Abstract
Aims
This study sought to identify phenotypic variations among individuals with alcohol use disorder (AUD) that may, in part, help improve the effectiveness of existing AUD interventions.
Methods
Latent class analysis was conducted to examine the potential heterogeneity of AUD in a sample (N = 220; Mage = 51.19 years, standard deviation = 9.94; 37.7% female) of treatment-seeking participants diagnosed with AUD using DSM-5 criteria.
Results and Conclusions
Three distinct patterns of responses to the 11 DSM-5 AUD symptoms emerged: Class 1 (n = 114, 51.8%), Class 2 (n = 78, 35.5%) and Class 3 (n = 28, 12.7%). The identified profiles were further differentiated by demographics, alcohol-related constructs, individual difference characteristics and diagnostic and treatment variables. The findings have implications for refining AUD assessment as well as optimizing personalized treatment.
Short Summary: In a treatment-seeking sample (Mage = 51.19 years, 18–65 years), latent class analysis revealed three distinct groups based on the 11 DSM-5 Alcohol Use Disorder symptoms (Class 1, Class 2, Class 3). The identified groups differed on demographics, alcohol-related constructs, individual characteristics and diagnostic and treatment variables.
INTRODUCTION
Alcohol use disorder (AUD) remains a persistent public health problem in the USA with recent estimates, indicating that nearly 13% of the population meet criteria for current AUD with an increasing prevalence over the past decade (Grant et al., 2017). Despite the availability of treatments for AUD (e.g. Moyer et al., 2002), only about 25% of individuals with AUD seek formal treatment (Dawson et al., 2006). This may be due to a number of factors including lack of insurance, access to treatment, motivation to change or problem identification (e.g. Palmer et al., 2009). For those who do enter treatment, 40–60% of individuals continue to drink at the end of treatment (e.g. Hallford et al., 2003) and rates of relapse are greater than 50% among those who achieve abstinence at the end of treatment (e.g. Moos and Moos, 2006). Thus, improving current interventions for AUD remains a public health priority.
Individuals presenting for treatment vary greatly with respect to the number and type of self-reported AUD symptoms, leading to widely varying clinical presentations (Litten et al., 2015; Witkiewitz et al., 2018). In addition, alcohol problem severity is not simply a function of the extent of alcohol consumption; rather, individuals with similar levels of consumption often have varying degrees of social, employment and interpersonal problems (e.g. Witkiewitz, 2008). Some individuals may not drink heavily, but still experience alcohol-related consequences (Beseler et al., 2012), whereas others drink heavily for many years before the onset of significant problems (Cicchetti et al., 2016). A focus on examining and understanding the heterogeneity of AUD (e.g. Witkiewitz and Marlatt, 2007) may serve to guide the personalization of treatment for subsets of individuals.
Recently, the Alcohol and Addiction Research Domain Criteria (AARDoC) and the Addictions Neuroclinical Assessment (ANA) have been proposed as frameworks for advancing our understanding of AUD heterogeneity and as tools for advancing diagnosis and treatment (Litten et al., 2015; Kwako et al., 2016). These approaches include a range of neuroclinical measures (e.g. neuroimaging, genetic testing) and hold promise for tailoring treatment more effectively to the individual. Currently, the AARDoC is under development (Sher, 2015) and the ANA is undergoing validity testing (Votaw et al., 2020). While these frameworks represent a complex, theoretically driven approach to characterizing the known heterogeneity of AUD, a straightforward, accessible, empirically derived approach using information that is (a) familiar to clinicians and (b) has the potential to inform treatment (e.g. Babor and Caetano, 2006) may have significant clinical utility. The DSM-5 (APA, 2013) satisfies both recommendations.
The DSM-5 is the most frequently used tool for diagnosing AUD in clinical practice and includes several changes for the diagnosis of AUD, when compared to the previous DSM-IV-TR version (APA, 2000). Most notably, DSM-5 no longer distinguishes between alcohol abuse and dependence; instead, it introduces a unidimensional construct termed AUD (NIAAA, 2016). The DSM-5 criteria for AUD consist of 11 items that encompass abuse and dependence criteria and negative consequences related to alcohol use. This unidimensional model resolved the issue of diagnostic orphans (i.e. those who met only two abuse criteria and no dependence criteria and thus could not be given a diagnosis nor could they receive insurance reimbursable treatment) and resolved questions about the relationship between abuse and dependence that was difficult to characterize (Hasin et al., 2013). In addition, to increase diagnostic validity, DSM-5 added a craving item to the AUD criteria and removed an item inquiring about legal problems. The DSM-5 also specifies AUD severity as mild, moderate or severe based on the number of symptom criteria endorsed. Mild AUD is specified when 2–3 items are endorsed, moderate AUD when 4–5 items are endorsed and severe AUD when 6 or more items are endorsed.
