Abstract
Background
Little is known about nursing faculty and nursing student's confidence or potential hesitancy to receive the Covid-19 vaccine once it was available.
Methods
An anonymous electronic survey of nursing students and faculty was conducted at a large academic center in the eastern U.S.
Findings
Both students and faculty reported they were fairly or completely confident that the vaccine was safe (n = 235, 89.4%) and that it would effectively mitigate their risk (n = 230, 87.5%). There was a 52.6% decrease in vaccine hesitancy from 6 months prior (p <.01); 22% (n = 58) of those currently willing to receive the vaccine reported moderate to high concern about its side-effects and/or long-term efficacy. Access to vaccine research, vaccine education, and watching others be inoculated, had mitigated their concerns from the previous six months.
Discussion
While both nursing students and faculty reported having high confidence in the efficacy and safety of the Covid-19 vaccine, concerns remained.
Keywords: Covid-19, Vaccine hesitancy, Nursing students, Nursing faculty
Introduction
The spring term of 2020 for colleges and universities was unprecedented in academic history due to the Covid-19 pandemic. The majority of nursing schools instructed students to return home mid-term to finish classes online while in-person clinical experiences for nursing students were concluded. Uncertainty and the associated stress about the changing academic landscape was experienced by both students and faculty and continued into the fall term when both groups returned to campus. While didactic classes were primarily conducted remotely and most nursing faculty worked from home, clinical rotations were expected to be conducted in-person at acute-care hospitals, long-term care facilities, and communities where Covid-19 exposure was greatest. Although rules and guidelines for isolation and quarantining were updated frequently as a strategy to contain further outbreak, the instability of the pandemic was an added stressor to an already academically challenging environment.
During this time of turmoil, societal controversies surrounding Covid-19 flourished and perpetuated mistrust of governmental agencies, the science behind the pandemic, and even the existence of the pandemic itself. General mistrust then shifted toward the development of the vaccine. Anti-vaccine sentiment posed a threat to achieving herd immunity. Vaccine hesitancy, defined as an, “approach characterizing behavior on a spectrum of potential attitudes and behaviors, ranging from active demand for vaccines to complete refusal,” became a potential public health crisis (Dubé et. al., 2021). By December 2020 when vaccines became available, healthcare workers were among the first to receive the vaccine. However, studies conducted as recently as March 2021 indicated that despite the vaccine becoming widely available, 18% of healthcare workers remained hesitant as to whether they would receive the vaccine (Kirzinger et. al., 2021) and only 50% of healthcare workers were vaccinated (Rosenbaum, 2021).
Nurses are trusted healthcare workers that play a vital role in the vaccine uptake process. During early vaccine rollouts, nursing students helped to administer vaccines as a way to increase vaccine access to communities at large including those underserved. Students helped to address concerns and even hesitancy in patients who had come to the clinics. However, factors related to vaccine hesitancy among academic faculty and students at a time when the Covid-19 vaccine was available, have not been examined. We aimed to assess vaccine confidence and hesitancy among students and faculty at a University School of Nursing affiliated with an academic medical center during the initial vaccine rollout. We also aimed to understand the reasons for willingness to receive the vaccine despite known controversies, if there were ongoing or latent concerns over its safety, and if these concerns had changed from the previous six months.
Methods
Design and Sample
We conducted a cross-sectional survey between February 18, 2021 and March 11, 2021 among nursing students and faculty at a University School of Nursing with an affiliated academic medical center located in the eastern United States. All adults (>18 years of age) who were enrolled as a student or appointed as a faculty member in the School of Nursing were eligible to participate in the study. The survey was distributed via email listservs. The email contained a description of the study along with the survey link, and two reminders were sent out over the course of the survey period. Research Electronic Data Capture (REDCap), a secure online software platform, was used to collect and manage the survey data (Harris et. al., 2019,2009). REDCap is a secure, web-based software platform designed to support data capture for research studies. Participation was voluntary and data were collected anonymously. This study was approved by the university's Human Research Protection Office.
