Abstract
Background
The 2017 ACC-AHA Hypertension Guideline recommends initiation of antihypertensive drug therapy based on blood pressure (BP) and an assessment of global cardiovascular disease (CVD) risk, but intensive lifestyle modification may lower BP to below recommended thresholds for treatment in some patients.
Methods
We examined the effects of lifestyle modification on calculated CVD risk and on the indications for BP-lowering medications in individuals with untreated hypertension. Participants included 144 adults with BP 130–160/80–99 mm Hg who were randomized to 16 weeks of DASH (Dietary Approaches to Stop Hypertension) diet plus behavioral weight management (DASH + WM), DASH diet alone (DASH), or Usual Care.
Results
The mean age of the study cohort was 52.0 years; the average baseline BP was 138 ± 9/86 ± 6 mm Hg. The 10-year CVD risk, as calculated by the Pooled Cohort Equations, was 5.7%. The adjusted 10-year risk fell to 4.4% in the DASH + WM group and to 5.0% in the DASH arm, but was not significantly changed (5.7%) in the Usual Care controls. The percentages of participants with guideline-based indications for antihypertensive drugs fell from 51% to 18% in the DASH + WM group and from 48% to 22% in the DASH group; and did not change significantly (49% to 44%) in the Usual Care group (P = 0.010 for the active intervention groups vs. Usual Care; P = 0.042 for DASH + WM vs. DASH).
Conclusions
These data demonstrate that in men and women with mildly elevated BP, lifestyle interventions can lower the calculated CVD risk and dramatically decrease the number of individuals for whom guideline-directed antihypertensive medication is indicated.
Keywords: antihypertensive drugs, blood pressure, DASH diet, hypertension, lifestyle modification
Graphical Abstract
Graphical Abstract.
Hypertension is an important risk factor for cardiovascular disease (CVD). Observational studies have demonstrated a graded association between both systolic blood pressure (BP) and diastolic BP and the risk of myocardial infarction or stroke.1,2 Worldwide, high BP is the leading cause of death and disability life-years,3,4 and in the United States it accounts for more deaths from CVD than any other modifiable risk factor.5
Lifestyle modifications are an important component of the therapy of hypertension. Adoption of the DASH (Dietary Approaches to Stop Hypertension) diet,6–8 decreasing dietary sodium intake,7 weight loss,9,10 and aerobic exercise9 lower BP and may reduce the need for drug therapy. A healthy lifestyle also favorably influences other CVD risk factors and thereby reduces overall cardiovascular risk.8
In middle-aged and older adults in whom BP remains elevated despite attempts at lifestyle modification, treatment with antihypertensive drugs reduces the incidence of heart failure, stroke, and myocardial infarction.11 The 2017 ACC-AHA Hypertension Guideline defines hypertension as a BP ≥130/80 mm Hg, and recommends reliance on not only the BP level but also the absolute CVD risk to guide implementation of pharmacologic therapy. Treatment of a lower risk patient with medical therapy is considered appropriate if the average BP exceeds 140/90 mm Hg. A treatment threshold of 130/80 mm Hg is recommended in patients with a high absolute risk of CVD events—i.e., those with clinical CVD, diabetes, chronic kidney disease, or a calculated 10-year CVD risk exceeding 10% based on the Pooled Cohort Equations.12
Although lifestyle interventions are recognized as effective in lowering BP in individuals with mild hypertension, we are not aware of prior studies that have quantified the impact of nonpharmacologic therapies on the need for drug treatment as defined by the 2017 ACC-AHA Hypertension Guideline. Moreover, the effects of lifestyle modification on calculated cardiovascular risk have not been extensively examined. The Exercise and Nutrition interventions for CardiOvasculaR hEalth (ENCORE) study assessed the effects of treatment with the DASH diet alone or in combination with a weight loss and exercise intervention on BP and other cardiovascular endpoints in hypertensive patients who were not taking BP-lowering medications.13 Both lifestyle interventions resulted in significant BP reductions, and low-density lipoprotein cholesterol was lowered in the diet plus weight management group.13,14 The principal objectives of this secondary analysis were to examine the impact of these interventions on (i) the calculated 10-year and lifetime CVD risk, as estimated from the Pooled Cohort Equations15; and (ii) the need for antihypertensive drug therapy, as recommended by the 2017 ACC-AHA Hypertension Guideline. These data will be of value to practitioners as they counsel patients with high BP on the potential benefits of lifestyle modification.
