Abstract
Background
The global healthcare system is continuing to confront major challenges during the current COVID-19 pandemic, with the second wave the deadliest one to date. This study aimed to identify and explore the challenges and burdens of frontline healthcare workers during the current pandemic, and to help prepare workforce support plans for them now and in the future.
Methods
A qualitative systematic review method involving thematic synthesis without meta-analysis was used to analyze relevant studies from five databases from November 2020 to February 2021: MEDLINE via PubMed, CINAHL Complete, Embase through Ovid, Scopus, and Web of Science. The quality of the studies was evaluated using the Critical Appraisal Skills Program Qualitative Research Checklist appraisal tools. This systematic review was conducted in accordance with the PRISMA statement. The informants are healthcare workers working at the frontlines and providing care to COVID-19 patients.
Results
Ten studies revealed the burden of healthcare providers during the COVID-19 pandemic, with having the related challenges experienced by 498 participants (doctors, nurses, pediatric nurses, paramedical staff, support staff, and physiotherapists). Our findings fell into four main themes as follows: inadequate preparedness; emotional challenges; insufficient equipment and information; and work burnout.
Conclusion
The study results demonstrate that the COVID-19 pandemic has had an impact on all aspects of life, especially for healthcare providers, who work on the frontlines. The pandemic has affected the frontline workers’ physical and psychological health, causing them to experience emotional distress such as fear, anxiety, depression, and stress. In addition, the pandemic can increase posttraumatic stress disorder, leading to burnout and discontinuity of healthcare workloads to ensure the patients’ safety and the high quality of care provided to the patients.
Keywords: COVID-19, healthcare personnel, qualitative studies, qualitative review, qualitative systematic review
Introduction
Healthcare providers are the frontline soldiers battling against the coronavirus disease 2019 (COVID-19) pandemic. The said pandemic is showing no signs of coming to an end, with a second wave of infections recorded worldwide to date. Most of the new cases spread rapidly through diverse communities.1–4 Worldometer5 reported that as of October 3, 2021, the total prevalence of global cases is 235 million and there have been 4.81 million deaths. As mentioned earlier, the healthcare providers, who are working as the frontliners during the pandemic, are perceived to be overwhelmed and experiencing burnout, even posttraumatic stress disorder (PTSD), from the deluge of COVID-19 cases they have been handling.6,7 Sixty percent of healthcare providers such as physicians, nurses, and pharmacists are reported to have experienced burnout.8–13 Their heavy workloads affect their ability to cope with the demands of their work and to derive a sense of fulfillment from ensuring patients’ safety and providing people with high-quality care.14–17
The responsibility of healthcare providers is to directly provide and manage COVID-19 care processes,18,19 which, considering the overwhelming number of cases, may cause them to develop mental health issues and fail to perceive their own psychological distress symptoms such as anxiety or depression.20,21 The perspectives of healthcare providers experiencing burnout during the current pandemic should thus be obtained to gain a better understanding of how they are handling such situation and to help them resolve their issues.22 This study thus systematically reviewed the qualitative researches that have been conducted on healthcare providers’ experiences during the current pandemic to synthesize their results and to gain a better understanding of the emotional aspects of workload burden. It also obtained the psychological perspectives of the healthcare providers facing heavy workloads due to the current pandemic situation. The study findings may contribute to the development of a return-to-work readiness program for healthcare providers with PTSD or other mental health issues for after the pandemic, to improve their ability to cope with the demands of their work and to manage their holistic health.
Materials and Methods
Study Design
This systematic qualitative review using the thematic synthesis method was conducted22 to analyze the experiences and mental health burdens of healthcare providers during the COVID-19 pandemic.
Search Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was used in this review.23 Five electronic bibliographic databases were searched: MEDLINE via PubMed, CINAHL (Cumulative Index to Nursing and Allied Health Literature) Complete, Embase through Ovid, Scopus, and Web of Science. The following keywords and Medical Subject Headings (MeSH) entries were used: healthcare workers, qualitative research, and SARS-CoV-2 or COVID-19. The data were collected from November 1, 2020 to February 1, 2021. The Critical Appraisal Skills Program Qualitative Research Checklist24 was used to appraise the quality of the method that was used in each of the selected studies. The critique of the research evidence included an assessment of the quality of the method used by each study. The checklist includes 10 questions for evaluating the study’s aims and objectives, the study design, the recruitment strategy used, the data analysis and synthesis, the results and findings, and the overall research value; in sum, the study’s quality, integrity, and overall research value. Each question is answerable with “yes,” “no,” “unclear,” or “not applicable,” as shown in Table 1. The studies that obtained less than 6 points were excluded. Two researchers independently assessed the eligible articles, and a third researcher conducted quality check and appraisal. Any disagreement or conflict was resolved through a discussion among the researchers.
