Abstract
Objectives
While a number of studies have documented a notable decline in age-standardized prevalence in dementia in the U.S. population, relatively little is known about how dementia has declined for specific age and race groups, and the importance of changing educational attainment on the downward trend. We assess (a) how the trends in dementia prevalence may have differed across age and race groups and (b) the role of changing educational attainment in understanding these trends.
Methods
This article estimates a series of logistic regression models using data from the Health and Retirement Study (2000–2014) to assess the relative annual decline in dementia prevalence and the importance of improving educational attainment for non-Hispanic Whites and non-Hispanic Blacks.
Results
Consistent with other studies, we found significant declines in dementia for non-Hispanic Blacks and non-Hispanic Whites across this period. Nonetheless, these declines were not uniform across age and race groups. Non-Hispanic Blacks aged 65–74 years had the steepest decline in this period. We also found that improved educational attainment in the population was fundamentally important in understanding declining dementia prevalence in the United States.
Discussion
This study shows the importance of improvement in educational attainment in the early part of the twentieth century to understand the downward trend in dementia prevalence in the United States from 2000 to 2014.
Keywords: Cognitive health, Educational attainment, Health and Retirement Study
Background
A number of studies have reported a decline in the prevalence of dementia in the U.S. population since 2000. Langa et al. (2017) reported, for example, that the age- and sex-standardized prevalence of dementia in the U.S. older population in 2012 was 8.6%, down from 11.6% in 2000. Chen and Zissimopoulos (2018) also reported declines in prevalence for non-Hispanic Blacks and Whites aged 65 years and older during the same period. Although the prevalence estimates differ somewhat in these studies due to methodological approaches, they nonetheless report significant reductions in dementia prevalence for older Black and White Americans in the early part of this century.
While a decline in dementia prevalence in the U.S. older population has been documented across a number of studies, researchers have offered alternative explanations for the decline. One explanation for the declining trend is improvements in educational attainment among older adults during the time period. Although empirical evidence of the role of improved levels of educational attainment for the recent trend is largely lacking, this argument is based on results from individual-level studies showing the large negative association between educational attainment and dementia prevalence and population-level studies documenting the increases in the educational attainment of the older population over the past few decades. The findings in a recent study by Crimmins et al. (2018) offer insight into this issue. Crimmins et al. showed that approximately half of the decline in life expectancy with dementia for the total U.S. population 2000–2010 was due to improved education.
To better evaluate the role of improved educational attainment on dementia trends, we also control for other factors that may play a role in the downward trend in dementia. For example, research has documented that the older population in recent decades has experienced improvements in childhood epidemiological environments, declines in smoking rates, and improved control of hypertension—all factors associated with a lower risk of dementia (Baumgart et al., 2015; Donley et al., 2018; Peters et al., 2008). Controlling for these types of factors allows us to evaluate the role of change in educational attainment in light of changes pertaining to other modifiable risk factors.
Because previous studies have largely assessed dementia trends for the older population as a whole (e.g., older than age 65 or 70), it is unclear whether important sociodemographic groups diverged or perhaps contributed in different ways to the overall national trend. Is the downward trend in dementia prevalence evident across the age range? Do Blacks and Whites both experience downward trends in dementia prevalence? We attempt to give some insight into potential differences in the dementia trend by examining the trend within two age groups, persons 65–75 and 75 and older, and for older non-Hispanic Blacks and Whites for 2000–2014. The analysis clarifies whether the magnitude of the trend varies across the race–age groups and provides estimates of the average annual magnitude of change. We note that with the exception of Chen and Zissimopoulos (2018), little research of which we are aware has examined long-term dementia trends for the Black population, which appears to be especially vulnerable. This approach also allows us to assess whether changes in educational attainment, as well as other changes in modifiable risk factors for dementia (such as changes in poor childhood circumstances, health behaviors, and health conditions), have widespread consequences across major race–age groups (Langa et al., 2017; Rocca et al., 2011).
Education, Cognition, and Dementia
The hypothesis that educational attainment has significantly contributed to the downward trend in dementia in the United States is based on the seismic improvement in educational attainment in the first half of the twentieth century and the importance of education for cognitive development. High school graduation rates among persons aged 17 years, for example, climbed from about 10% in 1910, to 18% in 1920, to 30% in 1930, and slightly more than 50% in 1940 (Goldin, 1998). At the same time that high school graduation rates were increasing, the average number of days per year students attended school also rose dramatically (National Center for Education Statistics, 1993). Part of the upward shift in graduation rates and attendance was driven by institutional changes in instruction and the demand for skilled workers in manufacturing. The model for high school education, for example, shifted from an emphasis on classical learning in 1900 (e.g., Greek and Latin instruction) to the basic model of high school that we know today (e.g., instruction in English and mathematics). At the population level, more Americans spent more of their lives in school. Exposure to schooling increased dramatically among the older population considered in this study. Students were being prepared for a dynamic labor market.
The growth in educational exposure implies growth at the population level in the stock of cognitive abilities attained by early adulthood (Lövdén et al., 2020; Mather, 2020). Potentially, this growth in the stock of educational attainment could be related to the downward trend in dementia prevalence through two major mechanisms. One mechanism is that the association between cognitive function in old age and educational attainment could reflect this early life association carried forward across the adult life course. A second mechanism is that persons with different levels of education could have differential rates of cognitive decline in adulthood.
