ABSTRACT
This study aimed to investigate the current trends in antimicrobial resistance among Pseudomonas aeruginosa clinical isolates of canine and feline origin and the prevalence of their sequence types (STs) and type III secretion system (T3SS) virulotypes, which remains unknown in Japan. A total of 240 nonduplicate clinical isolates of P. aeruginosa from dogs (n = 206) and cats (n = 34) collected from 152 primary care animal hospitals between August 2017 and October 2019 were examined. PCR detection of T3SS genes (exoU and exoS) and carbapenemase genes, multilocus sequence typing, and whole-genome sequencing of the representative carbapenem-resistant isolates were performed. Resistance rates to imipenem and meropenem were 6.67% and 2.08%, respectively. A high resistance rate (17.92%) was encountered with ciprofloxacin. The exoU−/exoS+ was the predominant T3SS virulotype (195 isolates, 81.3%), followed by exoU+/exoS− (35 isolates, 14.6%), exoU−/exoS− (7 isolates, 2.9%), and exoU+/exoS+ (3 isolates, 1.3%). A high frequency of the high-risk clones ST235 and clonal complex 235 (CC 235) (28.9%), followed by ST357 (21.1%), were noted among these 38 exoU+ isolates. Seventeen carbapenem-resistant isolates comprising 2 exoU+ isolates, including an ST235 isolate, and 15 exoU−/exoS+ isolates belonging to non-ST235/CC235 were detected, of which all were carbapenemase negative. Different combinations of mutations among oprD, efflux pump regulatory genes, and AmpC β-lactamase regulatory genes were identified among representative isolates with high-level resistance to imipenem. This study emphasizes the occurrence of ST235 isolates among companion animals, which may represent a threat to public health because of the ability of this clone to acquire and spread resistance elements, including carbapenemase genes.
IMPORTANCE Pseudomonas aeruginosa is an environmentally ubiquitous and important opportunistic human pathogen responsible for life-threatening health care-associated infections. Because of its extensive repertoire of virulence determinants and intrinsic and acquired resistance mechanisms, the organism could be one of the most clinically and epidemiologically important causes of morbidity and mortality. In recent years, worldwide spreading of multidrug-resistant high-risk clones, particularly sequence type 235 (ST235), has become a serious public health threat. Companion animals which share much of their living environment with humans could be important reservoirs and spreaders of antimicrobial-resistant bacteria and resistance genes of clinical importance in humans, such as extended-spectrum β-lactamase-producing Enterobacterales and methicillin-resistant Staphylococcus aureus. However, antimicrobial resistance, virulence, and genotyping of P. aeruginosa in companion animals remain largely unknown. This work sheds light on the potential spread of high-risk clones in companion animals.
KEYWORDS: Pseudomonas aeruginosa, companion animal, T3SS, ST235
INTRODUCTION
Pseudomonas aeruginosa is an important opportunistic human pathogen capable of causing a wide variety of life-threatening acute and chronic infections and is also a major cause of health care-associated infections. The bacterium is environmentally ubiquitous, inhabiting soil, water, plants, and animals, and can be isolated from the skin, throat, and stool of healthy persons. P. aeruginosa is equipped with an extensive repertoire of virulence determinants implicated in pathogenesis and intrinsic and acquired resistance mechanisms, which makes the organism one of the most clinically and epidemiologically important causes of morbidity and mortality (1).
Recent studies have raised attention to the increasing worldwide prevalence of P. aeruginosa high-risk clones that are multidrug resistant (MDR) or extensively drug resistant (XDR) in hospitals. Those internationally recognized high-risk clones include sequence type 235 (ST235), ST111, ST233, ST244, ST357, ST308, ST175, ST277, ST654, and ST298 (2). Carbapenem resistance in P. aeruginosa can be mediated by several mechanisms, including the interaction of OprD inactivation, Mex efflux system overexpression, and intrinsic AmpC β-lactamase overexpression and the production of acquired carbapenemases. VIM- and IMP-type metallo-β-lactamases are the most commonly encountered carbapenemases in P. aeruginosa, including international high-risk clones, although other carbapenemases, such as KPC, GES, NDM, and SPM, have also been reported globally (2). In Japan, GES, IMP, and VIM types have so far been identified among carbapenemase-producing high-risk clones, including ST235, ST244, ST357, ST308, ST175, and ST277 (2). Particularly, outbreaks of ST235 producing IMP type or GES 5 have been reported in clinical settings in Japan (3, 4).
One of the most important virulence factors resulting in a poor prognosis of infections is the type III secretion system (T3SS) (5). The system injects bacterial effector exotoxins, including ExoU (phospholipase A2), ExoS (Rho GTPase-activating protein [RhoGAP]/ADP-ribosyltransferase [ADPRT]), ExoT (RhoGAP/ADPRT), and ExoY (adenyl cyclase) identified so far, into host cells (6). ExoU and ExoS are responsible for the cytotoxic phenotype and invasive phenotype, respectively, contributing more significantly to pathogenesis than the other exotoxins (7, 8). ExoU is located in pathogenicity island 2 (PAPI-2), and ExoS shows mostly mutually exclusive distributions, while ExoT and ExoY are carried by most of the strains (9). The exoU+ genotype has been frequently associated with multidrug resistance, fluoroquinolone resistance, and highly virulent phenotypes, as represented by the ST235 high-risk clone, resulting in increased mortality in bloodstream infections (10–12).
Companion animals have been recognized as potential reservoirs of antimicrobial resistance genes and resistant bacteria that can be transmitted to humans (13, 14). However, studies on P. aeruginosa virulence and antimicrobial resistance in companion animals are scarce and have focused mostly on human isolates. In France, ST233 and potential high-risk clones ST395 and ST253 have been found among 29 carbapenemase-negative carbapenem-nonsusceptible P. aeruginosa clinical isolates of canine and feline origin (15). VIM-2-positive ST233 and IMP-45-positive ST308 P. aeruginosa have been reported to be associated with possible human-to-dog transmission in Brazil and China (16, 17). In a US canine study, exoU−/exoS+, exoU+/exoS−, and exoU-/exoS− T3SS virulotypes have been identified in 15, 3, and 1 isolates, respectively, among 19 isolates from ocular infections, while exoU−/exoS+ and exoU+/exoS+ virulotypes have been detected in 5 and 1 isolates, respectively, among 6 normal conjunctival microflora isolates (18).
In Japan, only a few epidemiological studies are available to date on the antimicrobial resistance of P. aeruginosa clinical isolates of companion animal origin (19, 20). A recent study has documented the low rates of resistance to ceftazidime (0.5%), ciprofloxacin (9%), and amikacin (2.5%), and neither imipenem-resistant isolates nor metallo-β-lactamase producers have been identified (20). This study investigates the current trends in antimicrobial resistance among P. aeruginosa clinical isolates of canine and feline origin and the prevalence of their STs and T3SS virulotypes, which remains unknown in Japan, to better understand their epidemiological aspects.
RESULTS
Prevalence of antibiotic resistance and T3SS virulotypes among P. aeruginosa isolates.
The ranges of MICs for 240 isolates of P. aeruginosa against imipenem and meropenem were ≤1 to >64 mg/liter and ≤0.5 to 16 mg/liter, respectively. The rates of resistance were 6.67% (16 isolates) for imipenem and 2.08% (5 isolates) for meropenem (Table 1). Notably, those results are comparable to the corresponding carbapenem resistance rates, namely, 5.7% for imipenem and 2.8% for meropenem in P. aeruginosa isolates among outpatients in 2019 obtained from the Japan Nosocomial Infections Surveillance (JANIS) database (Table 1) (https://janis.mhlw.go.jp/report/open_report/2019/3/1/ken_Open_Report_201900_Outpatient.pdf). In contrast, the resistance rates against piperacillin, piperacillin-tazobactam, ceftazidime, and cefepime were 0.83% (2 isolates), 0.83% (2 isolates), 0.83% (2 isolates), and 0.42%, (1 isolate), respectively, which were lower than those from JANIS data of outpatient isolates. The resistance levels of aminoglycosides were 0.42% (1 isolate) for amikacin, 2.08% (5 isolates) for gentamicin, and 1.67% (4 isolates) for tobramycin. A high resistance rate was encountered with ciprofloxacin (43 isolates, 17.92%), surpassing the resistance rate against levofloxacin among clinical isolates from both inpatients (9.8%) and outpatients (6.0%). Individual MIC values for each isolate are listed in Table S1 in the supplemental material.
TABLE 1.
