Abstract
Background
Patients with chronic obstructive pulmonary disease complicated with coronary heart disease are a major public health problem, but it has not been widely accepted by the public or health professionals, the purpose of this study is to conduct a meta-analysis of the literature reports on the risk of coronary heart disease in patients with chronic obstructive pulmonary disease.
Methods
Data sources are PubMed and Web of Science searched up to August 2021. Design is meta-analysis.
Results
Literature searches yielded 8877 records, meta-analysis showed that the risk of coronary heart disease in chronic obstructive pulmonary disease patients was 1.24 times higher than that in non-chronic obstructive pulmonary disease patients (HR=1.24,95% CL 1.16–1.32).
Conclusion
The findings suggest that patients with chronic obstructive pulmonary disease are at a higher risk of developing coronary heart disease than non-chronic obstructive pulmonary disease patients.
Keywords: meta-analytic methods, coronary heart disease risk, chronic obstructive pulmonary disease, COPD
Introduction
COPD is characterized by chronic pulmonary inflammation, which leads to progressive and irreversible airflow obstruction, and periodic acute exacerbations deteriorate and aggravate.1 The global prevalence rate of COPD was 251 million in 2016 and 3.17 million people died in 2015.2 CHD and COPD are among of the three main causes of death in the world.3,4 COPD increases the risk of CHD due to chronic systemic/local inflammation.1,3–6 And traditional cardiovascular risk factors such as smoking, hypertension, hyperlipidemia are highly prevalent in patients with COPD, they could contribute to COPD progression.7 Epidemiological studies have also shown that the incidence of cardiovascular death in patients with COPD is high.5 Patients with COPD complicated with CHD are a major public health problem.
The 2016 European guidelines for Cardiovascular Disease Prevention published by European Society of Cardiology show that the main risk factors for CHD are age, sex, Family history/genetics, smoking, living habits, blood pressure, blood lipid level and so on, excluding COPD.8 Although it has been previously reported that COPD is closely related to the increase in CHD, it has not been widely accepted by the public or health professionals.
Therefore, the purpose of this study is to conduct a meta-analysis of the literature reports on the risk of CHD in patients with COPD. At present, there is no literature report on meta-analysis using cohort study. Compared with the meta-analysis of previous case-control studies, the latter did not consider the time experienced and may draw inappropriate conclusions, and the former has a stronger causality and can better prove that COPD is a risk factor for CHD.
Methods
Literature Search
A systematic literature search was all literature at PubMed and Web of Science before August 2021, a meta-analysis was performed using a predefined search strategy to investigate the association between COPD and CHD prevalence in a cohort study, the specific search term is (((COPD) AND (coronary disease OR coronary heart disease OR chronic coronary artery disease OR acute coronary syndrome OR arteriosclerotic cardiovascular disease)) AND Hazard Ratio). Titles and abstracts, where available, were screened for possible inclusion and then full-text versions of potential inclusion studies were obtained for further screening, done independently by the author. The characteristics and results of the study were tabulated and compared.
Inclusion and Exclusion Criteria
I included five cohort studies that reported Hazard Ratio and corresponding 95% confidence intervals based on multifactorial adjustments in the Cox model. The subjects were the general population, the exposure group was diagnosed with COPD, the non-exposure group was not diagnosed with COPD, and the result was CHD.
Risk of Bias Assessment
I use PRISMA to evaluate.
Data Analysis
In this study, fixed effect model meta-analysis was used to merge the results, and O - E and Variance was used to deal with HR values, all of which were carried out on Review Manager 5.4.1. I used the P value of Q and I2 to test the heterogeneity, such as I2 more than 70% or P < 0.05, then considered that the statistical heterogeneity was too large, and the sensitivity analysis was used for further treatment. Evaluation of publication bias by funnel diagram.