METHODS
Participants
Participants were 144 healthy, but overweight to obese, men and women with hypertension who were not treated with BP-lowering medications. Eligibility criteria included age >35 years, body mass index of 25–39.9 kg/m2, sedentary lifestyle, and BP 130–160/80–99 mm Hg. Exclusion criteria included clinical or laboratory evidence of cardiac disease, chronic kidney disease, or diabetes requiring insulin or oral hypoglycemic agents.
Study design
Details of the study protocol have been described previously.13 The study was approved by the institutional review board at Duke University Medical Center and written informed consent was obtained from each participant before enrollment. The trial is registered with clinicaltrials.gov (Identifier: NCT00571844).
Participants were recruited from physician referrals, community-based screenings, and advertisements. Eligibility was established during a series of screening visits that included a history and physical examination, measurement of height and weight, a fasting glucose and lipid profile, and determination of baseline BP. Participants were then randomized with equal probability to one of the following 16-week treatment conditions: (i) DASH diet plus behavioral weight management (DASH + WM); (ii) DASH diet alone (DASH); or (iii) Usual Care. Measurements of weight, fasting glucose and lipids, and BP were repeated at the conclusion of the intervention.
BP measurements
BP was measured by a trained examiner, blinded to the study group assignment, using a mercury sphygmomanometer, and adhering to the guidelines for proper BP measurement technique described in JNC-7.16 After the participant rested for 5 minutes in the seated position, 4 readings were acquired, each 2 minutes apart, and the results averaged. Measurements were acquired on 4 screening sessions over a 3–4-week period for baseline values, and on 4 visits to the research clinic during the final week of the intervention phase.
Interventions
Following randomization, participants entered a 2-week controlled feeding period during which they were provided meals according to their assigned dietary patterns (DASH diet, reduced calorie DASH diet, or control diet). Additional details of the study diets are described in a previous publication.13 Following the initial 2 weeks of controlled feeding, participants were instructed to maintain the DASH diet either with (DASH + WM) or without (DASH) weight loss.
(1) DASH alone: Participants in the DASH condition met weekly with the study nutritionist in small group sessions to discuss the DASH diet and receive feedback on their adherence to the diet. The goal of the weekly sessions was to assist participants in learning how to buy and prepare the appropriate foods, to enhance their motivation to choose to eat those foods, and to overcome obstacles to following the diet.
(2) DASH plus WM: Participants in the DASH + WM condition received the same instruction in the DASH diet as the DASH group, but their small group sessions also included a weekly cognitive-behavioral weight loss intervention and supervised exercise sessions 3 times per week. The cognitive-behavioral weight loss intervention emphasized reduced caloric consumption and utilized cognitive-behavioral strategies such as portion control and Appetite Awareness Training, a self-monitoring strategy in which individuals learn to identify internal cues of moderate hunger and fullness and to use these cues to guide their eating behavior. The supervised exercise routine consisted of 10 minutes of warm up exercises, 30 minutes of biking and/or walking or jogging at 70%–85% of the initial heart rate reserve, and 5 minutes of cool down exercises.
(3) Usual Care controls: Participants in the Usual Care condition were asked to maintain their usual dietary and exercise habits for the 4 months of the intervention.
Assessment of cardiovascular risk and indications for antihypertensive therapy
The 10-year and lifetime risks of CVD were calculated for each eligible subject using the ACC-AHA Pooled Cohort Equations.15 This CVD risk assessment tool is designed to estimate the 10-year risk of atherosclerotic events, including coronary death, nonfatal myocardial infarction, and fatal or nonfatal stroke in individuals 40–79 years of age. Similarly, lifetime risks of CVD and of CVD death were calculated for subjects ≤59 years of age.17
Participants were classified as having an indication for medical antihypertensive therapy based on recommendations of the 2017 ACC-AHA Hypertension Guideline. Criteria for drug therapy included either BP ≥140/90 mm Hg or BP ≥130/80 mm Hg in combination with an estimated 10-year CVD risk ≥10% or a diagnosis of diabetes.