Table 1.
The Critical Appraisal Skills Program Qualitative Research Checklist
| Categories | Articles | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A125 | A226 | A327 | A428 | A529 | A630 | A731 | A832 | A933 | A1034 | |
| Was there a clear statement of the aims of the research? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Is the qualitative method appropriate? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the research design appropriate for addressing the aims of the research? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the recruitment strategy appropriate for the aims of the research? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Were the data collected in a way that addressed the research issue? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the relationship between the researcher and the participants adequately considered? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Were ethical issues taken into consideration? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the data analysis sufficiently rigorous? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Is there a clear statement of the findings? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| How valuable is the research? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
Abbreviation: Y, “yes”.
Inclusion and Exclusion Criteria
This qualitative systematic review included empirical primary studies with a qualitative research design and published in English that aimed to obtain the perceptions of healthcare providers working with COVID-19 patients. Non-English studies that did not focus on healthcare workers and presented research findings for other pandemic diseases were not included in the review.
Selection and Quality Assessment
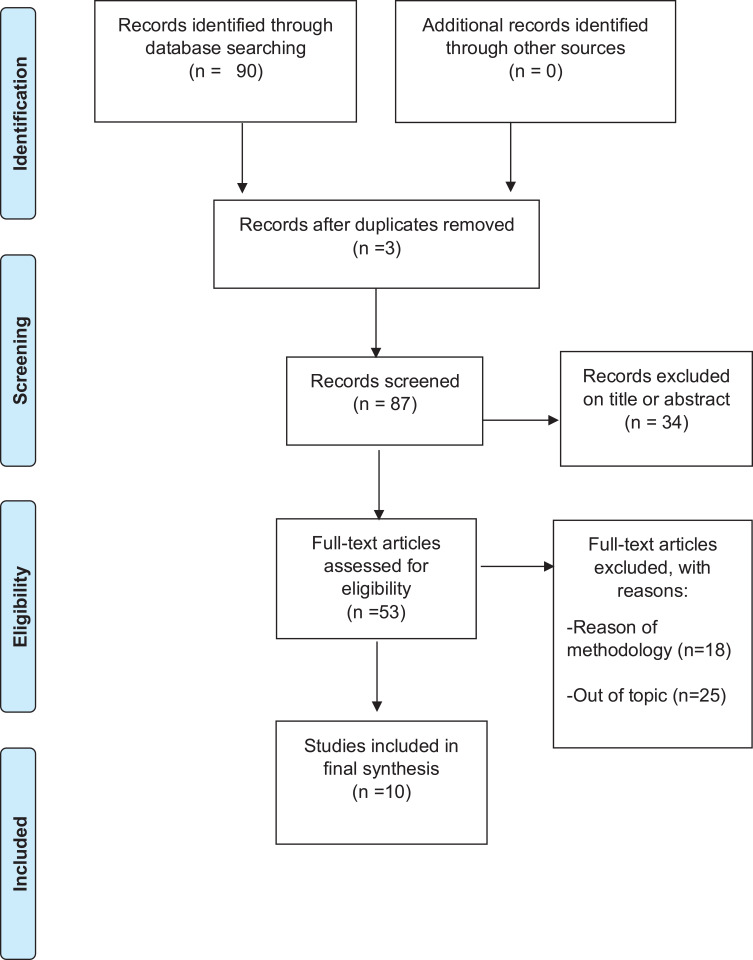
Ninety articles were initially identified in the search. From among these, 13 duplicates were identified through EndNote X9 (Thomson Reuters, PA, USA) and were removed. Sixty-four articles with only the abstract provided were screened by title and abstract to eliminate those among them that were clearly irrelevant to the review, and the 43 full-text articles were screened by title, method, and outcomes for the same purpose. The eligible articles were retrieved and were further discussed. In total, 20 articles were potentially relevant full-text papers, but 10 of these were excluded due to their research design. Finally, only 10 articles met all the inclusion criteria and were thus qualified to be included in the rigorous appraisal (Figure 1).