Lövdén et al. (2020) recently provided a valuable review of the current state of the evidence that is informative for our study of dementia trends. First, they note that there is consistent evidence that the association between educational attainment and cognitive function is stable and robust throughout adulthood. There is less consistent evidence, however, for the idea that education’s association with dementia risk reflects differential rates of cognitive decline where higher levels of education are presumed to be protective. At least based on the evidence thus far, then, greater stocks of educational attainment and improvements in cognitive function in the population over time should be associated with a downward trend in dementia.
In many ways, it should not be surprising to expect that educational attainment is linked to dementia risk through the establishment of cognitive abilities. During schooling, individuals acquire new knowledge, they learn how to keep knowledge in mind, and they learn how to respond to changing and new tasks in a dynamic environment. Schools immerse students in a cognitively challenging environment. Education also usually occurs during a period of the life course when, biologically speaking, cognitive development occurs at a rapid pace. Some evidence also supports the idea that the ages of peak cognitive performance occur later in the life course with more years of educational attainment (Guerra-Carrillo et al., 2017). In addition, a recent meta-analysis (Xu et al., 2016) reported a dose–response relationship between educational attainment and dementia risk for both low and high categories of educational attainment. In essence, there is robust evidence that more years of education lengthen and deepen cognitive development and function which is associated with a lower risk of dementia.
Race Differences in Education
Although race-specific estimates of educational attainment trends in the United States are difficult to come by, there are several indicators pointing to significant improvements in the schooling of Blacks and Whites in the early part of the twentieth century. For example, in 1900, about 53% of 5- to 19-year-old Whites were enrolled in school compared to 30% of Blacks; by 1940, enrollment had increased more for Blacks than for Whites and the gap had narrowed to about 70% for Whites and 63% for Blacks (National Center for Education Statistics, 1993; Figure 1).
Figure 1.
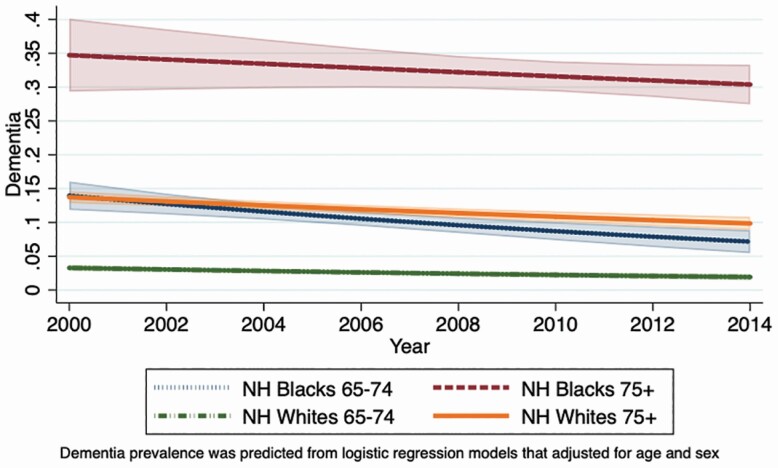
Predicted prevalence of dementia from 2000 to 2014 for non-Hispanic (NH) Whites and Blacks aged 65–74 and 75 and older (HRS). HRS = Health and Retirement Study.
Another dimension of Blacks’ and Whites’ schooling experience trend is the quantity of exposure during the school year (Glymour & Manly, 2008). Approximately 80% of Blacks aged 65 years and older alive today were born in the Jim Crow South regardless of their region of current residence (Glymour & Manly, 2008; Hayward et al., 2000). Many older Black Americans, then, experienced “sharecropper childhoods” and segregated schools. While Southern Black school districts were underresourced (Carruthers & Wanamaker, 2017), their school year was also shorter on average than White school districts in the early part of the twentieth century (Glymour & Manly, 2008). Similar to the change in the racial gap in school enrollment, the quantity of schooling during the school year for Blacks rose also more sharply than Whites, converging (although not reaching) the levels experienced by Whites by 1950.
Although schooling substantially rose for both Blacks and Whites throughout the early part of the twentieth century, it is less clear how these race differences may have influenced the trends in dementia risk for Blacks and Whites. The ambiguity rests to some degree on whether educational attainment’s association with cognitive function and dementia risk is robust for both race groups, given the racialized schooling and adult life course experiences of older Black and White Americans. Somewhat surprisingly, the available evidence points to a robust association for both race groups despite different average levels of achievement and differences in a social context (Barnes et al., 2011; Farina et al., 2019; Weuve et al., 2018). Recent evidence from a population-based study of persons living in a region that had experienced Apartheid—a context similar to the Jim Crow South—also shows a robust and linear association of educational attainment and cognitive function (Kobayashi et al., 2017). Black and White older adults seem to benefit similarly from additional educational experience despite significant contextual differences. This association suggests that the historical trends in greater exposure to schooling will be important in accounting for the downward trend in dementia prevalence for both race groups.
Data, Measures, and Approach
Our study of U.S. dementia prevalence trends, 2000–2014, is based on the nationally representative Health and Retirement Study (HRS). These data have played an important role in prior studies documenting the national trends in cognitive health (Chen & Zissimopoulos, 2018; Langa et al., 2017). The HRS is a panel survey of the U.S. population older than the age 50. The HRS interviews respondents approximately every 2 years and uses a steady-state design to replenish the sample every 6 years with younger cohorts. This design feature makes it possible to employ the HRS to assess dementia prevalence in a national sample of Americans every 2 years from 2000 to 2014, based on respondents’ cognitive status at that time. Cross-sectional weights allow us to obtain nationally representative estimates of dementia prevalence for each survey wave.