The MICs and the antimicrobial resistance rates for the 240 P. aeruginosa isolates from dogs and cats
| Antimicrobial agent(s) | MIC range (mg/liter) | MIC50 (mg/liter) | MIC90 (mg/liter) | Resistance (%) | 2019 JANIS dataa on human clinical isolates (resistance %) from: |
|
|---|---|---|---|---|---|---|
| Inpatients | Outpatients | |||||
| Piperacillin | ≤4 to >128 | 8 | 16 | 0.83 | 10.3 | 3.4 |
| Piperacillin-tazobactam | ≤8/4 to 128/4 | ≤8/4 | 16/4 | 0.83 | 8.4 | 2.5 |
| Ceftazidime | ≤2 to 64 | ≤2 | 8 | 0.83 | 8.7 | 2.9 |
| Cefepime | ≤2 to 32 | 4 | 8 | 0.42 | 5.9 | 2.3 |
| Aztreonam | ≤2 to 64 | 8 | 32 | 11.25 | 13.3 | 6.5 |
| Imipenem | ≤1 to >64 | 2 | 4 | 6.67 | 16.2 | 5.7 |
| Meropenem | ≤0.5 to 16 | ≤0.5 | 2 | 2.08 | 10.6 | 2.8 |
| Gentamicin | ≤1 to >32 | 2 | 4 | 2.08 | 3.1 | 2.6 |
| Amikacin | ≤2 to >64 | 4 | 8 | 0.42 | 0.9 | 0.8 |
| Tobramycin | ≤2 to >32 | ≤2 | ≤2 | 1.67 | NAb | NA |
| Ciprofloxacin | ≤0.5 to >8 | ≤0.5 | 4 | 17.92 | 9.8 (levofloxacin) | 6.0 (levofloxacin) |
JANIS, Japan Nosocomial Infections Surveillance.
NA, not available.
The presence of 40 mg/liter phenylalanine-arginine β-naphthylamide (PaβN) did not inhibit the growth of 43 ciprofloxacin-resistant P. aeruginosa isolates except 1, for which the PAβN concentration not affecting its growth (20 mg/liter) was used for the efflux pump inhibition. All 43 isolates, including 7 carbapenem-resistant isolates, showed more than or equal to a 4-fold reduction in the MIC of ciprofloxacin in the presence of PAβN (data not shown).
Overall, the frequency of exoU and exoS genes was 15.8% (38/240 isolates) and 82.5% (198/240 isolates), respectively. PCR revealed 4 T3SS virulotypes among 240 isolates, namely, 35 exoU+/exoS− isolates (14.6%), 195 exoU−/exoS+ isolates (81.3%), 3 exoU+/exoS+ isolates (1.3%), and 7 exoU−/exoS− isolates (2.9%). Table 2 shows the distribution of T3SS virulotypes according to antimicrobial resistance. The exoU+/exoS− isolates, compared with the exoU−/exoS+ isolates, were significantly associated with resistance to piperacillin (P = 0.02843), piperacillin-tazobactam (P = 0.03787), gentamicin (P = 0.009844), and tobramycin (P = 0.04685). Alternatively, no statistically significant association was found between these virulotypes and resistance to imipenem, meropenem, and ciprofloxacin.
TABLE 2.
Distribution of T3SS virulotypes among P. aeruginosa clinical isolates from companion animals according to antimicrobial resistance
| Antimicrobial(s) | No. (%) of isolates by T3SS virulotype |
P value for comparison between exoU+/exoS− and exoU−/exoS+ | |||
|---|---|---|---|---|---|
| exoU+/exoS− (n = 35) | exoU−/exoS+ (n = 195) | exoU+/exoS+ (n = 3) | exoU−/exoS− (n = 7) | ||
| Piperacillin | 6 (17) | 11 (6) | 0 | 0 | 0.02843 |
| Piperacillin-tazobactam | 6 (17) | 12 (6) | 0 | 0 | 0.03787 |
| Ceftazidime | 1 (3) | 5 (3) | 0 | 0 | |
| Cefepime | 1 (3) | 12 (6) | 0 | 0 | |
| Aztreonam | 8 (23) | 49 (25) | 0 | 0 | |
| Imipenem | 4 (11) | 41 (21) | 0 | 0 | |
| Meropenem | 2 (6) | 11 (6) | 0 | 0 | |
| Gentamicin | 6 (17) | 8 (4) | 0 | 0 | 0.009844 |
| Amikacin | 0 (0) | 2 (1) | 0 | 0 | |
| Tobramycin | 3 (9) | 3 (2) | 0 | 0 | 0.04685 |
| Ciprofloxacin | 6 (17) | 60 (31) | 0 | 1 | |
| Colistin | 0 (0) | 1 (1) | 0 | 0 | |
Multilocus sequence typing (MLST) of exoU+ isolates.
The 35 exoU+/exoS− isolates were assigned to 20 STs from which 2 new STs, namely, ST235-like and ST3654, were identified (Table 3). The 3 exoU+/exoS+ isolates belonged to different STs, including a new ST, ST3653. The high frequency of high-risk clone ST235 (8, 21.1%) and ST141 (1, 2.6%), ST235-like (1, 2.6%), and ST3653 (1, 2.6%) belonging to CC235 was noted among those 38 exoU+ isolates (11, 28.9%). Other high-risk clones and clonal complexes identified were ST357 (8, 21.1%), ST2644 (CC274) (3, 7.9%), ST308 (2, 5.3%), ST253 (1, 2.6%), and ST446 (CC298) (1, 2.6%).
TABLE 3.
STs identified among the 38 exoU+ P. aeruginosa clinical isolates from companion animals
| MLST sequence type |
Clonal complex | No. of clinical isolates by virulotype and animal |
Total no. of isolates | |||
|---|---|---|---|---|---|---|
|
exoU+/exoS− (n = 35) |
exoU+/exoS+ (n = 3) |
|||||
| Dog | Cat | Dog | Cat | |||
| ST235 | CC235 | 5 | 2 | 1 | 8 | |
| ST141 | 1 | 1 | ||||
| ST235-likea | 1 | 1 | ||||
| ST3653b | 1 | 1 | ||||
| ST357 | CC357 | 7 | 1 | 8 | ||
| ST2644 | CC274 | 3 | 3 | |||
| ST308 | CC308 | 2 | 2 | |||
| ST671 | CC560 | 1 | 1 | 2 | ||
| ST253 | CC253 | 1 | 1 | |||
| ST313 | CC313 | 1 | 1 | |||
| ST316 | CC316 | 1 | 1 | |||
| ST2555 | 1 | 1 | ||||
| ST446 | CC298 | 1 | 1 | |||
| ST606 | NAc | 1 | 1 | |||
| ST773 | NA | 1 | 1 | |||
| ST829 | NA | 1 | 1 | |||
| ST1121 | NA | 1 | 1 | |||
| ST1248 | NA | 1 | 1 | |||
| ST1334 | NA | 1 | 1 | |||
| ST3654b | NA | 1 | 1 | |||
| Total | 32 | 3 | 3 | 38 | ||
Novel trpE allele was associated with ST235-like.
Sequence types newly assigned in this study.
NA, not assigned.
Phenotypic characteristics of carbapenem-resistant P. aeruginosa isolates.
Among the 240 isolates, 17 (7.1%) were resistant to imipenem and/or meropenem. Detection of carbapenemase production by a modified carbapenem inactivation method using Tris-HCl (CIMTris) assay yielded negative results for all 17 isolates. In those isolates, the major carbapenemase genes blaIMP, blaNDM, blaVIM, and blaGES were not detected (Table 4).
TABLE 4.
