Abstract
Background
To evaluate the prognosis of acute cerebral infarction at 1-year follow-up in different circulation infarctions.
Methods
Clinical data of 858 consecutive patients with acute cerebral infarction were collected. Of the 858 cases, 21 (2.45%) were lost to follow-up and 837 completed follow-up and thus were enrolled in this study. At 1-year follow-up, death or moderate-to-severe dysfunction (modified Rankin Scale (mRS) ≥ 3 points) was regarded as the poor prognostic endpoint. Univariate analysis and multivariate logistic stepwise regression analysis were performed to assess the prognosis. The prediction probability of indicators was obtained for the multivariate model, and the receiver operating characteristic curve was delineated to calculate the area under the curve (AUC) to predict the fitness of the model.
Results
The older the age, the greater the probability of a poor prognosis. Patients with previous diabetes and cerebral infarction had a poor prognosis. The higher the National Institutes of Health Stroke Scale and mRS scores and the lower the Barthel index at admission, the worse the prognosis of the patients. The longer the hospital stay, the worse the prognosis of the patients. The prognosis of different circulation infarctions was different. The AUC of the multivariate model was AUC = 0.893, and the 95% confidence interval was 0.870–0.913, indicating a good fit. The prognosis of anterior circulation infarction (ACI) was worse than that of posterior circulation infarction (PCI) (P < 0.05). The prognosis of patients with ACI and PCI was not significantly different from that of patients with ACI or PCI alone (P > 0.05).
Conclusions
Diabetes, the Barthel index at admission and previous cerebral infarction are poor prognostic factors of acute cerebral infarction. The prognosis of ACI is worse than that of PCI. Different factors affect the prognosis of different circulatory system infarctions.
Keywords: Acute cerebral infarction, Anterior circulation, Posterior circulation, Prognosis, Prognostic factor
Background
Acute cerebral infarction accounts for approximately 85% of all strokes and has a high disability and mortality rate [1, 2]. Therefore, the prevention and treatment of acute cerebral infarction are important in this respect. Few clinical studies compared the aetiology and prognostic factors of different circulation strokes, and variable analyses are unavailable [3, 4]. Initial stroke severity, age, consciousness level, hyperglycaemia and stroke mechanisms are related to the prognosis after acute cerebral infarction, which may differ between anterior circulation infarction (ACI) and posterior circulation infarction (PCI) [5, 6]. The present study aimed to evaluate the prognostic factors of acute cerebral infarction at 1-year follow-up in different circulation infarctions.
Methods
Study object
This prospective cohort study was approved by local ethics associations and hospital ethics committees. All methods were performed in accordance with the ethical guidelines and regulations. This study was carried out in compliance with the STROBE guidelines. Data were consecutively collected on 858 patients with acute cerebral infarction who were hospitalised in the Department of Neurology, Aerospace Center Hospital, Peking University Aerospace School of Clinical Medicine from December 1, 2012 to November 4, 2015. Data included demographics, medial history, self-care ability before admission, stroke severity, biochemical indicators and imaging manifestations.
Inclusion criteria:
Age > 18 years;
Acute cerebral infarction which was initially diagnosed in accordance with World Health Organization standards and confirmed by brain MRI;
Time from onset to hospital admission ≤ 14 days;
The aetiology of each patient was grouped in accordance with TOAST classification (large atherosclerosis, small artery occlusion, cardiogenic embolism and other types with clear or unknown causes). Written informed consent was obtained from all patients enrolled or their next of kin.
Exclusion criteria:
Patients with haemorrhagic stroke or TIA;
Asymptomatic cerebral infarction;
Non-cerebrovascular disease events, such as primary brain tumours, subdural haemorrhage, Todd’s palsy, etc.;
Time interval from onset to hospital admission > 14 days;
Those who had not signed the informed consent.
Data collection
In this prospective cohort study, baseline data were collected by professionally trained neurologists through face-to-face interviews, and those data in the paper-based case report form were entered by trained personnel. The medical records of patients meeting the inclusion criteria were used to establish an electronic database with Epidata3.1 software, record data and information, and implement parallel double entry, including (1) basic information: gender, age, marital status, education level, occupation; (2) past medical and personal history: hypertension, diabetes, heart disease, cerebrovascular disease history (cerebral infarction, cerebral haemorrhage, transient ischaemic attack and so on), history of cardiogenic diseases (chronic heart failure, atrial fibrillation, coronary heart disease and so on), cancer, history of smoking, history of drinking and so on; (3) clinical features: time from onset to hospital admission, baseline US National Institutes of Health Stroke Scale (NIHSS) score, modified Rankin Scale (mRS) score, Barthel index and so on; (4) laboratory data: haemoglobin, blood glucose, blood lipids, renal function and so on; (5) imaging data and TOAST classification; (6) clinical data at 3-, 6-, 9- and 12-month follow-up.
Follow-up and outcome events
Follow-up visits were conducted by doctors over the phone or through face-to-face interviews. Telephone follow-up was performed by well-trained interviewers. Since the onset, the patients were followed up for 3, 6, 9 and 12 months with a time deviation of no more than 7 days. The primary outcome was poor prognosis, defined as ① death (after discharge) with acute cerebral infarction as the direct or indirect cause of death and ② moderate-to-severe disability and inability of self-care, that is, mRS ≥ 3 points.