Although the survey began in 1992, we include only the sample waves from 2000 to 2014 because consistent cognitive information for both community-dwelling and nursing home residents aged 65 years and older first became available in 2000; the final releases for these data in 2016 and 2018 (with the final weights) were not available at the time of initial journal submission. For each wave of data, respondents aged 65 and older are included. The analytic sample is composed of pooled observations from 2000 and including 2014, and each wave is treated as a cross-section (see Supplementary Table 2).
Measures
Cognitive status is based on either respondent or proxy assessments. For self-respondents, a battery of tests was used to assess cognitive function (i.e., immediate recall of 10 words, delayed recall of the same 10 words, five trials of serial 7s, and backward counting). For respondents who could not complete the cognitive assessment, cognitive function was based on proxy assessments of memory, assessments of five instrumental activities of daily living, and the interviewer’s assessment of difficulty in completing the survey. Based on score criteria identified by Crimmins et al. (2011), the scores for the self-respondents and proxy respondents can be divided into three cognitive status categories: normal, cognitive impairment without dementia, or dementia. The cognitive status categories have been validated using clinical diagnoses and survey scores in the HRS Aging, Demographics, and Memory Study (Crimmins et al., 2011).
The number of years since 2000 is used to measure the time trend. The range is 0–14, providing an annual account for each year from 2000 to 2014.
To assess the role of changing educational attainment in the older adult population, we use a continuous measurement of education based on the number of schooling years which is self-reported by each respondent. This measurement ranges from 0 to 17 years or more.
To test for alternative explanations related to possible declines in dementia, we also evaluate other common risk factors. For early life exposures, we use two variables—childhood health problems (a dichotomous variable identifying whether the respondent reported their health as a child was poor/fair) and childhood adversity (a 0–4 scale identifying summing dichotomous responses to whether father’s occupation at age 16 was blue collar, mother’s and father’s education was less than 8 years, and whether they perceived themselves as poor during childhood). For later-life adult health conditions, we include hypertension (not diagnosed, diagnosed but not treated, and diagnosed and treated), stroke, diabetes, and heart problems based on whether a doctor ever told the respondents that they have the condition. Lastly, we also include covariates for self-reported smoking experience, alcohol use, and body mass index (BMI) to control for other factors that might also contribute to the trend in dementia prevalence. All of the covariates have been identified as dementia risk factors in a large number of studies. Comparing these results to models with education allows us to determine whether these changes among older adults during this period may also be a driving factor in declining dementia.
Analysis
The analysis of the dementia prevalence trends is based on logistic regression models predicting the log odds of having dementia (1/0) as a function of a time-trend variable (a continuous measure of years since 2000) and our set of covariates. The continuous measure also allows for a straightforward assessment of the effects of compositional change and comparison of trends across groups. The effect of the trend measure was expressed as an odds ratio (OR) in the results shown below which allows us to identify the average annual change in dementia prevalence. For example, the OR of 0.976 would translate into a relative decline of about 2.4% in dementia prevalence per year over the 14-year period.
Models were estimated separately for U.S.-born non-Hispanic Blacks and Whites for two age groups, 65–74 and 75 and older. We controlled for the respondent’s age within each age group to adjust for possible aging within the broader age groups across the observation waves. All results were also adjusted for sex composition. As an ancillary analysis, we also fit gender-stratified models (Supplementary Table S1). Although there is evidence of a modest gender difference for Whites aged 75 and older, education nonetheless plays an important role in explaining the declining trend for both genders. Because our focus is on evaluating the trends for Blacks and Whites across the two major age groups, we do not report these results in the main body of the text. We have not extended the analysis to Hispanics because of the group’s heterogeneity (e.g., nativity, country of origin) in the HRS. Those Hispanic respondents who are immigrants also have drastically lower levels of schooling than all other groups, and the education occurred largely outside the United States.
To assess how dementia trends reflected changes in population characteristics, we estimated two sets of logistic regression models that controlled for the covariates and assessed changes in the OR estimate of the trend. The first set of models assessed how controlling for each covariate separately altered the trend (e.g., educational attainment, smoking, controlled hypertension). To the extent that the covariates statistically account for the trend, the odds ratio is expected to approach 1.0, indicating no trend over the 14-year period. This gives us an overall assessment of the sensitivity of the trend to changes in education and each alternative explanation over the observation period (e.g., changes in education compared to controlled hypertension).
We then estimated the second set of models that were nested. These models sequentially added covariates to the models in order to assess how controlling for changes in population characteristics in the combined set of risk factors statistically alters the trend from 2000 to 2014. Our models are as follows: trend (M1), M1 plus education (M2), M2 plus the measures of childhood conditions (M3), M3 plus the health behavior measures (M4), and M4 plus the addition of the cardiometabolic conditions (M5). We are specifically interested in whether covariates such as early-life factors and the health conditions alter the trend net of the impact of educational attainment.