Statistical analysis
Baseline characteristics of the study participants are expressed as means ± SD or number (percentage). Analyses of treatment-related changes in 10-year CVD risk, lifetime CVD risk, and risk of lifetime CVD death were examined using general linear models, controlling for age, sex, race, and the baseline level of the respective outcome, with treatment condition as the predictor of interest. Because risk equations for 10-year CVD risk are only valid for individuals aged 40–79 years, these analyses were restricted to participants within this age range (n = 131). Similarly, analyses of lifetime risks were limited to the 110 individuals ≤59 years of age. For analyses of indications for BP-lowering therapy, logistic regression models were employed in which the post-treatment indication for medical therapy of high BP (Yes or No) was modeled as the outcome, controlling for age, sex, and race, with treatment condition as the predictor of interest. Analyses of BP indications included all participants (n = 144). Within each model, 2 orthogonal contrasts were conducted comparing (i) both active treatment conditions (DASH + WM and DASH) with Usual Care, and (ii) DASH + WM with the DASH group. To examine potential moderating effects of baseline clinical characteristics, treatment group by baseline level interactions for age, gender, body mass index, systolic BP, and 10-year CVD risk were tested for 10-year risk and indications for antihypertensive medications as outcomes. All analyses were performed following the intent-to-treat principle. Missing data were handled using Markov chain multiple imputation within SAS (PROC MI). SAS version 9.4 (SAS Institute, Cary, NC) was used for all analyses.
RESULTS
Participant characteristics
A total of 144 participants were randomized to one of the lifestyle interventions: 49 to the DASH + WM group, 46 to the DASH condition, and 49 to Usual Care. Baseline characteristics of the sample are shown in Table 1. Participants were primarily middle aged (52 ± 10 years), white (60%), and female (67%), and had an average body mass index of 33.1 ± 3.9 kg/m2. Only 7% smoked cigarettes, and only 1 had diabetes. Average low-density lipoprotein cholesterol and high-density lipoprotein cholesterol levels were 126 ± 35 and 54 ± 14 mg/dl, respectively. The mean clinic BP was 138 ± 9/86 ± 6 mm Hg. The treatment groups were comparable across all baseline demographic and clinical variables.
Table 1.
Characteristics of the study cohort
| DASH + WM (N = 49) | DASH (N = 46) | Usual Care (N = 49) | All (N = 144) | |
|---|---|---|---|---|
| Age (years), m (SD) | 52.3 (10) | 51.8 (10) | 51.8 (9) | 52.0 (10) |
| Gender: female, % (N) | 69% (34) | 63% (29) | 69% (34) | 67% (97) |
| Ethnicity, % (N) | ||||
| Caucasian | 69% (34) | 50% (23) | 59% (29) | 60% (56) |
| African American | 31% (15) | 48% (22) | 39% (19) | 39% (86) |
| Asian | 0% (0) | 2% (1) | 2% (1) | 1% (2) |
| Hispanic | 4% (2) | 0 | 6% (3) | 3% (5) |
| Weight (kg), m (SD) | 93.9 (14) | 93.0 (14) | 92.6 (15) | 93.1 (14.1) |
| BMI (kg/m2), m (SD) | 33.5 (4.4) | 32.8 (3.4) | 33.0 (3.9) | 33.1(3.9) |
| Current smoker, % (N) | 4% (2) | 7% (3) | 10% (5) | 7% (10) |
| Diabetes % (N) | 2% (1) | 0% (0) | 0% (0) | <1% (1) |
| Systolic BP (mm Hg), m (SD) | 138.7 (8.2) | 137.6 (9.0) | 138.0 (9.5) | 138.1 (8.8) |
| Diastolic BP (mm Hg), m (SD) | 85.5 (6.8) | 86.1 (6.1) | 85.6 (5.8) | 85.8 (6.2) |
| Total cholesterol (mg/dl) | 209 (36) | 199 (41) | 206 (40) | 205 (39) |
| LDL cholesterol (mg/dl) | 128 (32) | 122 (37) | 126 (37) | 126 (35) |
| HDL cholesterol (mg/dl) | 55 (14) | 53 (14) | 55 (16) | 54 (14) |
Abbreviations: BMI, body mass index; BP, blood pressure; DASH, DASH diet; DASH + WM, DASH diet and weight management; HDL, high-density lipoprotein; LDL, low-density lipoprotein; N, number.
Baseline 10-year and lifetime risks of CVD and number of subjects with indications for antihypertensive medications are summarized in Table 2. The estimated 10-year risk of atherosclerotic events was 5.7 ± 6.1%, and exceeded 10% in 21 participants. The average estimated lifetime risk of CVD events was 21.3 ± 8.9%, and the lifetime risk of CVD death was 11.0 ± 6.1%. Criteria for treatment with antihypertensive medications, as defined by the 2017 ACC-AHA Hypertension Guideline, were present in 49% of the sample.