This revised DSM-5 conceptualization characterizes AUD as a heterogeneous disorder, suggesting that there may be different phenotypes of AUD. There can be significant clinical utility in characterizing different typologies of AUD, including the prediction of treatment outcomes, providing patients with more specific information about their condition and improving diagnostic accuracy in service of selecting a targeted, personalized treatment (e.g. Casey et al., 2013). Recent studies examining the heterogeneity of DSM-5 AUD symptom criteria have recruited college students in the USA (Rinker and Neighbors, 2015), a general US population (Casey et al., 2013), a general Brazilian population (Castaldelli-Maia et al., 2014), young adults in Australia (Swift et al., 2016) and an elderly sample in Denmark (Mejldal et al., 2020). These studies found classes of individuals ranging from mild to severe AUD and have generally concluded that AUD severity exists on a continuum. Notably, three of these studies did not include treatment-seeking individuals diagnosed with AUD, and thus, the findings from these studies may not generalize to treatment-seeking samples. Also, data from non-clinical samples do not provide clinicians with the information needed to tailor treatment for individuals seeking treatment for AUD. The study by Mejldal et al. (2020) examined the heterogeneity of AUD among a clinical sample of elderly outpatients and found no connection between DSM-5 latent classes and alcohol consumption at the end of treatment. However, as noted by the authors, AUD among elderly adults is generally less severe compared to middle-aged and younger individuals, and treatment of older adults with AUD is often more successful.
In order to understand if there are distinct classes of AUD for a wider age range of adults (i.e. 18–65), the current study utilized a person-centered analytic technique, latent class analysis (LCA; e.g. Lanza and Rhoades, 2013), to identify patterns of responses to the 11 DSM-5 symptom criteria among a sample of treatment-seeking individuals diagnosed with AUD. More specifically, the LCA analysis tells clinicians and researchers not only the number of, but also which symptoms an individual is likely to endorse as opposed to the DSM-5 treating all symptoms as equivalent and merely counting how many symptoms the individual endorsed. The DSM-5 approach of counting symptoms obscures individual variability by ignoring the content of the endorsed items. An LCA brings parsimony to a heterogeneous diagnosis like AUD by identifying common symptom patterns.
To further validate the identified AUD classes, a series of potential correlates of the AUD classes were examined, including demographics, alcohol-related constructs, individual difference characteristics and diagnostic and treatment variables.
METHOD
Participants
Participants (N = 220) were recruited via radio and television advertisements for an outpatient alcohol treatment study (Stasiewicz et al., 2019). Study participants were (a) men and women between the ages of 18 and 65 years, (b) met DSM-5 criteria for AUD, (c) consumed alcohol in the past 3 months, (d) lived within commuting distance of the treatment site and (e) provided written informed consent. Exclusion criteria included: (a) diagnosis of a severe mental illness (i.e. schizophrenia, current bipolar disorder), (b) current drug use diagnosis other than tobacco or marijuana, (c) attended substance use disorder treatment during the past 6 months and (d) legally mandated to attend treatment.
The Institutional Review Board at the University at Buffalo approved the study. Of the 359 men and women screened, 65 (18.1%) were ineligible and 66 (18.4%) were no longer interested or lost to contact prior to study enrollment. Of the remaining 228 (63.5%) individuals who completed the in-person baseline assessment, 8 (2.2%) were ineligible. Thus, analyses are based on the remaining 220 individuals who enrolled in the study.
Procedure
All phone interviews, assessments and treatment occurred at a publicly funded outpatient substance use clinic in Buffalo, NY. Participants calling in response to radio and television advertisements were screened by phone for eligibility, which included questions regarding recent alcohol use, and treatment-related measures (e.g. commitment to change). At the conclusion of the telephone screen, those who were eligible to continue were scheduled for an in-person baseline assessment session approximately 1 week later, which involved multiple self-report questionnaires and a semi-structured interview to determine diagnoses for alcohol and substance use disorders. Individuals who were eligible at baseline were enrolled in a 12-week cognitive–behavioral treatment study and participated in an end-of-treatment assessment. The current data are derived from this parent study, which was designed to investigate pretreatment changes in drinking (Stasiewicz et al., 2019).
Measures
Demographics
Information on participants’ age, gender, level of education, marital status and ethnicity were collected at the phone screen. Information about participants’ income was collected at the baseline interview. Twelve levels of past-year income were assessed (e.g. 1 = 0 to less than $1000, 12 = $80,000 or more) and those levels were collapsed into four levels for subsequent analyses (See Table 3).
Table 3.