Features of the 17 carbapenem-resistant P. aeruginosa isolates
| Isolate |
Animal species |
Clinical sample | MLST sequence type | T3SS virulotype |
Carbapenemase detection |
MIC (mg/liter)a of: |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Name | exoU+/exoS− | exoU−/exoS+ | CIMTris | PCR detection of blaIMP, blaNDM, blaVIM, and blaGES | IPM | IPM + PAβN | IPM + APB | IPM + PaβN + APB | MEPM | MEPM + PAβN | MEPM + APB | MEPM + PaβN + APB | |||
| 1 | CA10562 | Dog | Ear discharge | ST3014 (CC3014) | − | + | − | − | 8 | 1 | 0.5 | ≤0.25 | ||||
| 2 | CA12133 | Dog | Ear discharge | ST1600 | − | + | − | − | 64 | 4 | 8 | 1 | ||||
| 3 | CA12482 | Cat | Skin | ST198 (CC198) | − | + | − | − | 16 | 16 | 1 | 1 | ||||
| 4 | CA13227 | Dog | Ear discharge | ST209 (CC274) | − | + | − | − | 8 | 8 | 1 | 1 | ||||
| 5 | CA13620 | Dog | Ear discharge | ST277 (CC277) | − | + | − | − | 4 | 2 | 0.5 | ≤0.25 | 4 | 4 | 4 | 2 |
| 6 | CA13876 | Cat | Nasal discharge | ST1097 | − | + | − | − | 8 | 4 | 0.5 | ≤0.25 | ||||
| 7 | CA14241 | Dog | Ear discharge | ST3045 | − | + | − | − | 16 | 16 | 1 | 2 | ||||
| 8 | CA16138 | Dog | Ear discharge | ST3574b (CC262) | − | + | − | − | 8 | 2 c | 4 | 1 c | ||||
| 9 | CA16209 | Dog | Ear discharge | ST606 | + | − | − | − | 8 | 1 | 0.5 | ≤0.25 | ||||
| 10 | CA17343 | Dog | Uterine pus | ST348 (CC348) | − | + | − | − | 128 | 8 c | 4 | 0.5 c | 16 | 2 c | 8 | 2 c |
| 11 | CA17462 | Dog | Urine | ST270 | − | + | − | − | 4 | 1 | 0.5 | ≤0.25 | ||||
| 12 | CA17502 | Dog | Ear discharge | ST155 (CC155) | − | + | − | − | 16 | 4 | 8 | 4 | ||||
| 13 | CA19603 | Cat | Ear discharge | ST235 (CC235) | + | − | − | − | 32 | 16 | 2 | NGd | 8 | 1 | 4 | NGd |
| 14 | CA19802 | Dog | Urine | ST399 (CC399) | − | + | − | − | 32 | 16 | 2 | 2 | 16 | 8 | 8 | 4 |
| 15 | CA19818 | Dog | Urine | ST266 | − | + | − | − | 4 | 2 | ≤0.25 | ≤0.25 | ||||
| 16 | CA20091 | Dog | Ear discharge | ST348 (CC348) | − | + | − | − | 4 | 4 | 0.5 | 0.5 | ||||
| 17 | CA20115 | Dog | Urine | ST3135 | − | + | − | − | 4 | 8 | 0.5 | 0.5 | ||||
A decrease of more than 4-fold in MIC values are indicated in bold.
Sequence type newly assigned in this study.
PAβN concentration of 20 mg/liter was used.
No visible growth was observed in the presence of imipenem or meropenem plus 20- or 40-mg/liter PAβN and 300-mg/liter APB.
The presence of 40-mg/liter PAβN did not inhibit the growth of 17 carbapenem-resistant P. aeruginosa, except for 2 isolates (no. 8 and 10), for which PAβN concentration not affecting their growth (20 mg/liter) was used for the efflux pump inhibition. A 4-fold or greater decrease in the MICs of imipenem and/or meropenem with the addition of PAβN was observed in 8 of 17 isolates (47.1%) (Table 4). In the presence of 3-aminophenylboronic acid (APB), an inhibitor of AmpC β-lactamase, most isolates (15/16, 93.8%) exhibited a greater than or equal to an 8-fold reduction in the MICs of imipenem, while MICs of meropenem for 5 isolates were not affected. It was noticed that APB and PAβN plus APB effectively change interpretive categories from imipenem resistant/intermediate (MIC, ≥8/4 mg/liter) to susceptible (MIC, ≤2 mg/liter) in 13 (81.3%) and 15 isolates (93.8%), respectively. Meropenem MIC of an isolate (no. 12) with the imipenem-susceptible, meropenem-resistant phenotype was affected by PAβN (4-fold reduction) but was not affected by APB.
Genotypic characteristics of carbapenem-resistant P. aeruginosa isolates.
MLST sequence types and T3SS virulotypes of 17 carbapenem-resistant isolates are shown in Table 4. These isolates were assigned to 16 STs, including a newly identified ST3574 (CC262). They contained 2 exoU+/exoS− isolates and 15 exoU−/exoS+ isolates. It was of note that high-risk international clones ST235 with an exoU+/exoS− virulotype (no. 13) and ST277 with an exoU-/exoS+ virulotype (no. 5) were each identified in 1 isolate. The remaining 1 exoU+/exoS− isolate belonged to ST606 (no. 9). ST348 with an exoU−/exoS+ virulotype was detected in 2 isolates, namely, no. 10 and 16 (11.8%), of which 1 exhibited high-level resistance to imipenem (MIC, 128 mg/liter).
Genomic features of carbapenem-resistant isolates.
Three representative P. aeruginosa isolates, including 2 showing high-level resistance to imipenem (no. 2 and 10; MICs, ≥ 64 mg/liter) and 1 isolate of the ST235 international high-risk clone (no. 13), were subjected to whole-genome sequencing (WGS). The assembled genomes of isolate no. 2, 10, and 13 contained 71, 118, and 143 contig sequences, with a total length of 6,270,234 bp, 6,831,356 bp, and 6,646,878 bp, respectively, with a GC content ranging from 66.1% to 66.5%.
Multiple antimicrobial resistance genes, including species-intrinsic blaOXA-50-like, blaPDC, aph(3′)-IIb, fosA, and catB7 were found among the 3 isolates, where ST1600/O3 (isolate no. 2) harbored newly identified blaOXA-937 (Table 5). In addition, ST348/O2 (isolate no. 10) with a ciprofloxacin MIC of 0.5 mg/liter harbored crpP (ciprofloxacin-modifying enzyme) that was recently identified in a P. aeruginosa clinical isolate in Mexico (21). ST235/O11 (isolate no. 13) also contained 2 different class 1 integron-associated gene cassettes, and 1 contained qnrVC1-aac(6′)-Ib-blaOXA-10-aadA1-dfrA14 and the other contained aadB-cmlA10-aadA2-sul1, conferring resistance to quinolones, aminoglycosides, β-lactams, trimethoprim, chloramphenicol, and sulfonamide. Different amino acid substitutions in AmpR were observed in the ST348/O2 and ST235/O11 isolates. The ST1600/O3 isolate with a ciprofloxacin MIC of 32 mg/liter had Ser466Phe in the quinolone resistance-determining region (QRDR) of GyrB.
TABLE 5.
Genetic characteristics of P. aeruginosa isolates no. 2, no. 10, and no. 13
| Characteristic | Results for: |
||
|---|---|---|---|
| Isolate 2 (CA12133) | Isolate 10 (CA17343) | Isolate 13 (CA19603) | |
| Sequence type/serotype | ST1600/O3 | ST348/O2 | ST235/O11 |
| Antimicrobial resistance genes | blaPDC-3, blaOXA-937, aph(3′)-IIb, fosA, catB7 | blaOXA-494, blaPDC-5, aph(3′)-IIb, fosA, catB7, crpP | blaOXA-488, blaPDC-35, aph(3′)-IIb, fosA, catB7, qnrVC1-aac(6′)-Ib-blaOXA-10-aadA1-dfrA14, aadB-cmlA10-aadA2-sul1 |
| Amino acid substitutionsa | |||
| AmpC regulators | |||
| AmpR | Arg244Trp, Gly273Glu | Gly283Glu, Met288Arg | |
| AmpD | Ser5Phe, Gly148Ala, Asp183Tyr | Gly148Ala | |
| AmpDh2 | |||
| AmpDh3 | Ile67Thr | Ala219Thr | Ala208Val |
| MexAB-OprM regulators | |||
| MexR | Val126Glu | ||
| NalC | Gly71Glu, Ser209Arg | Glu153Gln | |
| NalD | |||
| MexCD-OprJ regulator | |||
| NfxB | Arg21His, Asp56Gly, Gly133Ser | ||
| MexEF-OprN regulators | |||
| MexS | Asp249Asn | Gly78Ser, Asp249Asn | frameshift (Δnt 362T) |
| MexT | |||
| MexXY-OprA regulator | |||
| MexZ | Frameshift (Δnt 399G) | ||
| OprD mutationsa | Thr103Ser, Lys115Thr, Phe170Leu | Premature stop codon (W65stop) | Δnt 1–75 |
| QRDR mutationa | Ser466Phe (GyrB) | ||
| Heavy metal resistance genes | copRS, copAB, czcABCD, colRS, chrA, sodA | copRS, copAB, copD, czcABCD, colRS, chrA, sodA | copRS, copAB, czcABCD, colRS, chrA, sodA |
| Virulence-associated genes | T1SS (aprA, aprX, hasAp), T2SS (lasA, lasB, plcH, plcN, plcB, prpL, phoA, lipA, lipC, loxA, toxA, paAP), T3SS (exoT, exoS, exoY), H2-T6SS (tssB2, pldB), H3-T6SS (tssB3), QS (lasI, lasR, rhlI, rhlR), others (fliC, rhlAB) | T1SS (aprA, aprX, hasAp), T2SS (lasA, lasB, plcH, plcN, plcB, prpL, phoA, lipA, lipC, loxA, toxA, cbpD, paAP), T3SS (exoT, exoS, exoY), H2-T6SS (tssB2, pldB), H3-T6SS (tssB3), QS (lasI, lasR, rhlI, rhlR), others (fliC, rhlAB) | T1SS (aprA, aprX, hasAp), T2SS (lasA, lasB, plcH, plcN, plcB, prpL, phoA, lipA, lipC, loxA, toxA, cbpD, paAP), T3SS (exoT, exoU, exoY), H2-T6SS (tssB2, pldA, pldB), H3-T6SS (tssB3), QS (lasI, lasR, rhlI, rhlR), others (fliC, rhlAB) |
Amino acid substitution compared to the sequences of Pseudomonas aeruginosa strain PAO1 (GenBank accession number AE004091).