In addition to these models, we also performed a sensitivity analysis to verify that the observed downward trend for dementia prevalence from 2000 to 2014 had occurred throughout the entire period and was not driven by specific years or set of years within that time period. To this end, we compared the continuous time trend (shown in the manuscript) to a model with dummy variables for each year (minus 1) that allows for the changes between waves to vary. Using model fit criteria, we conclude that model fit does not significantly differ between the presented model and alternative specifications. The models both show a downward linear trend across the entire 14-year period for all groups. Thus, the analysis is based on the continuous trend measure to provide an overall summary of the trend for the observation period.
Results
Table 1 presents basic descriptive information of respondents included in the analysis for the two observation waves, 2000 and 2014, that bracket the trend period in order to provide an overall benchmark of how these characteristics changed. Similar to other studies assessing dementia trends using the HRS, the proportion of the sample with dementia was significantly lower for both age–race groups in 2014 compared to 2000. For example, the proportion of non-Hispanic Blacks aged 75 years and older with dementia dropped from 38.4% in 2000 to 30.0% in 2014. As one might expect, the dementia rates were substantially higher for the older age group and for non-Hispanic Blacks compared to non-Hispanic Whites. Note that the reported proportions are unadjusted for age (within the age categories) and sex.
Table 1.
Descriptive Information on Education, Childhood Conditions, Health Behaviors, and Cardiometabolic Conditions in 2000 and 2014, by Age and Race Group (HRS)
| Age 65–74 | Age 75 and older | |||
|---|---|---|---|---|
| 2000 | 2014 | 2000 | 2014 | |
| Total Ns | ||||
| Non-Hispanic Blacks | 702 | 741 | 562 | 705 |
| Non-Hispanic Whites | 4,229 | 3,179 | 3,951 | 4,128 |
| Proportion with Dementia | ||||
| Non-Hispanic Blacks | 16.1% | 7.8%* | 38.4% | 30.0%* |
| Non-Hispanic Whites | 3.6% | 1.9%* | 16.0% | 12.7%* |
| Education | ||||
| Non-Hispanic Blacks | 10.25 | 12.35* | 8.8 | 11.12* |
| Non-Hispanic Whites | 12.56 | 13.73* | 11.88 | 12.95* |
| Poor Childhood Health | ||||
| Non-Hispanic Blacks | 9.6% | 4.8%* | 5.2% | 7.6% |
| Non-Hispanic Whites | 5.8% | 4.5% | 6.1% | 5.2% |
| Poor Childhood SES | ||||
| Non-Hispanic Blacks | 47.0% | 42.0% | 46.3% | 46.8% |
| Non-Hispanic Whites | 31.9% | 22.6%* | 32.4% | 30.8% |
| Smoking Behavior | ||||
| Non-Hispanic Blacks | ||||
| Never Smoked | 38.5% | 37.8% | 49.4% | 46.1% |
| Former Smoker | 45.5% | 44.2% | 42.9% | 49.2% |
| Current Smoker | 15.9% | 18.0% | 7.7% | 4.7% |
| Non-Hispanic Whites | ||||
| Never Smoked | 38.4% | 41.4%* | 48.0% | 46.1%* |
| Former Smoker | 48.2% | 47.6%* | 46.6% | 49.5%* |
| Current Smoker | 13.5% | 10.9%* | 5.4% | 4.4%* |
| Over 35 BMI | ||||
| Non-Hispanic Blacks | 13.9% | 19.7%* | 6.1% | 10.7%* |
| Non-Hispanic Whites | 5.9% | 13.4%* | 2.7% | 5.8%* |
| Diabetes | ||||
| Non-Hispanic Blacks | 23.7% | 38.0%* | 21.8% | 39.8%* |
| Non-Hispanic Whites | 14.6% | 24.2%* | 13.8% | 24.1%* |
| Heart Condition | ||||
| Non-Hispanic Blacks | 25.4% | 25.6% | 30.8% | 37.5%* |
| Non-Hispanic Whites | 23.5% | 28.4%* | 36.8% | 42.3%* |
| Stroke | ||||
| Non-Hispanic Blacks | 10.6% | 13.6%* | 16.9% | 17.0% |
| Non-Hispanic Whites | 7.6% | 8.0% | 15.6% | 15.7% |
| Hypertension | ||||
| Non-Hispanic Blacks | ||||
| Not Reported | 35.0% | 19.1%* | 30.3% | 13.6%* |
| Reported, Untreated | 3.0% | 5.5%* | 7.2% | 5.7%* |
| Reported, Treated | 62.0% | 75.4%* | 62.5% | 80.7%* |
| Non-Hispanic Whites | ||||
| Not Reported | 53.2% | 38.0%* | 47.1% | 30.0%* |
| Reported, Untreated | 4.5% | 7.3%* | 5.4% | 6.3%* |
| Reported, Treated | 42.3% | 54.8%* | 47.5% | 63.6%* |
Note: BMI = body mass index; HRS = Health and Retirement Study; SES = socioeconomic status.
*p < .05.
A couple of the risk factors included in this analysis differed significantly between 2000 and 2014 for both race groups. Educational attainment was significantly higher in 2014 compared to 2000, especially for non-Hispanic Blacks, pointing to its potential importance in accounting for the downward trend in prevalence. Treated hypertension, another possible explanation for the trend, also was higher in 2014 compared to 2000 for all age–race groups. However, there were other differences in the risk factors that point to possible countervailing influences on the trend, including the rise in obesity, diabetes, and heart problems.