Survey Items
Demographic information collected included self-reported age, sex, race/ethnicity, marital status, education, nursing degree, faculty or student status, student or faculty rank, nursing licensure, and workplace/clinical supervision setting. We assessed vaccine hesitancy with the question “Are you willing to receive the COVID-19 vaccination?” with available response options of “Yes, during the initial rollout” (i.e., willing), “Yes, but choose to delay timing of vaccine” (i.e., hesitant), and “No” (i.e., unwilling). Vaccine uptake was assessed by the question “Have you already received the first dose of the COVD-19 vaccine?” Those who had received the vaccination or who were hesitant to receive the vaccination were asked to rank order the following reasons for getting the vaccination: “I want to protect myself and my family/friends,” “I want to protect my patients,” “It would be the best way to avoid getting seriously ill from the disease,” “It would allow me to feel safe around other people,” “My work recommends it,” “Life would get back to normal.” They were given space for free text responses. Questions asked about the extent to which individuals are confident that the vaccine is safe and effective (completely/fairly/somewhat/slightly/not at all), expectation for the efficacy of the vaccine (lifetime immunity/limited time immunity/reduction in symptom severity only/will not be effective/unsure), and degree of knowledge of the vaccine development process (a great deal/much/somewhat/a little/not at all). Again, they were given space for a free text response. Participants were given a list of potential concerns about the vaccine and asked to indicate all concerns during the last 6 months. On a 5-point Likert scale with 5 being highest concern and 1 being lowest concern, participants were asked to indicate their level of concern about the vaccination 6 months ago and now. A free text response was provided for participants to indicate what, if anything, changed their level of concern over the past 6 months. An open space was provided for participants to give any final comments, “Is there any additional information you wish to share about your thoughts or concerns regarding the COVID-19 vaccine?”
Analysis
Analyses were conducted using IBM® SPSS® Statistics v25 (IBM Corp., n.d.). For the categorical variables, we reported cell frequencies among both students and faculty. For age as a continuous variable, we assessed a mean and standard deviation. McNemar's Chi-Squared test was conducted to determine % change in attitudes towards the vaccine over 6 months. Statistical significance was set as p < .05.
Findings
Sample Characteristics
A total of 58 faculty and 205 students completed the survey (response rates: students 19%; faculty 46%). Over half of the faculty and students worked in a patient facing role (n = 144, 54.4%). Of the 144 respondents, 120 students and 24 faculty also worked in a clinical setting either as a patient care technician or clinical instructor. Representation among faculty was evenly split: Assistant Professor (n = 24, 41.4%), Associate Professor (n =10, 17.2%), Professor (n = 17, 29.3%), Instructor (n = 7, 12.1%). Students were also well represented across academic years: Freshman (n = 48, 23.4%), Sophomore (n = 39, 19.0%), Junior (n = 22, 10.7%), Senior (n = 41, 20.0%), Graduate Student (n = 49, 23.9%), Post-Doctoral Scholar (n = 6, 2.9%). Table 1 provides further description of the sample by student or faculty role.
Table 1.
Characteristics of Sample by Role
| Characteristics | Student n (%) | Faculty n (%) |
|---|---|---|
| Sex | ||
| Men | 24 (11.8) | 9 (15.8) |
| Women | 179 (87.7) | 48 (84.4) |
| Nonbinary | 1 (0.5) | – |
| Missing | – | 1 |
| Age, mean (SD) | 54.07 (13.4) | 23.9 (7.5) |
| Race | ||
| White | 173 (84.4) | 56 (94.6) |
| Non-White | 32 (15.6) | 2 (3.4) |
| Ethnicity | ||
| Hispanic or Latino | 9 (3.4) | – |
| Not Hispanic or Latino | 193 (94.1) | 58 (100) |
| Unknown | 1 (0.5) | – |
| Prefer not to answer | 2 (.01) | – |
| Do not think they will get Covid-19 | 32 (55.2) | 87 (42.4) |
| Received 1st dose of Covid-19 vaccine | 143 (70.8) | 38 (67.9) |
Perceptions of the Covid-19 Vaccine
Both students and faculty reported that they were fairly or completely confident that the vaccine was safe [faculty (n = 54, 94.7%), students (n = 181, 88.3%)] and that it would completely or fairly effectively mitigate their risk [faculty (n =55, 94.8%), students (n = 175, 85.4%)]. The majority of students and faculty reported that they had enough information on what to expect when receiving the vaccine [faculty (n = 57, 98.3%), students (n = 186, 90.7%)] and had “adequate information about the Covid-19 vaccination to make an informed decision about whether or not to receive it” [faculty (n =56, 96.6%), students (n = 191, 93.2%)].