Figure 1.
PRISMA flow diagram of the selection process.
Note: Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71.23
Data Extraction
The following data were extracted from the selected articles: title, year of publication, language published in, country where the study was conducted, study objectives, study method used, sample size, data analysis method used, and findings.
Data Analysis
A narrative table and summary were prepared by the first author while the second author checked the data accuracy. For data synthesis, the thematic analysis and synthesis method developed by Thomas Harden22 was used to categorize the recurring themes in the 10 selected qualitative studies. Thematic synthesis has been found to generate initial codes from the selected articles, describe the themes based on the codes with similar results, and provide basis for deciding on the review and abstract themes, all on the basis of clear qualitative data.
The authors worked independently to review and develop codes, and then each author aggregated the analytical themes twice for each study to double-check the methodical rigor. The primary investigator (PI) and co-primary investigator (co-PI) then reviewed the codes and themes to ensure that these were valid.
Results
Study Characteristics
This qualitative systematic review included 10 primary studies with a qualitative design.25–34 All the studies were conducted in 2020 in China (n = 2), the United States (n = 2), the United Kingdom (n = 2), South Korea (n = 1), Brazil (n = 1), Iran (n = 1), and Lebanon (n = 1), and the articles on them were published in the same year. These 10 selected studies had 498 healthcare worker participants, including doctors, nurses, pediatric nurses, paramedics, support staff, and physiotherapists, as summarized in Table 2.
Table 2.
Summary of Included Studies
| Author (Year), Country | Study Aim | Target Sample | Study Design | Data Collection Method | Major Findings |
|---|---|---|---|---|---|
| Góes et al25 (2020), Brazil | To identify the challenges faced by pediatric nurses in relation to the COVID-19 pandemic | Pediatric nurses (n = 26) | Qualitative approach | Semi-structured interviews | • Presence of stress from being frontline workers • Limited time to prepare for care provision • Insufficient number of workers, leading to the healthcare providers’ exhaustion and burnout while providing care to COVID-19 patients |
| Fawaz and Samaha26 (2020), Lebanon | To explore the psychological effects of being quarantined following exposure to COVID-19 | Healthcare professionals (n = 13) | Qualitative research | Semi-structured interviews and phenomenology analysis | • Presence of psychological challenges due to quarantines • Presence of fear, anger, being conflicted, frustration, anxiety • Conflict between professional duty and family obligation • Stigma • insufficient equipment and information |
| Arnetz et al27 (2020), USA | To explore the US nurses’ perceptions of the most salient sources of their stress in the early stages of the COVID-19 pandemic | Nurses (n = 455) | Qualitative content analysis of open-ended questions | • The open-ended question “What are the most stressful situations you have dealt with during the COVID-19 pandemic?” • Thematic analysis, providing the framework of the code system |
• Emotional distress caused by dealing with many unknowns during the pandemic • Exhaustion with the pandemic • Helplessness during the pandemic • Lack of trust in the workplace • Inadequate protective equipment (eg, PPEs) |
| Lee and Lee28 (2020), South Korea | To explore the experiences of nurses who provided care for COVID-19 patients | Hospital nurses (n = 18) | Qualitative study of phenomenological analysis | In-depth individual interviews by telephone | • Emotional distress • Lack of preparation for providing COVID-19 patient care • Unfamiliar work, challenges posed by having to wear PPEs, and unpredictable nature of the COVID-19 pandemic • Burnout from heavy workload • Need for support from family and friends |
| George et al29 (2020), Bangalore | To describe the initial dilemma and mental stress experienced by healthcare providers, and the adaptive measures taken by them | A healthcare team of doctors, nurses, and paramedical and support staff (n = 42) |
Mixed-method study | Qualitative in-depth interviews | • Emotional distress such as stress, stigma, fear, guilt, and isolation • Exhaustion and burnout due to heavy workload |
| Galehdar et al30 (2020), Iran | To explore nurses’ experiences of psychological distress while providing care to COVID-19 patients | Nurses (n = 11) | Qualitative research | Conventional content analysis | • High level of psychological distress • Negative feeling toward PPEs |