A mutated OprD porin by amino acid substitutions Thr103Ser, Lys115Thr, and Phe170Leu (ST1600/O3); a premature stop codon (ST348/O2); and a 75-bp deletion leading to a frameshift (ST235/O11) were identified (Table 5). These isolates had amino acid substitutions in the MexAB-OprM repressors MexR and NalC, Gly71Glu and Ser209Arg in NalC (ST1600/O3), and Val126Glu in MexR and Glu153Gln in NalC (ST235/O11). The substitutions of Arg21His, Asp56Gly, and Gly133Ser in NfxB of MexCD-OprJ and Asp249Asn in MexS of MexEF-OprN were found in the ST1600/O3 isolate. Gly78Ser and Asp249Asn in MexS of MexEF-OprN were also noted in the ST348/O2 isolate. In the ST235/O11 isolate, a frameshift mutation (a deletion of a T at position 362) was identified in MexS.
Three isolates shared virulence genes encoding secretion system components of types I (T1SS) and II (T2SS), LasR-LasI and RhlR-RhlI quorum-sensing (QS) systems, FliC flagellin, and rhamnolipid synthetic enzyme RhlAB (22, 23). However, different types of gene clusters were found in T3SS, namely, exoT/exoS/exoY for ST1600/O3 and ST348/O2 isolates and exoT/exoU/exoY for an ST235/O11 isolate. Also, three isolates shared pldB (H2-T6SS effector encoding gene), whereas only one ST235/O11 isolate also carried pldA (H2-T6SS effector encoding gene) (24). Heavy metal resistance genes, including those associated with copper (copRS, copAB, and copD), cobalt/zinc/cadmium (czcABCD), chromate (chrA), cadmium (sodA), and colRS regulating multimetal resistance, were identified among them (25).
Whole-genome multilocus sequence typing (wgMLST).
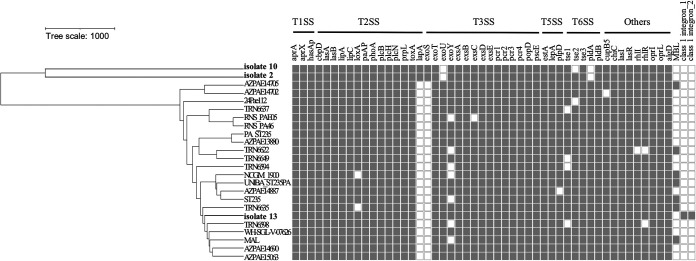
The genomic diversity of the ST235 isolates was assessed by wgMLST gene-by-gene comparison. The animal-derived ST235/O11 isolate with exoU+/exoS− virulotype (isolate 13, CA19603) clustered with 21 ST235 isolates of human origin characterized by the exoU+ genotype (Fig. 1). They shared mostly important virulence-associated genes, including pldA and pldB. It is worth noting that the class I integron-associated gene cassettes that confer antimicrobial resistance, i.e., qnrVC1-aac(6′)-Ib-blaOXA-10-aadA1-dfrA14 and aadB-cmlA10-aadA2-sul1, were identified in isolate 13.
FIG 1.
Whole-genome multilocus sequence typing (wgMLST) of P. aeruginosa ST235/O11 isolates. The carbapenem-resistant, carbapenemase nonproducing ST235/O11 isolate 13 (CA19603) in this study and 21 representative strains of human origin were analyzed. The presence (gray) or absence (white) of virulence-associated genes, metallo-β-lactamase (MBL) genes, and class 1 integron-associated gene cassettes among strains are shown. ST1600/O3 (isolate 2, CA12133) and ST348/O2 (isolate 10, CA17343) in this study are also included for comparison. MBL, blaIMP, blaNDM, and blaVIM; class 1 integron_1, qnrVC1-aac(6′)-Ib-blaOXA-10-aadA1-dfrA14; class 1 integron_2, aadB-cmlA10-aadA2-sul1.
DISCUSSION
The perspective of One Health emphasizes the importance of AMR monitoring and integrated actions across human, food, animal, and environmental health. However, there are few studies on the epidemiology of antimicrobial resistance in P. aeruginosa clinical isolates from companion animals that share a living environment with humans. The strength of our study is that we included 240 P. aeruginosa clinical isolates collected from 152 primary care animal hospitals across the country, allowing us to understand the current situation of their antimicrobial resistance in companion animals as well as to investigate the resistance trends over time in Japan by comparing the results with those in earlier studies (19, 20). Namely, a trend toward a progressive increase in the frequency of imipenem resistance, from 0% in 2003 to 2010 (19), to 0.5% in 2014 to 2015 (20), to 6.67% in 2017 to 2019 (this study) is noted according to the breakpoints of the Clinical and Laboratory Standards Institute (CLSI) M100 30th edition guidelines (26).
The carbapenem resistance rates of isolates from companion animals were found to be similar to those from human outpatients in Japan, leading to concerns about the transmission of carbapenem-resistant P. aeruginosa between humans and companion animals in community settings. The ciprofloxacin resistance rate of 17.92% in our study is nearly flat from the previous years; 23.39% was found in 2003 to 2010 and 14.87% in 2014 to 2015 (19, 20). Constant amounts of veterinary fluoroquinolones such as enrofloxacin and orbifloxacin, at 0.90 tons per year during 2013 and 2018, have been used for dogs and cats as described in the Nippon AMR One Health Report (NAOR) 2020 (in Japanese, https://www.mhlw.go.jp/content/10900000/000715546.pdf). However, consumption of fluoroquinolones which are approved for human use such as levofloxacin and ciprofloxacin in companion animals cannot be traced because their prescription is left to the discretion of veterinarians in Japan. Thus, attention is necessary to monitor for high levels of resistance to ciprofloxacin, which is an active metabolite of enrofloxacin in companion animals, because ciprofloxacin is an effective treatment option in many human diseases. In contrast, piperacillin, piperacillin-tazobactam, ceftazidime, and cefepime retained activity against >99% of animal isolates, which is greater than the activity against isolates from hospital inpatients and outpatients (Table 1). Interestingly, in companion animals, none of the carbapenem-resistant isolates produced carbapenemases, and no multidrug-resistant P. aeruginosa isolates (MDRP) as defined by the Infectious Diseases Control Law in Japan (resistant to imipenem [MIC, ≥16 mg/liter], amikacin [MIC, ≥32 mg/liter], and ciprofloxacin [MIC, ≥4 mg/liter]) were identified, which is consistent with observations in previous animal studies (19, 20). However, our study detected four pre-MDRP isolates with imipenem MICs of ≥16 mg/liter and ciprofloxacin MICs of ≥4 mg/liter, emphasizing the need for continuous surveillance of resistance trends of this important pathogen.
To our knowledge, only one study has analyzed the T3SS virulotypes in a limited number of P. aeruginosa isolates from canine, reporting that 3 of 19 isolates from ocular infections were exoU+ genotypes (18). This study revealed that the prevalence of T3SS virulence genes among 240 clinical isolates of canine and feline origin (15.8% for exoU and 82.5% for exoS) is more similar to that of 90 environmental isolates (17.8% for exoU and 82.2% for exoS) than that of 243 human isolates from bloodstream infections (20.6% for exoU and 76.1% for exoS) (12, 27). There was no significant association between the exoU+/exoS− virulotype and ciprofloxacin and carbapenem resistance, contrary to some other studies reporting such an association in human isolates (11, 28). However, the exoU+ genotype has been an independent risk factor for early mortality of human bloodstream infections (11, 12), and our results draw attention to the prevalence of exoU+ isolates in a greater number of animal isolates.