Table 2 provides information about the magnitude and direction of the 2000–2014 trends for the age–race groups. The largest relative change is the decline in dementia for Blacks aged 65–74—a relative decline in dementia prevalence of 5.2% per year (OR = 0.948, M1). Whites in this age group also experienced a relatively large decline of 3.8% per year (OR = 0.962). The rate of decline for persons 75 years of age and older was less than that observed for the younger ages, and the trend for Blacks—though downward—was not statistically significant. It should be noted that the magnitude of decline for Whites 75 and older varied somewhat by gender: women had a steeper decline in dementia prevalence than men (Supplementary Table S1). Comparison of the trends for the 65–74 and 75 and older age groups suggests that the bulk of the trend in dementia status for persons older than age 65 reflects greater relative improvements at younger ages.
Table 2.
Odds Ratios (SE) of Dementia Prevalence Trend From 2000 to 2014 Derived From Logistic Regression, Adjusted for Changes in Population Characteristics for Older Adults, by Age–Race Group (HRS)
| Whites 65–74 | Whites 75 and older | Blacks 65–74 | Blacks 75 and older | |
|---|---|---|---|---|
| M1: Trend | 0.962*** (0.009) | 0.973*** (0.005) | 0.948*** (0.005) | 0.986 (0.011) |
| M2: Trend + Education | 0.986 (0.011) | 0.990* (0.004) | 0.993 (0.014) | 1.023* (0.009) |
| M3: Trend + Child conditions | 0.975* (0.010) | 0.981*** (0.005) | 0.955*** (0.012) | 0.993 (0.012) |
| M4: Trend + Smoking | 0.962*** (0.010) | 0.974*** (0.005) | 0.949*** (0.012) | 0.986 (0.011) |
| M5: Trend + BMI | 0.962*** (0.010) | 0.973*** (0.005) | 0.948*** (0.012) | 0.986 (0.011) |
| M6: Trend + Diabetes | 0.956*** (0.010) | 0.971*** (0.005) | 0.938*** (0.013) | 0.984 (0.011) |
| M7: Trend + Heart condition | 0.960*** (0.009) | 0.973*** (0.005) | 0.938*** (0.013) | 0.985 (0.011) |
| M8: Trend + Stroke | 0.957*** (0.010) | 0.973*** (0.005) | 0.938*** (0.013) | 0.985 (0.011) |
| M9: Trend + Hypertension | 0.955*** (0.009) | 0.972*** (0.005) | 0.943*** (0.012) | 0.985 (0.011) |
Note: BMI = body mass index; HRS = Health and Retirement Study.
***p < .001, **p < .01, *p < .05.
Figure 1 displays the trends as predicted prevalence rates for the entire 2000–2014 period based on the trend slope given in Table 2. Not surprisingly, given the group differences in relative decline noted above, dementia prevalence for non-Hispanic Blacks aged 65–74 years dropped substantially and the race gap narrowed somewhat over the period for this age group. Note that the race gap in dementia prevalence is especially prominent for persons aged 75 years and older despite downward trends over the period. These parallel trends point to persistence in the racial gap in dementia even with overall improvements in cognitive health over the period. In 2000, the predicted percentage of Blacks aged 75 years and older with dementia is 35% compared to 16% of Whites. By 2014, the percentages dropped so that 31% of older Blacks and 12% of older Whites had dementia. About 19 percentage points separated the two race groups at the older ages across the 14-year period, an enormous disparity in the burden of dementia.
Turning back to the results in Table 2, controlling for educational attainment significantly reduced the downward trend in dementia prevalence for all age–race groups, except for Blacks aged 75 and older years, where the trend became positive and significant. In other words, had educational attainment not improved among older Blacks, the models would have predicted an increase in dementia prevalence over the time period. With regard to the other groups, the slope approached 1.0, indicating no change over time. Additionally, when examining gender-stratified models shown in Supplementary Table S1, controlling for education also flattened the trend for both genders, although it did not fully attenuate the trend for White women 75 and older.
When childhood conditions (poor childhood health and childhood socioeconomic status [SES]) were controlled in Table 3, the trend effects were only modestly attenuated, and the downward trends remained significant for all groups except older Blacks. Controlling for smoking and BMI did not alter the trend. The downward trend slightly steepened (changes were not statistically significant) when diabetes, heart disease, stroke, and hypertension were controlled. Controlling hypertension, especially, has been invoked to account for the downward trend, yet there is no evidence of this explanation for the 2000–2014 period.
Table 3.
Odds Ratios (SE) of Dementia Prevalence Trend From 2000 to 2014 Derived From Nested Logistic Regression Models with Adjustments for Population Characteristics, by Race–Age Group (HRS)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| NH Whites 65–74 | 0.962*** (0.009) | 0.986 (0.011) | 0.988 (0.011) | 0.989 (0.011) | 0.976* (0.011) |
| NH White 75 and older | 0.973*** (0.005) | 0.990* (0.004) | 0.992 (0.005) | 0.992 (0.005) | 0.991 (0.004) |
| NH Blacks 65–74 | 0.948*** (0.012) | 0.993 (0.014) | 0.992 (0.015) | 0.993 (0.015) | 0.984 (0.015) |
| NH Blacks 75 and older | 0.986 (0.011) | 1.023* (0.009) | 1.025* (0.010) | 1.026* (0.010) | 1.026** (0.009) |
Notes: HRS = Health and Retirement Study; NH = non-Hispanic. Model 1: Trend; Model 2: + Education; Model 3: + Childhood conditions; Model 4: + Health behaviors; Model 5: + Cardiometabolic conditions (Diabetes, Stroke, Hypertension, Heart condition).