Statistical methods
A normal distribution test was initially performed to compare the baseline characteristics which did not conform to a normal distribution. Continuous variables were represented by median and interquartile ranges, and non-parametric dual independent sample tests were conducted. For categorical variables, a χ2 test was applied. Yates continuity correction or Fisher’s exact probability test was carried out if necessary. Single-factor analysis was performed on the previously described data. Multivariate logistic stepwise regression analysis was performed with the index of P < 0.1. Prediction probabilities of the indexes were obtained for the multivariate model. Medcalc software was used to delineate the receiver operating characteristic curve (ROC) and calculate the area under the curve (AUC) to predict the fitness of the model. On the basis of the different circulatory systems of cerebral infarction, a multivariate logistic stepwise regression analysis was performed to evaluate the prognostic factors. Statistical analysis was performed using SPSS 25.0 (SPSS Inc., Chicago, IL) and MedCalc software with a two-tailed test, and statistical significance was considered at P < 0.05.
Results
General
A total of 858 patients met the inclusion criteria, of whom 21 cases (2.45%) were lost to follow-up and 837 completed follow-up and thus were enrolled in this study. Some data were missing in the profile, including haemoglobin in 19 patients, triglycerides in 19 patients, low-density lipoprotein in 19 patients, high-density lipoprotein in 19 patients, cholesterol in 19 patients, blood glucose in 17 patients, creatinine in 17 patients and urea nitrogen in 17 patients. Smoking and drinking were classified data. Each was divided into several levels. For example, smoking was divided into four levels. The number of patients in each level added up to the total number of patients in each group. One level comprised 437 non-smokers: 316 (72.3%) in the good prognosis group and 121 (27.7%) in the poor prognosis group.
Univariate and multivariate analysis
Univariate analysis revealed poor prognostic factors (P < 0.1), as shown in Table 1.
Table 1.
Univariate analysis of baseline characteristics and laboratory indicators of patients with acute cerebral infarction
| Clinical features and laboratory indicators | Good prognosis (n = 630) | Poor prognosis (n = 207) | Non-parametric test(Z or X2 )value | P value |
|---|---|---|---|---|
| Age (years), M(QR) | 64 (21) | 74 (16) | − 8.130 | 0.000 |
| Admission NIHSS, M(QR) | 2 (4) | 8 (9) | − 13.315 | 0.000 |
| Barthel index, M(QR) | 90 (30) | 35 (50) | − 14.781 | 0.000 |
| Hemoglobin (g/L), M(QR) | 141 (22) | 136 (27) | − 3.972 | 0.000 |
| Triglycerides (mmol/L), M(QR) | 1.40 (1.04) | 1.19 (1.09) | − 2.417 | 0.016 |
| Cholesterol (mmol/L), M(QR) | 4.56 (1.34) | 4.34 (1.83) | − 1.652 | 0.098 |
| Low-density lipoprotein (mmol/L), M(QR) | 2.59 (1.04) | 2.45 (1.42) | − 1.933 | 0.053 |
| High density lipoprotein (mmol/L), M(QR) | 0.75 (0.24) | 0.75 (0.28) | − 0.311 | 0.756 |
| Blood sugar (mmol/L), M(QR) | 6.58 (3.46) | 7.30 (4.28) | − 3.150 | 0.002 |
| Creatinine (umol/L), M(QR) | 71.10 (23.28) | 73.20 (27.80) | − 2.182 | 0.029 |
| Urea nitrogen (umol/L), M(QR) | 5.30 (2.23) | 6.00 (3.10) | − 4.174 | 0.000 |
| Gender, n(%) | 5.034 | 0.025 | ||
| Female | 182 (28.9%) | 77 (37.2%) | ||
| Male | 448 (71.1%) | 130 (62.8%) | ||
| History | ||||
| Diabetes, n(%) | 7.394 | 0.007 | ||
| No | 436 (69.2%) | 122 (58.9%) | ||
| Yes | 194 (30.8%) | 85 (41.1%) | ||
| Hypertension, n(%) | 3.615 | 0.057 | ||
| No | 225 (35.7%) | 59 (28.5%) | ||
| Yes | 405 (64.3%) | 148 (71.5%) | ||
| Hyperlipidemia, n(%) | 0.260 | 0.610 | ||
| No | 527 (83.7%) | 170 (82.1%) | ||
| Yes | 103 (16.3%) | 37 (17.9%) | ||
| Smoking, n(%) | 10.294 | 0.016 | ||
| No smoking | 316 (50.2%) | 121 (58.5%) | ||
| Quit smoking | 67 (10.6%) | 26 (12.5%) | ||
| Still smoking | 240 (38.1%) | 55 (26.6%) | ||
| Unknown | 71 (1.1%) | 5 (2.4%) | ||
| Drinking, n(%) | 15.959 | 0.014 | ||
| No drinking | 407 (64.6%) | 159 (76.8%) | ||
| Drink moderately | 146 (23.2%) | 28 (13.5%) | ||
| Moderate drinking | 33(5.2%) | 6 (2.9%) | ||
| Heavy drinking | 10(1.6%) | 1 (0.5%) | ||
| Unknown alcohol consumption | 12(1.9%) | 2 (1.0%) | ||
| Quit alcohol | 19 (3.0%) | 9 (4.3%) | ||
| Unknown | 3 (0.5%) | 2 (1.0%) | ||