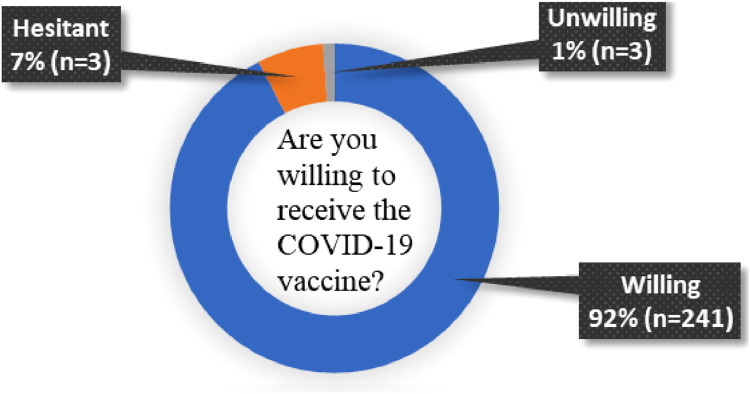
Covid-19 Vaccine Hesitancy
The majority (n=241, 92%) of students and faculty combined were willing to receive the Covid-19 vaccine (Figure 1 ). The top 3 reasons given by faculty for their willingness to receive the vaccine were 1) To protect friends and family, 2) To avoid illness, and 3) To feel safe around others. The top 3 reasons given by students for their willingness to receive the vaccine were 1) To protect friends and family, 2) To protect their patients, and 3) To avoid illness. Participants were given the opportunity to provide additional reasons as to why they were willing to get the vaccine. Qualitative responses (n = 17) varied from “it was the right thing to do!” to “It will allow me to resume travel out of country.” 2 participants listed medical and mental health reasons as personal reasons to receive the vaccine
Figure 1.
Covid-19 intention to be vaccinated
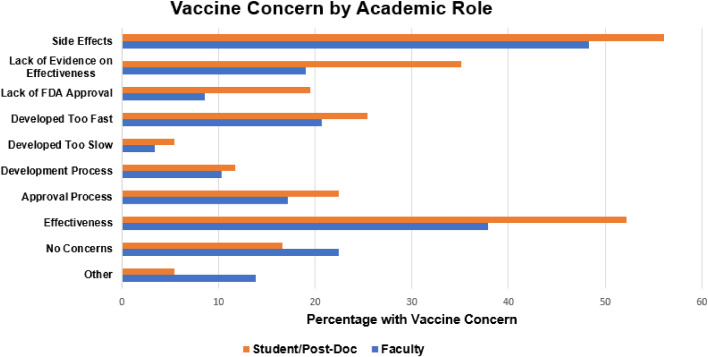
Covid-19 Vaccine Uptake and Concerns
At the time of the survey, 70% (n = 170) of both students and faculty had received one dose of the Covid-19 vaccine. Despite the relatively high level of vaccine uptake, many students and faculty reported moderate to high concern about its development, approval, side effects, and/or effectiveness [faculty (n =13, 22.4%), students (n = 45, 22%)]. Figure 2 summarizes possible reasons for those concerns.
Figure 2.
Vaccine concerns by academic role
When given the opportunity to write in additional comments regarding concerns about the vaccine, students and faculty expounded on their choices, or reported additional concerns. Nine faculty and 29 students responded. The percentages reported are specific to the total qualitative responses for each question. Their comments are summarized topically in four categories: 1) Concerns over short and long-term effects, 2) Concerns over racial inequities, 3) Mixed responses, and 4) No concerns. Few comments discussed the development, approval process, or lack of FDA approval.
Short and Long-Term Effects
Only one student mentioned being concerned about the short-term side effects; they were worse than what she had anticipated. Out of the respondents, the majority of comments from students (n = 14, 48.2%) were concerned about the long-term side effects. Fertility was mentioned 5 times, with one student summarizing “Possible fertility issues-however that is so hard to research and actually point that the Covid vaccine caused fertility issues.” Another student reported having “Serious concerns for childbearing females and children. Would not get the vaccine if I was in this category or had children and would not currently recommend it to others in this category.” Several students (n = 3, 10%) were also worried about the lack of evidence regarding the vaccine's long-term ability to prevent Covid-19 infection. Faculty did not mention concerns over the short or long-term effects of the vaccine.