Among global high-risk clones with MDR/XDR profiles, ST235 is highly associated with exoU, and this combination has been a predictor of a highly unfavorable prognosis (29). Thus, MLST analysis of exoU+ isolates is of clinical importance, as ST235 has not been confirmed among P. aeruginosa isolates from companion animals. MLST revealed clonal heterogeneity in the 38 exoU+ isolates, including exoU+/exoS− and exoU+/exoS+ virulotypes, with the presence of 20 STs, including 3 newly identified STs. Notably, the global high-risk clone ST235 was detected in 7 exoU+/exoS− isolates and in 1 exoU+/exoS+ isolate. Moreover, 3 CC235 isolates were found in 2 exoU+/exoS− isolates and in 1 exoU+/exoS+ isolate. Thus, 11 ST235/CC235 isolates were detected in 38 exoU+ isolates (28.9%), resulting in an overall ST235/CC235 frequency of 20.8% in 53 isolates with the exoU+ genotype and/or carbapenem resistance that were typed by MLST. In contrast, ST235/CC235 isolates were not found in 15 exoU+/exoS− isolates resistant to carbapenems. The CC235 has been linked with metallo-β-lactamase genes and, hence, is responsible for their dissemination worldwide, including to Japan (4, 30). Our findings provide important insights into the role of companion animals as the potential reservoirs of P. aeruginosa high-risk clones, although they did not harbor metallo-β-lactamase genes.
In P. aeruginosa, mutational overexpression of a multidrug efflux pump, MexAB-OprM, leads to reduced susceptibility to fluoroquinolones and most β-lactams, including meropenem, while imipenem is not affected (31). MexAB-OprM overexpression combined with OprD inactivation produces high-level meropenem resistance (MIC, >32 mg/liter) (32). Mutational inactivation of OprD contributes mainly to imipenem resistance, even achieving high-level resistance (MIC, >32 mg/liter), but drives only moderate resistance to meropenem (32). In addition, OprD inactivation, in combination with AmpC β-lactamase overexpression, confers resistance to carbapenems (33). In the present study, 7.1% (17/240) of isolates from companion animals were found to be carbapenem resistant but carbapenemase non-IMP producers. MIC assays performed in the presence of an efflux pump inhibitor PAβN and/or AmpC β-lactamase inhibitor APB revealed the contribution of AmpC β-lactamase production to imipenem resistance in 10 of 12 imipenem-resistant meropenem-susceptible isolates. In the remaining 2 isolates, the active role of efflux pumps (isolate 8) or the synergistic role of AmpC β-lactamase production and efflux pumps (isolate 2, imipenem MIC of 64 μg/ml) in mediating imipenem resistance is estimated. Among 4 imipenem- and meropenem-resistant isolates, AmpC β-lactamase-mediated imipenem resistance is considered in 3 isolates, including 1 also exhibiting efflux pump-mediated meropenem resistance (isolate 13, imipenem MIC of 32 mg/liter, meropenem MIC of 8 mg/liter). The involvement of the synergistic effect of AmpC β-lactamase production and efflux pumps in imipenem resistance and that of the efflux pump mechanism in meropenem resistance could be considered in the remaining 1 isolate (isolate 10, imipenem MIC of 128 mg/ml, meropenem MIC of 16 mg/liter). Efflux pump-mediated meropenem resistance is suggested for a meropenem-resistant imipenem-susceptible isolate.
Representative isolates analyzed by WGS contained defective oprD mutations in ST348/O2 (isolate 10) and ST235/O11 (isolate 13), while 3 amino acid substitutions observed in ST1600/O3 (isolate 2) may not be involved in carbapenem resistance because they have been frequently detected among carbapenem-susceptible isolates, including P. aeruginosa PA14 (34). Also, substitutions in regulators of AmpC β-lactamases (PDC variants) are found in these isolates, i.e., AmpR (Gly283Glu and Met288Arg), AmpD (Gly148Ala and Asp183Tyr), and AmpDh3 (Ala208Val and Ala219Thr), which have frequently been identified in wild-type isolates and P. aeruginosa PA14, and are considered nonsignificant (35, 36). All substitutions in MexAB-OprM regulators, namely, Arg21His and Asp56Gly in NfxB repressor of MexCD-OprJ and Asp249Asn in MexS repressor of the MexEF-OprN, have been found in susceptible isolates, including P. aeruginosa PA14, and thus may not be related to the overexpression of those efflux pumps (37–39). In consequence, carbapenem resistance may arise from AmpC derepression due to Ser5Phe in AmpD and/or Ile67Thr in AmpDh3 (40) combined with MexCD-OprJ overexpression due to Gly133Ser in NfxB in the ST1600/O3 isolate. A significant association between MexCD-OprJ overexpression and meropenem and imipenem resistance has been described (41). Carbapenem resistance in ST348/O2 and ST235/O11 isolates may be attributed to mutational inactivation of OprD combined with MexEF-OprN overexpression due to Gly78Ser or a frameshift mutation in MexS (39). MexEF-OprN overexpression, with a concomitant loss of OprD caused by mutated MexS, has been linked to carbapenem resistance (42). Besides, the involvement of AmpC (PDC) variants in decreased imipenem susceptibility cannot be excluded (43).
In conclusion, this study confirms the presence of high-risk clones in canine and feline isolates with the exoU+ genotype; ST235/CC235 isolates were the most predominant, followed by ST357 isolates. These animal isolates belonging to high-risk clones were found to be carbapenemase nonproducers, although international high-risk clones have been associated frequently with carbapenemase production. Nonetheless, the predominant occurrence of ST235 among companion animals may represent a threat to public health because of the ability of this clone to acquire and spread resistance elements, including carbapenemase genes. A comprehensive survey of P. aeruginosa needs to be conducted to better understand the spread of antimicrobial resistance elements, STs, and T3SS virulotypes at the human-animal-environment interface and to assess their clinical implications on humans and animals.
MATERIALS AND METHODS
Bacterial strains.
A total of 240 nonduplicate clinical isolates of P. aeruginosa from dogs (n = 206) and cats (n = 34) were collected from 152 primary care animal hospitals across Japan between August 2017 and October 2019. Those isolates were received from different geographic regions, as follows: Kanto (n = 117 from 71 hospitals), Chubu (n = 32 from 25 hospitals), Kinki (n = 24 from 19 hospitals), Chugoku (n = 21 from 11 hospitals), Tohoku (n = 19 from 9 hospitals), Kyushu (n = 13 from 10 hospitals), Hokkaido (n = 9 from 4 hospitals), and Shikoku (n = 5 from 3 hospitals). Clinical sources of the isolates were ear (n = 149), urine (n = 33), skin (n = 28), nasal cavity (n = 16), uterus (n = 3), cornea (n = 2), and others (n = 9, including 3 isolates of unknown origin). P. aeruginosa was confirmed with matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) (Bruker Daltonics Japan, Yokohama, Japan) using ≥2.000 score cutoffs for species-level identification.
Antimicrobial susceptibility testing.
MICs were determined by the broth microdilution method recommended by the CLSI using a custom-designed microtiter panel (Kyokuto Optopanel MP; Kyokuto Pharmaceutical, Tokyo, Japan), and the results were interpreted according to CLSI M100 30th edition guidelines for human (26). Escherichia coli ATCC 25922 and P. aeruginosa ATCC 27853 were used as quality-control strains.
Detection of T3SS virulence genes (exoU and exoS).
All isolates were subjected to PCR detection of T3SS effector toxin genes exoU and exoS using specific primers as shown in Table 6 (44, 45). The amplification products from some arbitrarily selected isolates were sequenced to confirm the reliability of the results.
TABLE 6.