Table 2.
Baseline 10-year and lifetime risks of cardiovascular disease and indications for antihypertensive medications
| N | DASH + WM | DASH | Usual Care | All | |
|---|---|---|---|---|---|
| Ten-year risk of CVD events (%), mean (SD) | 131 | 5.1 (5.2) | 6.9 (7.9) | 5.2 (5.0) | 5.7 (6.1) |
| Ten-year risk of CVD events >10% (%), mean (SD) | 131 | 5 (11%) | 9 (23%) | 7 (16%) | 21 (16%) |
| Lifetime risk of CVD (%), mean (SD) | 110 | 22.5 (9.1) | 20.9 (9.7) | 20.3 (8.2) | 21.3 (8.9) |
| Lifetime risk of CVD death (%), mean (SD) | 110 | 11.7 (6.0) | 10.9 (6.4) | 10.5 (6.0) | 11.0 (6.1) |
| Indication for BP medication, % (N) | 144 | 25 (51%) | 22 (48%) | 24 (49%) | 71 (49%) |
Abbreviations: BP, blood pressure; CVD, cardiovascular disease; DASH, DASH diet; DASH + WM, DASH diet and weight management; N, number.
Overall effects of lifestyle interventions
The effects of the lifestyle interventions on dietary intake, body weight, and aerobic fitness have been described previously.13,14 Participants in the DASH intervention groups consumed significantly more fruits and vegetables, less saturated fat, and less dietary sodium than those randomized to the Usual Care control condition. The weight change was −8.7 kg and the percent improvement in peak VO2 (exercise capacity) was 19% in the DASH + WM group, compared with minimal changes in the other treatment arms. As summarized in Table 3, participants in the active treatment groups had significant reductions in systolic BP, diastolic BP, total cholesterol, and low-density lipoprotein cholesterol, and these improvements in BP and lipids were greater in the DASH + WM group than in the DASH group.
Table 3.
Changes in BP and serum lipids
| DASH + WM | DASH | Usual Care |
P
Treatment vs. Usual Care |
P
DASH + WM vs. DASH |
|
|---|---|---|---|---|---|
| Systolic BP (mm Hg), mean (95% CI) | −16.1 (−13.0, 19.2) | −11.2 (−8.1, −14.3) | −3.4 (−0.4, −6.4) | <0.001 | 0.020 |
| Diastolic BP, mean (95% CI) | −9.9 (−8.1, −11.6) | −7.5 (−5.8, −9.3) | −3.8 (−2.2, −5.5) | <0.001 | 0.048 |
| Total cholesterol (mg/dl), mean (95% CI) | −20.8 (−27.7, −13.8) | −8.1 (−1.0, −15.3) | 3.4 (−3.3, 9.9) | <0.001 | 0.020 |
| LDL cholesterol (mg/dl), mean (95% CI) | −14.2 (−8.2, −20.3) | −5.5 (0.7, −11.7) | 3.2 (−9.0, 2.5) | <0.001 | 0.044 |
| HDL cholesterol (mg/dl), mean (95% CI) | −0.1 (−1.8, 1.7) | −3.3 (−3.8, −2.7) | −0.5 (−2.1, 1.2) | 0.757 | 0.029 |
Abbreviations: BP, blood pressure; CI, confidence interval; DASH, DASH diet; DASH + WM, DASH diet and weight management; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Impact of lifestyle interventions on 10-year and lifetime risks of cardiovascular events
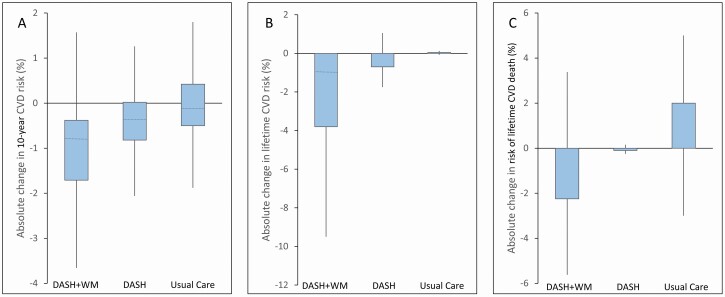
The 10-year risks of CVD events before and after the interventions were estimated using the Pooled Cohort Equations in the 131 participants 40–79 years of age, and the lifetime risks of CVD or cardiovascular death were calculated in the 110 individuals ≤59 years of age. The decreases in risk were most dramatic in the DASH + WM group and intermediate in the DASH group. The changes in risk estimates are shown in Figure 1, and the post-treatment risks, adjusted for baseline values, are summarized in Table 4. The 10-year