AUD class differences in demographics and potentially related constructs
| Class 1 (n = 114, 51.8%) |
Class 2 (n = 78, 35.5%) |
Class 3 (n = 28, 12.7%) |
F/χ2 | Partial η2 | ||||
|---|---|---|---|---|---|---|---|---|
| M/% | SD | M/% | SD | M/% | SD | |||
| Age | 50.14 | 9.94 | 51.33 | 10.51 | 55.04 | 7.28 | F (2, 217) = 2.78 | 0.03 |
| Gender | χ2 (2) = 11.74** | |||||||
| Male | 66.7% | 48.7% | 82.1% | |||||
| Female | 33.3% | 51.3% | 17.9% | |||||
| Race | N/A | |||||||
| White/Caucasian | 86.7% | 85.9% | 92.9% | |||||
| American Indian/Alaskan Native | 0.0% | 2.6% | 0.0% | |||||
| Native Hawaiian/Pacific Islander | 0.9% | 0.0% | 0.0% | |||||
| Black/African-American | 8.9% | 10.3% | 7.1% | |||||
| Other | 3.5% | 1.2% | 0.0% | |||||
| Hispanic/Latino (yes) | 7.1% | 3.5% | 3.8% | χ2 (2) = 0.68 | ||||
| Years of education | 14.99 | 2.33 | 15.50 | 2.68 | 15.21 | 2.22 | F (2, 215) = 1.00 | 0.01 |
| Marital status | N/A | |||||||
| Single, never married | 16.7% | 16.4% | 10.7% | |||||
| Single, divorced | 16.7% | 17.7% | 14.3% | |||||
| Single, widowed | 1.8% | 1.4% | 0.0% | |||||
| Single, married but separated | 4.4% | 5.9% | 7.1% | |||||
| Living with partner as if married | 7.8% | 7.7% | 10.7% | |||||
| Married and living with spouse | 52.6% | 50.9% | 57.2% | |||||
| Income | χ2 (6) = 11.08 | |||||||
| <$10,000 | 2.7% | 6.4% | 3.7% | |||||
| $10,000–40,000 | 23.9% | 29.5% | 18.5% | |||||
| $40,000–70,000 | 33.6% | 25.6% | 11.1% | |||||
| <$70,000 | 39.8% | 38.5% | 66.7% | |||||
| Daily drinkers (vs. non) | 28.1% | 32.1% | 32.1% | χ2 (2) = 0.81 | ||||
| Age at which drinking began | 18.01 | 6.93 | 18.77 | 6.43 | 18.86 | 9.25 | F (2, 217) = 0.34 | 0.01 |
| Age at which drinking became a problem | 31.68b | 12.78 | 36.69c | 13.61 | 39.93c | 14.83 | F (2, 217) = 5.90** | 0.05 |
| AUDIT-C | 15.70b | 4.15 | 12.74c | 3.77 | 10.86c | 3.88 | F (2, 217) = 23.00*** | 0.18 |
| ADS | 17.18b | 6.19 | 12.35c | 6.36 | 8.36d | 5.17 | F (2, 217) = 29.61*** | 0.21 |
| SIP-A | 40.08b | 7.67 | 32.27c | 6.56 | 28.71c | 0.46 | F (2, 202) = 42.24*** | 0.28 |
| AASE | 2.95b | 0.83 | 3.18c | 0.74 | 3.54c | 0.70 | F (2, 216) = 6.62** | 0.06 |
| SOCRATES | ||||||||
| Recognition | 3.65b | 0.62 | 4.17c | 0.56 | 3.92c | 0.60 | F (2, 216) = 10.38*** | 0.09 |
| Taking steps | 4.22b | 0.61 | 3.89c | 0.74 | 4.01bc | 0.72 | F (2, 216) = 5.54** | 0.05 |
| DSM-5 categorye | N/A | |||||||
| Mild (2–3) | 0.0% | 0.0% | 21.4% | |||||
| Moderate (4–5) | 0.0% | 17.9% | 46.4% | |||||
| Severe (6–11) | 100.0% | 82.1% | 28.6% | |||||
| Number of comorbid mental disorders | χ2 (4) = 20.03*** | |||||||
| 0 | 39.5% | 60.3% | 82.1% | |||||
| 1 | 21.0% | 14.1% | 10.7% | |||||
| 2 | 39.5% | 25.6% | 7.2% | |||||
| Number of treatment sessions attended | 7.39b | 4.61 | 7.53bc | 4.49 | 9.64c | 3.93 | F (2, 217) = 2.94 | 0.03 |
| Proportion of the participants that attended at least 6 of the 12 treatment sessions | 62.3% | 60.3% | 78.6% | χ2 (2) = 0.12 | ||||
| After treatment WHO drinking risk levelf | ||||||||
| Low | 75.7% | 64.9% | 89.3% | χ2 (2) = 6.70* | ||||
| Moderate/high/very high | 24.3% | 35.1% | 10.7% | |||||
Note. Daily drinkers were defined as those who drank ≥6 days per week averaged over 180 days upon baseline, as assessed by TLFB. N/A, not applicable. The chi-square statistics do not apply here, because when the expected frequency for a given cell is less than 1, the chi-square distribution will not be a reasonably accurate approximation of the distribution of the chi-square statistics (Cohen, 2001). Means with different superscripts were significantly different from each other.
eFor the whole sample, 2.7% individuals met the criteria for mild, 12.3% for moderate and 84.5% for severe.
fAdditional analyses indicated that even after accounting for before treatment baseline risk level (7 days before 1st treatment session), the MS class compared to the LS class was marginally correlated with being in the moderate/high/very high as opposed to the low category at the end of treatment.
* P < 0.05.
** P < 0.01.
*** P < 0.001.
Alcohol Use Disorders Identification Test-C
The Alcohol Use Disorders Identification Test-C (AUDIT-C; Bush et al., 1998) is a 6-item (α = 0.70) screening tool developed to identify persons who are hazardous drinkers or who are likely to have an active AUD. Each item has five response options that are weighted such that 0–4 points are possible per item. The AUDIT-C was administered during the phone screen as a check to ensure that individuals referred on to the baseline assessment were likely to meet DSM-5 criteria for an AUD. This measure has good sensitivity and specificity for identifying AUD among men and women (Bush et al., 1998).