| Cerebral Infarction, n(%) | 39.796 | 0.000 | ||
| No | 480 (76.2%) | 110 (53.1%) | ||
| Yes | 150 (23.8) | 97 (46.9%) | ||
| Cerebral hemorrhage, n(%) | 9.937 | 0.002 | ||
| No | 616 (97.8%) | 193 (93.2%) | ||
| Yes | 14 (2.2%) | 14 (6.8%) | ||
| TIA, n(%) | 3.256 | 0.071 | ||
| No | 623 (98.9%) | 201 (97.1%) | ||
| Yes | 7 (1.1%) | 6 (2.9%) | ||
| Heart failure, n(%) | 4.176 | 0.041 | ||
| No | 624 (99.0%) | 201 (97.1%) | ||
| Yes | 6 (1.0%) | 6 (2.9%) | ||
| Coronary Heart Disease, n(%) | 6.182 | 0.013 | ||
| No | 529 (84.0%) | 158 (76.3%) | ||
| Yes | 101 (16.0%) | 49 (23.7%) | ||
| Atrial fibrillation, n(%) | 12.796 | 0.000 | ||
| No | 589 (93.5%) | 177 (85.5%) | ||
| Yes | 41 (6.5%) | 30 (14.5%) | ||
| Tumor, n(%) | 10.673 | 0.001 | ||
| No | 615 (97.6%) | 192 (92.8%) | ||
| Yes | 15 (2.4%) | 15 (7.2%) | ||
| MRS at admission, n(%) | 263.515 | 0.000 | ||
| 0 | 13 (2.1%) | 2 (1.0%) | ||
| 1 | 175 (27.8%) | 6 (2.9%) | ||
| 2 | 192 (30.5%) | 24 (11.6%) | ||
| 3 | 154 (24.4%) | 36 (17.4%) | ||
| 4 | 87 (13.8%) | 77 (37.2%) | ||
| 5 | 9 (1.4%) | 62 (30.0%) | ||
| Length of hospital stay, n(%) | 124.628 | 0.000 | ||
| < 2 weeks | 402 (63.8%) | 67 (32.4%) | ||
| ≥ 2 weeks and < 4 weeks | 214 (34.0%) | 92 (44.4%) | ||
| ≥ 4 weeks | 14 (2.2%) | 48 (23.2%) | ||
| TOAST type, n(%) | 48.677 | 0.000 | ||
| Atherosclerotic stroke | 333 (52.9%) | 104 (50.2%) | ||
| Cardiogenic embolism | 20 (3.2%) | 27 (13.0%) | ||
| Arteriole occlusive stroke | 133 (21.1%) | 14 (6.8%) | ||
| Uncertain cause | 144 (22.8%) | 62 (30.0%) | ||
| Circulatory system, n(%) | 21.415 | 0.000 | ||
| Anterior circulatory system | 387 (61.4%) | 151 (72.9%) | ||
| Posterior circulatory system | 207 (32.9%) | 35 (16.9%) | ||
| Anterior and posterior circulatory system | 36 (5.7%) | 21 (10.2%) |
Continuous variables are represented by the median (interquartile range), and categorical variables are represented by the number of cases (percentage of the two groups)
Further multivariate logistic regression analysis was performed on the above poor prognosis (P < 0.1), and adjusting factors such as gender, smoking, drinking and diabetes were included. The results are shown in Table 2. The older the age, the greater the probability of a poor prognosis. Patients with previous diabetes and cerebral infarction had a poor prognosis. The higher the NIHSS and mRS scores at and the lower the Barthel index at admission, the worse the prognosis of patients; the longer the hospital stay, the worse the prognosis of the patients. The prognosis of different circulation infarctions was different. ACI has worse prognosis than PCI (P < 0.05); the prognosis of the patients with ACI–PCI did not differ significantly from that of the patients with ACI or PCI alone (P > 0.05).
Table 2.
Multivariate logistic analysis for prognostic factors of acute cerebral infarction at 1-year follow-up
| Prognostic factors | B | Standard error | Wald | Significance | Exp(B) | 95% CI of EXP(B) | |
|---|---|---|---|---|---|---|---|
| Age | 0.049 | 0.010 | 24.863 | 0.000 | 1.050 | 1.030 | 1.070 |
| History of diabetes | 0.570 | 0.228 | 6.227 | 0.013 | 1.768 | 1.130 | 2.767 |
| Infarction | 0.981 | 0.227 | 18.674 | 0.000 | 2.666 | 1.709 | 4.160 |
| Admission MRS | 0.324 | 0.161 | 4.053 | 0.044 | 1.382 | 1.009 | 1.894 |
| Admission NIHSS | 0.068 | 0.032 | 4.602 | 0.032 | 1.071 | 1.006 | 1.139 |
| Barthel index | − 0.024 | 0.007 | 11.003 | 0.001 | 0.976 | 0.963 | 0.990 |
| Circulatory systema | 8.461 | 0.013 | |||||
| 1 | 0.779 | 0.269 | 8.373 | 0.004 | 2.180 | 1.286 | 3.695 |
| 3 | 0.358 | 0.489 | 0.534 | 0.465 | 1.430 | 0.548 | 3.732 |
| Circulatory systemb | 8.461 | 0.013 | |||||
| 2 | − 0.779 | 0.269 | 8.373 | 0.004 | 0.459 | 0.271 | 0.778 |
| 3 | − 0.422 | 0.450 | 0.877 | 0.349 | 0.656 | 0.272 | 1.585 |
| Hospital stay | 0.794 | 0.176 | 20.475 | 0.000 | 2.213 | 1.569 | 3.121 |
Circulatory systema is the control of posterior circulatory infarction
Circulatory systemb is the control of the anterior circulation infarction
1 = Anterior circulatory system
2 = Posterior circulatory system
3 = Anterior and posterior circulatory system
ROC curve
The predicted probabilities of poor prognosis indicators for the multivariate model were calculated. MedCalc software was used to delineate ROC and calculate the AUC to predict the fitness of the model (AUC = 0.893, 95% confidence interval [CI], 0.870–0.913), as shown in Fig. 1.