| Nyashanu et al31 (2020), UK | To explore the challenges faced by different frontline workers in health and social care during the COVID-19 pandemic | Healthcare providers (n = 40), including nurses (n = 15), support workers (n = 15), and managers (n = 10) | Explorative qualitative research | In-depth, one-to-one, semi-structured interviews | • Inadequate pandemic preparedness • Psychological distress such as anxiety and fear • Challenges of social distancing |
| Bennett et al32 (2020), UK | To gain insights into the experiences and concerns of frontline National Health Service (NHS) workers while caring for COVID-19 patients | Community of NHS workers (doctors, nurses, and physiotherapists) with social media access (n = 54) | Qualitative analysis | Thematic analysis to identify themes | • Posttraumatic distress caused by being overwhelmed with one’s workload • Feeling of shock from the rapidly changing nature of the pandemic • Healthcare providers’ perception of inequality in the workplace, leading to rifts between the senior manager and the frontline staff |
| Eftekhar et al33 (2020), Iran | To undertake an in-depth exploration of the experiences of healthcare staff working during the COVID-19 pandemic | Healthcare professionals (n = 97) | Qualitative study | Thematic analysis and semi-structured interviews | • Adaptation to the pandemic era. • Psychological distress in the long term, such as anxiety, fear, depression, helplessness, hopelessness, and burnout |
| Liu et al34 (2020), China | To describe the experiences of physicians and nurses caring for COVID-19 patients in the early stages of the pandemic | Nurses (n = 9) Physicians (n = 4) |
Qualitative study | • Semi-structured, in-depth interviews by telephone • Data analysis using the phenomenological method |
• Challenges in providing care in COVID-19 wards • Heavy workloads • Perception of fear caused by working as a frontliner in a stressful situation |
Abbreviations: COVID-19, coronavirus disease 2019; PPE, personal protective equipment.
The 10 selected studies were qualitative studies, but one used a mixed-method approach29 with appropriate rigor. The data collection methods that were used by the studies consisted of semi-structured, one-to-one, and in-depth interviews. Most of the studies conducted the interviews by telephone and through social media, and used thematic and content analyses as data analysis methods.
Main Findings
The thematic synthesis identified four themes from the data regarding the participants’ real experiences in providing care to patients during the COVID-19 pandemic: inadequate preparedness, emotional challenges, insufficient equipment and information, and work burnout, as shown in Table 3.
Table 3.
Summary of Thematic Analysis
| Main Themes | Code in the Texts |
|---|---|
| Inadequate preparedness | • Frontline work without preparedness28 • Limited pandemic preparedness31 • Poor coping with rapid changes32 |
| Emotional challenges | • Fear of unpredictable enemy28 • Emotional distress due to the fear of contracting the virus30 • Stigma of contracting the virus29 • Anxiety and fear among frontline workers31 • New experiences of drastic changes32 • Negative psychological effects33 Fear of providing COVID-19 care27 • Fear of transmitting the virus34 • Fear of being in the frontlines25 • Fear of contracting the virus26 • Stigma26,29 |
| Insufficient equipment and information | • Lack of standardized guidelines for COVID-19 prevention and control31 • Inadequate training and information on new diseases27,29 • Dealing with an unpredictable pandemic27 • Lack of PPEs26,29 |
| Work burnout | • Burnout due to being in the frontlines, fighting against COVID-1928,29,33,34 • Exhaustion and burnout due to the widespread COVID-19 infection27 • Inequality within the healthcare system32 |
Abbreviations: COVID-19, coronavirus disease 2019; PPE, personal protective equipment.
Discussion
In this research work, 10 empirical qualitative studies were systematically reviewed to synthesize their findings and to identify how healthcare providers manage their mental health amidst their burdens while working with COVID-19 patients. They play crucial roles as frontliners coping with a disease of which little is known and that is thus unpredictable This review addressed the experience and perceptions of the healthcare providers worldwide to gain a better understanding of how they feel while working with serious COVID-19 patients. Altogether, the findings of this research work can help healthcare providers manage and improve their mental health status. The study findings offer a deeper understanding of healthcare providers’ perceptions of their psychological conditions in four themes: (1) inadequate preparedness; (2) emotional challenges; (3) insufficient equipment and information; and (4) work burnout.