risk, adjusted for baseline values, fell to 4.4 (3.9, 4.8)% in those randomized to the DASH + WM group and to 5.0 (4.5, 5.5)% in the DASH group, and did not change [5.7 (5.2, 6.2)%] in the Usual Care group (P < 0.001 for DASH + WM and DASH vs. Usual Care; P = 0.070 for DASH + WM vs. DASH). There was a baseline 10-year CVD risk × treatment interaction (P < 0.001); reductions in CVD risk were greater among participants with higher baseline risk scores, both for comparisons of the active interventions vs. Usual Care (P < 0.001) and DASH + WM vs. DASH (P = 0.005). Similarly, older participants exhibited a greater reduction in calculated CVD risk with the interventions (P < 0.012). The effects of lifestyle modification on 10-year CVD risk were not influenced by gender, body mass index, or baseline systolic BP. Similarly, there were trends for the lifetime CVD risk and the lifetime risk of CVD death to decrease with the active interventions (P = 0.099 for lifetime risk of CVD; P = 0.012 for lifetime risk of CVD death).
Figure 1.
Treatment-related changes in CVD risk, including the 10-year risk of CVD (a), the lifetime risk of CVD (b), and risk of lifetime CVD death (c). The upper and lower borders of the boxes represent the upper and lower quartiles, respectively, and the lines within the boxes represent medians. Abbreviations: CVD, cardiovascular disease; DASH, DASH diet; DASH + WM, DASH diet and weight management.
Table 4.
Post-treatment 10-year and lifetime risks of CVD and CVD death, adjusted for baseline values
| DASH + WM | DASH | Usual Care |
P
Treatment vs. Usual Care |
P
DASH + WM vs. DASH |
|
|---|---|---|---|---|---|
| Ten-year risk of CVD events (%), mean (95% CI) | 4.4 (3.9, 4.8) | 5.0 (4.5, 5.5) | 5.7 (5.2, 6.2) | <0.001 | 0.070 |
| Lifetime risk of CVD (%), mean (95% CI) | 17.7 (15.3, 20.2) | 18.0 (15.5, 20.6) | 20.6 (18.2, 22.0) | 0.099 | 0.138 |
| Lifetime risk of CVD death (%), mean (95% CI) | 9.8 (9.0, 10.6) | 10.2 (9.3, 11.0) | 11.2 (10.4, 12.0) | 0.012 | 0.071 |
Abbreviations: BP, blood pressure; CI, confidence interval; CVD, cardiovascular disease; DASH, DASH diet; DASH + WM, DASH diet and weight management.
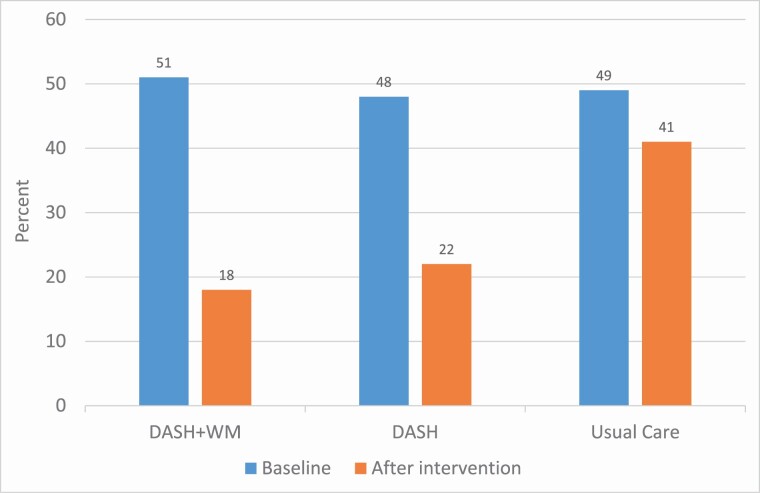
Impact of lifestyle interventions on indications for antihypertensive medications
The BP reductions and improved 10-year CVD risk observed in the active treatment groups resulted in significant decreases in the numbers of individuals meeting criteria for guideline-directed antihypertensive medical therapy, as depicted in Figure 2. For the entire cohort, indications for BP-lowering drugs, as defined by the ACC-AHA 2017 Hypertension Guideline, were present in 49% (n = 71) of participants at study entry. The percentages of subjects meeting criteria for treatment with antihypertensive medications fell from 51% to 18% in the DASH + WM group and from 48% to 22% in the DASH group, but did not significantly change (49% to 44%) in the Usual Care group (P = 0.002 for the active intervention groups vs. Usual Care; P = 0.581 for DASH + WM vs. DASH). The effects of the lifestyle interventions on indications for antihypertensive medications did not vary by age, gender, body mass index, baseline systolic BP, or calculated 10-year risk of CVD.