Fig. 1.
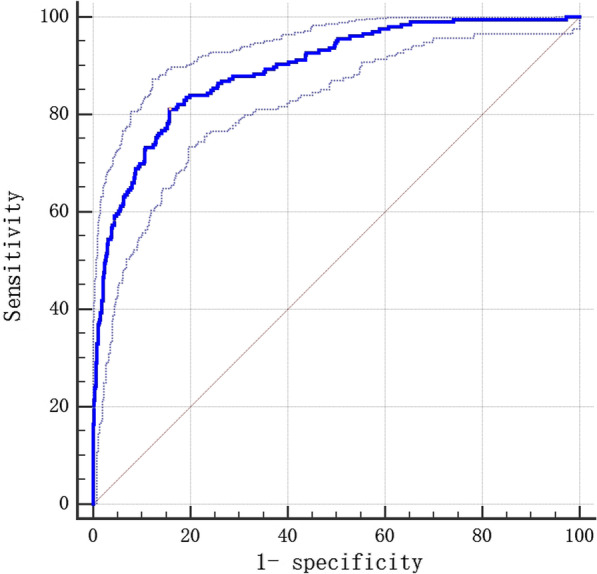
ROC curve of logistic multivariate prediction model for the prognosis of acute cerebral infarction patients at 1-year follow-up AUC = 0.893, P < 0.001, Youden IndexJ = 0.6535, Specificity = 84.29, Sensitivity = 81.07
Different circulation infarctions
The number of patients with ACI was 538, including 521 with infarction in the middle cerebral artery and 17 in the anterior cerebral artery. Meanwhile, the number of patients with PCI was 242, including 105 with infarction in the posterior cerebral artery, 46 in the basilar artery, 16 in the pontine branch, 17 in the superior cerebellar artery, 5 in the anterior inferior artery and 53 in the posterior inferior cerebellar artery. The number of patients with ACI-PCI was 57.
Group analysis
Univariate analysis according to different circulatory systems of cerebral infarctions had different prognostic factors. The results are shown in Table 3 (P < 0.1).
Table 3.
Univariate analysis of baseline characteristics and laboratory indicators in patients with ACI andPCI
| Clinical features and laboratory indicators | Good prognosis in ACI (n = 387) | Poor prognosis in ACI (n = 151) | Non-parametric test (Z or X2 value) | P value | Good prognosis in PCI (n = 207) | Poor prognosis in PCI (n = 35) | Non-parametric test (Z or X2 value) | P valve |
|---|---|---|---|---|---|---|---|---|
| Age (years), M(QR) | 64 (22) | 74 (16) | − 6.964 | 0.000 | 63 (19) | 74 (15) | − 3.286 | 0.001 |
| Admission NIHSS, M(QR) | 3 (4) | 8 (8) | − 10.742 | 0.000 | 2 (3) | 6 (10) | − 5.291 | 0.000 |
| Barthel index, M(QR) | 90 (30) | 40 (50) | − 12.124 | 0.000 | 90 (30) | 50 (60) | − 5.991 | 0.000 |
| Hemoglobin (g/L), M(QR) | 141 (22) | 136 (25) | − 2.743 | 0.006 | 141 (18) | 138 (31) | − 1.466 | 0.148 |
| Triglycerides (mmol/L), M(QR) | 1.395 (1.700) | 1.190 (1.750) | − 2.260 | 0.024 | 1.390 (1.030) | 1.510 (1.250) | − 0.255 | 0.799 |
| Cholesterol (mmol/L), M(QR) | 4.490 (1.350) | 4.540 (1.885) | − 0.262 | 0.793 | 4.640 (1.410) | 4.270 (1.840) | − 1.078 | 0.281 |
| Low-density lipoprotein (mmol/L), M(QR) | 2.580 (1.098) | 2.520 (1.430) | − 0.805 | 0.421 | 2.570 (1.050) | 2.480 (1.450) | − 0.877 | 0.380 |
| High density lipoprotein (mmol/L), M(QR) | 0.745 (0.230) | 0.760 (0.305) | − 1.132 | 0.258 | 0.750 (0.270) | 0.720 (0.260) | − 0.533 | 0.594 |
| Blood sugar (mmol/L), M(QR) | 6.470 (3.205) | 7.025 (4.218) | − 2.703 | 0.007 | 6.945 (3.980) | 8.120 (4.500) | − 1.842 | 0.065 |
| Creatinine (umol/L), M(QR) | 71.000 (24.000) | 72.800 (29.700) | − 1.507 | 0.132 | 71.100 (21.600) | 77.700 (29.600) | − 2.231 | 0.026 |
| Urea nitrogen (umol/L), M(QR) | 5.300 (2.350) | 6.000 (3.125) | − 3.427 | 0.001 | 5.400 (2.075) | 6.000 (3.800) | − 2.187 | 0.029 |
| Gender, n(%) | 4.675 | 0.031 | 0.002 | 0.960 | ||||
| Female | 109 (28.2%) | 57 (37.7%) | 60 (29.0%) | 10 (28.6%) | ||||
| Male | 278 (71.8%) | 94 (62.3%) | 147 (71.0%) | 25 (71.4%) | ||||
| History | ||||||||
| Diabetes, n(%) | 4.412 | 0.036 | 7.710 | 0.005 | ||||
| No | 277 (71.6%) | 94 (62.3%) | 134 (64.7%) | 14 (40.0%) | ||||
| Yes | 110 (28.4%) | 57 (37.7%) | 73 (35.3%) | 21 (60.0%) | ||||