The first theme was inadequate preparedness or being poorly prepared for working during a serious pandemic. Most of the healthcare providers in the reviewed studies stated that they were overwhelmed as they had to work in crisis situations, which affected them physically and emotionally as they had limited time to prepare for the rapid increase of new cases. Lee et al (2020)28 explored the experiences of South Korean nurses who were also unprepared to work with COVID-19 patients as they were unfamiliar with the little-known disease. George et al (2020)32 conducted a study on Indian healthcare providers working in an urban slum area in the first 40 days of the crisis who had limited preparation for such and who thus developed several mental health problems. Bennett et al (2020)32 presented the experiences of the UK frontliners who could hardly cope with the rapid changes occurring during the pandemic, which made them suffer from physical and mental health issues while taking care of COVID-19 patients.
The second theme that was found in the study data was facing the challenges posed by several types of emotional distress that developed during the pandemic, such as fear,29,31 stigma,26,29 anxiety,31,33 and depression.31 33 Goes et al (2020)25 found that in Brazil, pediatric nurses are suffering from stress as frontline workers, in addition to psychological distress, which may lead to discontinued occupational health and poor quality of care provided. Fawaz and Samaha (2020)26 explored the perceptions of Lebanese healthcare professionals who had been quarantined after caring for patients with COVID-19. They had developed psychological distress, such as fear, anger, frustration, and stigma, and they were overwhelmed by the conflicts that they encountered between their professional duties and their duties toward their families. Arnet et al (2020) 27 surveyed the sources of stress in the US nurses working with COVID-19 patients and found that most of them were overwhelmed by the unpredictability of COVID-19 and were afraid of passing on the virus to their families. Lee et al (2020)28 found that South Korean nurses fear and struggle with working as frontliners in the unpredictable pandemic. George et al (2020)29 found that the Indian healthcare professionals who worked in the frontlines in the first 40 days of the COVID-19 crisis perceived emotional distress such as stress caused by the unpredictable nature of the new virus strains emerging and fear of contracting the COVID-19. Also, they had been stigmatized and felt guilt toward their families and friends, who could contract the virus from them. Galehdar et al (2020)28 explored Iranian nurses’ experiences of mental distress while working with COVID-19 patients and found that most of them had a high level of psychological distress (eg, anxiety and fear) and stated that they considered working during the COVID-19 pandemic a waste of their time. Nyashanu et al (2020)31 conducted a study on the UK frontline workers providing care to COVID-19 patients and found that most of them had anxiety and fear caused by the limited time that they had to prepare for the unpredictable pandemic, and their poor preparation for such as a result. Bennett et al (2020)32 stated that the members of the UK National Health Service (doctors, nurses, physiotherapists) are insecure about providing care to COVID-19 patients due to their limited time to prepare for the pandemic and the rapid changes occurring in the disease. Eftekhar et al (2020)33 found that the Iranian healthcare providers who are in the frontlines during the COVID-19 pandemic perceive negative emotions in themselves that may affect them in the long term, such as anxiety, depression, fear, hopelessness, and burnout. Consequently, the pandemic is affecting them psychologically, making them feel overwhelmed and causing them to suffer from several emotional problems due to their lack of experience in dealing with the dreaded disease, their lack of pandemic preparedness, and the inadequate control guidelines available to prevent their infection.
The third theme obtained from the study data was the fact that there are insufficient equipment and information about the pandemic. Goes et al (2020)25 demonstrated that Brazilian pediatric nurses are facing challenges due to the insufficiency of the available protective equipment (eg, personal protective equipment [PPE]) and of the guidelines for the standard precautions for frontline workers during the pandemic. Similarly, Arnetz et al (2020) 27 investigated the US nurses’ sources of stress and found that these were their lack of trust in workplace safety due to the inadequate protective equipment (eg, PPEs) and the poor preparation of the protocol or guideline for providing care to COVID-19 patients. Also, Nyashanu et al (2020)31 found that the UK healthcare workers have inadequate protective equipment such as PPEs.