Primers used for PCR amplification in this study
| Gene by type | Primer sequencea (5′ to 3′) | Amplicon size (bp) |
|---|---|---|
| T3SS virulence genes | ||
| exoU | F; ATGCATATCCAATCGTTG | 2,000 |
| R; TCATGTGAACTCCTTATT | ||
| exoS | F; CTTGAAGGGACTCGACAAGG | 504 |
| R; TTCAGGTCCGCGTAGTGAAT | ||
| Carbapenemase genes | ||
| bla IMP | F; ACCGCAGCAGAGTCTTTGCC | 587 |
| R; ACAACCAGTTTTGCCTTACC | ||
| bla NDM | F; GGGCCGTATGAGTGA | 758 |
| R; GAAGCTGAGCACCGCATTAG | ||
| bla VIM | F; ATGTTCAAACTTTTGAGTAAG | 801 |
| R; CTACTCAACGACTGAGCG | ||
| bla GES | F; ATGCGCTTCATTCACGCAC | 864 |
| R; CTATTTGTCCGTGCTCAGGA | ||
| MLST | ||
| acsA | F; ACCTGGTGTACGCCTCGCTGAC | 842 |
| R; GACATAGATGCCCTGCCCCTTGAT | ||
| aroE | F; TGGGGCTATGACTGGAAACC | 825 |
| R; TAACCCGGTTTTGTGATTCCTACA | ||
| guaA | F; CGGCCTCGACGTGTGGATGA | 940 |
| R; GAACGCCTGGCTGGTCTTGTGGTA | ||
| nuoD | F; ACCGCCACCCGTACTG | 1,042 |
| R; TCTCGCCCATCTTGACCA | ||
| ppsA | F; GGTCGCTCGGTCAAGGTAGTGG | 989 |
| R; GGGTTCTCTTCTTCCGGCTCGTAG | ||
| trpE | F; GCGGCCCAGGGTCGTGAG | 811 |
| R; CCCGGCGCTTGTTGATGGTT | ||
| mutL | F; AGGTTCGCGACCTGTTCTT | 688 |
| R; GGACTCTCCAGCACGCTCT |
F, forward primer; R, reverse primer.
Analysis of carbapenem-resistant P. aeruginosa isolates.
Detection of carbapenemase activity in P. aeruginosa isolates exhibiting resistance to imipenem and/or meropenem was performed using the modified carbapenem inactivation method CIMTris (46). Carbapenemase genes (blaIMP, blaNDM, blaVIM, and blaGES) were detected by PCR assay using specific primers as shown in Table 6.
The imipenem and meropenem MICs were determined using microdilution panels prepared in-house in the absence and in the presence of 20- or 40-mg/liter efflux pump inhibitor PaβN (MP Biomedicals, Santa Ana, CA), 20- or 40-mg/liter PAβN plus 300-mg/liter APB (Sigma-Aldrich Japan, Tokyo, Japan), and 300-mg/liter APB in parallel. P. aeruginosa ATCC 27853 was used as the control strain. MIC reduction (4-fold or greater) in the presence of PaβN and/or APB was considered the participation of efflux pump and/or AmpC β-lactamase in the resistance to those carbapenems.
MLST analysis.
MLST for carbapenem-resistant isolates and exoU+ isolates was performed according to the MLST scheme described by Curran et al. except that Tks Gflex DNA polymerase (TaKaRa Bio, Otsu, Japan) and alternative PCR primers for mutL shown in Table 6 were used (47, 48). Briefly, seven housekeeping genes (acsA, aroE, guaA, mutL, nuoD, ppsA, and trpE) were amplified and sequenced. Those sequences were submitted to the PubMLST database (https://pubmlst.org/organisms/pseudomonas-aeruginosa) for the assignment of allelic numbers and STs. Those STs were assigned to clonal complexes, as defined by closely related ST groups within the single-locus variant or double-locus variant linkages (49).
WGS analysis of high-level imipenem-resistant P. aeruginosa.
WGS and de novo assembly of three representative carbapenem-resistant isolates were conducted in a manner like that described previously (50). Briefly, the genome was sequenced using the 150-bp paired-end method with the NovaSeq6000 platform (Illumina, San Diego, CA), and the resulting raw reads were assembled de novo into scaffolds using the SPAdes v.3.14.1. The assembled scaffolds were queried with ResFinder 4.1 and PAst 1.0 that are available from the Center for Genomic Epidemiology (http://www.genomicepidemiology.org) for the prediction of antibiotic resistance genes and in silico serotyping, respectively. A wgMLST tree was constructed using PGAdb-builder (http://wgmlstdb.imst.nsysu.edu.tw), with the addition of the genomes of 21 P. aeruginosa strains belonging to ST235-O11 obtained from the NCBI database (Table 7). The phylogenetic tree was visualized using iTOL v5 (http://itol.embl.de/). An in-depth exploration of heavy metal resistance and virulence genes was performed manually on WGS data.
TABLE 7.
List of 21 ST235/O11 P. aeruginosa reference genomes included in the wgMLST
| Strain | Isolation source | Country | GenBank assembly accession no. |
|---|---|---|---|
| ST235 | Homo sapiens | Italy | GCA_011634585.1 |
| UNIBA_ST235PA | Blood | Italy | GCA_013276295.1 |
| TRN6637 | Homo sapiens | Russia | GCA_001921165.1 |
| PA_ST235 | Blood | Spain | GCA_000737795.1 |
| MAL | Homo sapiens | France | GCA_901035125.1 |
| 24Pae112 | Blood | Colombia | GCA_003433235.1 |
| WH-SGI-V-07626 | Homo sapiens | USA | GCA_001452025.1 |
| RNS_PA46 | Burn wound | Australia | GCA_001623955.1 |
| RNS_PAE05 | Hand sanitizer | Australia | GCA_001623985.1 |
| TRN6594 | Homo sapiens | Argentina | GCA_001921015.1 |
| TRN6598 | Homo sapiens | South Africa | GCA_001921025.1 |
| TRN6622 | Homo sapiens | Thailand | GCA_001921095.1 |
| TRN6635 | Homo sapiens | Russia | GCA_001921125.1 |
| TRN6649 | Homo sapiens | Nigeria | GCA_001921175.1 |
| NCGM 1900 | Homo sapiens | Japan | GCA_000829275.1 |
| AZPAE13880 | Homo sapiens | Mexico | GCA_000795725.1 |
| AZPAE14887 | Intra-abdominal tract infection | Croatia | GCA_000790725.1 |
| AZPAE14690 | Urinary tract infection | Romania | GCA_000794555.1 |
| AZPAE14702 | Respiratory tract infection | Philippines | GCA_000794785.1 |
| AZPAE14705 | Urinary tract infection | Greece | GCA_000795805.1 |
| AZPAE15063 | Respiratory tract infection | Brazil | GCA_000793315.1 |
The nucleotide sequences of AmpC β-lactamase regulator genes (ampR, ampD, ampDh2, and ampDh3); oprD porin genes; efflux system regulator genes (mexR, nalC, nalD, mexZ, nfxB, mexS, and mexT); and QRDR of gyrA, gyrB, parC, and parE genes were compared with those of the reference strain P. aeruginosa PAO1 (GenBank accession number AE004091).
Analysis of ciprofloxacin-resistant P. aeruginosa isolates.
Efflux pump-mediated fluoroquinolone resistance was investigated in ciprofloxacin-resistant isolates using efflux pump inhibitor PAβN as described above. A decrease of more than 4-fold in MIC in the presence of PAβN was considered the participation of efflux pumps in the resistance to ciprofloxacin.
Statistical analysis.
The Fisher’s exact test was performed to assess the association between T3SS virulotypes (exoU+/exoS− and exoU−exoS+) and antimicrobial resistance by using R v4.0.5. Resistant and intermediate isolates were grouped as resistant for statistical analyses. P value of ≤0.05 were considered statistically significant.
Data availability.
Genome assemblies for P. aeruginosa isolates no. 2 (CA12133), 10 (CA17343), and 13 (CA19603) have been deposited in the DDBJ/EMBL/GenBank database under the GenBank assembly accession numbers GCA_015704805.1, GCA_014596255.1, and GCA_014596275.1, and the BioProject accession number PRJNA648803.
ACKNOWLEDGMENTS
This work was supported by JSPS KAKENHI grant no. JP18K08428.
We declare no conflicts of interest.
Footnotes
Supplemental material is available online only.
Contributor Information
Noriyuki Nagano, Email: naganon@shinshu-u.ac.jp.
Ayush Kumar, University of Manitoba.