***p < .001, **p < .01, *p < .05.
The nested models showing how the trend coefficients change with cumulative adjustment of the covariates are presented in Table 3. As is evident, once educational attainment was controlled, no additional changes or attenuation in the trend slopes occurred when other covariates were added to the models. Our results showed that educational attainment, the key factor considered in this analysis, dampened the downward slope in dementia prevalence for the age–race groups, and that other observed risk factors do not appear to be have contributed to further changes in the trend.
Discussion
The decline in dementia prevalence shown here is consistent with the findings from a number of other studies. What is new is that the trend was evident across the entire 2000–2014 period, was steepest among younger Black Americans, and that educational attainment was fundamentally important in understanding the prevalence changes in the U.S. Black and White population. The United States experienced a dramatic expansion of schooling in the early part of the twentieth century, which led to increasing years of completed schooling for older adults from 2000 to 2014. The increases in educational attainment appear to have made older adults less prone to dementia. This finding is consistent with the idea that the stock of cognitive ability and function has grown in the U.S. population with the improved levels of education (Lövdén et al., 2020). The reduction in dementia prevalence for this time period or demographic groups does not appear to be a direct reflection of changes in medical care or intervention per se.
Goldin (1998, p. 371) called the period 1910–1940 the “second great transformation of American schooling: the rise of the public high school.” The first was the development of the common school in the mid-nineteenth century, while a third transformation has occurred more recently in the growth of college education in the second half of the twentieth century. Goldin contends that neither the first nor third transformations was as dramatic as the rise of the public high school.
Still, the rise in college education has been significant since 1950. College education rose from about 6% for White males in 1950 to 22% in 1980 after which it began to level off. For Black males, about 2% were college educated in 1950 compared to 12% in 1980, although it has continued to increase. What is unclear is whether this increase in college education in the population will have significant implications for future trends in dementia prevalence or whether educational attainment’s influence has largely played out. Recent analyses (Farina et al., 2019) point to lower rates of dementia prevalence for college-educated non-Hispanic Blacks and Whites compared to high school graduates, yet the biggest gap is between those with a high school degree and those with less than a high school degree. In addition, other analyses identify that while the association between educational attainment and dementia risk is evident for different levels of education, there is some evidence that the association is somewhat stronger at lower levels of education (Barnes et al., 2011). The floor of the educational attainment distribution has also shifted upward over time. These changes suggest that the upward shift in the distribution of educational attainment may continue to dampen dementia prevalence in the United States in the next few decades, although the effects may not be as dramatic as those accruing from the “second great transformation of American schooling.”
It is also important to note that the older population is changing with respect to the other dementia risk factors. Obesity has increased significantly in the older population (as has diabetes), as has the expansion of obesity over more years of life (Stokes et al., 2017). This type of change could potentially contribute to reversing the downward trend or dampen it significantly. A recent study (Zheng, 2020) provides evidence that these types of changes are already evident among the Baby Boom cohort. The study documents worsening cognitive functioning among Baby Boomers compared to earlier birth cohorts which appears to reflect lower wealth, less marriage, greater levels of psychological risk factors, and worse cardiovascular risk factors.
The future is, thus, unclear in terms of the likely direction of the dementia prevalence trend. What is less ambiguous, however, is that the trend will be influenced by changes in exposures and behaviors in the population. The future number of people living with dementia does not simply reflect population aging, although that is clearly a major component. Population changes in modifiable factors also will play a role.
Our study set out to examine the trends in dementia prevalence for Whites and Blacks and the impact of improving educational attainment for the trends within each group. We found evidence that educational attainment mattered for both Blacks and Whites, separately. This points to the importance of improving educational attainment for the entire population as a key public health lever in reducing dementia prevalence. Although the specific causal mechanisms are still unclear, the pattern is consistent with the idea that additional years of education in the population are associated with improved cognitive abilities and reduced dementia risk across major groups in the population. This pattern is consistent with other research documenting the robustness of the association between educational attainment and cognitive function across contexts defined by countries, SES groups, and gender (Barnes et al., 2011; Kobayashi et al., 2017; Weber et al., 2014; Xu et al., 2016). Additionally, while we do not directly evaluate disparities per se, our research documents persistent differences over time, with Black Americans experiencing dramatically high rates of dementia.