Figure 2.
Percentages of participants in the 3 treatment arms with an indication for antihypertensive therapy at baseline and at the completion of the intervention. Abbreviations: DASH, DASH diet; DASH + WM, DASH diet and weight management.
DISCUSSION
Our analysis of data from the ENCORE study demonstrates that lifestyle modification in untreated patients with mild essential hypertension can (i) reduce the calculated 10-year and lifetime risks of CVD, as calculated by the Pooled Cohort Equations, and (ii) dramatically reduce the number of patients who meet criteria for guideline-directed antihypertensive medical therapy. Significant effects were observed with adoption of the DASH diet, and the benefits were amplified by addition of a weight-loss program that included caloric restriction and aerobic exercise.
The reductions in 10-year and lifetime risks of CVD events in participants randomized to the lifestyle intervention groups were statistically and clinically significant, and were attributable to both lowering of BP and improvement in lipid profile. The effects of nonpharmacologic interventions on CVD risk scores have not been studied extensively. In the PREMIER clinical trial, untreated individuals with BP 120–159/80–95 mm Hg participated in 1 of 3 intervention groups: (i) implementation of “established” recommendations, including weight loss, moderate intensity physical activity, dietary sodium restriction, and moderation of alcohol consumption; (ii) an “established plus DASH” intervention, which also included the DASH diet; and (iii) an “advice only” comparison group. The relative risk ratio comparing 6-month to baseline Framingham risk was 0.86 (0.81, 0.91, P < 0.001) in the “established” group and 0.88 (0.83, 0.94, P < 0.001) in the “established plus DASH” intervention compared with “advice only.” 8 The relative reduction in calculated 10-year CVD risk with our DASH + WM intervention was approximately 20%, and the true reduction in risk may have been underestimated by the Pooled Cohort Equations. As described in our previous reports, exercise capacity, left ventricular mass, vascular stiffness, vascular endothelial function, and insulin resistance—measures of cardiometabolic risk or cardiovascular structure and function that are independent predictors of adverse cardiovascular outcomes but are not incorporated into most risk assessment tools—were improved by the DASH diet in combination with diet and exercise.13,14
The individual components of the ENCORE interventions are well-established nonpharmacologic therapies for high BP. The DASH eating plan, a diet that is high in fruits, vegetables, and low-fat dairy products, reduces systolic BP by approximately 11 mm Hg in hypertensives,6,7 as observed in ENCORE. In patients who are overweight or obese, weight loss is accompanied by a dose-dependent fall in BP,9,10 with an expected decrease of about 1 mm Hg for every kg of weight loss. Increased physical activity also results in a significant drop in BP,9,18 especially if combined with caloric restriction.9 Although lifestyle interventions are recognized as effective in lowering BP, few studies have quantified the impact of nonpharmacologic therapies on the need for drug treatment. In the TONE study, elderly hypertensive patients treated with a single medication were randomized to dietary sodium restriction, weight loss, both, or usual care interventions and withdrawal of antihypertensive medications was attempted after 30 days. At 6 months after drug withdrawal, only 29% of those in the weight loss and sodium restriction group required medication, were hypertensive (defined as BP >150/90 mm Hg), or experienced CVD events, compared with 60% of controls.19 In the PREMIER study, hypertension was defined as BP >140/90 mm Hg. The baseline hypertension prevalence was 38%, and at 6 months fell to 17% in the “established” group and to 12% in “established plus DASH” group, compared with 26% in the “advice only” comparison group.8 We are not aware of previous studies that examined the impact of lifestyle interventions on the indications for medical therapy outlined in the 2017 ACC-AHA Hypertension Guideline. Importantly, our analyses suggest that nearly two-thirds of patients with modestly elevated BP who meet criteria for antihypertensive drug therapy can achieve BPs in the desired range with an intensive lifestyle modification program, obviating the expense, inconvenience, and potential side effects of drug treatment.