Timeline Follow-Back
The Timeline Follow-Back (TLFB; Sobell and Sobell, 1992) is a calendar-based retrospective recall interview of daily alcohol use. Participants were administered the TFLB by trained, experienced interviewers at baseline for the past 180 days, weekly during treatment and at end of treatment. To examine end-of-treatment drinking, which captures the entire treatment phase of the study, the World Health Organization (WHO, 2000) risk levels of alcohol use (very high risk, high risk, moderate risk and low risk) were calculated based on the participant reports of the number of standard drinks (defined as 0.6 ounces of absolute alcohol) consumed, which were converted to grams of pure alcohol (0.6 ounces = 14 g). WHO risk levels were then calculated based on the average grams of alcohol consumed per day and dichotomized into two levels: low risk versus moderate/high/very high risk. This dichotomy is based on research demonstrating that low-risk drinking at the end of treatment assessment predicts better long-term outcomes (Witkiewitz et al., 2017).
Mini International Neuropsychiatric Interview
This diagnostic measure was adapted for this study and based on the DSM-5 diagnostic criteria. The parent study from which the current data are derived began recruitment during the transition from the DSM-IV to the DSM-5, and the new version of the Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) utilizing DSM-5 criteria was published 2 years after the initiation of this study. The substance use disorder modules were modified (i.e. the addition of the craving item) to reflect the revised DSM-5 diagnostic criteria and to match the wording in the forthcoming version of the MINI.
Alcohol Dependence Scale
The Alcohol Dependence Scale (ADS; Skinner and Allen, 1982) is a 25-item (α = 0.82) measure of the severity of alcohol dependence that assesses alcohol withdrawal symptoms, impaired control over drinking, awareness of a compulsion to drink, increased tolerance to alcohol and salience of alcohol-seeking behavior. The individual items have varying response options, ranging from 2 to 4 choices with higher scores indicating greater dependence.
Short Inventory of Problems-Alcohol
The Short Inventory of Problems-Alcohol (SIP-A; Miller et al., 1995) is a 15-item (α = 0.86) measure of the adverse consequences of alcohol use. Participants indicate how often each of the listed consequences has occurred in the past 3 months (‘never’, ‘once or a few times’, ‘once or twice a week’, ‘daily or almost daily’; scored 0–3).
Stages of Change and Treatment Readiness Scale
The Stages of Change and Treatment Readiness Scale (SOCRATES; Miller and Tonigan, 1996) is a 19-item measure designed to assess individuals’ awareness of problem drinking and motivation to change drinking behavior. Items are rated on a 1 (strongly disagree) to 5 (strongly agree) Likert scale and form three subscales: (a) ambivalence (α = 0.67), (b) recognition (α = 0.72) and (c) taking steps (α = 0.87).
Alcohol Abstinence Self-Efficacy Scale
The Alcohol Abstinence Self-Efficacy (AASE; DiClemente et al., 1994) Scale is a 20-item (α = 0.93) measure developed to assess the construct of self-efficacy as applied to alcohol abstinence. Participants rate their confidence to abstain in each situation on a 5-point Likert scale that ranges from 1 (not at all likely) to 5 (extremely likely).
Analytic strategy
First, LCA was used to identify potential AUD symptom classes using the 11 DSM-5 AUD diagnostic criteria (see Table 1). As a special case of finite mixture modeling, which models categorical latent variables that represent subpopulations where population membership is not known but is inferred from the data (McLachlan and Peel, 2000), LCA provides classification of individuals and explains the relationships among the observed dependent variables.
Table 1.
DSM-5 AUD diagnostic criteria items
| Item |
| 1. Alcohol is often taken in larger amounts or over a longer period than was intended (Larger/Longer) |
| 2. There is a persistent desire or unsuccessful efforts to cut down or control alcohol use (Quit/Control) |
| 3. A great deal of time is spent in activities necessary to obtain alcohol, use alcohol or recover from its effects (Time Spent) |
| 4. Craving, a strong desire or urge to use alcohol (Craving) |
| 5. Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school or home (Neglect Roles) |
| 6. Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol (Social/Interpersonal) |
| 7. Important social, occupational or recreational activities are given up or reduced because of alcohol use (Activities Given Up) |
| 8. Recurrent alcohol use in situations in which it is physically hazardous (Hazardous Use) |
| 9. Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problems that is likely to have been caused or exacerbated by alcohol (Physical/Psychological) |
| 10. Tolerance (Tolerance) |
| 11. Withdrawal (Withdrawal) |
Model fit was compared using Akaike information criterion (Akaike, 1973), Bayesian information criterion (Schwartz, 1978) and the Sample-Size Adjusted Bayesian Information Criterion (Sclove, 1987). Further, a significant P value on the Bootstrap Likelihood Ratio Test indicated that a k class solution fit better than a k − 1 class solution within a model (McLachlan and Peel, 2000). Starting with a 1-class model, classes were added iteratively until either the addition of a class did not improve or detracted from the model fit. The optimal model was further determined by classification quality (entropy and estimated posterior probabilities for each individual in each class), class sizes and the conceptual meaningfulness and interpretability of the classes identified. Entropy approaching 1.0 (e.g. Celeux and Soromenho, 1996) suggests adequate separation of the classes. LCA was conducted in Mplus 8.2 (Muthén and Muthén, 1998–2017).
There are two competing approaches to identifying latent classes/profiles using finite mixture modeling, each with its own strengths and limitations. One approach is to derive latent classes from an unconditional model without any auxiliary variables (covariates, distal outcomes or both) included in the model estimation. The alternative approach includes auxiliary variables during class formation, through either a one-step or a three-step process. The unconditional model is advantageous in terms of the logic of model building and the interpretation of latent classes (e.g. Clark and Muthén, 2009; Asparouhov and Muthén, 2014; Nylund-Gibson and Masyn, 2016). However, this unconditional model approach may introduce biased associations between the identified classes and auxiliary variables that are added. The current three-step approach (either the ML 3-step or the BCH) represents an attempt to address the above issue and at the same time to retain the latent classes estimated in the first step, although BCH1 seems to perform better for both adjusting classification error and resistance to latent class membership shifting (Nylund-Gibson et al., 2019).