Racial Inequities
A few students and faculty (n = 3, 8.0%) were concerned about inequities in vaccine development and access to the vaccine. A student succinctly wrote, “Majority of clinical trial subjects were white, with limited inclusion of other races. For the Moderna vaccine, only about 4.7% of trial subjects were Asian. There's also no research on efficacy in pregnant women and children yet” (Artiga et al., 2021). One student reported that racial health inequities contributed to mistrust, “Close friends' opinions on the vaccine, especially since they are Black and have mistrust with healthcare.” One faculty responded, “inequities in access to vaccine; too little education for the public about the risk-benefits.”
Mixed Responses
We also found a mixed assortment of concerns that we summarize here. 1 student expressed concern about the speed of the vaccine development, “Possible long-term effects of the virus given that development was somewhat quick.” 2 students mentioned the use of mRNA to make the vaccine, “Alterations of RNA is very concerning to me.” Faculty had concerns related to the distribution of the vaccine, “lack of organized and structured distribution network”, “federal and state incompetence,” and “mistrust of the previous administration,” but “more confident with new administration at federal level.”
No concerns
A few students and faculty said that they were never very concerned. One student summarized this perspective, “never did I have a concern that was enough for me to consider not wanting the vaccine.”
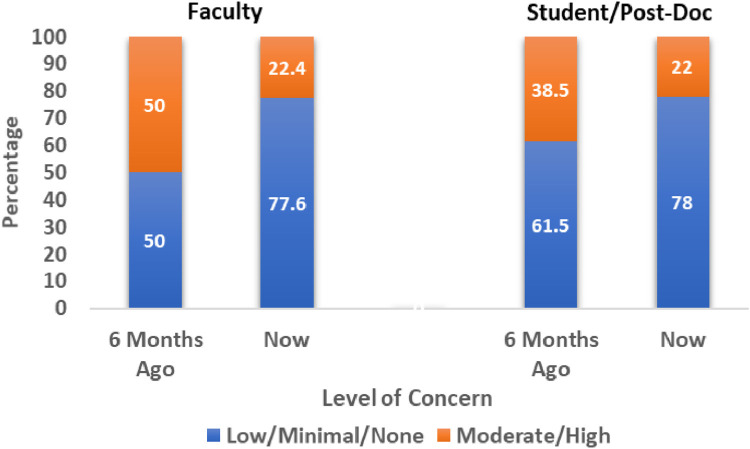
Change in Covid-19 Vaccine Concerns
From August 2020 to February 2021, there was a 52.6% decrease in concern in both students and faculty over the previous 6 months (p <.001). Faculty were more concerned about the vaccine than students 6 months prior to our survey. Thus faculty experienced a greater decrease in concerns than students, with both 22% (n = 45) of students and faculty reporting ongoing concerns (Figure 3 ). We asked participants what had changed their attitudes and perspectives towards the vaccine. This question elicited the strongest and highest number of qualitative responses; 18 faculty and 62 students shared their opinions. We found there to be 4key topics that summarized why their level of concern had changed: 1) Better and more available research, 2) Watching others get the vaccine, 3) Political reasons, and 4) Wanting an improved life.
Figure 3.
Change in level of concern from August 2020 to February 2021
Up-to-Date Rigorous Research and Education
This topic garnered five faculty responses (29.0%) and 29 student responses (46.8%) and was the primary reason given for increased vaccine confidence in both students and faculty. Students reported that they had gained a greater education about the vaccine since the previous summer, “more education on the process of the vaccine and the technology.” Another student said, “I started doing more research and was presented with more information from trustworthy sources.” Faculty were more likely to phrase their responses in terms of research findings, “Population COVID incident data” and “Research and RCT evidence.”
Watching Others Get the Vaccine
This theme was most important to the students and was mentioned 15 times (24.1%). One student was swayed by the appeals from authority, “Seeing the types of scholars, academics, and experts get behind the vaccine and its science.” Others were convinced by seeing their peers get the vaccine “People I know have gotten it and the short-term effect seems to be ok” with 1 student stating “many people have had the vaccine already and they aren't dropping dead.” For another student, the ability to see a family member get the vaccine without ill effects reduced their concern, “My mother received both doses of the vaccine and has not had any problems since.” Only 1 faculty member reported this to be an important reason for their decrease concerns of the vaccine, “Seeing other people get the vaccine safely before me helped me to feel more confident.”
