Abstract
Background The COVID-19 pandemic has raised concerns regarding its psychological effect on university students, especially healthcare students. We aimed at assessing the risk of mental health problems according to the type of university studies, by adjusting for potential confounders. Methods We used data from the COSAMe study, a national cross-sectional survey including 69,054 French university students during the first quarantine. The mental health outcomes evaluated were suicidal thoughts, severe self-reported distress (as assessed by the Impact of Events Scale–Revised), stress (Perceived Stress Scale), anxiety (State-Trait Anxiety Inventory, State subscale), and depression (Beck Depression Inventory). Multivariable logistic regression analyzes were performed to test the association between the type of university studies (healthcare studies: medical and non-medical, and non-healthcare studies) and poor mental health outcomes, adjusted for sociodemographic characteristics, precariousness indicators, health-related data, quality of social relationships, and data about media consumption. Results Compared to non-healthcare students (N = 59,404), non-medical healthcare (N = 5,431) and medical students (N = 4,193) showed a lower risk of presenting at least one poor mental health outcome (adjusted OR [95%CI] = 0.86[0.81–0.92] and 0.87[0.81–0.93], respectively). Compared to non-healthcare students, medical students were at lower risk of suicidal thoughts (0.83[0.74–0.93]), severe self-reported distress (0.75[0.69–0.82]) and depression (0.83[0.75–0.92]). Non-medical healthcare students were at lower risk of severe selfreported distress (0.79[0.73–0.85]), stress (0.92[0.85–0.98]), depression (0.83[0.76–0.91]), and anxiety (0.86[0.80–0.92]). Limitations This is a large but not representative cross-sectional study, limited to the first confinement. Conclusions Being a healthcare student is a protective factor for mental health problems among confined students. Mediating factors still need to be explored.
Keywords: COVID-19, Healthcare students, Anxiety, Depression, Medical students
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic and quarantine have raised concerns regarding their negative psychological effects on populations (Brooks et al., 2020). These worries were rapidly confirmed (Wang et al., 2020), especially among university students, whose vulnerability to mental health difficulties is well established (Ibrahim et al., 2013). For instance, the nationwide COSAMe study found high prevalence rates of self-reported suicidal thoughts, distress, depression, anxiety, and stress, among 69,054 French students surveyed during the first COVID-19 lockdown (Wathelet et al., 2020).
Notably, specific concerns have been raised about healthcare students, considered as particularly vulnerable to mental health disorders, due to several stressors such as heavy academic and clinical workload, examinations, competition, difficulties in combining personal and professional life, financial burdens, or exposure to human suffering (Dyrbye et al., 2006). Indeed, previous reports found high rates of depression and anxiety in this population (Dyrbye et al., 2006; Gorter et al., 2008; Zhang et al., 2018). A systematic review, published before the COVID-19 outbreak, even estimated at 33.8% the prevalence of anxiety among medical students (Quek et al., 2019).
Surprisingly, a recent systematic review including studies conducted during the COVID-19 pandemic found a lower prevalence rate of anxiety (28%) in medical students than before the pandemic (Lasheras et al., 2020). Two Chinese studies also found that medical students were less likely to suffer from distress, severe anxiety, and depression than non-medical students during the initial stage of the 2019 coronavirus disease (Chang et al., 2020; Xie et al., 2020). However, those two studies compared medical students to non-medical students, grouping together healthcare students (except medical students) and others.
This exploratory study reanalyzed the prevalence rates of self-reported suicidal thoughts, distress, stress, anxiety, and depression obtained by the COSAMe study during the first COVID-19 related lockdown in France. Here, we aimed at comparing medical, non-medical healthcare, and non-healthcare French university students and assessing the risk of mental health problems according to the type of university studies, by adjusting for potential confounders.