In our case, the primary research aim was to develop a DSM-5-based AUD typology specifically using the 11 symptom criteria, from which clinical utility, such as improving diagnostic accuracy in service of selecting a targeted, personalized treatment, may be derived. In other words, we were concerned about the meaning or interpretation of the latent classes as measured by the 11 DSM-5 symptoms. Comparing the identified classes on potential baseline correlates, as well as treatment-related variables, was secondary and supplementary, as a means of further validating the classes.
Next, analyses for AUD class differences in demographics, alcohol-related constructs, individual difference characteristics and diagnostic and treatment variables were conducted using analysis of variance or chi-square tests, as appropriate.
RESULTS
AUD classes
Table 2 presents model fit statistics for each solution of the LCA model using logistic regression. Although the four-class model performed slightly better than the three-class model, two of the profiles that emerged out of the four-class solution were conceptually indistinguishable from each other; thus, the three-class solution was considered more theoretically interpretable and more parsimonious and was retained.
Table 2.
Fit statistics for AUD items based on LCA model
| No. of classes | LL | AIC | BIC | SSABIC | Entropy | BLRT (P) | Smallest n |
|---|---|---|---|---|---|---|---|
| 1 | −1290.02 | 2602.04 | 2639.37 | 2604.51 | − | − | |
| 2 | −1235.54 | 2517.07 | 2595.12 | 2522.24 | 0.63 | P < 0.001 | 72 |
| 3 | −1215.16 | 2500.31 | 2619.09 | 2508.17 | 0.70 | P = 0.010 | 28 |
| 4 | −1199.04 | 2492.07 | 2651.57 | 2502.69 | 0.78 | P = 0.030 | 13 |
| 5 | −1187.39 | 2492.77 | 2693.00 | 2506.03 | 0.80 | P = 0.390 | 15 |
Note. Highlighted in bold is the preferred class solution. LL, log-likelihood; AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; SSABIC, Sample-Size Adjusted Bayesian Information Criterion; BLRT, Bootstrap Likelihood Ratio Test.
As shown in Fig. 1, Class 1 (51.8% of participants) endorsed nearly all of the AUD diagnostic criteria items, with the exception of craving, at the highest rate among the three classes. Class 2 (35.5% of participants) reported a moderate to high rate of response on the majority of the items; rates on items hazardous use and social/interpersonal were the lowest among the three classes and rates on item craving were the highest. Excepting hazardous use and social/interpersonal, all other items were rated the lowest among Class 3 (12.7% of participants) compared with the other two classes, with items time spent, activities given up and withdrawal endorsed at a very low rate. Using maximum posterior probability, class membership for each participant was extracted from the estimated model for subsequent analyses.
Fig. 1.
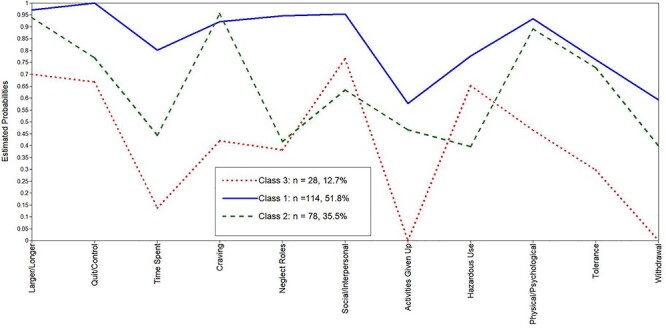
Profiles of AUD using conditional probabilities. Note. On the x-axis of the graph are the 11 AUD items and the conditional probability of endorsing each item is on the y-axis.
Characteristics of the AUD classes
Demographics
Characteristics of the three AUD classes are summarized in Table 3. There were a proportionally greater number of males than females in both Class 1 and Class 3, but not Class 2. The three classes did not differ on any other demographic variables.
Alcohol-related variables
Although all participants started drinking at roughly the same age (~18 years), drinking became problematic earlier for Class 1 as compared to the other two classes. In addition, Class 1 had higher scores on the AUDIT, ADS and the SIP-A relative to the other two classes. The AUD class profiles were not found to differ with regard to proportion of daily versus non-daily drinkers. Class 1 was further distinguished from the other two classes, exhibiting lower AASE and reduced awareness of problem drinking (SOCRATES-recognition subscale) and having taken more steps towards changing drinking behavior (SOCRATES-taking steps subscale).
Co-morbid mental disorders
Class 1 had a higher rate of comorbid mental health disorders than the other two classes, such that 21.0% of Class 1, 14.1% of Class 2 and 10.7% of Class 3 were diagnosed with one comorbid mental disorder and 39.5% of Class 1, 25.6% of Class 2 and 7.2% of Class 3 were diagnosed with two comorbid mental disorders, respectively.
Treatment outcome
At the end of treatment, a greater proportion of individuals were drinking at levels above the low risk category of WHO guidelines in both Class 1 (35.1%) and Class 2 (24.3%).