Finally, the fourth theme obtained from the study data was work burnout. Most of the healthcare providers worldwide are overwhelmed by their workload due to the insufficiency of the healthcare staff on account of the rapid and wide spread of the disease, and perceive inequality within the healthcare system. Arnetz et al (2020)27 found that the US nurses were exhausted and felt helpless in the workplace during the early stages of the pandemic as they did not trust the management and as there were inadequate sources of help for them throughout the pandemic thus far. They were also not comfortable donning a PPE while working. Lee et al (2020)28 reported that the South Korean nurses’ burnout due to the pandemic is affecting them physically and emotionally. That is, they feel exhausted and fear that they will fail to cope with their posttraumatic distress, which directly affects their relationship with their co-workers and patients and the quality of care that they provide. George et al (2020)29 reported that Bangalore’s healthcare providers working with COVID-19 patients are exhausted and burnt out due to their heavy workload. Bennett et al (2020)32 reported that the UK healthcare workers perceive the existence of inequity in the workplace, as shown by the rifts between the senior managers and those who are on the frontlines. Eftekhar et al (2020)33 found that the Iranian healthcare providers have difficulty adapting to the pandemic and are largely unsuccessful in coping with their emotional issues, thus experiencing burnout. Liu et al (2020)34 found that the nurses and physicians in China are overwhelmed by their heavy workloads and are thus fearful and stressed due to the unpredictable pandemic.
To date, the COVID-19 pandemic has changed the world. Healthcare providers worldwide are unprepared for it and are facing many uncertainties with regard to it. They have been working without proper preparation, training, or standardized guidelines. Consequently, they are unsuccessful in their coping responses due to the insufficiency of the relevant information, equipment, support, and equality of respect to work. Healthcare providers working with COVID-19 patients are overwhelmed and exhausted by their workload burden34 and by the uncertainties of the pandemic and have thus come to experience burnout. More than 50% of the healthcare frontliners are reported to have become burnt out.35–38 Additionally, most of them have emotional challenges stemming from their fear of death, guilt for transmitting the virus to their families, and stigma from the community.29 Also, they feel depressed due to their multiple duties, their challenging new work environments (eg, having to work in a negative room), and their discomfort with their PPEs especially in restricted zones.34 Besides, they experience loss of control when carrying out heavy duties, expressing that they work like robots, enjoy their human relationships in the workplace less, and feel sad that they have to avoid touching, hugging, and talking with their co-workers.33
In summary, globally, healthcare providers who are on the frontlines of the battle against the COVID-19 pandemic, providing care to COVID-19 patients, are struggling and experiencing burnout, making them frustrated and stressed out due to posttraumatic stress.32 This research work focused on how healthcare workers manage to work under stress during the COVID-19 pandemic. On the basis of the study’s findings, it is strongly recommended that healthcare providers be equipped with pandemic preparedness to help them cope with the demands of their work before, during, and after the COVID-19 pandemic. Such frontliners may suffer from mental health issues as they have dedicated themselves to providing direct care for their COVID-19 patients and carrying out their duties toward their family at the same time. Pandemic preparedness may prevent symptoms of emotional distress and may promote teamwork in carrying the burdens posed by the pandemic, thus preventing the occurrence of occupational health issues, helping healthcare providers maintain positive relationships in the workplace, and improving the patients’ safety and the quality of care provided to the patients.
Conclusion
Healthcare providers are the ones who are battling against COVID-19 at the frontlines, in the midst of rapidly changing procedures for dealing with the ongoing crisis. They experience challenges in dealing with the unpredictable pandemic due to their limited preparedness, the rapid changes occurring in the disease, and the difficulty of performing their duties due to the lack of protocol, accurate information, and proper equipment for preventing contamination. Limited preparedness may lead to physical and psychological problems such as high levels of stress, anxiety, fear, helplessness, hopelessness, anger, and stigma. However, healthcare providers working with COVID-19 patients endeavor to fulfill their duties professionally and sacrifice as much as they could. On the other hand, their heavy workload may lead to their burnout and to the discontinuity of their healthcare practice, and may threaten the patients’ safety. The findings from this research work suggest that a better understanding of healthcare providers’ experiences while providing care to COVID-19 patients may help in developing training programs for them and in enabling them to better manage the pandemic. In addition, programs focusing on the PTSD symptoms of healthcare providers can be implemented to help them more effectively cope with the current crisis, improve their mental health during work, and reduce their posttraumatic disorders stemming from the COVID-19 pandemic.
Acknowledgment
We would like to thank the participants in our work for their valuable data, the reviewers for their helpful comments and suggestions to improve our study. The study was partially funded by the Suan Sunandha Rajabhat University in Bangkok, Thailand.