Limitations
Dementia prevalence reflects both dementia incidence and mortality. Although the current analysis does not evaluate these trends and their sensitivity to population compositional changes, future research will delve into these issues more deeply to connect trends in prevalence and incidence. Second, in our assessment of educational attainment’s role in the prevalence trends, we do not construe education’s effects as necessarily causal or immutable. Changes in educational quality, curriculum/content, and educational selection processes, for example, are aspects of education that are likely to be important to consider in future research on long-term dementia trends. Education is also associated with other adult characteristics which could have changed over time (e.g., occupation) and are important for understanding cognitive status (Baldivia et al., 2008; Fujishiro et al., 2017; Kobayashi et al., 2017). This issue is especially critical to consider in better understanding why education’s association with dementia risk is so robust for both race groups despite dramatic differences in a social context. Third, we did not assess trends for Hispanics or other minority groups such as Asians. A large proportion of Hispanics were foreign-born and only had very low levels of education acquired in another country (Garcia et al., 2019), making them difficult to compare to non-Hispanic Blacks and Whites when assessing the role of education and alternative factors on dementia trends. Nonetheless, future work incorporating Hispanics is likely to be highly informative of how social context shapes the association between educational attainment, cognitive abilities, and cognitive function. Fourth, these data reflect the composition of older adults from multiple cohorts at each time period. We are unable to account for differential mortality selection. Blacks aged 75 and older, for example, are most likely a highly select group of older adults. Despite mortality selection, however, selection is unlikely to explain the downward trend as older Blacks and Whites became less select over time due to continued improvements in survivorship. Finally, we assessed whether practice effects (i.e., do respondents’ exposure to prior tests result in learning the test and in improved scores?) might be contributing to the downward trend in dementia prevalence. We tested whether there was statistical evidence of downward trends within educational groups, hypothesizing that the highest education group would be most likely to exhibit a practice effect. We found no statistical evidence of a downward trend in dementia prevalence within the education groups, supporting our argument that the upward shift in the educational attainment over the observation period underlies the downward trends in dementia prevalence.
Conclusions
This analysis makes clear that dementia declines over the 2000–2014 period, for Whites over age 65, and for Blacks 65–74 years of age. Our findings point to the importance of improvements in educational attainment as a key factor associated with the downward trends of dementia prevalence. The downward trend was unrelated to other dementia risk factors such as controlled hypertension, changes in health behaviors, or changes in early life conditions. At least for the 2000–2014 period and for these demographic groups, the results suggest the importance of improvements in cognitive ability and function, established at younger ages and carried into the adult life course, for the downward trend in dementia prevalence. This finding has implications not only for understanding current trends in the United States, but also the potential role of the growth in cognitive ability and functioning in other countries that underwent similar rapid expansions in schooling.
Funding
This research was partially supported by a grant from the National Institute on Aging (NIA; R56AG057778, PI: M. Hayward) and infrastructure grants from Eunice Kennedy Shrive National Institute of Child Health and Human Development (P2CHD042849 and T32HD007081, Population Research Center, University of Texas at Austin; T32 HD091058, Carolina Population Center, University of North Carolina at Chapel Hill); and NIA (P30AG017265-19S1, R01 AG060110, and T32AG000037, University of Southern California). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
None declared.
Author Contributions
M. D. Hayward conceived the idea, planned the study, wrote the manuscript, and supervised the data analysis. M. P. Farina edited the manuscript, helped plan the study, and completed all statistical analyses. Y. S. Zhang helped plan the study and edited the manuscript. J. K. Kim supervised the statistical analysis and edited the manuscript. E. M. Crimmins helped plan the study, revised the manuscript, and contributed to study design.
Supplementary Material
References
- Baldivia, B., Andrade, V. M., & Bueno, O. F. A. (2008). Contribution of education, occupation and cognitively stimulating activities to the formation of cognitive reserve. Dementia & Neuropsychologia, 2(3), 173–182. doi: 10.1590/S1980-57642009DN20300003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes, L. L., Wilson, R. S., Hebert, L. E., Scherr, P. A., Evans, D. A., & Mendes de Leon, C. F. (2011). Racial differences in the association of education with physical and cognitive function in older blacks and whites. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66(3), 354–363. doi: 10.1093/geronb/gbr016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgart, M., Snyder, H. M., Carrillo, M. C., Fazio, S., Kim, H., & Johns, H. (2015). Summary of the evidence on modifiable risk factors for cognitive decline and dementia: A population-based perspective. Alzheimer’s & Dementia, 11(6), 718–726. doi: 10.1016/j.jalz.2015.05.016 [DOI] [PubMed] [Google Scholar]
- Carruthers, C. K., & Wanamaker, M. H. (2017). Returns to school resources in the Jim Crow South. Explorations in Economic History, 64, 104–110. doi: 10.1016/j.eeh.2017.02.004 [DOI] [Google Scholar]