DISCUSSION
The purpose of the current study was to advance our understanding of the heterogeneity of AUD by identifying latent classes of adults aged 18–65 seeking treatment for AUD. By using LCA, we aimed to (a) identify subgroups of individuals with AUD characterized by unique DSM-5 symptom profiles and (b) examine the relationship between identified symptom profiles, baseline characteristics and treatment outcome measures. Overall, we identified three distinct classes of drinkers based on their endorsement of DSM-5 AUD symptom criteria; the classes differed on several measures of baseline functioning and treatment-related constructs.
The LCA, based on the 11 AUD symptom criteria, revealed three unique subgroups of drinkers with a current AUD diagnosis. Class 1 was the largest latent class (51.8%) of the three latent classes, reflecting a high level of participant endorsement of all 11 AUD symptoms. Characteristics of this class include a greater proportion of males, earlier onset of problem drinking and higher rate of comorbid mental health disorders. All individuals in this class met criteria for the DSM-5 classification of AUD-severe and had higher baseline scores on several measures of alcohol problem severity and lower AASE. Compared to Class 3, this latent class also had a greater proportion of individuals whose drinking exceeded the WHO low drinking risk level at the end of treatment. These findings indicate that this class may need specialized clinical attention to build patient motivation to change. Additional sessions may be required to consolidate treatment gains.
Class 2 was the second largest (35.5%). This group endorsed a moderate to high rate of response on the 11 AUD symptoms. Within this class, nearly all participants endorsed the craving item. Similar to Class 1, this group had a greater proportion of individuals who exceeded the WHO low drinking risk level at the end of treatment, as compared to Class 3.
Class 3 was the smallest of the three latent classes (12.7%). This group endorsed the lowest rates for all items except for hazardous use and social/interpersonal. Within this class, time spent, activities given up and withdrawal were the least often endorsed items. Compared to the other two classes, Class 3 had the lowest rates of individuals diagnosed with one or two co-morbid mental health disorders.
These findings advance the literature on the typology of AUD. Although prior work has uncovered subgroups of individuals with AUD based on DSM-5 criteria (Rinker and Neighbors, 2015; Swift et al., 2016), to our knowledge this study is one of the only studies that have differentiated individuals seeking treatment for AUD. Indeed, the AUD symptom patterns identified for both Classes 1 and 3 in the current study are similar to those found by Mejldal et al. (2020) who also examined variation of the AUD among a clinical sample aged 60 and older. However, in their moderate symptomatic class, the most frequently endorsed item is hazardous use, instead of craving displayed in our sample. Taken together, these studies suggest that the items in the DSM-5 can be used to identify clinically meaningful subgroups of people with AUD.
The classes identified in the current study vary by baseline measures of AUD problem severity, comorbid mental disorders and outcome. Given recent advances in the development of personalized approaches to treatment using AARDoC and ANA domains (e.g. Litten et al., 2015), two classification systems based on different phases of the addiction cycle (i.e. binge–intoxication, withdrawal–negative affect and preoccupation–anticipation), the current findings support the development of individually tailored interventions based on patterns of DSM-5 symptom endorsement. For instance, given that craving was the most salient symptom in Class 2, individuals in this class might benefit from strategies for craving management. For Class 1, treatment may need to address a much broader set of skills, including managing craving, drink refusal and problem solving. Additional time for intervention may also be warranted for this class.
The current findings also have implications for when to address certain clinical phenomena during treatment. For example, Class 2 endorsed drinking more or longer than intended, experiencing craving or a strong urge to drink and continuing to drink even though it contributed to (worsened) another mental or physical health problem at a much higher rate relative to other DSM-5 symptoms. This behavior pattern suggests that there might be value in addressing urges and cravings earlier in treatment before discussing and implementing strategies for adhering to safe drinking guidelines.
Regarding treatment outcome, Classes 1 and 2 had a higher proportion of individuals drinking in excess of the WHO low risk drinking category at the end of treatment. This may reflect a general assumption that certain patterns of symptoms are harder to treat. However, Mejldal et al. (2020) did not find such a class difference in drinking outcomes assessed as either drinking days or drinks per drinking days. They argue that alcohol consumption may not be a clear indication of AUD severity. Indeed, recent discussions in the alcohol treatment literature recommend ‘moving beyond abstinence to cast a broader net’ (Witkiewitz, 2013, p. E9).
As described above, compared to other typologies such as the AARDoC and ANA, a typology based on DSM-5 criteria has a greater likelihood of dissemination, given that the DSM-5 is available to all practitioners and a typology based on AUD criteria would be relatively straightforward to compute. A typology based on DSM-5 criteria has the additional advantage of using criteria that are familiar to many clinicians and does not require specialized knowledge or equipment as the ANA requires (e.g. fMRI). Such convenience would permit broad and rapid dissemination of treatment recommendations based on latent classes of AUD and allow for the delivery of tailored treatments that target specific symptom patterns, potentially leading to enhanced treatment outcomes while conserving scarce clinical resources.