2. Methods
2.1. COSAMe study
The study used data from the first time measurement (from April 17 to May 4, 2020) of the repeated cross-sectional university-based COSAMe survey. A total of 69,054 students fully completed the study questionnaire. They were asked to report suicidal thoughts during the previous month, distress resulting from a stressful life event (as assessed by the Impact of Events Scale-Revised – IES-R), perceived stress (Perceived Stress Scale – PSS-10), depression (Beck Depression Inventory – BDI-13), and anxiety (20-item State-Trait Anxiety Inventory, State subscale – STAI Y-2). Outcomes were the presence of severe self-reported symptoms, i.e., suicidal thoughts or a high score (i.e., IES-R score >36; PSS-10 score >26; BDI-13 score >15; or STAI-Y2 score >55) on at least one scale.
Sociodemographic characteristics (gender, year of study, area, being a foreign student, living in a worst hit department), precariousness indicators (loss of income due to quarantine, quality housing), health-related data (history of psychiatric follow-up, physical activity during the quarantine, and having experienced symptoms consistent with COVID-19), social relationship data (feeling socially integrated before the quarantine, having children, housing composition during the quarantine, concern for relatives’ health, and quality of social relationships during the quarantine, regular outings during quarantine due to associative, university or professional activities), and media/information data (consumption of media information related to the pandemic, and quality of information perceived) were also collected.
This survey was examined by a French research ethics committee, the Comité de Protection des Personnes Ile-de France VIII, before its initiation. Oral or written consent was not required for this study because responding to the survey was considered consent to participate.
The CHERRIES checklist, recommended for reporting the results of Internet e-surveys, is available in Supplementary material 1 (Gunther, 2004). Detailed methods (provided in Supplementary material 2) have been published elsewhere (Wathelet et al., 2020).
2.2. University studies
To explore prevalence rates according to the type of university studies, respondents were classified into 3 categories: medical students, non-medical healthcare students (i.e., nursing, pharmacy, dental, physiotherapy, midwifery, speech-therapist and psychologist students, as well as future physical educators, nutritionists, biomedicals, and nursing assistants), and non-healthcare students (all students who did not match the previous categories were considered as non-healthcare students).
In France, the PACES (the first common core year for health studies) is common for four specializations: medicine, pharmacy, dentistry, and midwifery. The PACES consists of a common component for all students, and a specialized component chosen by the student. PACES students who specified their specialization were assigned to the corresponding group: medical students for "medicine" and non-medical healthcare students for "pharmacy", "dentistry", and "midwifery". When there was no indication of the specialization, the medical studies being the most popular, the students were assigned to the medical students' group.
2.3. Statistical analysis
We described the sample using numbers and percentages. Chi-2 tests were realized to compare sample characteristics and mental health outcome distributions according to the type of university studies (medical, non-medical healthcare, and non-healthcare studies).
Multivariable logistic regression analyzes were performed to assess the association between the type of university studies and having at least one poor mental health outcome. Similar analyzes were performed for each mental health outcome, i.e., self-reported suicidal thoughts and severe self-reported symptoms of distress, stress, depression, and anxiety. Subgroup analyzes by year of study (1st year, 2nd or 3rd year, 4th year and above) were also performed. All explanatory variables were included. Associations between the type of university studies and mental health outcomes are presented as adjusted odds ratios (aORs) and 95% confidence intervals (CI).
Data analysis was performed using R version 3.6.1 (R Project for Statistical Computing). The significance level was set at α = 0.05, and all tests were 2-tailed.
3. Results
3.1. Sample characteristics
A total of 69,028 students were analyzed (26 students were excluded because no information regarding the type of university studies was available). There were 4193 medical students, 5431 non-medical healthcare students, and 59,404 non-healthcare students.
The distribution of the variables significantly differed depending on the type of studies (Supplementary Table 1). Notably, medical students were mostly in their first year of study (67.1% vs 44.2% and 45.8% for other non-medical healthcare and non-healthcare students, respectively, p < 0.001). They were less likely to report a loss of income (13.1% vs 22.3% and 22.5%, p < 0.001), to declare a history of psychiatry follow-up (8.2% vs 14.8% and 10.0%, p < 0.001) and to have experienced symptoms consistent with COVID-19 (20.4% vs 24.7% and 23.6%, p < 0.001) but more likely to consider living in high-quality housing (86.5% vs 82.5% and 82.0%, p < 0.001). They also considered themselves as better informed (37.8% vs 32.5% and 35.1%, p < 0.001).