| Hypertension, n(%) | 1.069 | 0.301 | 3.669 | 0.055 | ||||
| No | 144 (37.2%) | 49 (32.5%) | 69 (33.3%) | 6 (17.1%) | ||||
| Yes | 243 (62.8%) | 102 (67.5%) | 138 (66.7%) | 29 (82.9%) | ||||
| Hyperlipidemia, n(%) | 0.069 | 0.792 | 0.601 | 0.438 | ||||
| No | 324 (83.7%) | 125 (82.8%) | 171 (82.6%) | 27 (77.1%) | ||||
| Yes | 63 (16.3%) | 26 (17.2%) | 36 (17.4%) | 8 (22.9%) | ||||
| Smoking, n(%) | 9.009 | 0.029 | 0.981 | 0.806 | ||||
| No smoking | 187 (48.3%) | 86 (57.0%) | 108 (52.2%) | 19 (54.3%) | ||||
| Quit smoking | 36 (9.3%) | 18 (11.9%) | 28 (13.5%) | 6 (17.1%) | ||||
| Still smoking | 160 (41.4%) | 43 (28.5%) | 68 (32.9%) | 10 (28.6%) | ||||
| Unknown | 4 (1.0%) | 4 (2.6%) | 3 (1.4%) | 0 (0.0%) | ||||
| Drinking, n(%) | 11.319 | 0.079 | 4.865 | 0.561 | ||||
| No drinking | 252 (65.1%) | 117 (77.4%) | 131 (63.3%) | 25 (71.4%) | ||||
| Drink moderately | 90 (23.2%) | 20 (13.2%) | 47 (22.7%) | 7 (20.0%) | ||||
| Moderate drinking | 23 (5.9%) | 6 (4.0%) | 9 (4.4%) | 0 (0.0%) | ||||
| Heavy drinking | 6 (1.6%) | 1 (0.7%) | 4 (1.9%) | 0 (0.0%) | ||||
| Unknown alcohol consumption | 7 (1.8%) | 1 (0.7%) | 5 (2.4%) | 0 (0.0%) | ||||
| Quit alcohol | 8 (2.1%) | 5 (3.3%) | 9 (4.3%) | 3 (8.6%) | ||||
| Unknown | 1 (0.3%) | 1 (0.7%) | 2 (1.0%) | 0 (0.0%) | ||||
| Cerebral Infarction, n(%) | 18.812 | 0.000 | 8.944 | 0.003 | ||||
| No | 284 (73.4%) | 82 (54.3%) | 166 (80.2%) | 20 (57.1%) | ||||
| Yes | 103 (26.6%) | 69 (45.7%) | 41 (19.8%) | 15 (42.9%) | ||||
| Cerebral hemorrhage, n(%) | 9.636 | 0.002 | 0.127 | 0.722 | ||||
| No | 377 (97.4%) | 138 (91.4%) | 203 (98.1%) | 34 (97.1%) | ||||
| Yes | 10% (2.6%) | 13 (8.6%) | 4 (1.9%) | 1 (2.9%) | ||||
| TIA, n(%) | 0.243 | 0.622 | 0.269 | |||||
| No | 381 (98.4%) | 147 (97.4%) | 206 (99.5%) | 34 (97.1%) | ||||
| Yes | 6 (1.6%) | 4 (2.6%) | 1 (0.5%) | 1 (2.9%) | ||||
| Heart failure, n(%) | 1.690 | 0.194 | 0.467 | |||||
| No | 384 (99.2%) | 147 (97.4%) | 204 (98.6%) | 34 (97.1%) | ||||
| Yes | 3 (0.8%) | 4 (2.6%) | 3 (1.4%) | 1 (2.9%) | ||||
| Coronary Heart Disease, n(%) | 3.894 | 0.048 | 0.011 | 0.915 | ||||
| No | 321 (82.9%) | 114 (75.5%) | 176 (85.0%) | 30 (85.7%) | ||||
| Yes | 66 (17.1%) | 37 (24.5%) | 31 (15.0%) | 5 (14.3%) | ||||
| Atrial fibrillation, n(%) | 4.366 | 0.037 | 0.252 | 0.615 | ||||
| No | 360 (93.0%) | 132 (87.4%) | 197 (95.2%) | 32 (91.4%) | ||||
| Yes | 27 (7.0%) | 19 (12.6%) | 10 (4.8%) | 3 (8.6%) | ||||
| Tumor, n(%) | 10.072 | 0.002 | 0.312 | 0.576 | ||||
| No | 380 (98.2%) | 140 (92.7%) | 200 (96.6%) | 35 (100.0%) | ||||
| Yes | 7 (1.8%) | 11 (7.3%) | 7 (3.4%) | 0 (0.0%) | ||||
| MRS at admission, n(%) | 159.495 | 0.000 | 60.548 | 0.000 | ||||
| 0 | 10 (2.6%) | 2 (1.3%) | 2 (1.0%) | 0 (0.0%) | ||||
| 1 | 94 (24.3%) | 5 (3.3%) | 76 (36.7%) | 1 (2.9%) | ||||
| 2 | 128 (33.1%) | 18 (11.9%) | 55 (26.6%) | 5 (14.3%) | ||||
| 3 | 95 (24.5%) | 27 (17.9%) | 45 (21.7%) | 7 (20.0%) | ||||
| 4 | 54 (14.0%) | 58 (38.4%) | 27 (13.0%) | 14 (40.0%) | ||||
| 5 | 6 (1.5%) | 41 (27.2%) | 2 (1.0%) | 8 (22.8%) | ||||
| Length of hospital stay, n(%) | 78.143 | 0.000 | 30.651 | 0.000 | ||||
| < 2 weeks | 257 (66.4%) | 51 (33.8%) | 125 (60.4%) | 12 (34.3%) | ||||