Political and Travel Reasons
Students (n = 3, 2.8%) and faculty (n = 5, 27.7%) mentioned the change in the U.S. administration as a factor in reducing concern about the vaccine. 1 faculty member simply wrote “a new president” as the reason for her increased confidence in the vaccine. Another faculty member was interested in the ability to travel, “Increased desire to travel out of country and news of requiring vaccination to do so without quarantine restrictions.”
No Change or Increase in Level of Concern
A few students and faculty (n = 3, 4.0%) reported no change or decrease in concern. 1 faculty was concerned about the continued problems in distribution “concerns remain high due to inequities in distribution” and another student reported becoming more concerned when she had severe side effects “I got more concerned after I had some pretty bad side effects from the vaccine.”
Discussion
For the present study, we surveyed students and faculty at a large academic institution in the U.S. about their confidence in the Covid-19 vaccine development and rollout process as well as their willingness and hesitancy to receive the vaccine. We found that most students and faculty were willing to get the vaccine and 70% had already received it. Our findings also indicated that their willingness to receive the vaccine was not without concerns and/or hesitation. There remained concerns about the long and short-term effects of receiving the vaccine, its development process, and the inequities associated with vaccine rollout. Finally, the level of concern seemed to have been mitigated by several factors including increased availability and rigor of vaccine research, opportunity to watch peers/colleagues get vaccinated with minimal to no side effects, and the change in the U.S. administration.
Our study both corroborates and extends previous research on vaccine hesitancy in nursing students and faculty. A study surveyed students and faculty in the northeastern U.S. about their willingness to receive the vaccine during August and September 2020. With a response rate of 94% faculty, 33% adjunct, and 70% students, respectively, they found similar to the reports in the present study's reports of vaccine hesitation in August 2020, that only 60% of full-time faculty and 45% of part-time faculty and students were willing to receive the vaccine prior to the vaccine rollout (Manning et. al., 2021). Likewise, a study of 2,249 undergraduate nursing students located across seven countries (Greece, Albania, Spain, Cyprus, Italy, Czech Republic, Kosovo) was conducted in December 2020 about their willingness to get the vaccine (Patelarou et al., 2021). Pooled analyses revealed that only 43% of nursing students were willing to receive the vaccine (Patelarou et al., 2021). They did not report a response rate. However, 86% of Italian nursing students were willing to get the vaccine possibly due to the severity of the pandemic in Italy that previous year. Given that the vaccine rollout had begun by December 2020 in many countries including the U.S., these results suggest that vaccine hesitancy was a world-wide phenomenon.
While most responses about the uncertainty of long-term effects were general in nature, many students, most of whom were young women, expressed concerns about the possibility of the vaccine affecting fertility. Blog posts, media outlets, and historical concerns over the effect of vaccines on fertility collectively fostered Covid-19 vaccine hesitancy (Male, 2021). Concerns over fertility as a disincentive to receiving the vaccine has been discredited at this time (Iacobucci, 2021), however, this is an example of the powerful effects that social media and other media outlets can have on public health.
Health equity concerns were commonly mentioned by nursing students and faculty in our survey. In the midst of the Covid-19 pandemic in 2020, renewed attention was brought to issues of racial health disparities. At the time of our survey, despite state guidelines indicating that anyone over the age of 65 were eligible for the vaccine, there were reports that older whites in our communities were more likely to receive the vaccine than older Blacks (Beery et al., 2021). Students were also volunteering at this time to vaccinate underserved patients in community settings. While it is unknown to what extent these reports and experiences affected the student's or faculty's willingness to receive the vaccine, it likely negatively affected their attitudes towards the vaccine trials and distribution.
Our survey, which was conducted in February and March 2021 after the emergency approval for the vaccine in the U.S., indicated that previous vaccine hesitancy had diminished, as indicated by the high percentage of both faculty and students who were willing to receive the vaccine (90%) and high vaccine uptake rate (70% had receive their first dose). Although we found that most of our participants had intended to receive and/or had received the vaccine, concerns remained. The role of up-to-date and rigorous vaccine research played a key role in the decrease in vaccine concerns in both students and faculty. In August and September 2020, the vaccine trials’ results had not yet been disseminated and this may have accounted for the vaccine hesitancy reported in our study and prior studies (Manning et al., 2021). As information from trusted sources became available, nurse researchers and students learned of the robust efficacy of the Covid-19 vaccines to prevent illness and severe disease. Both faculty and students indicated that this increase in information and data was a primary reason for their intention to receive the vaccine.