Despite the study strengths, there are several limitations that point to future research directions. First, estimated posterior probabilities indicated that Classes 1 and 2 were not very well distinguished from each other, with the given set of the 11 DSM-5 AUD items. Second, given that LCA is largely an empirically based or data-driven approach, the use of larger independent samples or simulation analyses should be considered to cross-validate the current AUD profiles identified. A quick and easy algorithm for assigning individuals to classes according to their DSM-5 scores should also be developed. An additional downside to this empirically based approach is the possibility of reifying the identified classes (Nagin and Tremblay, 2005; Raudenbush, 2005). To avoid this pitfall, in addition to complementing diagnosis, we recommend using the AUD profiles to predict broader treatment outcomes such as psychosocial functioning. Third, longitudinal research is needed to determine the treatment trajectory of the three AUD classes. For example, although Class 1 reports greater levels of alcohol problem severity at baseline, it remains unknown whether and which individuals in this class transition out of an AUD diagnosis during treatment. To discern this, alternative analytic strategies such as latent transition analysis (LTA; e.g. Reboussin et al., 1998) may be pursued. Finally, the generalization of the current findings to other cultural/ethnic groups may be limited, given that the current sample was predominately White/Caucasian. Potential cultural/ethnic variation in manifestations of AUD symptoms warrants future investigation.
In conclusion, this study advances the field by revealing three distinct subgroups of treatment-seeking individuals with AUD with these groups differing on baseline levels of alcohol problem severity and treatment outcome. Future research in this area should attempt to replicate these classes with larger samples and with other cultural/ethnic groups. The current findings have important implications for AUD precision medicine that considers specific symptom patterns with potential utility to guide the content and timing of alcohol treatment content.
FUNDING
This research was supported by RO1 AA022080 and T32 AA007583 from the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health. The funding source had no role in the study design, collection, analyses and interpretation of the data; writing of the manuscript or the decision to submit the manuscript for publication.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
None declared.
Footnotes
Additional BCH was conducted and the results largely replicated the findings using the unconditional model approach.
Contributor Information
Junru Zhao, School of Social Work, University at Buffalo—The State University of New York, 1021 Main Street, Buffalo, NY 14203, USA.
Braden Linn, Clinical and Research Institute on Addictions, University at Buffalo—The State University of New York, 1021 Main Street, Buffalo, NY 14203, USA.
Clara Bradizza, School of Social Work, University at Buffalo—The State University of New York, 1021 Main Street, Buffalo, NY 14203, USA.
Joseph Lucke, Department of Psychiatry, University at Buffalo—The State University of New York, 1021 Main Street, Buffalo, NY 14203, USA.
Melanie Ruszczyk, School of Social Work, University at Buffalo—The State University of New York, 1021 Main Street, Buffalo, NY 14203, USA.
Paul Stasiewicz, School of Social Work, University at Buffalo—The State University of New York, 1021 Main Street, Buffalo, NY 14203, USA.
References
- Akaike H (1973) Information theory and an extension of the maximum likelihood principle. In Petrov BN and Csaki F (eds), 2nd International Symposium on Information Theory, pp. 267–81. Budapest, Hungary: Akademiai Kiad. [Google Scholar]
- APA (2013) Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Arlington: American Psychiatric Association. [Google Scholar]
- APA (2000) Diagnostic and Statistical Manual of Mental Disorders (DSM-4®). Washington, DC: American Psychiatric Association. [Google Scholar]
- Asparouhov T, Muthén B (2014) Auxiliary variables in mixture modeling: three-step approaches using M plus. Struct Equ Model 21:329–41. doi: 10.1080/10705511.2014.915181. [DOI] [Google Scholar]
- Babor TF, Caetano R (2006) Subtypes of substance dependence and abuse: Implications for diagnostic classification and empirical research. Addiction 101:104–10. [DOI] [PubMed] [Google Scholar]
- Beseler CL, Taylor LA, Kraemer DT et al. (2012) A latent class analysis of DSM-IV alcohol use disorder criteria and binge drinking in undergraduates. Alcohol Clin Exp Res 36:153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, Mcdonell MB et al. (1998) The AUDIT alcohol consumption questions (AUDIT-C) - an effective brief screening test for problem drinking. Arch Intern Med 158:1789–95. [DOI] [PubMed] [Google Scholar]
- Casey M, Adamson G, Stringer M (2013) Empirical derived AUD sub types in the US general population: A latent class analysis. Addict Behav 38:2782–6. [DOI] [PubMed] [Google Scholar]
- Castaldelli-Maia JM, Silveira CM, Siu ER et al. (2014) DSM-5 latent classes of alcohol users in a population-based sample: results from the São Paulo Megacity Mental Health Survey, Brazil. Drug Alcohol Depend 136:92–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G, Soromenho G (1996) An entropy criterion for assessing the number of clusters in a mixture model. J Classif 13:195–212. [Google Scholar]
- Cicchetti D, Jester JM, Buu A et al. (2016) Longitudinal phenotypes for alcoholism: heterogeneity of course, early identifiers, and life course correlates. Dev Psychopathol 28:1531–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark S, Muthén B (2009). Relating latent class analysis results to variables not included in the analysis. https://www.statmodel.com/download/relatinglca.pdf (30 October 2020, date last accessed)
- Cohen B (2001) Explaining Psychological Science, 2nd edn. New York: John Wiley & Sons. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS et al. (2006) Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction 101:824–34. [DOI] [PubMed] [Google Scholar]