| ≥ 2 weeks and < 4 weeks | 123 (31.8%) | 70 (46.3%) | 75 (36.2%) | 13 (37.1%) | ||||
| ≥ 4 weeks | 7 (1.8%) | 30 (19.9%) | 7 (3.4%) | 10 (28.6%) | ||||
| TOAST type, n(%) | 33.715 | 0.000 | 8.654 | 0.034 | ||||
| Atherosclerotic stroke | 204 (52.7%) | 75 (49.7%) | 106 (51.2%) | 20 (57.1%) | ||||
| Cardiogenic embolism | 12 (3.1%) | 13 (8.6%) | 5 (2.4%) | 4 (11.4%) | ||||
| Arteriole occlusive stroke | 95 (24.6%) | 11 (7.3%) | 37 (17.9%) | 3 (8.6%) | ||||
| Uncertain cause | 76 (19.6%) | 52 (34.4%) | 59 (28.5%) | 8 (22.9%) |
Continuous variables are represented by the median (interquartile range), and categorical variables are represented by the number of cases (percentage of the two groups)
Covariates of the multivariate analysis of the prognosis of different circulation infarctions were entered in accordance with the abovementioned undivided system to balance the differences in matching. Different circulatory systems had different poor prognosis factors. The results are shown in Tables 4, 5 and 6.
Table 4.
Multivariate logistic analysis for prognosis of patients with ACI at 1-year follow-up
| Prognostic factors | B | Standard error | Wald | Significance | Exp(B) | 95% CI of EXP(B) | |
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| Age | 0.050 | 0.011 | 20.282 | 0.000 | 1.052 | 1.029 | 1.075 |
| Cerebral infarction history | 1.019 | 0.265 | 14.774 | 0.000 | 2.771 | 1.648 | 4.659 |
| NIHSS at admission | 0.109 | 0.051 | 4.640 | 0.031 | 1.115 | 1.010 | 1.232 |
| Length of hospital stay | 0.793 | 0.213 | 13.884 | 0.000 | 2.211 | 1.456 | 3.356 |
| Barthel index | − 0.030 | 0.007 | 16.628 | 0.000 | 0.970 | 0.956 | 0.984 |
Table 5.
Multivariate logistic analysis for prognosis of patients with PCI at 1-year follow-up
| Prognostic factors | B | Standard error | Wald | Significance | Exp(B) | 95% CI of EXP(B) | |
|---|---|---|---|---|---|---|---|
| Lower limit | Lower limit | ||||||
| Cerebral infarction history | 0.976 | 0.494 | 3.900 | 0.048 | 2.655 | 1.007 | 6.995 |
| MRS at admission | 0.709 | 0.319 | 4.946 | 0.026 | 2.032 | 1.088 | 3.795 |
| Length of hospital stay | 0.785 | 0.349 | 5.056 | 0.025 | 2.193 | 1.106 | 4.349 |
Table 6.
Multivariate logistic analysis for prognosis with ACI-PCI at 1-year follow-up
| Prognostic factors | B | Standard error | Wald | Significance | Exp(B) | 95% CI of EXP(B) | |
|---|---|---|---|---|---|---|---|
| Lower limit | Lower limit | ||||||
| Cerebral infarction history | 2.097 | 0.982 | 4.561 | 0.033 | 8.144 | 1.188 | 55.820 |
| Hemoglobin | − 0.039 | 0.019 | 3.915 | 0.048 | 0.962 | 0.926 | 1.000 |
| Barthel index | − 0.058 | 0.017 | 11.908 | 0.001 | 0.943 | 0.913 | 0.975 |
Discussion
Acute cerebral infarction has high disability and mortality. Early prediction of long-term adverse outcomes of patients with acute cerebral infarction based on prognostic factors can help guide early intervention to obtain the best possible outcome and quality of life for patients with acute cerebral infarction. This prospective cohort study analysed the poor rains of patients with acute cerebral infarction during the 1-year follow-up and compared the prognoses of patients with different circulatory infarctions.