Abbreviations
COVID-19, CoV, novel coronavirus; coronavirus disease 2019; SARS-CoV, Severe acute respiratory syndrome; MERS-CoV, Middle East Respiratory Syndrome; PRISMA, Preferred reporting items for systematic reviews and meta-analyses; PPE, personal protective equipment, PTSD, posttraumatic stress disorder.
Disclosure
The authors of this study declare that they have no conflicts of interest in this project.
References
- 1.Bateman ME, Hammer R, Byrne A, et al. Death Cafés for prevention of burnout in intensive care unit employees: study protocol for a randomized controlled trial (STOPTHEBURN). Trials. 2020;21(1):1019. doi: 10.1186/s13063-020-04929-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suksatan W, Choompunuch B, Koontalay A, Posai V, Abusafia AH. Predictors of Health Behaviors Among Undergraduate Students During the COVID-19 Pandemic: a Cross-Sectional Predictive Study. J Multidiscip Healthc. 2021;14:727–734. doi: 10.2147/JMDH.S306718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choompunuch B, Suksatan W, Sonsroem J, Kutawan S, In-udom A. Stress, adversity quotient, and health behaviors of undergraduate students in a Thai university during COVID-19 outbreak. Belitung Nursing J. 2021;7(1):1–7. doi: 10.33546/bnj.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Posai V, Suksatan W, Choompunuch B, Koontalay A, Ounprasertsuk J, Sadang JM. Assessment of the Health-Promoting Behaviors of Hospitalized Patients with Non-Communicable Diseases During the Second Wave of COVID-19. J Multidiscip Healthc. 2021;14:2185–2194. doi: 10.2147/JMDH.S329344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Worldometers. COVID-19 Coronavirus pandemic; 2021. https://www.worldometers.info/coronavirus/. Accessed October 3, 2021.
- 6.Duarte I, Teixeira A, Castro L, et al. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health. 2020;20(1):1885. doi: 10.1186/s12889-020-09980-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaku SM, Moscoso A, Sibeoni J, Sravanti L. Transformative learning in early-career child and adolescent psychiatry in the pandemic. Lancet Psychiatry. 2021;8(2):e5. doi: 10.1016/S2215-0366(20)30524-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammer R, Ravindran N, Nielsen N. Can Death Cafés resuscitate morale in hospitals? Med Humanit. 2021;47(1):2. doi: 10.1136/medhum-2018-011607 [DOI] [PubMed] [Google Scholar]
- 9.Dzau VJ, Kirch DG, Nasca TJ. To care is human—collectively confronting the clinician-burnout crisis. N Engl J Med. 2018;378(4):312–314. doi: 10.1056/NEJMp1715127 [DOI] [PubMed] [Google Scholar]
- 10.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement: burnout syndrome in critical care health care professionals: a call for action. Am J Critical Care. 2016;25(4):368–376. doi: 10.4037/ajcc2016133 [DOI] [PubMed] [Google Scholar]
- 11.Edmondson EK, Kumar AA, Smith SM. Creating a Culture of Wellness in Residency. Acad Med. 2018;93(7):966–968. doi: 10.1097/ACM.0000000000002250 [DOI] [PubMed] [Google Scholar]
- 12.Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001. doi: 10.5811/westjem.2015.9.27945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sajjadi S, Norena M, Wong H, Dodek P. Moral distress and burnout in internal medicine residents. Can Med Educ J. 2017;8(1):e36–e43. doi: 10.36834/cmej.36639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watkins S, Ruskin KJ, Schwengel DA. Patient Safety and Physician Well-Being: impact of COVID-19. ASA Monitor. 2021;85(1):21. doi: 10.1097/01.ASM.0000725848.61435.b5 [DOI] [Google Scholar]
- 15.Carayon P, Perry S. Human factors and ergonomics systems approach to the COVID-19 healthcare crisis. Int J Quality Health Care. 2021;33(Supplement_1):1–3. doi: 10.1093/intqhc/mzaa109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139(3):e20162163. doi: 10.1542/peds.2016-2163 [DOI] [PubMed] [Google Scholar]
- 17.Knupp AM, Patterson ES, Ford JL, Zurmehly J, Patrick T. Associations among nurse fatigue, individual nurse factors, and aspects of the nursing practice environment. JONA. 2018;48(12):642–648. doi: 10.1097/NNA.0000000000000693 [DOI] [PubMed] [Google Scholar]
- 18.Cole A, Ali H, Ahmed A, Hamasha M, Jordan S. Identifying Patterns of Turnover Intention Among Alabama Frontline Nurses in Hospital Settings During the COVID-19 Pandemic. J Multidiscip Healthc. 2021;14:1783–1794. doi: 10.2147/JMDH.S308397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paiano M, Jaques AE, Nacamura PAB, Salci MA, Radovanovic CAT, Carreira L. Mental health of healthcare professionals in China during the new coronavirus pandemic: an integrative review. Rev Bras Enferm. 2020;73((Suppl 2)):e20200338. doi: 10.1590/0034-7167-2020-0338 [DOI] [PubMed] [Google Scholar]
- 20.Sommerstein R, Fux CA, Vuichard-Gysin D, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect Control. 2020;9(1):100. doi: 10.1186/s13756-020-00763-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. doi: 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Critical Appraisal Skills Programme. CASP qualitative research checklist; 2013. https://www.casp-uk.net/casp-tools-checklists.Accessed February 1, 2021.