Results
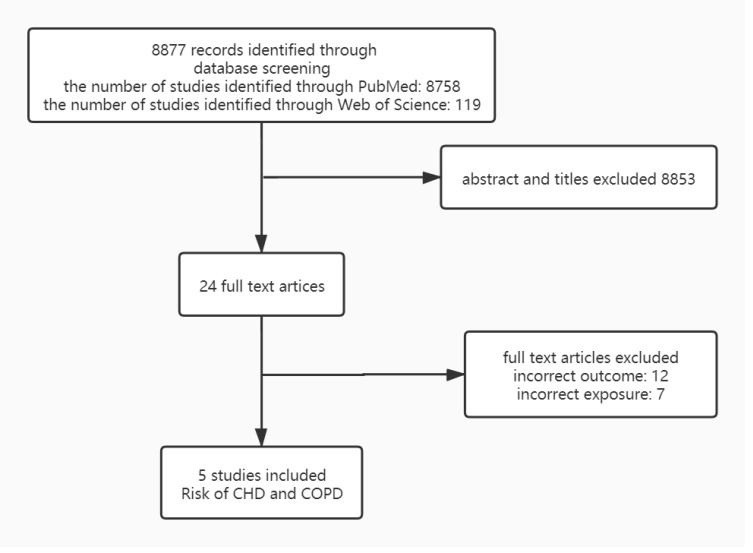
Literature searches yielded 8877 records. After title and abstract screening, 24 records were selected for full-text assessment, which resulted in the inclusion of 5 studies. The inclusion and exclusion process is summarized in Figure 1. The total number of patients is 26,603. The meta-analyses were based on 5 separately conducted cohort studies,9–13 the characteristics and results of included study are shown in Table 1.
Figure 1.
The inclusion and exclusion data process summarization. Data sources were all PubMed and web of science searched up to August 2021 based on specific search term.
Table 1.
Characteristics and Results of Included Studies – Risk of CHD in People with COPD
| Study | Design and Setting | Population | CHD Definition | Maximally Adjusted Estimate (95% CI) | Factors Adjusted for |
| Li et al 20159 | A nationwide retrospective cohort study using the Taiwan National Health Institute Research Database from 1998 to 2008, with a follow-up period extending to the end of 2010 | For the claims data collected from 1998 to 2008, the ICD-9-CM code 496 was used to identify newly diagnosed chronic COPD or inclusion in the study cohort. All patients without a history of COPD were randomly selected from the registry of beneficiaries. The study enrolled 20728 COPD patients and 41147 controls. | According to (ICD-9-CM410-414) | HR 1.34(1.17-1.54) | Sex, age and comorbidities |
| Liao et al 201510 | A retrospective cohort design using the Taiwan Health Insurance Research Database. Patients in the study cohort were followed to the end of 2011. | The eligible study subjects were patients who received a discharge diagnosis of COPD (ICD-9-CM codes: 490–492, 496) during a hospitalization between January 1, 2002 and December 31, 2011.Control subjects were selected from hospitalized patients. The study included 8640 patients with COPD and 17280 controls. | According to (ICD-9-CM) | HR 1.58(1.2-2.08) | Age, gender and comorbidities |
| Mattila et al 201811 | The Mini-Finland Health Survey was carried out between 1978 and 1980.Patients were followed up through record linkage with national registers through 2011. | The data from 5576 subjects who had all pertinent health information collected through interviews, questionnaires, and clinical examinations, and for whom a comprehensive health examination was performed. | A major coronary event includes hospital care periods with ICD codes 410 and 411.0 (ICD-8 and ICD-9) and I20.0, I21, and I22 (ICD-10) | HR 1.06(0.79-1.42) | Age, gender and confounding factors |
| Ingebrigtsen et al 202012 | Data from The Copenhagen General Population Study. Recruitment began in 2003, and a follow-up examination of all individuals was initiated in 2014 and is still ongoing. | Identified 54046 individuals defined by one of eight groups of different phenotypes of airway disease, based on the information obtained in the questionnaires and results of spirometry, and a reference group consisting of participants with no respiratory disease. | Coronary heart disease (ICD-8:410-414 and ICD-10:I20–I25) | Stage 1+2 HR 1.5 (1.38-1.62) Stage 3+4 HR 2.15 (1.75-2.66) | Age and gender |
| Liao et al 201513 | The data used in the present study were derived from a sub-dataset of the NHIRD that comprises all records collected from 1996 to 2010 on 1 million randomly sampled beneficiaries enrolled in the NHI in 2010. | 20492 patients with COPD were selected to be the study patients and were designated as the COPD cohort. For each COPD patient, two non-COPD patients were randomly selected from the same study period according to the same exclusion criteria and were frequency-matched with the COPD patients according to age and sex to construct the non-COPD cohort, which comprised 40765 patients. | Coronary artery disease (ICD-9-CM410–414) | HR 1.19(1.09-1.20) | Age and sex |
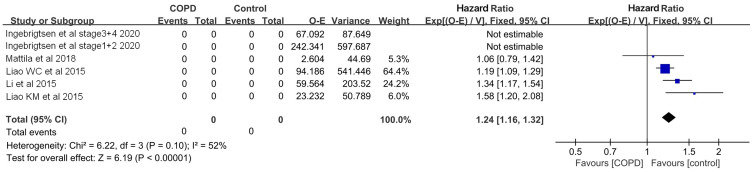
One of the five studies were excluded and will be discussed later. Of the four studies included, three found that COPD patients had a higher risk of developing CHD than non-COPD patients, and all of the three studies resulted in HR adjusted for age, sex, co-illness or confounding factors, while one adjusted only for age and sex. The meta-analysis of the four studies included showed that the risk of CHD in COPD patients was 1.24 times higher than that in non-COPD patients (HR=1.24,95% CL 1.16–1.32) (Figure 2).