3.2. Mental health outcomes
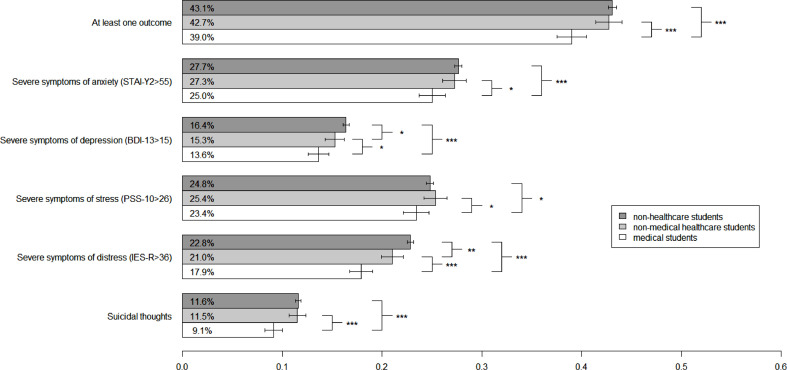
Compared to non-healthcare students and non-medical healthcare students, medical students were less likely to report at least one poor mental health outcome (39.0% vs 42.7%, p < 0.001, compared to other healthcare students, and 39.0% vs 43.1%, p < 0.001, compared to non-healthcare students). No difference was observed between non-medical healthcare students and non-healthcare students (Fig. 1 ).
Fig. 1.
Prevalence rates of mental health outcome according to the type of university studies and results of bivariate analyzes. * = <0.05; ** = <0.01; *** = <0.001.
Prevalence rates of all poor mental health outcomes were significantly lower among medical students compared to other healthcare students and compared to non-healthcare students: 9.1% vs 11.5% (p < 0.001) and 11.6% (p < 0.001) for suicidal thoughts, 17.9% vs 21.0% (p < 0.001) and 22.8% (p < 0.001) for severe distress, 23.4% vs 25.4% (p = 0.029) and 24.8% (p = 0.049) for severe stress, 13.6% vs 15.3% (p = 0.025) and 16.4% (p < 0.001) for severe depression, and 25.0% vs 27.3% (0.015) and 27.7% (p < 0.001) for severe anxiety. Compared to non-healthcare students, non-medical healthcare students were significantly at lower risk of severe self-reported depression (15.3% vs 16.4%, p = 0.035) and distress (21.0% vs 22.8%, p = 0.003).
After adjustment, compared to non-healthcare students, non-medical healthcare and medical students were significantly at lower risk of presenting at least one poor mental health outcome (adjusted OR [95%CI] = 0.86 [0.80–0.91] and 0.87 [0.81–0.93], respectively) (Table 1 ).
Table 1.
Results of multivariate regression models assessing the association between type of university studies and mental health outcomes, in the global sample and according to the year of study.
| Global sample | 1st year | 2nd or 3rd year | 4th year or more | ||
|---|---|---|---|---|---|
| N = 69,028 | N = 32,402 | N = 23,135 | N = 13,491 | ||
| aOR$ [95%CI] | aOR$ [95%CI] | aOR$ [95%CI] | aOR$ [95%CI] | ||
| At least one outcome | Non-healthcare students | 1 [ref] | 1 [ref] | 1 [ref] | 1 [ref] |
| Non-medical healthcare students | 0.86 [0.80–0.91] | 0,96 [0,87–1,05] | 0,79 [0,72–0,88] | 0,75 [0,64–0,89] | |
| Medical students | 0.87 [0.81–0.93] | 0,97 [0,89–1,06] | 0,76 [0,64–0,90] | 0,60 [0,49–0,73] | |
| Suicidal thoughts | Non-healthcare students | 1 [ref] | 1 [ref] | 1 [ref] | 1 [ref] |
| Non-medical healthcare students | 0.93 [0.84–1.02] | 0,94 [0,81–1,08] | 1,00 [0,86–1,16] | 0,73 [0,55–0,96] | |
| Medical students | 0.83 [0.74–0.93] | 0,78 [0,67–0,90] | 0,88 [0,66–1,15] | 1,05 [0,78–1,40] | |
| Severe symptoms of distress (IES-R>36) | Non-healthcare students | 1 [ref] | 1 [ref] | 1 [ref] | 1 [ref] |
| Non-medical healthcare students | 0.79 [0.73–0.85] | 0,94 [0,85–1,05] | 0,69 [0,62–0,78] | 0,61 [0,49–0,74] | |
| Medical students | 0.75 [0.69–0.82] | 0,86 [0,77–0,95] | 0,63 [0,51–0,78] | 0,48 [0,37–0,62] | |
| Severe symptoms of stress (PSS-10>26) | Non-healthcare students | 1 [ref] | 1 [ref] | 1 [ref] | 1 [ref] |