Age, NIHSS and mRS scores are closely related to the prognosis of cerebral infarction. The structure and function of blood vessels change with age, which could damage the function of vascular endothelial cells. The latter plays a vital role in the occurrence and development of stroke [7]. The higher the scores of NIHSS and mRS, the more severe the neurological damage and the worse the prognosis. Shortening the length of hospital stay can reduce the occurrence of complications and the psychological stress and depression of patients, thereby improving the prognosis. Early rehabilitation is a cost-effective and safe program which allows severely ill survivors to be discharged early and improve functional recovery [8]. Therefore, the longer the hospital stay, the worse the prognosis of patients. The results of this study are the same.
Diabetes is an independent risk factor for acute cerebral infarction. Patients with diabetes are prone to vascular injury, and the decrease in vascular elasticity affects their contraction function, thereby reducing the perfusion level of the ischaemic penumbra [9]. Long-term hyperglycaemia can also damage vascular endothelial cells, leading to increased circulatory dysfunction and ischaemia [10]. The results of this study showed that diabetes is a poor prognostic factor for acute ischemic stroke. The Barthel index score as a scoring system has a high predictive value for the prognosis of patients with acute cerebral infarction; the lower the score, the worse the prognosis [11]. The results of this study are consistent with them. Our study found that the patient’s medical history of cerebral infarction is a predictive indicator of a poor prognosis of acute cerebral infarction. In addition, the poor prognosis of different circulatory system infarctions plays a role. Studies have shown that patients with asymptomatic carotid artery stenosis and cerebral infarction have a higher risk of stroke recurrence and a poor prognosis during 10-year long-term follow-up [12].
At present, few studies compared the long-term adverse prognoses of patients with acute ACI or PCI. According to reports, the mortality rate of PCI is higher than 25%, and the risk of PCI recurrence is higher than that of anterior circulation ischaemia [13]. However, the development of neuroimaging has promoted the research of PCI diagnosis, and great progress has been achieved in the treatment of cerebrovascular diseases, thereby improving the prognosis of PCI [14, 15]. The NEMC-PCR Center’s research shows that 78.7% of patients with PCI have a good prognosis [16]. Another study showed that the 1-month, 3-month and 1-year mortality rates of patients with PCI are lower than those of patients with anterior circulation ischaemia (3.93%, 5.3%, 9.7% vs. 7.26%, 9.3%, 13.7%, respectively, P < 0.05). The proportion of PCI patients with poor prognosis a year after the onset is also lower than that of patients with anterior circulation ischaemia (6.5% vs. 15.2%, P < 0.05) [17]. This study found that different circulatory infarctions are poor predictors of the prognosis of acute cerebral infarction. The prognosis of different circulatory infarctions was different (P < 0.05). The prognosis of ACI was worse than that of PCI (OR value, 2.180; 95% CI, 1.286–3.695; P value, 0.004 < 0.01); the prognosis of patients with ACI–PCI was better than that of patients with ACI or PCI alone (mean P value > 0.05). In terms of prognostic factors, aetiology, clinical manifestations and prognosis, many scholars believe that PCI is different from ACI [3, 18]. Clinicians should treat patients with ACI, PCI or ACI–PCI based on specific causes and prognostic factors rather than the location of the infarction itself [19]. Multivariate analysis of this study showed that different circulatory infarctions have different prognostic factors. This result can serve as a basis for clinicians to estimate the prognosis and perform secondary prevention to shorten the length of hospital stay and thus improve the prognosis.
Given that this study is a single-centre study, the number of samples is limited. Moreover, the vessel segment (M1, M2, etc.) of the occlusion site was not specifically analyzed in this study. It is necessary to further study a larger sample size and analyze the location of vascular occlusion in order to better confirm the results of the current study.
Conclusions
Diabetes, the Barthel index at admission and previous cerebral infarction are poor prognostic factors of acute cerebral infarction. The prognosis of patients with ACI–PCI does not differ significantly from that of patients with ACI or PCI alone. The prognosis of ACI is worse than that of PCI. Different factors affect the prognosis of different circulatory system infarctions.
Acknowledgements
Not applicable.
Abbreviations
- mRS
Modified Rankin Scale
- NIHSS
National Institutes of Health Stroke Scale
- ROC
The receiver operating characteristic curve.