REFERENCES
- 1.Gellatly SL, Hancock RE. 2013. Pseudomonas aeruginosa: new insights into pathogenesis and host defenses. Pathog Dis 67:159–173. doi: 10.1111/2049-632X.12033. [DOI] [PubMed] [Google Scholar]
- 2.Del Barrio-Tofiño E, López-Causapé C, Oliver A. 2020. Pseudomonas aeruginosa epidemic high-risk clones and their association with horizontally-acquired β-lactamases: 2020 update. Int J Antimicrob Agents 56:106196. doi: 10.1016/j.ijantimicag.2020.106196. [DOI] [PubMed] [Google Scholar]
- 3.Sekiguchi J, Asagi T, Miyoshi-Akiyama T, Kasai A, Mizuguchi Y, Araake M, Fujino T, Kikuchi H, Sasaki S, Watari H, Kojima T, Miki H, Kanemitsu K, Kunishima H, Kikuchi Y, Kaku M, Yoshikura H, Kuratsuji T, Kirikae T. 2007. Outbreaks of multidrug-resistant Pseudomonas aeruginosa in community hospitals in Japan. J Clin Microbiol 45:979–989. doi: 10.1128/JCM.01772-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hishinuma T, Tada T, Kuwahara-Arai K, Yamamoto N, Shimojima M, Kirikae T. 2018. Spread of GES-5 carbapenemase-producing Pseudomonas aeruginosa clinical isolates in Japan due to clonal expansion of ST235. PLoS One 13:e0207134. doi: 10.1371/journal.pone.0207134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galle M, Carpentier I, Beyaert R. 2012. Structure and function of the type III secretion system of Pseudomonas aeruginosa. Curr Protein Pept Sci 13:831–842. doi: 10.2174/138920312804871210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hauser AR. 2009. The type III secretion system of Pseudomonas aeruginosa: infection by injection. Nat Rev Microbiol 7:654–665. doi: 10.1038/nrmicro2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sawa T, Shimizu M, Moriyama K, Wiener-Kronish JP. 2014. Association between Pseudomonas aeruginosa type III secretion, antibiotic resistance, and clinical outcome: a review. Crit Care 18:668. doi: 10.1186/s13054-014-0668-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleiszig SM, Wiener-Kronish JP, Miyazaki H, Vallas V, Mostov KE, Kanada D, Sawa T, Yen TS, Frank DW. 1997. Pseudomonas aeruginosa-mediated cytotoxicity and invasion correlate with distinct genotypes at the loci encoding exoenzyme S. Infect Immun 65:579–586. doi: 10.1128/iai.65.2.579-586.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Juan C, Peña C, Oliver A. 2017. Host and pathogen biomarkers for severe Pseudomonas aeruginosa infections. J Infect Dis 215:S44–S51. doi: 10.1093/infdis/jiw299. [DOI] [PubMed] [Google Scholar]
- 10.Subedi D, Vijay AK, Kohli GS, Rice SA, Willcox M. 2018. Association between possession of ExoU and antibiotic resistance in Pseudomonas aeruginosa. PLoS One 13:e0204936. doi: 10.1371/journal.pone.0204936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peña C, Cabot G, Gómez-Zorrilla S, Zamorano L, Ocampo-Sosa A, Murillas J, Almirante B, Pomar V, Aguilar M, Granados A, Calbo E, Rodríguez-Baño J, Rodríguez-López F, Tubau F, Martínez-Martínez L, Oliver A, Spanish Network for Research in Infectious Diseases (REIPI) . 2015. Influence of virulence genotype and resistance profile in the mortality of Pseudomonas aeruginosa bloodstream infections. Clin Infect Dis 60:539–548. doi: 10.1093/cid/ciu866. [DOI] [PubMed] [Google Scholar]
- 12.Recio R, Mancheño M, Viedma E, Villa J, Orellana MÁ, Lora-Tamayo J, Chaves F. 2020. Predictors of mortality in bloodstream infections caused by Pseudomonas aeruginosa and impact of antimicrobial resistance and bacterial virulence. Antimicrob Agents Chemother 64:e01759-19. doi: 10.1128/AAC.01759-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maeyama Y, Taniguchi Y, Hayashi W, Ohsaki Y, Osaka S, Koide S, Tamai K, Nagano Y, Arakawa Y, Nagano N. 2018. Prevalence of ESBL/AmpC genes and specific clones among the third-generation cephalosporin-resistant Enterobacteriaceae from canine and feline clinical specimens in Japan. Vet Microbiol 216:183–189. doi: 10.1016/j.vetmic.2018.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Taniguchi Y, Koide S, Maeyama Y, Tamai K, Hayashi W, Tanaka H, Iimura M, Suzuki M, Nagano Y, Arakawa Y, Nagano N. 2020. Predominance of methicillin-resistant Staphylococcus aureus SCCmec type II-CC5 and SCCmec type IV-CC1/CC8 among companion animal clinical isolates in Japan: findings from phylogenetic comparison with human clinical isolates. J Glob Antimicrob Resist 20:253–259. doi: 10.1016/j.jgar.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Haenni M, Bour M, Châtre P, Madec JY, Plésiat P, Jeannot K. 2017. Resistance of animal strains of Pseudomonas aeruginosa to carbapenems. Front Microbiol 8:1847. doi: 10.3389/fmicb.2017.01847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandes MR, Sellera FP, Moura Q, Carvalho MPN, Rosato PN, Cerdeira L, Lincopan N. 2018. Zooanthroponotic transmission of drug-resistant Pseudomonas aeruginosa, Brazil. Emerg Infect Dis 24:1160–1162. doi: 10.3201/eid2406.180335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Wang X, Schwarz S, Zhang R, Lei L, Liu X, Lin D, Shen J. 2014. IMP-45-producing multidrug-resistant Pseudomonas aeruginosa of canine origin. J Antimicrob Chemother 69:2579–2581. doi: 10.1093/jac/dku133. [DOI] [PubMed] [Google Scholar]
- 18.Ledbetter EC, Mun JJ, Kowbel D, Fleiszig SM. 2009. Pathogenic phenotype and genotype of Pseudomonas aeruginosa isolates from spontaneous canine ocular infections. Invest Ophthalmol Vis Sci 50:729–736. doi: 10.1167/iovs.08-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harada K, Arima S, Niina A, Kataoka Y, Takahashi T. 2012. Characterization of Pseudomonas aeruginosa isolates from dogs and cats in Japan: current status of antimicrobial resistance and prevailing resistance mechanisms. Microbiol Immunol 56:123–127. doi: 10.1111/j.1348-0421.2011.00416.x. [DOI] [PubMed] [Google Scholar]
- 20.Yukawa S, Tsuyuki Y, Sato T, Fukuda A, Usui M, Tamura Y. 2017. Antimicrobial resistance of Pseudomonas aeruginosa isolated from dogs and cats in primary veterinary hospitals in Japan. Jpn J Infect Dis 70:461–463. doi: 10.7883/yoken.JJID.2016.536. [DOI] [PubMed] [Google Scholar]
- 21.Chávez-Jacobo VM, Hernández-Ramírez KC, Romo-Rodríguez P, Pérez-Gallardo RV, Campos-García J, Gutiérrez-Corona JF, García-Merinos JP, Meza-Carmen V, Silva-Sánchez J, Ramírez-Díaz MI. 2018. CrpP is a novel ciprofloxacin-modifying enzyme encoded by the Pseudomonas aeruginosa pUM505 plasmid. Antimicrob Agents Chemother 62:e02629-17. doi: 10.1128/AAC.02629-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCarthy KL, Wailan AM, Jennison AV, Kidd TJ, Paterson DL. 2018. P aeruginosa blood stream infection isolates: a “full house” of virulence genes in isolates associated with rapid patient death and patient survival. Microb Pathog 119:81–85. doi: 10.1016/j.micpath.2018.03.062. [DOI] [PubMed] [Google Scholar]