| Non-medical healthcare students | 0.92 [0.85–0.98] | 0,94 [0,84–1,04] | 0,94 [0,84–1,05] | 0,77 [0,64–0,93] | |
| Medical students | 0.99 [0.91–1.07] | 1,15 [1,04–1,26] | 0,76 [0,62–0,93] | 0,59 [0,46–0,74] | |
| Severe symptoms of depression (BDI-13>15) | Non-healthcare students | 1 [ref] | 1 [ref] | 1 [ref] | 1 [ref] |
| Non-medical healthcare students | 0.83 [0.76–0.91] | 0,92 [0,81–1,04] | 0,81 [0,70–0,93] | 0,58 [0,43–0,76] | |
| Medical students | 0.83 [0.75–0.92] | 0,90 [0,80–1,02] | 0,69 [0,53–0,89] | 0,52 [0,37–0,72] | |
| Severe symptoms of anxiety (STAI-Y2>55) | Non-healthcare students | 1 [ref] | 1 [ref] | 1 [ref] | 1 [ref] |
| Non-medical healthcare students | 0.86 [0.80–0.92] | 0,98 [0,88–1,09] | 0,80 [0,72–0,90] | 0,69 [0,57–0,83] | |
| Medical students | 0.93 [0.85–1.00] | 1,09 [0,99–1,20] | 0,69 [0,57–0,84] | 0,60 [0,48–0,76] |
Adjusted for all variables described in Supplementary Table 1.
Compared to non-healthcare students, medical students were significantly at lower risk of suicidal thoughts (0.83 [0.74-0.93]), severe self-reported distress (0.75 [0.69–0.82], and depression (0.83 [0.75–0.92]). There was no significant association with severe anxiety and stress. Compared to non-healthcare students, non-medical healtlcare students were significantly at lower risk of severe self-reported distress (0.79 [0.73–0.85]), stress (0.92 [0.85–0.98]), depression (0.83 [0.76-0.91]), and anxiety (0.86 [0.80–0.92]). There was no significant association with suicidal thoughts.
Similar patterns were found in the subgroup analyzes, except for first year students. Within this sub-group, compared to non-healthcare students, medical students were less at risk of suicidal thoughts and severe self-reported distress (0.78 [0.67–0.90] and 0.86 [0.77–0.95], respectively). However, they were more at risk of severe stress (1.15 [1.04–1.26]). No difference was found between non-medical healthcare students and non-healthcare students.
4. Discussion
This survey study of 69,028 students found high prevalence rates of mental health problems whatever the type of university studies (medical, non-medical healhcare, and non-healthcare studies). Healthcare studies (both medical and non-medical healthcare students) were associated with a lower risk of presenting at least one poor mental health outcome (a 13% and a 14% decrease, respectively, compared to non-healthcare students). Compared to non-healthcare students, medical students were significantly at lower risk of suicidal thoughts, severe self-reported distress, and depression. Compared to non-healthcare students, non-medical healthcare students were significantly at lower risk of severe self-reported distress, stress, depression, and anxiety.
These results are in line with those found by two recent Chinese studies (Chang et al., 2020; Xie et al., 2020). However, unlike these studies, we differentiated non-medical healthcare students from non-healthcare students. Similar results were found in all healthcare students (medical and non-medical), with a reduced risk of reporting a poor mental health outcome in the two samples, compared to other students.