Contemporary hypertension treatment guidelines advocate an assessment of global CVD risk to guide thresholds for initiating drug therapy, and recommend maintenance of a desirable body weight, regular aerobic exercise, and adoption of a healthy and balanced diet by all patients with high normal or elevated BP.12,20,21 In the 2017 ACC-AHA guideline, nonpharmacologic interventions are recommended for adults with elevated BP or hypertension, and drug therapy is advised at a threshold BP of 130/80 or 140/90 mm Hg, depending on the patient’s absolute risk of a CVD event.12 Our data suggest that implementation of an intensive lifestyle modification program may obviate the need for medications in some hypertensive patients. An intensive trial of diet and exercise may be warranted before prescribing medications in motivated patients who have modest BP elevations. This strategy is supported by the recent observation that some patients may be less likely to adhere to a healthy lifestyle after preventive medical therapy is initiated.22
Strengths of our study include the randomized, controlled design and blinded assessment of endpoints; the high level of adherence to the lifestyle interventions on the part of participants; and the low number of drop-outs. A limitation is the relatively small sample size at a single site. In addition, our intervention was only 16 weeks in duration and the long-term benefits of the behavioral modifications were not examined. Participants were generally healthy and had modest elevations in BP, and our results may not be generalizable to patients with more severe hypertension or multiple chronic illnesses. Moreover, participants were highly motivated and adherent to our research protocol. The extent to which similar levels of engagement in lifestyle modification can be achieved by patients in a typical clinical setting is uncertain. Nonetheless, the data provide compelling evidence that behavioral interventions can lead to a significant reduction in calculated CVD risk and a decrease in the need for antihypertensive medications in many patients with modest elevations in BP. Additional research is needed to examine the benefits of lifestyle modification in individuals with multiple comorbidities, and in treated patients with higher levels of BP.
FUNDING
This study was supported by grant HL074103 from the National Heart, Lung, and Blood Institute; grant M01-RR-30 from the General Clinical Research Center; grant 5UL1RR024128 from the National Center for Research Resources; and the National Institutes of Health Roadmap for Medical Research.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2. Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, White IR, Caulfield MJ, Deanfield JE, Smeeth L, Williams B, Hingorani A, Hemingway H. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383:1899–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Hassen Abate K, Akinyemiju TF, Ali R, Alvis-Guzman N, Azzopardi P, Banerjee A, Bärnighausen T, Basu A, Bekele T, Bennett DA, Biadgilign S, Catalá-López F, Feigin VL, Fernandes JC, Fischer F, Gebru AA, Gona P, Gupta R, Hankey GJ, Jonas JB, Judd SE, Khang Y-HH, Khosravi A, Kim YJ, Kimokoti RW, Kokubo Y, Kolte D, Lopez A, Lotufo PA, Malekzadeh R, Melaku YA, Mensah GA, Misganaw A, Mokdad AH, Moran AE, Nawaz H, Neal B, Ngalesoni FN, Ohkubo T, Pourmalek F, Rafay A, Rai RK, Rojas-Rueda D, Sampson UK, Santos IS, Sawhney M, Schutte AE, Sepanlou SG, Shifa GT, Shiue I, Tedla BA, Thrift AG, Tonelli M, Truelsen T, Tsilimparis N, Ukwaja KN, Uthman OA, Vasankari T, Venketasubramanian N, Vlassov VV, Vos T, Westerman R, Yan LL, Yano Y, Yonemoto N, Zaki MES, Murray CJLL, Abate KH, Akinyemiju TF, Ali R, Alvis-Guzman N, Azzopardi P, Banerjee A, Bärnighausen T, Basu A, Bekele T, Bennett DA, Biadgilign S, Catalá-López F, Feigin VL, Fernandes JC, Fischer F, Gebru AA, Gona P, Gupta R, Hankey GJ, Jonas JB, Judd SE, Khang Y-HH, Khosravi A, Kim YJ, Kimokoti RW, Kokubo Y, Kolte D, Lopez A, Lotufo PA, Malekzadeh R, Melaku YA, Mensah GA, Misganaw A, Mokdad AH, Moran AE, Nawaz H, Neal B, Ngalesoni FN, Ohkubo T, Pourmalek F, Rafay A, Rai RK, Rojas-Rueda D, Sampson UK, Santos IS, Sawhney M, Schutte AE, Sepanlou SG, Shifa GT, Shiue I, Tedla BA, Thrift AG, Tonelli M, Truelsen T, Tsilimparis N, Ukwaja KN, Uthman OA, Vasankari T, Venketasubramanian N, Vlassov VV, Vos T, Westerman R, Yan LL, Yano Y, Yonemoto N, El Sayed Zaki M, Murray CJLL. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA 2017; 317:165–182. [DOI] [PubMed] [Google Scholar]