- 23.Sauvage S, Hardouin J. 2020. Exoproteomics for better understanding Pseudomonas aeruginosa virulence. Toxins (Basel) 12:571. doi: 10.3390/toxins12090571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wettstadt S, Wood TE, Fecht S, Filloux A. 2019. Delivery of the Pseudomonas aeruginosa phospholipase effectors PldA and PldB in a VgrG- and H2-T6SS-dependent manner. Front Microbiol 10:1718. doi: 10.3389/fmicb.2019.01718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Redfern J, Wallace J, van Belkum A, Jaillard M, Whittard E, Ragupathy R, Verran J, Kelly P, Enright MC. 2021. Biofilm associated genotypes of multiple antibiotic resistant Pseudomonas aeruginosa. BMC Genomics 22:572. doi: 10.1186/s12864-021-07818-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clinical and Laboratory Standards Institute. 2020. Performance standards for antimicrobial susceptibility testing. CLSI document M100-Ed30. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 27.Rutherford V, Yom K, Ozer EA, Pura O, Hughes A, Murphy KR, Cudzilo L, Mitchell D, Hauser AR. 2018. Environmental reservoirs for exoS+ and exoU+ strains of Pseudomonas aeruginosa. Environ Microbiol Rep 10:485–492. doi: 10.1111/1758-2229.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agnello M, Wong-Beringer A. 2012. Differentiation in quinolone resistance by virulence genotype in Pseudomonas aeruginosa. PLoS One 7:e42973. doi: 10.1371/journal.pone.0042973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Recio R, Villa J, Viedma E, Orellana MÁ, Lora-Tamayo J, Chaves F. 2018. Bacteraemia due to extensively drug-resistant Pseudomonas aeruginosa sequence type 235 high-risk clone: facing the perfect storm. Int J Antimicrob Agents 52:172–179. doi: 10.1016/j.ijantimicag.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 30.Edelstein MV, Skleenova EN, Shevchenko OV, D'souza JW, Tapalski DV, Azizov IS, Sukhorukova MV, Pavlukov RA, Kozlov RS, Toleman MA, Walsh TR. 2013. Spread of extensively resistant VIM-2-positive ST235 Pseudomonas aeruginosa in Belarus, Kazakhstan, and Russia: a longitudinal epidemiological and clinical study. Lancet Infect Dis 13:867–876. doi: 10.1016/S1473-3099(13)70168-3. [DOI] [PubMed] [Google Scholar]
- 31.Horcajada JP, Montero M, Oliver A, Sorlí L, Luque S, Gómez-Zorrilla S, Benito N, Grau S. 2019. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa infections. Clin Microbiol Rev 32:e00031-19. doi: 10.1128/CMR.00031-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riera E, Cabot G, Mulet X, García-Castillo M, del Campo R, Juan C, Cantón R, Oliver A. 2011. Pseudomonas aeruginosa carbapenem resistance mechanisms in Spain: impact on the activity of imipenem, meropenem and doripenem. J Antimicrob Chemother 66:2022–2027. doi: 10.1093/jac/dkr232. [DOI] [PubMed] [Google Scholar]
- 33.Quale J, Bratu S, Gupta J, Landman D. 2006. Interplay of efflux system, ampC, and oprD expression in carbapenem resistance of Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother 50:1633–1641. doi: 10.1128/AAC.50.5.1633-1641.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ocampo-Sosa AA, Cabot G, Rodríguez C, Roman E, Tubau F, Macia MD, Moya B, Zamorano L, Suárez C, Peña C, Domínguez MA, Moncalián G, Oliver A, Martínez-Martínez L, Spanish Network for Research in Infectious Diseases (REIPI) . 2012. Alterations of OprD in carbapenem-intermediate and -susceptible strains of Pseudomonas aeruginosa isolated from patients with bacteremia in a Spanish multicenter study. Antimicrob Agents Chemother 56:1703–1713. doi: 10.1128/AAC.05451-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cabot G, Ocampo-Sosa AA, Domínguez MA, Gago JF, Juan C, Tubau F, Rodríguez C, Moyà B, Peña C, Martínez-Martínez L, Oliver A, Spanish Network for Research in Infectious Diseases (REIPI) . 2012. Genetic markers of widespread extensively drug-resistant Pseudomonas aeruginosa high-risk clones. Antimicrob Agents Chemother 56:6349–6357. doi: 10.1128/AAC.01388-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moya B, Juan C, Albertí S, Pérez JL, Oliver A. 2008. Benefit of having multiple ampD genes for acquiring β-lactam resistance without losing fitness and virulence in Pseudomonas aeruginosa. Antimicrob Agents Chemother 52:3694–3700. doi: 10.1128/AAC.00172-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jeannot K, Elsen S, Köhler T, Attree I, van Delden C, Plésiat P. 2008. Resistance and virulence of Pseudomonas aeruginosa clinical strains overproducing the MexCD-OprJ efflux pump. Antimicrob Agents Chemother 52:2455–2462. doi: 10.1128/AAC.01107-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Llanes C, Hocquet D, Vogne C, Benali-Baitich D, Neuwirth C, Plésiat P. 2004. Clinical strains of Pseudomonas aeruginosa overproducing MexAB-OprM and MexXY efflux pumps simultaneously. Antimicrob Agents Chemother 48:1797–1802. doi: 10.1128/AAC.48.5.1797-1802.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Llanes C, Köhler T, Patry I, Dehecq B, van Delden C, Plésiat P. 2011. Role of the MexEF-OprN efflux system in low-level resistance of Pseudomonas aeruginosa to ciprofloxacin. Antimicrob Agents Chemother 55:5676–5684. doi: 10.1128/AAC.00101-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmidtke AJ, Hanson ND. 2008. Role of ampD homologs in overproduction of AmpC in clinical isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother 52:3922–3927. doi: 10.1128/AAC.00341-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hassuna NA, Darwish MK, Sayed M, Ibrahem RA. 2020. Molecular emidemiology and mechanisms of high-level resistance to meropenem and imipenem in Pseudomonas aeruginosa. Infect Drug Resist 13:285–293. doi: 10.2147/IDR.S233808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Köhler T, Epp SF, Curty LK, Pechère JC. 1999. Characterization of MexT, the regulator of the MexE-MexF-OprN multidrug efflux system of Pseudomonas aeruginosa. J Bacteriol 181:6300–6305. doi: 10.1128/JB.181.20.6300-6305.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rodríguez-Martínez JM, Poirel L, Nordmann P. 2009. Extended-spectrum cephalosporinases in Pseudomonas aeruginosa. Antimicrob Agents Chemother 53:1766–1771. doi: 10.1128/AAC.01410-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lanotte P, Watt S, Mereghetti L, Dartiguelongue N, Rastegar-Lari A, Goudeau A, Quentin R. 2004. Genetic features of Pseudomonas aeruginosa isolates from cystic fibrosis patients compared with those of isolates from other origins. J Med Microbiol 53:73–81. doi: 10.1099/jmm.0.05324-0. [DOI] [PubMed] [Google Scholar]
- 45.Petit SM, Lavenir R, Colinon-Dupuich C, Boukerb AM, Cholley P, Bertrand X, Freney J, Doléans-Jordheim A, Nazaret S, Laurent F, Cournoyer B. 2013. Lagooning of wastewaters favors dissemination of clinically relevant Pseudomonas aeruginosa. Res Microbiol 164:856–866. doi: 10.1016/j.resmic.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 46.Uechi K, Tada T, Shimada K, Kuwahara-Arai K, Arakaki M, Tome T, Nakasone I, Maeda S, Kirikae T, Fujita J. 2017. A modified carbapenem inactivation method, CIMTris, for carbapenemase production in Acinetobacter and Pseudomonas species. J Clin Microbiol 55:3405–3410. doi: 10.1128/JCM.00893-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Curran B, Jonas D, Grundmann H, Pitt T, Dowson CG. 2004. Development of a multilocus sequence typing scheme for the opportunistic pathogen Pseudomonas aeruginosa. J Clin Microbiol 42:5644–5649. doi: 10.1128/JCM.42.12.5644-5649.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khuntayaporn P, Yamprayoonswat W, Yasawong M, Chomnawang MT. 2019. Dissemination of carbapenem-resistance among multidrug resistant Pseudomonas aeruginosa carrying metallo-β-lactamase genes, including the novel blaIMP-65 gene in Thailand. Infect Chemother 51:107–118. doi: 10.3947/ic.2019.51.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Francisco AP, Vaz C, Monteiro PT, Melo-Cristino J, Ramirez M, Carriço JA. 2012. PHYLOViZ: phylogenetic inference and data visualization for sequence based typing methods. BMC Bioinformatics 13:87. doi: 10.1186/1471-2105-13-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hayashi W, Yoshida S, Izumi K, Koide S, Soga E, Takizawa S, Arakawa Y, Nagano Y, Nagano N. 2021. Genomic characterisation and epidemiology of nosocomial Serratia marcescens isolates resistant to ceftazidime and their plasmids mediating rare blaTEM-61. J Glob Antimicrob Resist 25:124–131. doi: 10.1016/j.jgar.2021.03.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material. Download SPECTRUM00408-21_Supp_1_seq10.xlsx, XLSX file, 0.1 MB (34.1KB, xlsx)
Data Availability Statement
Genome assemblies for P. aeruginosa isolates no. 2 (CA12133), 10 (CA17343), and 13 (CA19603) have been deposited in the DDBJ/EMBL/GenBank database under the GenBank assembly accession numbers GCA_015704805.1, GCA_014596255.1, and GCA_014596275.1, and the BioProject accession number PRJNA648803.