Little is known about the mediating factors, especially among non-medical healthcare students, but a recent study identified that medical students involved in the COVID-19 response reported lower levels of anxiety, depression, and burnout compared with their non-involved peers (Aebischer et al., 2020). These results are in line with studies among healthcare workers suggesting that the pandemic has a stronger psychological impact on non-front-line or non-medical professionals than on front-line healthcare workers (Horn et al., 2021; Hummel et al., 2021). Stress associated with the feeling that quarantine compromised professional prospects, which might be less important among healthcare students, has also been put forward (Le Vigouroux et al., 2021).
If these assumptions can contribute to the explanation of the results for the more advanced students, this is not the case for first year students, as they have no clinical activity, and have not passed the entrance exam yet (Bolatov et al., 2020) suggested that online learning due to the COVID-19 pandemic might have mediated this risk reduction by decreasing the usual exposure to stresss (Dyrbye et al., 2006): decrease of expenses, ability to combine studying with personal life, self-education, and reduction of the clinical placements. However, in the subgroup analyzes, we observed that among first year students, medical studies were associated with a higher risk of stress, which seems to invalidate this hypothesis among the first year students. On the other hand, medical studies were a protective factor against suicidal thoughts and distress, including among first year students. As observed during previous epidemics, Khalid et al. found that psychological distress was associated with lack of knowledge about the COVID-19 (Khalid et al., 2021). In our study, the quality of the information received was evaluated but the level of knowledge, presumed to be higher among healthcare students, was not evaluated and could explain our results. Finally, among medical students, self-efficacy and self-esteem were identified as protective factors for psychological distress (Arima et al., 2020), and higher levels of resilience, observed in both clinical (students in the third year and above) and pre-clinical (students in first and second years) undergraduate medical students, may have promoted adaptive coping strategies facing the pandemic context (van der Merwe et al., 2020). These coping strategies might also explain the results of pre-pandemic studies, which had already observed a higher prevalence of mental health disorders in non-healthcare students than in healthcare students (Honney et al., 2010; Sheokand and Kumar, 2019; Voltmer et al., 2019).
5. Limitations
The following limitations should be considered in the interpretation of these results: (1) a probable self-selection bias, limited by the large number of respondents and the performance of multivariate analyzes to take into account the inter-group differences, (2) the assignment to the group of medical students for PACES students without specifying specialization which may have led to an information bias, (3) the impossibility of establishing a causal link between pandemic context and mental health disorders in a cross-sectional study, but our results are in line with many previous studies, (4) the data collected were declarative, which may have limited the quality of the adjustment for the socio-economic indicators, medical data and quality of information received, and (5) this study is limited to the first confinement, studies confirming this result beyond the first confinement should be carried out.
In conclusion, although we measured high prevalence rates of mental health disorders whatever the type of university studies, being a healthcare student is a protective factor for mental health problems among confined students in the COVID-19 pandemic context, at least during the first quarantine in France. Factors mediating the lower rate of mental health symptoms in health students still need to be explored.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Arnaud Leroy: Writing – original draft. Marielle Wathelet: Conceptualization, Writing – review & editing, Formal analysis, Writing – original draft. Thomas Fovet: . Enguerrand Habran: Formal analysis. Benoît Granon: . Niels Martignène: Formal analysis. Ali Amad: . Charles-Edouard Notredame: . Guillaume Vaiva: Conceptualization, Writing – review & editing. Fabien D'Hondt: Conceptualization.
Declaration of Competing Interest
AL is consultant for Kinnov Therapeutics. All other authors declare that they have no conflicts of interest.
Acknowledgments
We thank the French Ministry of Higher Education, Research, and Innovation and the French National Center for School and University Affairs for disseminating the survey. We are also grateful to university students for their participation.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jadr.2021.100260.