- 4. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng ATA, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FGR, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Hanafiah KM, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CDH, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJC, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, Van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJL, Ezzati M. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009; 6:e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997; 336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 7. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER III, Simons-Morton DG, Karanja N, Lin PH; DASH-Sodium Collaborative Research Group . Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344:3–10. [DOI] [PubMed] [Google Scholar]
- 8. Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR; Writing Group of the PREMIER Collaborative Research Group . Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003; 289:2083–2093. [DOI] [PubMed] [Google Scholar]
- 9. Blumenthal JA, Sherwood A, Gullette EC, Babyak M, Waugh R, Georgiades A, Craighead LW, Tweedy D, Feinglos M, Appelbaum M, Hayano J, Hinderliter A. Exercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioning. Arch Intern Med 2000; 160:1947–1958. [DOI] [PubMed] [Google Scholar]
- 10. Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 2003; 42:878–884. [DOI] [PubMed] [Google Scholar]
- 11. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387:957–967. [DOI] [PubMed] [Google Scholar]
- 12. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:e13–e115.. [DOI] [PubMed] [Google Scholar]
- 13. Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med 2010; 170:126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Blumenthal JA, Babyak MA, Sherwood A, Craighead L, Lin PH, Johnson J, Watkins LL, Wang JT, Kuhn C, Feinglos M, Hinderliter A. Effects of the dietary approaches to stop hypertension diet alone and in combination with exercise and caloric restriction on insulin sensitivity and lipids. Hypertension 2010; 55:1199–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129:S49–S73. [DOI] [PubMed] [Google Scholar]
- 16. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 17. Lloyd-Jones DM, Braun LT, Ndumele CE, Smith SC Jr, Sperling LS, Virani SS, Blumenthal RS. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. Circulation 2019; 139:e1162–e1177. [DOI] [PubMed] [Google Scholar]
- 18. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136:493–503. [DOI] [PubMed] [Google Scholar]
- 19. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, Cutler JA. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA 1998; 279:839–846. [DOI] [PubMed] [Google Scholar]
- 20. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group . 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 21. Nakhla M, Howlett JG, Bacon SL, Firoz T, Gabor JY, Zarnke KB, Tremblay G, Cloutier L, Lewanczuk R, Gupta M, Nerenberg KA, Townsend RR, Don-Wauchope A, Ruzicka M, Campbell TS, Benoit G, Herman RJ, Vallée M, Rabi DM, Oh P, Milot A, Lamarre-Cliche M, Rey E, Fournier A, Penner SB, Gryn SE, Daskalopoulou SS, Kaczorowski J, Burgess E, Poirier L, Prebtani APH, Trudeau L, Feldman RD, Dionne J, Dasgupta K, Tran KC, McLean D, Schiffrin EL, Kline G, McFarlane PA, Côté A-M, Campbell NRC, Field T, Selby P, Padwal RS, Hamet P, Lavoie KL, Gilbert RE, Sivapalan P, Kuyper LM, Grégoire JC, Pipe A, Wein TH, Grover S, Feber J, Edwards C, Butalia S, Honos G, Roerecke M, Rabkin SW, Leung AA, Prasad GVR, Woo V, Arcand J, Magee LA, Harris KC, Shoamanesh A, Hill MD, Sharma M, Leiter LA, Tsuyuki RT, Jones C, McBrien K, Moe GW, Logan AG, Hegele RA, Dresser GK, Bolli P, Lindsay P, Gelfer M, Tobe SW, Hiremath S. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol 2018; 34:506–525. [DOI] [PubMed] [Google Scholar]
- 22. Korhonen MJ, Pentti J, Hartikainen J, Ilomäki J, Setoguchi S, Liew D, Kivimäki M, Vahtera J. Lifestyle changes in relation to initiation of antihypertensive and lipid-lowering medication: a cohort study. J Am Heart Assoc 2020; 9:e014168. [DOI] [PMC free article] [PubMed] [Google Scholar]