Figure 2.
Forest plot shows risk of CHD in people with COPD. It showed that the risk of CHD in COPD patients was 1.24 times higher than that in non-COPD patients.
Abbreviations: COPD, chronic obstructive pulmonary disease; CHD, coronary heart disease.
Discussion
Because only in the study of Ingebrigtsen, the situation of COPD was graded, while other literatures only pointed out that they had COPD, and because of the insufficient number of literatures, it was impossible to carry out subgroup analysis. Therefore, the study of Ingebrigtsen was divided into Ingebrigtsen stage1+2 2020 and Ingebrigtsen stage3+4 2020 according to the original text.
In evaluating the published bias of six studies with funnel maps, Ingebrigtsen stage3+4 2020 was located outside the dotted line of funnel maps, possibly because the subjects included in the study had a higher burden of disease and were more likely to develop CHD than other studies, so Ingebrigtsen stage3+4 2020 was excluded.
When the other five studies were tested for heterogeneity, Q was P < 0.05, I2 was 79%, HR = 1.34 (95% CL 1.27–1.41), heterogeneity was too large, sensitivity analysis was carried out, excluding Ingebrigtsen stage1+2 2020, P > 0.05, I2 = 52%, there was no heterogeneity and HR=1.24 (95% CL 1.16–1.32). Ingebrigtsen stage1+2 2020 reversed the heterogeneity results, but did not change the relationship between COPD patients and the risk of CHD. The source of heterogeneity may mainly come from the differences of the study population, on the one hand, the population inclusion criteria are different, the other studies include the full degree of COPD, while the COPD, of the item is only included in the COPD, of the stage1+2, on the other hand, the sample size in the item is too large, which leads to greater heterogeneity. As a result, Ingebrigtsen stage1+2 2020 was removed.
The combined analysis results of this study show that COPD patients have a higher risk of CHD, and COPD is a risk factor for CHD, which is consistent with the current research on the mechanism of CHD. Though the mechanisms by which COPD increases CHD risk are not clear, patients with COPD often display abnormally high concentrations of circulating systemic inflammatory could be the main reason,3–6 and the lung hyperinflation also represent one of the most important problem related to the high thoracic pressure that could be generated.14 However, public or health professionals and patients with COPD still generally have insufficient understanding of “COPD increases the risk of developing CHD,” leading to poor prevention of coronary heart disease. The exact cause is unclear, but the lack of specific guidelines for COPD as a risk factor for CHD and the management of coronary heart disease and cardiovascular risk factors in COPD patients may be an important contributing factor.
In addition, clinical studies proved that anti-inflammatory treatment and the bronchodilators lower the incidence of cardiovascular events.14–16 Therefore, the therapies of directly or indirectly modulating chronic inflammation and the bronchodilators is an important approach for prevention of CHD and treatment of COPD. The development of reasonable exercise and nutritional interventions for pulmonary rehabilitation is also an important therapeutic measure. Studies have shown that reasonable lung rehabilitation can reduce cardiovascular risk factors and help to improve prognosis.17
The main limitation of our research is that, most articles are adjusted for age, sex, co-illness or confounding factors to get the final HR value, but Liao WC 2015 only adjusts the basic age and sex.13 And most of the articles did not grade COPD except Ingebrigtsen 2020. I hope that there will be more cohort research in the future research. Because it has a stronger causal relationship than case-control studies, and it is clearer about the relationship between risk factors and disease.
Conclusion
The findings suggest that patients with COPD are at a higher risk of developing CHD than non-COPD patients.
Funding Statement
There is no funding to report.
Abbreviations
CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease.
Data Sharing Statement
This is a meta-analysis of previously published studies.
Ethics Approval
The present meta-analysis was not required for the ethics approval in our institute, because none of patients of our institute were included.
Patient and Public Involvement
No patient involved.
