K.E., Yap M.B.H., Pilkington P.D., Jorm A.F. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2014;169:61–75. doi: 10.1016/j.jad.2014.08.006. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol's too long: consider the brief cope. Int. J. Behav. Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cassidy T., McLaughlin M., Giles M. Benefit finding in response to general life stress: measurement and correlates. Health Psychol. Behav. Med. 2014;2(1):268–282. doi: 10.1080/21642850.2014.889570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021;136:603–609. doi: 10.1016/j.jpsychires.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demetrovics Z., Király O., Koronczai B., Griffiths M.D., Nagygyörgy K., Elekes Z., …, Urban R. Psychometric properties of the Problematic Internet Use Questionnaire Short-Form (PIUQ-SF-6) in a nationally representative sample of adolescents. PLoS One. 2016;11(8) doi: 10.1371/journal.pone.0159409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson N.D., Small G.W., Merrill D.A., Chen S.T., Torres-Gil F., Siddarth P. Behavioral risk factors for self-reported depression across the lifespan. Mental Health Prevent. 2018;12:36–41. doi: 10.1016/j.mhp.2018.09.002. [DOI] [Google Scholar]
- Ford B.Q., Lwi S.J., Gentzler A.L., Hankin B., Mauss I.B. The cost of believing emotions are uncontrollable: youths’ beliefs about emotion predict emotion regulation and depressive symptoms. J. Experiment. Psychol. 2018;147(8):1170–1190. doi: 10.1037/xge0000396. [DOI] [PubMed] [Google Scholar]
- Gruber, J., Prinstein, M., Abramowitz, J.S., Albano, A.M., Aldao, A., Borelli, J., & ... Weinstock, L. (2020). Clinical psychological science's call to action in the time of COVID-19. 10.31234/osf.io/desg9.
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav. Res. Ther. 2006;44(1):1–25. doi: 10.1016/J.BRAT.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hays R.D., Martin S.A., Sesti A.M., Spritzer K.L. Psychometric properties of the medical outcomes study sleep measure. Sleep Med. 2005;6(1):41–44. doi: 10.1016/j.sleep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Hofmann S.G. Cognitive factors that maintain social anxiety disorder: a comprehensive model and its treatment implications. Cogn. Behav. Ther. 2007;36(4):193–209. doi: 10.1080/16506070701421313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y., Wang Y., Oh J. Digital media use and social engagement: how social media and smartphone use influence social activities of college students. Cyberpsychol., Behav. Soc. Networking. 2016;19(4):264–269. doi: 10.1089/cyber.2015.0408. [DOI] [PubMed] [Google Scholar]
- Kneeland E.T., Dovidio J.F. Emotion malleability beliefs and coping with the college transition. Emotion. 2019 doi: 10.1037/emo0000559. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin M.E., Lillis J., Seeley J., Hayes S.C., Pistorello J., Biglan A. Exploring the relationship between experiential avoidance, alcohol use disorders, and alcohol-related problems among first-year college students. J. Am. Coll. Health. 2012;60(6):443–448. doi: 10.1080/07448481.2012.673522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin M.E., MacLane C., Daflos S., Seeley J.R., Hayes S.C., Biglan A., Pistorello J. Examining psychological inflexibility as a transdiagnostic process across psychological disorders. J. Contextual Behav. Sci. 2014;3(3):155–163. doi: 10.1016/j.jcbs.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang A., Wu Y., Han N., Huang H. Impact of the COVID-19 pandemic on the mental health of college students: a systematic review and meta-analysis. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.669119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, S., Schleider, J.L., Nelson, B., Richmond, L., & Eaton, N.R. ( 2021, March 9). Gender and Racial/Ethnic Disparities in Undergraduate and Graduate Students’ Mental Health and Treatment Use amid the COVID-19 Pandemic. doi: 10.31234/osf.io/qhy5j. [DOI] [PMC free article] [PubMed]
- Macias Gil R., Marcelin J.R., Zuniga-Blanco B., Marquez C., Mathew T., Piggott D.A. COVID-19 pandemic: disparate health impact on the Hispanic/Latinx population in the United States. J. Infect. Dis. 2020;222(10):1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall A.L., Smith B.J., Bauman A.E., Kaur S. Reliability and validity of a brief physical activity assessment for use by family doctors. Br. J. Sports Med. 2005;39(5):294–297. doi: 10.1136/bjsm.2004.013771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., …, Sani G. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbreit N.D., Dobson K.S. Avoidance and depression: the construction of the cognitive–behavioral avoidance scale. Behav. Res. Ther. 2004;42(3):293–313. doi: 10.1016/S0005-7967(03)00140-2. [DOI] [PubMed] [Google Scholar]
- Ottenbreit N.D., Dobson K.S. Elsevier; 2008. Avoidance. In Risk Fctors in Depression; pp. 447–470. [DOI] [Google Scholar]
- Purtle J. COVID-19 and mental health equity in the United States. Soc. Psychiatry Psychiatr. Epidemiol. 2020;55(8):969–971. doi: 10.1007/s00127-020-01896-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroder H.S., Dawood S., Yalch M.M., Donnellan M.B., Moser J.S. Evaluating the domain specificity of mental health–related mind-sets. Soc. Psychol. Personal Sci. 2016;7(6):508–520. doi: 10.1177/1948550616644657. [DOI] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tamir M. Implicit theories of emotion: affective and social outcomes across a major life transition. Article J. Personal. Soc. Psychol. 2007 doi: 10.1037/0022-3514.92.4.731. [DOI] [PubMed] [Google Scholar]
- Tamir M., John O.P., Srivastava S., Gross J.J. Implicit theories of emotion: affective and social outcomes across a major life transition. J. Pers. Soc. Psychol. 2007;92(4):731–744. doi: 10.1037/0022-3514.92.4.731. [DOI] [PubMed] [Google Scholar]
- Thompson R.R., Garfin D.R., Holman E.A., Silver R.C. Distress, worry, and functioning following a global health crisis: a national study of Americans’ responses to Ebola. Clin. Psychol. Sci. 2017;5(3):513–521. [Google Scholar]
- Upton E., Clare P.J., Aiken A., Boland V.C., De Torres C., Bruno R., …, Peacock A. Changes in mental health and help-seeking among young Australian adults during the COVID-19 pandemic: a prospective cohort study. Psychol. Med. 2021:1–9. doi: 10.1017/S0033291721001963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K.A.S., Ralston P.A., O'Neal C.W., Ilich J.Z., Harris C.M., Coccia C., … Lemacks J. Linking life dissatisfaction to health behaviors of older African Americans through psychological competency and vulnerability. Res. Aging. 2013;35(5):591–611. [Google Scholar]
- Zazpe I., Bes-Rastrollo M., Ruiz-Canela M., Sánchez-Villegas A., Serrano-Martínez M., Martínez-González M.A. A brief assessment of eating habits and weight gain in a Mediterranean cohort. Br. J. Nutr. 2011;105(5):765–775. doi: 10.1017/S0007114510004149. [DOI] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., …, Gu X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet North Am. Ed. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann M., Chong A.K., Vechiu C., Papa A. Modifiable risk and protective factors for anxiety disorders among adults: a systematic review. Psychiatry Res. 2020;285 doi: 10.1016/j.psychres.2019.112705. [DOI] [PubMed] [Google Scholar]