Seeing others, including parents, peers, and authority figures, get the vaccine without reports of severe side effects helped to alleviate students’ and faculty's concerns. In public health terms, change can happen using a normative-reeducative strategy (Quinn & Sonenshein, 2007) meaning that while education about best infection prevention practices are taught (e.g. vaccine uptake, mask wearing), this theory posits that peoples’ healthcare decisions are not always rational and are affected by socio-cultural norms. The attitudes of the nursing students toward the vaccine were not only affected by better and improved research, but also by normalization of vaccine uptake in their own families and peer groups. At the time of the survey, the nursing students were given the opportunity to be vaccinated at large clinics held just for them on specific days and times. Discussion of the vaccine clinics with their friends and peers, attending with a friend(s), and being vaccinated by their peers likely helped to normalize vaccine uptake and created an additional and effective incentive to get vaccinated.
Our students and faculty who were affiliated with an academic center were more willing to receive the vaccine compared to reports of vaccine hesitancy in other health professions (Kirzinger et. al., 2021). Health care workers can range from nursing assistants working in nursing or personal homes through highly educated professors or physicians. The Kaiser Family Foundation studies reported that 11% of those with 4 year degrees and 8% of those with postgraduate degrees were unwilling to receive the vaccine, while up to one quarter of those with less than a bachelor's degree were unwilling to get the vaccine (Kirzinger et. al., 2021). The high level of vaccine confidence in the present study corroborate these patterns – the students and faculty are affiliated with a large medical center, all faculty are doctorally prepared, and students are all part of a BSN program which is the highest entry level program for new nurses in the U.S. Future studies are needed to examine if nursing students and faculty at non research-intensive institutions, associate degree, or diploma nursing programs report the same confidence in the vaccine. Findings could assist in tailoring education and normative strategies to the type of educational programs involved.
The CDC, the Advisory Committee on Immunization Practices (ACIP), and the Healthcare Infection Control Practices Advisory Committee (HICPAC) recommend that all U.S. health care workers get vaccinated annually against influenza (Pearson et. al., 2006). In the U.S., 17 states require hospitals to mandate the influenza vaccine, and most non-VA hospitals require health care workers to get the influenza vaccine or wear a mask during the flu season (Greene et al., 2018). As a result, in the 2019/2020 flu season, 92% of U.S. nurses received the flu vaccine (Centers for Disease Control and Prevention, 2021). A pooled study of nursing students in seven international countries found a significant association between previous influenza vaccine uptake and willingness to receive the flu vaccine (p <.001) (Patelarou et al., 2021). At our academic institution, all nursing students and faculty are required to provide verification that they had received the flu vaccine in order to participate in clinical training. It is likely that the expectation of students and faculty to be vaccinated against other infectious diseases contributed to their overall willingness to receive the Covid-19 vaccine.
Mandating the Covid-19 vaccine in academic institutions may be controversial in certain populations of the U.S. and therefore some nursing schools will choose to provide encouragement only, potentially impacting future vaccine uptake rates. Several approaches can be utilized to encourage vaccine uptake among nursing students and faculty. Our survey results suggest that appeal from authority (research, CDC, institutional committees), along with continued education on the vaccine, should be integrated into programs that encourage vaccination. Another strategy to overcome latent hesitancy is to normalize vaccine uptake among the students themselves. We recommend student testimonials from those who have gotten the vaccine, outreach to nursing student organizations, and targeted campaigns to all undergraduate students. Future research can test these interventions to determine if they need to be further tailored to specific types of nursing programs.
Nursing, the most trusted occupation, will continue to be at the forefront of the campaigns to eradicate communicable diseases, with Covid-19 being one of the most important threats. Our study can be used as a springboard to assess and compare levels of ongoing hesitancy in nursing schools, and to provide suggestions for developing interventions that may mitigate hesitancy if it continues. Nurses are important to the public health of the U.S. and other global communities, and as such, are well positioned to promote vaccine confidence.
Limitations
A strength of the study was that it was conducted during the initial vaccine rollout allowing us to capture the perspectives and concerns of nursing faculty at the time they happened. However, as a cross-sectional study, we could only capture one moment in time. The dynamic nature of the pandemic means that our findings may not be translatable to next year or even the fall of 2021. Our findings, specific to the population of a research-intensive nursing school, may not translate to other populations, higher learning institutions, or even nursing non-research-intensive nursing schools. Compared to the Manning et. al. study, our response rate was lower, and therefore may not have been reflective of the majority of the nursing students or faculty. Those most interested in the Covid-19 vaccine, may have been the most likely to complete the survey leading to selection bias.