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.King PT. Inflammation in chronic obstructive pulmonary disease and its role in cardiovascular disease and lung cancer. Clin Transl Med. 2015;4(1):68. doi: 10.1186/s40169-015-0068-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Almagro P, Boixeda R, Diez-Manglano J, Gómez-Antúnez M, López-García F, Recio J. Insights into chronic obstructive pulmonary disease as critical risk factor for cardiovascular disease. Int J Chron Obstruct Pulmon Dis. 2020;15:755–764. doi: 10.2147/COPD.S238214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:95–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunisaki KM, Dransfield MT, Anderson JA, et al. Exacerbations of chronic obstructive pulmonary disease and cardiac events. A post hoc cohort analysis from the SUMMIT randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):51–57. doi: 10.1164/rccm.201711-2239OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Putcha N, Drummond MB, Wise RA, Hansel NN. Comorbidities and chronic obstructive pulmonary disease: prevalence, influence on outcomes, and management. Semin Respir Crit Care Med. 2015;36(4):575–591. doi: 10.1055/s-0035-1556063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aisanov Z, Khaltaev N. Management of cardiovascular comorbidities in chronic obstructive pulmonary disease patients. J Thorac Dis. 2020;12(5):2791–2802. doi: 10.21037/jtd.2020.03.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crisan L, Wong N, Sin DD, Lee HM. Karma of cardiovascular disease risk factors for prevention and management of major cardiovascular events in the context of acute exacerbations of chronic obstructive pulmonary disease. Front Cardiovasc Med. 2019;6:79. doi: 10.3389/fcvm.2019.00079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice. The sixth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts. developed with the special contribution of the European association for cardiovascular prevention & rehabilitation]. G Ital Cardiol. 2017;18(7):547–612. [DOI] [PubMed] [Google Scholar]
- 9.Li CH, Chen WC, Liao WC, et al. The association between chronic obstructive pulmonary disease and Parkinson’s disease: a Nationwide Population-Based Retrospective Cohort Study. Qjm an Int J Med. 2015;108(1):39–45. doi: 10.1093/qjmed/hcu136 [DOI] [PubMed] [Google Scholar]
- 10.Liao KM, Ho CH, Ko SC, Li CY. Increased risk of dementia in patients with chronic obstructive pulmonary disease. Medicine. 2015;94(23):e930. doi: 10.1097/MD.0000000000000930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattila T, Vasankari T, Rissanen H, Knekt P, Puukka P, Heliovaara M. Airway obstruction and the risk of myocardial infarction and death from coronary heart disease: a national health examination survey with a 33-year follow-up period. Eur J Epidemiol. 2018;33(1):89–98. doi: 10.1007/s10654-017-0278-3 [DOI] [PubMed] [Google Scholar]
- 12.Ingebrigtsen TS, Marott JL, Vestbo J, Nordestgaard BG, Lange P. Coronary heart disease and heart failure in asthma, COPD and asthma-COPD overlap. BMJ Open Respir Res. 2020;7(1):e000470. doi: 10.1136/bmjresp-2019-000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liao WC, Lin CL, Chang SN, Tu CY, Kao CH. The association between chronic obstructive pulmonary disease and dementia: a Population-Based Retrospective Cohort Study. Eur J Neurol. 2015;22(2):334–340. doi: 10.1111/ene.12573 [DOI] [PubMed] [Google Scholar]
- 14.Santus P, Radovanovic D, Di Marco S, et al. Effect of indacaterol on lung deflation improves cardiac performance in hyperinflated COPD patients: an interventional, randomized, double-blind clinical trial. Int J Chron Obstruct Pulmon Dis. 2015;10:1917–1923. doi: 10.2147/COPD.S91684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Liu X, Shi H, et al. NLRP3 inflammasome, an immune-inflammatory target in pathogenesis and treatment of cardiovascular diseases. Clin Transl Med. 2020;10(1):91–106. doi: 10.1002/ctm2.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santus P, Centanni S, Verga M, Di Marco F, Matera MG, Cazzola M. Comparison of the acute effect of tiotropium versus a combination therapy with single inhaler budesonide/formoterol on the degree of resting pulmonary hyperinflation. Respir Med. 2006;100(7):1277–1281. doi: 10.1016/j.rmed.2005.10.008 [DOI] [PubMed] [Google Scholar]
- 17.Gale NS, Duckers JM, Enright S, Cockcroft JR, Shale DJ, Bolton CE. Does pulmonary rehabilitation address cardiovascular risk factors in patients with COPD? BMC Pulm Med. 2011;11(1):20. doi: 10.1186/1471-2466-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]