Appendix. Supplementary materials
References
- Aebischer O., et al. Physical and psychological health of medical students involved in the coronavirus disease 2019 response in Switzerland. Swiss Med. wkly. 2020;150:w20418. doi: 10.4414/smw.2020.20418. [DOI] [PubMed] [Google Scholar]
- Arima M., et al. Factors associated with the mental health status of medical students during the COVID-19 pandemic: a cross-sectional study in Japan. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-043728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolatov A.K., et al. Online-learning due to COVID-19 improved mental health among medical students. Med. Sci. Educ. 2020 doi: 10.1007/s40670-020-01165-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020:912–920. doi: 10.1016/S0140-6736(20)30460-8. Lancet Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J., Yuan Y., Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40(2):171–176. doi: 10.12122/j.issn.1673-4254.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye L.N., Thomas M.R., Shanafelt T.D. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 2006:354–373. doi: 10.1097/00001888-200604000-00009. Lippincott Williams and Wilkins. [DOI] [PubMed] [Google Scholar]
- Gorter R., et al. Psychological stress and health in undergraduate dental students: fifth year outcomes compared with first year baseline results from five European dental schools. Eur. J. Dent. Educ. 2008;12(2):61–68. doi: 10.1111/j.1600-0579.2008.00468.x. [DOI] [PubMed] [Google Scholar]
- Gunther Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J. Med. Internet Res. 2004;6(3):e132. doi: 10.2196/JMIR.6.3.E34. 2004;6(3):e34 https://www.jmir.org/2004/3/e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honney K., et al. Comparison of levels of depression in medical and non-medical students. Clin. Teach. 2010;7(3):180–184. doi: 10.1111/J.1743-498X.2010.00384.X. [DOI] [PubMed] [Google Scholar]
- Horn M., et al. Psychological impact of the COVID-19 pandemic on non-frontline healthcare workers. Gen. Hosp. Psychiatry. 2021 doi: 10.1016/j.genhosppsych.2021.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummel S., et al. Mental health among medical professionals during the COVID-19 pandemic in eight European countries: cross-sectional survey study. J. Med. Internet Res. 2021;23(1):e24983. doi: 10.2196/24983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim A.K., et al. A systematic review of studies of depression prevalence in university students. J. Psychiatr. Res. 2013:391–400. doi: 10.1016/j.jpsychires.2012.11.015. Elsevier Ltd. [DOI] [PubMed] [Google Scholar]
- Khalid A., et al. Relationship between knowledge on COVID-19 and psychological distress among students living in quarantine: an email survey. AIMS Public Health. 2021;8(1):90–99. doi: 10.3934/publichealth.2021007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasheras I., et al. Prevalence of anxiety in medical students during the covid-19 pandemic: a rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health. 2020:1–12. doi: 10.3390/ijerph17186603. MDPI AG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Merwe L.J., Botha A., Joubert G. Resilience and coping strategies of undergraduate medical students at the university of the free state. S. Afr. J. Psychiatry. 2020;26:1–8. doi: 10.4102/sajpsychiatry.v26i0.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quek T.T.C., et al. The global prevalence of anxiety among medical students: a meta-analysis. Int. J. Environ. Res. Public Health. 2019 doi: 10.3390/ijerph16152735. MDPI AG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheokand, N., Kumar, P. (2018). Social Determinants, Psychosocial Function and Mental Health among Medical and Non-Medical Students. Journal of Disability Management and Rehabilitation, 4(1), 39-46. Available from: https://www.researchgate.net/publication/330290443_Social_Determinants_Psychosocial_Function_and_Mental_Health_among_Medical_and_Non-Medical_students [accessed Nov 02 2021].
- Le Vigouroux S., Goncalves A., Charbonnier E. The psychological vulnerability of french university students to the COVID-19 confinement. Health Educ. Behav. 2021 doi: 10.1177/1090198120987128. [DOI] [PubMed] [Google Scholar]
- Voltmer E., Obst K., Kötter T. Study-related behavior patterns of medical students compared to students of science, technology, engineering and mathematics (STEM): a three-year longitudinal study. BMC Med. Educ. 2019;19(1) doi: 10.1186/S12909-019-1696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M., et al. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Netw. Open. 2020 doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie L., et al. The immediate psychological effects of coronavirus disease 2019 on medical and non-medical students in China. Int. J. Public Health. 2020;65(8):1445–1453. doi: 10.1007/s00038-020-01475-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.Y., et al. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: a meta-analysis. J. Nurs. Manag. 2018;26(7):810–819. doi: 10.1111/jonm.12589. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.