- 25.Góes FGB, Silva A, Santos AS, et al. Challenges faced by pediatric nursing workers in the face of the COVID-19 pandemic. Rev Lat Am Enfermagem. 2020;28:e3367. doi: 10.1590/1518-8345.4550.3367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fawaz M, Samaha A. The psychosocial effects of being quarantined following exposure to COVID-19: a qualitative study of Lebanese health care workers. Int J Soc Psychiatry. 2020;66(6):560–565. doi: 10.1177/0020764020932202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse Reports of Stressful Situations during the COVID-19 Pandemic: qualitative Analysis of Survey Responses. Int J Environ Res Public Health. 2020;17(21):8126. doi: 10.3390/ijerph17218126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee N, Lee H-J. South Korean Nurses’ Experiences with Patient Care at a COVID-19-Designated Hospital: growth after the Frontline Battle against an Infectious Disease Pandemic. Int J Environ Res Public Health. 2020;17(23):9015. doi: 10.3390/ijerph17239015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.George CE, Inbaraj LR, Rajukutty S, de Witte LP. Challenges, experience and coping of health professionals in delivering healthcare in an urban slum in India during the first 40 days of COVID-19 crisis: a mixed method study. BMJ Open. 2020;10(11):e042171. doi: 10.1136/bmjopen-2020-042171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galehdar N, Kamran A, Toulabi T, Heydari H. Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: a qualitative study. BMC Psychiatry. 2020;20(1):489. doi: 10.1186/s12888-020-02898-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nyashanu M, Pfende F, Ekpenyong M. Exploring the challenges faced by frontline workers in health and social care amid the COVID-19 pandemic: experiences of frontline workers in the English Midlands region, UK. J Interprof Care. 2020;34(5):655–661. doi: 10.1080/13561820.2020.1792425 [DOI] [PubMed] [Google Scholar]
- 32.Bennett P, Noble S, Johnston S, Jones D, Hunter R. COVID-19 confessions: a qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open. 2020;10(12):e043949. doi: 10.1136/bmjopen-2020-043949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eftekhar AM, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: a qualitative study. Am J Infect Control. 2021;49(5):547–554. doi: 10.1016/j.ajic.2020.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Q, Luo D, Haase JE, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Global Health. 2020;8(6):e790–e798. doi: 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maglalang DD, Sorensen G, Hopcia K, et al. Job and family demands and burnout among healthcare workers: the moderating role of workplace flexibility. SSM Population Health. 2021;14:100802. doi: 10.1016/j.ssmph.2021.100802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Torrente M, Sousa PAC, Sánchez-Ramos A, et al. To burn-out or not to burn-out: a cross-sectional study in healthcare professionals in Spain during COVID-19 pandemic. BMJ Open. 2021;11(2):e044945. doi: 10.1136/bmjopen-2020-044945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. 2021;94(6):1345–1352. doi: 10.1007/s00420-021-01695-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dzeng E, Wachter RM. Ethics in Conflict: moral Distress as a Root Cause of Burnout. J Gen Intern Med. 2020;35(2):409–411. doi: 10.1007/s11606-019-05505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]