- Diclemente CC, Carbonari JP, Montgomery RP et al. (1994) The Alcohol Abstinence Self-Efficacy scale. J Stud Alcohol 55:141–8. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD et al. (2017) Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 74:911–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallford HG, Tivis RD, Nixon SJ (2003) An empirical assessment of post-treatment alcohol consumption. Psychiatry Res 121:197–205. [DOI] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M et al. (2013) DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry 17:834–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwako LE, Momenan R, Litten RZ et al. (2016) Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry 80:179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S, Rhoades B (2013) Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci 14:157–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litten RZ, Ryan ML, Falk DE et al. (2015) Heterogeneity of alcohol use disorder: understanding mechanisms to advance personalized treatment. Alcohol Clin Exp Res 39:579–84. [DOI] [PubMed] [Google Scholar]
- McLachlan G, Peel D (2000) Finite Mixture Models. New York: John Wiley. [Google Scholar]
- Mejldal A, Andersen K, Bilberg R et al. (2020) DSM-5 latent classes of alcohol users among treatment seeking older adults. Subst Use Misuse 55:1214–22. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan S (1996) Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychol Addict Behav 10:81–9. [Google Scholar]
- Miller WR, Tonigan S, Longabaugh R (1995) The Drinker Inventory of Consequences (DrinC): An instrument for assessing adverse consequences of alcohol abuse. NIAAA Project MATCH monograph series. Washington, DC: Government Printing Office. [Google Scholar]
- Moos RH, Moos BS (2006) Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction 101:212–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE (2002) Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction 97:279–92. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (1998–2017) Mplus User’s Guide (8th ed.). Los Angeles: Muthen and Muthen. [Google Scholar]
- Nagin DS, Tremblay RE (2005) Developmental trajectory groups: Fact or a useful statistical tradition? Criminology 43:873–904. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (2016). Alcohol use disorder: A comparison between DSM–IV and DSM–5. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-use-disorder-comparison-between-dsm
- Nylund-Gibson K, Grimm R, Masyn K (2019) Prediction from latent classes: a demonstration of different approaches to include distal outcomes in mixture models. Struct Equ Model 26:1–19. doi: 10.1080/10705511.2019.1590146. [DOI] [Google Scholar]
- Nylund-Gibson K, Masyn KE (2016) Covariates and mixture modeling: results of a simulation study exploring the impact of misspecified effects on class enumeration. Struct Equ Model 23:782–97. doi: 10.1080/10705511.2016.1221313. [DOI] [Google Scholar]
- Palmer RS, Murphy MK, Piselli A et al. (2009) Substance user treatment dropout from client and clinician perspectives: a pilot study. Subst Use Misuse 44:1021–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush, SW (2005). How do we study “what happens next”? Ann Am Acad Pol Soc Sci 602(1), 131–144. [Google Scholar]
- Reboussin BA, Reboussin DM, Liang KY et al. (1998) Latent transition modeling of progression of health-risk behavior. Multivar Behav Res 33:457–78. [DOI] [PubMed] [Google Scholar]
- Rinker DV, Neighbors C (2015) Latent class analysis of DSM-5 alcohol use disorder criteria among heavy-drinking college students. J Subst Abus Treat 57:81–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz G (1978) Estimating the dimensions of a model. Ann Stat 6:461–4. [Google Scholar]
- Sclove LS (1987) Application of model-selection criteria to some problems in multivariate analysis. Psychometrika 52:333–43. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH et al. (1998) The Mini International Neuropsychiatric Interview (MINI): The development and validationof a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59 Suppl 20:22–33. [PubMed] [Google Scholar]
- Sher KJ (2015) Moving the alcohol addiction RDoC forward. Alcohol Clin Exp Res 39:591–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA, Allen BA (1982) Alcohol dependence syndrome: measurement and validation. J Abnorm Psychol 91:199–209. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline Follow-back: a technique for assessing self-reported ethanol consumption. In Allen J, Litten RZ (eds). Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa: Humana Press, 41–72. [Google Scholar]
- Stasiewicz PR, Bradizza CM, Ruszczyk MU et al. (2019) The relationship of pretreatment trajectories of alcohol use to treatment outcome in men and women with alcohol use disorder. Alcohol Clin Exp Res 43:2637–2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift W, Slade T, Carragher N et al. (2016) Adolescent predictors of a typology of DSM-5 alcohol use disorder symptoms in young adults derived by latent class analysis using data from an Australian cohort study. J Stud Alcohol Drug 77:757–65. [DOI] [PubMed] [Google Scholar]
- Votaw V, Pearson M, Stein E et al. (2020) The addictions neuroclinical assessment negative emotionality domain among treatment-seekers with alcohol use disorder: construct validity and measurement invariance. Alcohol Clin Exp Res 44:679–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K (2008) Lapses following alcohol treatment: modeling the falls from the wagon. J Stud Alcohol Drug 69:594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K (2013). “Success” following alcohol treatment: moving beyond abstinence. Alcohol Clin Exp Res 37(S1): E9–13. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA (2007) Modeling the complexity of post-treatment drinking: it's a rocky road to relapse. Clin Psychol Rev 27:724–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Roos CR, Pearson MR et al. (2017) How much is too much? Patterns of drinking during alcohol treatment and associations with post-treatment outcomes across three alcohol clinical trials. J Stud Alcohol Drug 78:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Roos CR, Tofighi D et al. (2018) Broad coping repertoire mediates the effect of the combined behavioral intervention on alcohol outcomes in the COMBINE study: an application of latent class mediation. J Stud Alcohol Drug 79:199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2000) International Guide for Monitoring Alcohol Consumption and Related Harm. Geneva: World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