- Chen, C., & Zissimopoulos, J. M. (2018). Racial and ethnic differences in trends in dementia prevalence and risk factors in the United States. Alzheimer’s & Dementia (New York, N. Y.), 4, 510–520. doi: 10.1016/j.trci.2018.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins, E. M., Kim, J. K., Langa, K. M., & Weir, D. R. (2011). Assessment of cognition using surveys and neuropsychological assessment: the health and retirement study and the aging, demographics, and memory study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66(Suppl. 1), 162–171. doi: 10.1093/geronb/gbr048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins, E. M., Saito, Y., Kim, J. K., Zhang, Y. S., Sasson, I., & Hayward, M. D. (2018). Educational differences in the prevalence of dementia and life expectancy with dementia: Changes from 2000 to 2010. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(S1), S20–S28. doi: 10.1093/geronb/gbx135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donley, G. A. R., Lönnroos, E., Tuomainen, T. P., & Kauhanen, J. (2018). Association of childhood stress with late-life dementia and Alzheimer’s disease: The KIHD study. European Journal of Public Health, 28(6), 1069–1073. doi: 10.1093/eurpub/cky134 [DOI] [PubMed] [Google Scholar]
- Farina, M. P., Hayward, M. D., Kim, J. K., & Crimmins, E. M. (2019). Racial and educational disparities in dementia and dementia-free life expectancy. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(7), e105–e112. doi: 10.1093/geronb/gbz046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujishiro, K., MacDonald, L. A., Crowe, M., McClure, L. A., Howard, V. J., & Wadley, V. G. (2017). The role of occupation in explaining cognitive functioning in later life: Education and occupational complexity in a U.S. national sample of black and white men and women. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 74(7), 1189–1199. doi: 10.1093/geronb/gbx112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, M. A., Downer, B., Chiu, C. T., Saenz, J. L., Rote, S., & Wong, R. (2019). Racial/ethnic and nativity differences in cognitive life expectancies among older adults in the United States. The Gerontologist, 59(2), 281–289. doi: 10.1093/geront/gnx142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour, M. M., & Manly, J. J. (2008). Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology Review, 18(3), 223–254. doi: 10.1007/s11065-008-9064-z [DOI] [PubMed] [Google Scholar]
- Goldin, C. (1998). America’s graduation from high school: The evolution and spread of secondary schooling in the twentieth century. The Journal of Economic History, 58(2), 345–374. doi: 10.1017/S0022050700020544 [DOI] [Google Scholar]
- Guerra-Carrillo, B., Katovich, K., & Bunge, S. A. (2017). Does higher education hone cognitive functioning and learning efficacy? Findings from a large and diverse sample. PLoS One, 12(8), e0182276. doi: 10.1371/journal.pone.0182276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward, M., Crimmins, E., Miles, T., & Yu, Y. (2000). The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review, 65, 910–930. doi: 10.2307/2657519 [DOI] [Google Scholar]
- Kobayashi, L. C., Glymour, M. M., Kahn, K., Payne, C. F., Wagner, R. G., Montana, L., Mateen, F. J., Tollman, S. M., & Berkman, L. F. (2017). Childhood deprivation and later-life cognitive function in a population-based study of older rural South Africans. Social Science & Medicine (1982), 190, 20–28. doi: 10.1016/j.socscimed.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langa, K. M., Larson, E. B., Crimmins, E. M., & et al. (2017). A comparison of the prevalence of dementia in the united states in 2000 and 2012. Journal of American Medical Association Internal Medicine, 177(1), 51–58. doi: 10.1001/jamainternmed.2016.6807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lövdén, M., Fratiglioni, L., Glymour, M. M., Lindenberger, U., & Tucker-Drob, E. M. (2020). Education and cognitive functioning across the life span. Psychological Science in the Public Interest, 21(1), 6–41. doi: 10.1177/1529100620920576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather, M. (2020). How do cognitively stimulating activities affect cognition and the brain throughout life? Psychological Science in the Public Interest, 21(1), 1–5. doi: 10.1177/1529100620941808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Education Statistics . (1993). Elementary and secondary education. In Snyder T. D. (Ed.), 120 years of American education: A statistical portrait. National Center for Education Statistics. [Google Scholar]
- Peters, R., Poulter, R., Warner, J., Beckett, N., Burch, L., & Bulpitt, C. (2008). Smoking, dementia and cognitive decline in the elderly, a systematic review. BMC Geriatrics, 8, 36. doi: 10.1186/1471-2318-8-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca, W. A., Petersen, R. C., Knopman, D. S., Hebert, L. E., Evans, D. A., Hall, K. S.,Gao, S., Unverzagt, F. W., Langa, K. M., Larson, E. B., & White, L. R. (2011). Trends in the incidence and prevalence of Alzheimer’s disease, dementia, and cognitive impairment in the United States. Alzheimer’s & Dementia, 7(1), 80–93. doi: 10.1016/j.jalz.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes, A., Ni, Y., & Preston, S. H. (2017). Prevalence and trends in lifetime obesity in the U.S., 1988–2014. American Journal of Preventive Medicine, 53(5), 567–575. doi: 10.1016/j.amepre.2017.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber, D., Skirbekk, V., Freund, I., & Herlitz, A. (2014). The changing face of cognitive gender differences in Europe. Proceedings of the National Academy of Sciences of the United States of America, 111(32), 11673–11678. doi: 10.1073/pnas.1319538111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weuve, J., Barnes, L. L., Mendes de Leon, C. F., Rajan, K. B., Beck, T., Aggarwal, N. T., Hebert, L. E., Bennett, D. A., Wilson, R. S., & Evans, D. A. (2018). Cognitive aging in black and white Americans: Cognition, cognitive decline, and incidence of Alzheimer disease dementia. Epidemiology (Cambridge, Mass.), 29(1), 151–159. doi: 10.1097/EDE.0000000000000747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, W., Tan, L., Wang, H. F., Tan, M. S., Tan, L., Li, J. Q., Zhao, Q. F., & Yu, J. T. (2016). Education and risk of dementia: Dose–response meta-analysis of prospective cohort studies. Molecular Neurobiology, 53(5), 3113–3123. doi: 10.1007/s12035-015-9211-5 [DOI] [PubMed] [Google Scholar]
- Zheng, H. (2020). A new look at cohort trend and underlying mechanisms in cognitive functioning. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi: 10.1093/geronb/gbaa107 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.