Author Contribution
Jonna L. Morris: Conceptualization, Writing- original draft preparation, statistical analyses, methodology, investigation, Writing- reviewing and editing. Lynn Baniak: Conceptualization, Visualization, Investigation, Statistical Analyses, Writing- reviewing and editing. Faith Luyster: Conceptualization, Visualization, Writing-reviewing and editing; Jacqueline Dunbar-Jacob: Conceptualization, Writing- Reviewing and Editing.
Funding Sources
Clinical and Translational Sciences Institute at the University of Pittsburgh Grant Number UL1-TR-001857
References
- Artiga, S., Kates, J., Michaud, J., & Hill, L. (2021). Racial Diversity within COVID-19 Vaccine Clinical Trials: Key Questions and Answers. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-diversity-within-covid-19-vaccine-clinical-trials-key-questions-and-answers/.
- Beery, J., Bey, J., Gary-Webb, T., Gradeck, Issac, L., Kohler, J., Yonas, M. (2021). Missing our shot: COVID-19 Vaccine equity in allegheny county by urbankind institute – issuu. Retrieved from https://issuu.com/urbankind/docs/bec_vaccine_report. Accessed May 19, 2021.
- Centers for Disease Control and Prevention (CDC). (2021). Immunization of health-care workers: recommendations of the advisory committee on immunization practices (ACIP) and the hospital infection control practices advisory committee (HICPAC). Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/00050577.htm. Accessed May 21, 2021.
- Dubé È., Ward J.K., Verger P., Macdonald N.E. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annu. Rev Public Health. 2021;42:175–191. doi: 10.1146/annurev-publhealth. [DOI] [PubMed] [Google Scholar]
- Greene M.T., Fowler K.E., Ratz D., Krein S.L., Bradley S.F., Saint S. Changes in influenza vaccination requirements for health care personnel in us hospitals. JAMA Network Open. 2018;1 doi: 10.1001/jamanetworkopen.2018.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., Duda S.N. Vol. 95. 2019. The REDCap consortium: Building an international community of software platform partners. (Journal of Biomedical Informatics). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobucci G. Covid-19: No evidence that vaccines can affect fertility, says new guidance. BMJ (Clinical Research Ed.) 2021;372:n509. doi: 10.1136/bmj.n509. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows. Armonk, N.Y., USA.
- Kirzinger, A., Kearney, A., Hamel, L., Brodie, M. (2021). KFF/Washington Post Frontline Health Care Workers Survey – Vaccine Intentions –9666 | KFF, Retrieved from https://www.kff.org/report-section/kff-washington-post-frontline-health-care-workers-survey-vaccine-intentions/. Accessed May 21, 2021.
- Male V. Are COVID-19 vaccines safe in pregnancy? Nature Reviews Immunology. 2021;21:200–201. doi: 10.1038/s41577-021-00525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning M.Lou, Gerolamo A.M., Marino M.A., Hanson-Zalot M.E., Pogorzelska-Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nursing Outlook. 2021;69(4):565–573. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson Michele L., Bridges C.B., Harper S.A. Healthcare Infection Control Practices Advisory Committee (HICPAC); Advisory Committee on Immunization Practices (ACIP). Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006;55(RR-2):1–16. Erratum in: MMWR Recomm Rep. 2006 Mar 10;55(9):252. PMID: 16498385. [PubMed] [Google Scholar]
- Patelarou E., Galanis P., Mechili E.A., Argyriadi A., Argyriadis A., Asimakopoulou E., Patelarou A. Factors influencing nursing students’ intention to accept COVID-19 vaccination – A pooled analysis of seven countries. MedRxiv. 2021 doi: 10.1101/2021.01.22.21250321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn R.E., Sonenshein S. Four general strategies for changing human systems. The Nature of Organization Development. 2007:69–78. [Google Scholar]
- Rosenbaum L. Escaping Catch-22 — overcoming covid vaccine hesitancy. New England Journal of Medicine. 2021;384:1367–1371. doi: 10.1056/nejmms2101220. [DOI] [PubMed] [Google Scholar]