- AUC
the area under the curve
- BI
Barthel index
- ACI
Anterior circulation infarction
- PCI
Posterior circulation infarction
- ACI-PCI
Anterior and posterior circulation infarction
- TIA
Transient ischemic attack
- CHF
Chronic heart failure
- AF
Atrial fibrillation
- CHD
Coronary heart disease
Authors’ contributions
PG conceived and designed the study and helped to draft the manuscript. XY helped to draft the manuscript too. L-LC, W-TW, SZ, H-ML and X-YY performed the data collection and analyzed the data. L-LC wrote the paper. All authors approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This prospective cohort study was approved by the Ethics Committee of Peking University Aerospace School of Clinical Medicine. Written informed consent was obtained from all patients enrolled or their next of kin.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lawrence ES, Coshall C, Dundas R, Stewart J, Rudd AG, Howard R, et al. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke. 2001;32:1279–84. doi: 10.1161/01.STR.32.6.1279. [DOI] [PubMed] [Google Scholar]
- 2.Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–72. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 3.Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Consoli D, Wolfe CD, et al. Risk factors and outcome of subtypes of ischemic stroke. Data from a multicenter multinational hospital-based registry. The European Community Stroke Project. J Neurol Sci. 2006;244:143–50. doi: 10.1016/j.jns.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 4.De Marchis GM, Kohler A, Renz N, Arnold M, Mono ML, Jung S, et al. Posterior versus anterior circulation strokes: comparison of clinical, radiological and outcome characteristics. J Neurol Neurosurg Psychiatry. 2011;82:33–7. doi: 10.1136/jnnp.2010.211151. [DOI] [PubMed] [Google Scholar]
- 5.Wahlgren N, Ahmed N, Eriksson N, Aichner F, Bluhmki E, Dávalos A, et al. Multivariable analysis of outcome predictors and adjustment of main outcome results to baseline data profile in randomized controlled trials: Safe Implementation of Thrombolysis in Stroke-MOnitoring STudy (SITS-MOST) Stroke. 2008;39:3316–22. doi: 10.1161/STROKEAHA.107.510768. [DOI] [PubMed] [Google Scholar]
- 6.Ntaios G, Papavasileiou V, Faouzi M, Vanacker P, Wintermark M, Michel P. Acute imaging does not improve ASTRAL score’s accuracy despite having a prognostic value. Int J Stroke. 2014;9:926–31. doi: 10.1111/ijs.12304. [DOI] [PubMed] [Google Scholar]
- 7.Davignon J, Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation. 2004;109:Iii27-32. doi: 10.1161/01.CIR.0000131890.83839.5B. [DOI] [PubMed] [Google Scholar]
- 8.Gruther W, Pieber K, Steiner I, Hein C, Hiesmayr JM, Paternostro-Sluga T. Can early rehabilitation on the general ward after an intensive care unit stay reduce hospital length of stay in survivors of critical illness? A randomized controlled trial. Am J Phys Med Rehabil. 2017;96:607–15. doi: 10.1097/PHM.0000000000000718. [DOI] [PubMed] [Google Scholar]
- 9.Cipolla MJ, Porter JM, Osol G. High glucose concentrations dilate cerebral arteries and diminish myogenic tone through an endothelial mechanism. Stroke. 1997;28:405–10. doi: 10.1161/01.STR.28.2.405. [DOI] [PubMed] [Google Scholar]
- 10.Southerland AM, Johnston KC. Considering hyperglycemia and thrombolysis in the Stroke Hyperglycemia Insulin Network Effort (SHINE) trial. Ann N Y Acad Sci. 2012;1268:72–8. doi: 10.1111/j.1749-6632.2012.06731.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li QX, Zhao XJ. Value of the Barthel scale in prognostic prediction for patients with cerebral infarction. BMC Cardiovasc Disord. 2020;20:14. doi: 10.1186/s12872-019-01306-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Streifler JY, den Hartog AG, Pan S, Pan H, Bulbulia R, Thomas DJ, et al. Ten-year risk of stroke in patients with previous cerebral infarction and the impact of carotid surgery in the Asymptomatic Carotid Surgery Trial. Int J Stroke. 2016;11:1020–7. doi: 10.1177/1747493016660319. [DOI] [PubMed] [Google Scholar]
- 13.Flossmann E, Rothwell PM. Prognosis of vertebrobasilar transient ischaemic attack and minor stroke. Brain. 2003;126:1940–54. doi: 10.1093/brain/awg197. [DOI] [PubMed] [Google Scholar]
- 14.van der Hoeven EJ, Dankbaar JW, Algra A, Vos JA, Niesten JM, van Seeters T, et al. Additional diagnostic value of computed tomography perfusion for detection of acute ischemic stroke in the posterior circulation. Stroke. 2015;46:1113–5. doi: 10.1161/STROKEAHA.115.008718. [DOI] [PubMed] [Google Scholar]
- 15.Zhang DP, Ma QK, Zhang JW, Zhang SL, Lu GF, Yin S. Vertebral artery hypoplasia, posterior circulation infarction and relative hypoperfusion detected by perfusion magnetic resonance imaging semiquantitatively. J Neurol Sci. 2016;368:41–6. doi: 10.1016/j.jns.2016.06.043. [DOI] [PubMed] [Google Scholar]
- 16.Caplan LR, Wityk RJ, Glass TA, Tapia J, Pazdera L, Chang HM, et al. New England medical center posterior circulation registry. Ann Neurol. 2004;56:389–98. doi: 10.1002/ana.20204. [DOI] [PubMed] [Google Scholar]
- 17.Tao WD, Kong FY, Hao ZL, Lin S, Wang DR, Wu B, et al. One-year case fatality and disability after posterior circulation infarction in a Chinese hospital-based stroke study. Cerebrovasc Dis. 2010;29:376–81. doi: 10.1159/000281836. [DOI] [PubMed] [Google Scholar]
- 18.Kim JS, Nah HW, Park SM, Kim SK, Cho KH, Lee J, et al. Risk factors and stroke mechanisms in atherosclerotic stroke: intracranial compared with extracranial and anterior compared with posterior circulation disease. Stroke. 2012;43:3313–8. doi: 10.1161/STROKEAHA.112.658500. [DOI] [PubMed] [Google Scholar]
- 19.Zeng Q, Tao W, Lei C, Dong W, Liu M. Etiology and risk factors of posterior circulation infarction compared with anterior circulation infarction. J Stroke Cerebrovasc Dis. 2015;24:1614–20. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


